- Research article
- Open access
- Published:
Long-term follow up Helicobacter Pylori reinfection rate after second-line treatment: bismuth-containing quadruple therapy versus moxifloxacin-based triple therapy
BMC Gastroenterology volume 13, Article number: 138 (2013)
Abstract
Background
The increasing trend of antibiotic resistance requires effective second-line Helicobacter pylori (H. pylori) treatment in high prevalence area of H. pylori. The aim of our study was to evaluate the reinfection rate of H. pylori after second-line treatment that would determine the long-term follow up effect of the rescue therapy.
Methods
A total of 648 patients who had failed previous H. pylori eradication on standard triple therapy were randomized into two regimens: 1, esomeprazole (20 mg b.i.d), tripotassium dicitrate bismuthate (300 mg q.i.d), metronidazole (500 mg t.i.d), and tetracycline (500 mg q.i.d) (EBMT) or 2, moxifloxacin (400 mg q.d.), esomeprazole (20 mg b.i.d), and amoxicillin (1000 mg b.i.d.) (MEA). At four weeks after completion of eradication therapy, H. pylori tests were performed with 13C urea breath test or invasive tests. In patients who maintained continuous H. pylori negativity for the first year after eradication therapy, H. pylori status was assessed every year. For the evaluation of risk factors of reinfection, gender, age, clinical diagnosis, histological atrophic gastritis or intestinal metaplasia were analyzed.
Results
The recrudescence rate of the EBMT was 1.7% and of the MEA group 3.3% (p = 0.67). The annual reinfection rate of H. pylori of EBMT was found to be 4.45% and the MEA group 6.46%. Univariate analysis (Log-rank test) showed no association with any clinical risk factor for reinfection.
Conclusions
The long-term reinfection rate of H. pylori stayed low in both of bismuth-containing quadruple therapy and moxifloxacin-based triple therapy; thus reinfection cannot affect the choice of second-line treatment.
Trial registration
Clinical Trial Registration Number NCT01792700
Background
Helicobacter pylori (H. pylori) is a common pathogen of the gastric mucosa. It is estimated that at least 50% of the world’s human population has H. pylori infection [1]. Since the majority of patients with H. pylori infection do not have any related clinical disease, routine screening is not considered [2]. However, as the current evidence suggests that H. pylori play a major role in peptic ulcer disease, gastric MALT lymphoma and in gastric cancer [3], screening and treatment in these diseases are recommended in several guidelines [2, 4–7]. In addition, European guidelines recommend eradicating H. pylori infection in first-degree relatives of patients with gastric cancer, in long term NSAIDS or acid suppression users and in patients with functional dyspepsia [4]. According to these guidelines, public health efforts toward eradication will be more effective in H. pylori high prevalence areas. Naturally, it is expected that increasing use of antibiotics must lead to increased resistance of antibiotics. Currently, the most commonly used initial treatment is a triple regimen combining a proton pump inhibitor (PPI) with two antibiotics (clarithromycin and amoxicillin/or metronidazole) for the eradication of H. pylori[2, 4–7]. Although this regimen has been shown to be effective in numerous clinical trials, the most recent data show that the eradication rate has declined to less than 80% worldwide, largely related to development of resistance to clarithromycin [8]. In Korea, the recent eradication rate of this regimen was less than 80% in a long-term follow up study (≥ 5 years) [9, 10]. Therefore, this decreasing eradication rate requires effective second-line treatment. Many clinicians have been using second-line therapy with bismuth-containing quadruple therapy or including fluoroquinolone antibiotics such as levofloxacin and moxifloxacin. In this situation, reinfection of H. pylori will determine the long-term effect of the eradication therapy for H. pylori. If a regimen shows a high reinfection rate, then this eradication therapy should be avoided or strictly used only when absolutely indicated for H. pylori eradication. We reported the long-term annual reinfection rate of H. pylori in standard PPI-based triple therapy to be 3.51% per year in Korea [11]. Now that second-line therapy is frequently used there is increasing interest regarding the reinfection and recrudescence rates after rescue therapy. However, there are few reports regarding the reinfection rate of H. pylori after quadruple therapy [12] and none for quinolone based triple therapy. From this background the aim of our study was to evaluate the reinfection rate of H. pylori after two kinds of second-line treatment over a long-term follow up period. In addition, we investigated the risk factors for reinfection after this second-line treatment.
Methods
Study population
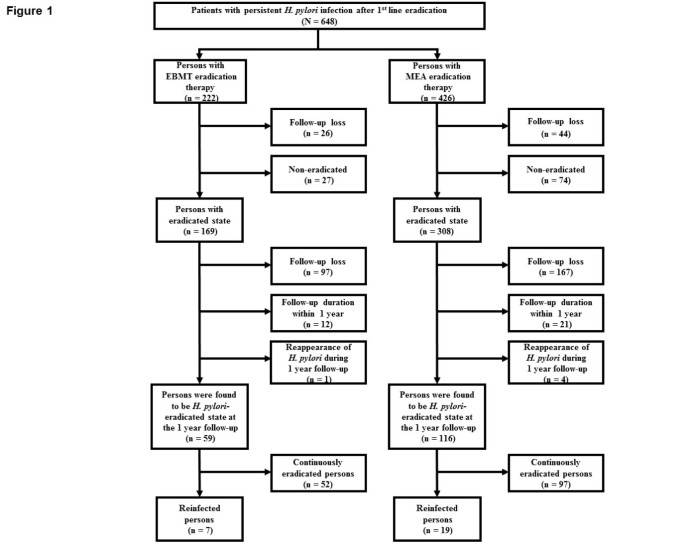
The schematic flow of this study is shown in Figure 1. This was a prospective study performed between 2003 and 2010 at Seoul National University Bundang Hospital in Korea. A total of 648 patients with persistent H. pylori infection after first-line treatment (PPI-based triple therapy) were enrolled. PPI-based triple therapy included PPI (standard dose), amoxicillin 1 g, and clarithromycin 500 mg, all twice daily, for 7 days. Patients were considered persistent H. pylori infection if 13C-urea breath test (UBT) or invasive H. pylori test (Giemsa histology, CLO test, culture) were positive despite PPI-based triple therapy. Patients were excluded from the study if they had a history of renal or hepatic impairment, previous gastric surgery, pregnancy or lactation, therapy with steroids or non-steroidal anti-inflammatory drugs, or therapy with a proton pump inhibitor (PPI) or antibiotics within four weeks of entry. Between 2003 and 2006, the 44 patients with persistent H. pylori infection were treated with bismuth-containing quadruple therapy. Between 2007 and 2010, 604 patients with persistent H. pylori infection were randomized into two kinds of second-line therapy (bismuth-containing quadruple therapy or moxifloxacin-based triple therapy). However, if the patient preferred one regimen, after sufficient information for side effect and eradication rate of each regimen a change was permitted. Finally, 222 patients were treated for 14 days with esomeprazole 20 mg b.i.d, tripotassium dicitrate bismuthate 300 mg q.i.d, metronidazole 500 mg t.i.d, and tetracycline 500 mg q.i.d (EBMT) as second-line treatment regimen for H. pylori infection. 426 patients were treated for 14 days with moxifloxacin 400 mg q.d, esomeprazole 20 mg b.i.d, and amoxicillin 1000 mg b.i.d (MEA) as second-line treatment regimen for H. pylori infection. At four weeks after completion of the second-line treatment, H. pylori eradication was evaluated by 13C-UBT or invasive tests. Invasive tests were performed in the patients in whom follow up endoscopic examination was necessary for peptic ulcer, adenoma or gastric cancer. H. pylori negative status after eradication was defined as a negative 13C-UBT or all negative of Giemsa stain, CLO test, and culture. Among 222 patients with EBMT eradication therapy and 426 patients with MEA eradication therapy, 169 patients and 308 patients were found to be in eradicated status, respectively (Figure 1).
All subjects provided informed consent, and the study protocol was approved by the Ethical Committee at Seoul National University Bundang Hospital. ClinicalTrials.gov registration number is NCT01792700.
Invasive Helicobacter pyloritest (Giemsa histology, CLO test, and culture) and histology
To determine the presence of current H. pylori infection, 10 biopsy specimens were taken from the gastric mucosa at each endoscopy (two biopsy specimens each from the greater curvature of the antrum and body, and three each from the lesser curvature of the antrum and body). Among them, four biopsy specimens (one each from the greater curvature and lesser curvature of the antrum and body) were fixed in formalin, and used for determination of H. pylori infection by Giemsa staining. Another four specimens from the four gastric mucosa areas mentioned above were used for H. pylori culturing. The remaining two specimens from the lesser curvature of the antrum and body were used for the rapid urease test (CLO test; Delta West, Bentley, Australia).
Four of the biopsy specimens used for determination of H. pylori infection were also used for histological evaluation. These specimens were examined for the presence of gastric atrophy and intestinal metaplasia by H&E staining. The presence of atrophy on any of four specimens was diagnosed as gastric atrophy, and the same method was applied to intestinal metaplasia. The definition of atrophy is the loss of appropriate glands including both metaplastic and non-metaplastic atrophy. Both metaplastic and non-metaplastic atrophy can be allocated to one of three grades of severity using grading criteria modeled on those suggested by the original and the updated Sydney System [13].
13C-urea breath test
Patients fasted for 4 h before testing. Then, 100 mg of 13C-urea powder (UBiTkit; Otsuka Pharmaceutical, Tokyo, Japan) was dissolved in 100 mL water and administered orally; a second breath sample was collected 20 min later. The collected samples were analyzed using an isotope-selective, non-dispersive infrared spectrometer (UBiT-IR300; Otsuka Pharmaceutical). The cutoff value used for H. pylori eradication was 2.5‰.
Follow-up of H. pyloritests
All of the eradicated patients received gastroscopy with invasive tests (modified Giemsa stain and CLO test) not only from greater and lesser curvature of antrum but also from body after 1 year. If any one of these tests were positive then the patient was regarded as recrudescence case. After this time the patients were followed up for one year with gastroscopy with invasive tests. However, when the patients preferred 13C-UBT or wanted to receive the gastroscopy every other year it was also accepted because the Korea government national health insurance program recommends biannual endoscopy instead of one year.
Statistical analysis
The annual reinfection rate (percentage per year) of H. pylori was calculated as (total number of infected patients/ cumulative observation years for all patients) X 100.
SPSS for Windows (version 18.0; SPSS, Inc., an IBM Company, Chicago, Illinois, USA) was used for all statistical analyses. Categorical variables were analyzed using the Pearson chi-square test or Fisher’s exact test, and continuous variables were analyzed using independent samples t-test. The risk of H. pylori reinfection with time was estimated using the Kaplan-Meier method. To determine the risk factors for reinfection, we used the log-rank test. Null hypotheses of no difference were rejected if p-values were less than 0.05.
Results
Patient characteristics
Among eradicated 169 patients in the EBMT group and eradicated 308 patients in the MEA group, 59 patients and 116 patients maintained H. pylori-negative status continuously for one year, respectively (Figure 1). Specifically, 110 patients dropped out in the EBMT group and 192 in the MEA group for the following three reasons: 97 patients in the EBMT group and 167 in the MEA group for not returning for gastroscopy or 13C-UBT after treatment, 12 in the EBMT group and 21 in the MEA group for follow-up duration within 1 year, 1 patient in the EBMT group and 4 in the MEA group for reappearance of H. pylori during 1 year follow-up. Finally, 59 patients and 116 patients in each group maintained H. pylori-negative continuously at one year. The demographic and clinical characteristics of two study groups, who maintained H. pylori-negative continuously at one year after the EBMT or MEA therapy, are summarized in Table 1. Gender, the mean age of the patients, clinical diagnosis, atrophic gastritis, and intestinal metaplasia of the two groups were similar. The enrolled early gastric cancer patients were cured by endoscopic submucosal dissection and follow-up was continuously performed regularly. During long-term follow-up patients in the EBMT or in the MEA group were divided into two groups: reinfected group and continuously eradicated group. The demographic and clinical characteristics of the reinfected and continuously eradicated group are summarized in Table 2. In the EBMT group and MEA group, there was no significant evidence that reinfection of H. pylori was related with gender, the mean age of the patients, clinical diagnosis, atrophic gastritis, and intestinal metaplasia. The H. pylori recrudescence and reinfection rates are shown in Table 3. One patient in the EBMT group and four patients in the MEA group, who were H. pylori positive again at 1 year follow-up, were assigned to recrudescence cases. The rate was calculated at 1.7% (1/60) for the EBMT group and 3.3% (4/120) for the MEA group, and these percentages were not significantly different (p = 0.67). During long-term follow-up 1 year after eradication H. pylori reappeared in 7 (11.9%) of EBMT group and in 19 (16.4%) of MEA group and these percentages were not significantly different depending on each rescue treatment (p = 0.43). Among the reinfected persons no one was belonged to the same household.
Long-term follow-up and reinfection rate
The mean duration of follow-up of 59 patients in the EBMT group and 116 in the MEA group was 31.9 months (range: 18–90 months) and 30.4 months (range: 18–59 months). The mean number of H. pylori tests per patient was found to be 2.05 tests for the EBMT group and 2.31 tests for the MEA group (Table 4). Reinfection with H. pylori occurred in 7 of 59 patients of EBMT group (11.9%) and in 19 of 116 patients of MEA group (16.4%) sporadically during the follow-up period. The calculated total annual reinfection rate was found to be 4.45% (7/157.17 patient years X 100) for EBMT and 6.46% (19/294.08 patient years X 100) for MEA.
Risk factors for reinfection
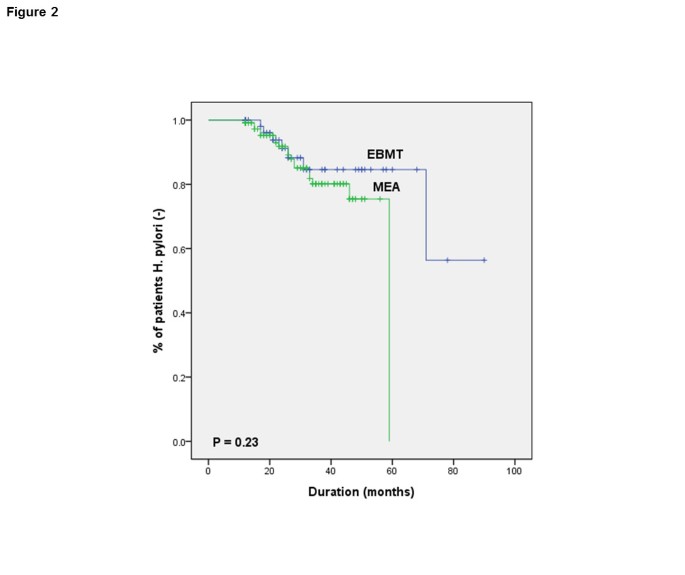
When the reinfected group (n = 26) and continuously eradicated group (n = 149) were compared in terms of demographic information and clinical characteristics, no statistical differences were found by univariate analysis (Log-rank test), in both groups (Table 5). Specially, there was no significant evidence that reinfection of H. pylori is related with eradication regimen (p = 0.23) (Figure 2).
Discussion
We performed a prospective study to investigate reinfection rate of H. pylori in patients who had been successfully treated with second-line therapy after an initial failure to eradicate H. pylori. To the best of our knowledge, this is the first report comparing the reinfection rate of EBMT and MEA therapy.
Reinfection is defined as an infection with a new strain of H. pylori that is different from the original strain after complete eradication, while recrudescence is a relapse of original strain, which was temporarily suppressed by eradication therapy [14, 15]. The recurrence rates of H. pylori decrease with time and decline sharply after the first year, and beyond the first year, recurrence rates come close to the rate of natural acquisition of H. pylori infection in adulthood [14, 16, 17]. From these reports the confirmation of continuous H. pylori negativity for the first year after eradication therapy has been accepted as complete eradication [18–20]. Therefore, in our study, reinfection was defined as the situation where tests for H. pylori infection, after continuous H. pylori negativity for the first year after eradication therapy, become positive again at a later stage. In addition, patients, who become H. pylori positive again during 1 year follow-up were classified as recrudescence cases. We could not perfectly distinguish between recrudescence of an original strain and reinfection because DNA analysis of the strain using molecular fingerprinting techniques was not performed. However, this definition is supported by data obtained using DNA analysis that the cause of H. pylori recurrence after first year is reinfection [14].
In the previous study, we reported that annual reinfection in patients received standard PPI-based triple eradication therapy in Korea was 3.51% and the recrudescence rate 4.9% [11]. This result was similar to the mean annual reinfection rate (3.4%), calculated from the studies performed in developed countries [16]. The increase in antimicrobial resistance with the standard triple therapy has led to an increase of alternative therapy. However, there are few reports regarding the reinfection of H. pylori in patients received second-line therapy. In 2006, our group reported the annual reinfection rate after second-line therapy (EBMT) during 1996–2004, at 6.0% per patients-years in Seoul, Korea [12]. In the present long-term follow-up study for up to 90 months we investigated the reinfection rate of EBMT and MEA therapy, performed during 2003–2010 in Gyeonggi province near Seoul, and those rates are 4.45% for EBMT and 6.46% for MEA per year. When eradication has truly been successful, reinfection is associated with the risk of re-exposure to H. pylori. Relatively low reinfection rates might be related to the decrease in prevalence of H. pylori infection [21] and the recent improvement of sanitation conditions in Korea. In addition, when the reinfection rate of these two kinds of rescue therapy were compared, there was no significant difference (p = 0.43). Therefore, we suggest that reinfection cannot affect the choice of second-line treatment.
In our study, recrudescence rate in the EBMT group and MEA group was found to be 1.7% and 3.3%, which appears slightly lower than reported after initial eradication with standard PPI-based triple regimen (4.9%) [11]. This result might be related to the decreasing trend in eradication rate of standard triple therapy in Korea. That is, the eradication rate of per protocol (PP) analysis decreased up to 75.9% in 2006 [9]. Some studies reported that the recurrence of H. pylori infection more frequently occurred in patients treated with a low efficacy regimen than in those treated with a high efficacy regimen, as a result of recrudescence of the organism after temporary suppression, not elimination [14, 16, 22, 23]. In the previous studies, the PP eradication rates were reported at 77.2% for the 7- and 93.6% for the 14 day EBMT regimen [24], and 83.8% for the 7-, 82.6% for the 10- and 79.9% for the 14 day MEA regimen [25]. Our lower recrudescence rate might be related to the higher efficacy of the EBMT and MEA regimens. In addition, there was no difference in the recrudescence rate between EBMT and MEA regimen (p = 0.67).
Limited information exists regarding risk factors for reinfection of H. pylori. Candidate risk factors include younger age [26, 27], infection of close contacts [14, 28], dental plaque [29, 30], and contaminated endoscopic equipment [14, 16, 31]. Other studies did not identify any factors predictive of H. pylori reinfection [32–34]. In the previous study, we reported that male gender and low income were significantly associated with reinfection of H. pylori by multivariate analysis [11]. However, the current study did not identify any predictive factors concerning H. pylori reinfection in the EBMT group and MEA group.
This study is the first study with large sample size and a long-term follow-up period in the investigation of reinfection rate of H. pylori in patients who had been successfully treated with second-line therapy after an initial failure to eradicate H. pylori. However, our study has limitations. First, recrudescence cases could be included in the reinfection cases. Theoretically the fingerprinting should be performed for the differentiation of reinfected and recrudescence. However, we did not perform DNA analysis to identify the strains. In clinical practice, it is not easy to perform DNA analysis. Secondly, despite our efforts to enroll all patients, many patients dropped out from this study, and refused to receive H. pylori tests every year, especially when there was no gastrointestinal symptom.
Conclusions
In summary, in Korea, the long-term reinfection rate of H. pylori stayed low in both bismuth-containing quadruple therapy and moxifloxacin-based triple therapy; thus reinfection cannot affect the choice of second-line treatment.
References
Go MF: Review article: natural history and epidemiology of Helicobacter pylori infection. Aliment Pharmacol Ther. 2002, 16 (Suppl 1): 3-15.
Chey WD, Wong BC: American College of Gastroenterology guideline on the management of Helicobacter pylori infection. Am J Gastroenterol. 2007, 102: 1808-1825. 10.1111/j.1572-0241.2007.01393.x.
McColl KE: Clinical practice. Helicobacter pylori infection. N Engl J Med. 2010, 362: 1597-1604. 10.1056/NEJMcp1001110.
Malfertheiner P, Megraud F, O'Morain CA, Atherton J, Axon AT, Bazzoli F, Gensini GF, Gisbert JP, Graham DY, Rokkas T, et al: Management of Helicobacter pylori infection–the Maastricht IV/ Florence Consensus Report. Gut. 2012, 61: 646-664. 10.1136/gutjnl-2012-302084.
Fock KM, Katelaris P, Sugano K, Ang TL, Hunt R, Talley NJ, Lam SK, Xiao SD, Tan HJ, Wu CY, et al: Second Asia-Pacific Consensus Guidelines for Helicobacter pylori infection. J Gastroenterol Hepatol. 2009, 24: 1587-1600. 10.1111/j.1440-1746.2009.05982.x.
Asaka M, Kato M, Takahashi S, Fukuda Y, Sugiyama T, Ota H, Uemura N, Murakami K, Satoh K, Sugano K: Guidelines for the management of Helicobacter pylori infection in Japan: 2009 revised edition. Helicobacter. 2010, 15: 1-20.
Kim N, Kim JJ, Choe YH, Kim HS, Kim JI, Chung IS: [Diagnosis and treatment guidelines for Helicobacter pylori infection in Korea]. Korean J Gastroenterol. 2009, 54: 269-278. 10.4166/kjg.2009.54.5.269.
Graham DY, Fischbach L: Helicobacter pylori treatment in the era of increasing antibiotic resistance. Gut. 2010, 59: 1143-1153. 10.1136/gut.2009.192757.
Chung JW, Lee GH, Han JH, Jeong JY, Choi KS, Kim do H, Jung KW, Choi KD, Song HJ, Jung HY, et al: The trends of one-week first-line and second-line eradication therapy for Helicobacter pylori infection in Korea. Hepato-gastroenterology. 2011, 58: 246-250.
Chung WC, Lee KM, Paik CN, Lee JR, Jung SH, Kim JD, Han SW, Chung IS: [Inter-departmental differences in the eradication therapy for Helicobacter pylori infection: a single center study]. Korean J Gastroenterol. 2009, 53: 221-227.
Kim MS, Kim N, Kim SE, Jo HJ, Shin CM, Lee SH, Park YS, Hwang JH, Kim JW, Jeong SH, et al: Long-term Follow-up Helicobacter Pylori Reinfection Rate and Its Associated Factors in Korea. Helicobacter. 2013, 18: 135-142. 10.1111/hel.12018.
Cheon JH, Kim N, Lee DH, Kim JM, Kim JS, Jung HC, Song IS: Long-term outcomes after Helicobacter pylori eradication with second-line, bismuth-containing quadruple therapy in Korea. Eur J Gastroenterol Hepatol. 2006, 18: 515-519. 10.1097/00042737-200605000-00010.
Rugge M, Correa P, Dixon MF, Fiocca R, Hattori T, Lechago J, Leandro G, Price AB, Sipponen P, Solcia E, et al: Gastric mucosal atrophy: interobserver consistency using new criteria for classification and grading. Aliment Pharmacol Ther. 2002, 16: 1249-1259. 10.1046/j.1365-2036.2002.01301.x.
Zhang YY, Xia HH, Zhuang ZH, Zhong J: Review article: 'true' re-infection of Helicobacter pylori after successful eradication–worldwide annual rates, risk factors and clinical implications. Aliment Pharmacol Ther. 2009, 29: 145-160. 10.1111/j.1365-2036.2008.03873.x.
Cameron EA, Bell GD, Baldwin L, Powell KU, Williams SG: Long-term study of re-infection following successful eradication of Helicobacter pylori infection. Aliment Pharmacol Ther. 2006, 23: 1355-1358. 10.1111/j.1365-2036.2006.02899.x.
Gisbert JP: The recurrence of Helicobacter pylori infection: incidence and variables influencing it. A critical review. Am J Gastroenterol. 2005, 100: 2083-2099. 10.1111/j.1572-0241.2005.50043.x.
Peitz U, Hackelsberger A, Malfertheiner P: A practical approach to patients with refractory Helicobacter pylori infection, or who are re-infected after standard therapy. Drugs. 1999, 57: 905-920. 10.2165/00003495-199957060-00006.
Bell GD, Powell KU: Helicobacter pylori reinfection after apparent eradication–the Ipswich experience. Scand J Gastroenterol Suppl. 1996, 215: 96-104.
Hildebrand P, Bardhan P, Rossi L, Parvin S, Rahman A, Arefin MS, Hasan M, Ahmad MM, Glatz-Krieger K, Terracciano L, et al: Recrudescence and reinfection with Helicobacter pylori after eradication therapy in Bangladeshi adults. Gastroenterology. 2001, 121: 792-798. 10.1053/gast.2001.28018.
Soto G, Bautista CT, Roth DE, Gilman RH, Velapatino B, Ogura M, Dailide G, Razuri M, Meza R, Katz U, et al: Helicobacter pylori reinfection is common in Peruvian adults after antibiotic eradication therapy. J infect Dis. 2003, 188: 1263-1275. 10.1086/379046.
Yim JY, Kim N, Choi SH, Kim YS, Cho KR, Kim SS, Seo GS, Kim HU, Baik GH, Sin CS, et al: Seroprevalence of Helicobacter pylori in South Korea. Helicobacter. 2007, 12: 333-340. 10.1111/j.1523-5378.2007.00504.x.
Xia HX, Talley NJ, Keane CT, O'Morain CA: Recurrence of Helicobacter pylori infection after successful eradication: nature and possible causes. Dig Dis Sci. 1997, 42: 1821-1834. 10.1023/A:1018827322470.
Seo M, Okada M, Shirotani T, Nishimura H, Maeda K, Aoyagi K, Sakisaka S: Recurrence of Helicobacter pylori infection and the long-term outcome of peptic ulcer after successful eradication in Japan. J clin Gastroenterol. 2002, 34: 129-134. 10.1097/00004836-200202000-00005.
Lee BH, Kim N, Hwang TJ, Lee SH, Park YS, Hwang JH, Kim JW, Jeong SH, Lee DH, Jung HC, et al: Bismuth-containing quadruple therapy as second-line treatment for Helicobacter pylori infection: effect of treatment duration and antibiotic resistance on the eradication rate in Korea. Helicobacter. 2010, 15: 38-45. 10.1111/j.1523-5378.2009.00735.x.
Yoon H, Kim N, Lee BH, Hwang TJ, Lee DH, Park YS, Nam RH, Jung HC, Song IS: Moxifloxacin-containing triple therapy as second-line treatment for Helicobacter pylori infection: effect of treatment duration and antibiotic resistance on the eradication rate. Helicobacter. 2009, 14: 77-85.
Gomez Rodriguez BJ, Rojas Feria M, Garcia Montes MJ, Romero Castro R, Hergueta Delgado P, Pellicer Bautista FJ, Herrerias Gutierrez JM: Incidence and factors influencing on Helicobacter pylori infection recurrence. Rev Esp Enferm Dig. 2004, 96: 424-627.
Shimizu T, Yarita Y, Kaneko K, Yamashiro Y, Segawa O, Ohkura R, Taneike I, Yamamoto T: Case of intrafamilial Helicobacter pylori reinfection after successful eradication therapy. Pediatr Infect Dis J. 2000, 19: 901-903. 10.1097/00006454-200009000-00024.
Gisbert JP, Arata IG, Boixeda D, Barba M, Canton R, Plaza AG, Pajares JM: Role of partner's infection in reinfection after Helicobacter pylori eradication. Eur J Gastroenterol Hepatol. 2002, 14: 865-871. 10.1097/00042737-200208000-00009.
Karczewska E, Konturek JE, Konturek PC, Czesnikiewicz M, Sito E, Bielanski W, Kwiecien N, Obtulowicz W, Ziemniak W, Majka J, et al: Oral cavity as a potential source of gastric reinfection by Helicobacter pylori. Dig Dis Sci. 2002, 47: 978-986. 10.1023/A:1015017502772.
Kilmartin CM: Dental implications of Helicobacter pylori. J Can Dent Assoc. 2002, 68: 489-493.
Sugiyama T, Naka H, Yachi A, Asaka M: Direct evidence by DNA fingerprinting that endoscopic cross-infection of Helicobacter pylori is a cause of postendoscopic acute gastritis. J Clin Microbiol. 2000, 38: 2381-2382.
Feydt-Schmidt A, Kindermann A, Konstantopoulos N, Demmelmair H, Ballauff A, Findeisen A, Koletzko S: Reinfection rate in children after successful Helicobacter pylori eradication. Eur J Gastroenterol Hepatol. 2002, 14: 1119-1123. 10.1097/00042737-200210000-00013.
Leal-Herrera Y, Torres J, Monath TP, Ramos I, Gomez A, Madrazo-de la Garza A, Dehesa-Violante M, Munoz O: High rates of recurrence and of transient reinfections of Helicobacter pylori in a population with high prevalence of infection. Am J Gastroenterol. 2003, 98: 2395-2402. 10.1111/j.1572-0241.2003.07708.x.
Thong-Ngam D, Mahachai V, Kullavanijaya P: Incidence of Helicobacter pylori recurrent infection and associated factors in Thailand. J Med Associ Thai. 2007, 90: 1406-1410.
Pre-publication history
The pre-publication history for this paper can be accessed here:http://0-www-biomedcentral-com.brum.beds.ac.uk/1471-230X/13/138/prepub
Acknowledgments
This work was supported by a grant from the National Research Foundation of Korea funded by the Korean Government (2012R1A1A3A04002680) and partly supported by the Seoul National University Budang Hospital Research fund (grants no 02-2010-014). MRCC of Seoul National University Hospital was consulted about the statistical analysis of the present manuscript.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors have no competing of interests to declare.
Authors’ contributions
KN- designed the study and performed the major role of collecting patients; KMS- collected patients’ data and wrote the manuscript; KSE- collected patients’ data and was involved in editing the manuscript; JHJ- collected patients’ data and were involved in editing the manuscript; SCM- collected patients’ data and were involved in editing the manuscript; PYS- collected patients’ data and were involved in editing the manuscript; LDH- collected patients’ data and was involved in editing the manuscript. All authors read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Kim, M.S., Kim, N., Kim, S.E. et al. Long-term follow up Helicobacter Pylori reinfection rate after second-line treatment: bismuth-containing quadruple therapy versus moxifloxacin-based triple therapy. BMC Gastroenterol 13, 138 (2013). https://0-doi-org.brum.beds.ac.uk/10.1186/1471-230X-13-138
Received:
Accepted:
Published:
DOI: https://0-doi-org.brum.beds.ac.uk/10.1186/1471-230X-13-138