- Research article
- Open access
- Published:
Priorities and challenges for health leadership and workforce management globally: a rapid review
BMC Health Services Research volume 19, Article number: 239 (2019)
Abstract
Background
Health systems are complex and continually changing across a variety of contexts and health service levels. The capacities needed by health managers and leaders to respond to current and emerging issues are not yet well understood. Studies to date have been country-specific and have not integrated different international and multi-level insights. This review examines the current and emerging challenges for health leadership and workforce management in diverse contexts and health systems at three structural levels, from the overarching macro (international, national) context to the meso context of organisations through to the micro context of individual healthcare managers.
Methods
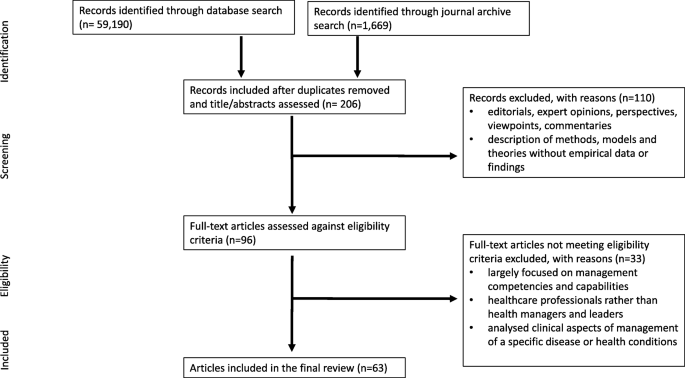
A rapid review of evidence was undertaken using a systematic search of a selected segment of the diverse literature related to health leadership and management. A range of text words, synonyms and subject headings were developed for the major concepts of global health, health service management and health leadership. An explorative review of three electronic databases (MEDLINE®, Pubmed and Scopus) was undertaken to identify the key publication outlets for relevant content between January 2010 to July 2018. A search strategy was then applied to the key journals identified, in addition to hand searching the journals and reference list of relevant papers identified. Inclusion criteria were independently applied to potentially relevant articles by three reviewers. Data were subject to a narrative synthesis to highlight key concepts identified.
Results
Sixty-three articles were included. A set of consistent challenges and emerging trends within healthcare sectors internationally for health leadership and management were represented at the three structural levels. At the macro level these included societal, demographic, historical and cultural factors; at the meso level, human resource management challenges, changing structures and performance measures and intensified management; and at the micro level shifting roles and expectations in the workplace for health care managers.
Conclusion
Contemporary challenges and emerging needs of the global health management workforce orient around efficiency-saving, change and human resource management. The role of health managers is evolving and expanding to meet these new priorities. Ensuring contemporary health leaders and managers have the capabilities to respond to the current landscape is critical.
Background
Health systems are increasingly complex; encompassing the provision of public and private health services, primary healthcare, acute, chronic and aged care, in a variety of contexts. Health systems are continually evolving to adapt to epidemiological, demographic and societal shifts. Emerging technologies and political, economic, social, and environmental realities create a complex agenda for global health [1]. In response, there has been increased recognition of the role of non-state actors to manage population needs and drive innovation. The concept of ‘collaborative governance,’ in which non-health actors and health actors work together, has come to underpin health systems and service delivery internationally [1] in order to meet changing expectations and new priorities. Seeking the achievement of universal health coverage (UHC) and the Sustainable Development Goals (SDGs), particularly in low- and middle-income countries, have been pivotal driving forces [2]. Agendas for change have been encapsulated in reforms intended to improve the efficiency, equity of access, and the quality of public services more broadly [1, 3].
The profound shortage of human resources for health to address current and emerging population health needs across the globe was identified in the World Health Organization (WHO) landmark publication ‘Working together for health’ and continues to impede progress towards the SDGs [4]. Despite some improvements overall in health workforce aggregates globally, the human resources for health challenges confronting health systems are highly complex and varied. These include not only numerical workforce shortages but imbalances in skill mix, geographical maldistribution, difficulty in inter-professional collaboration, inefficient use of resources, and burnout [2, 5, 6]. Effective health leadership and workforce management is therefore critical to addressing the needs of human resources within health systems and strengthening capacities at regional and global levels [4, 6,7,8].
While there is no standard definition, health leadership is centred on the ability to identify priorities, provide strategic direction to multiple actors within the health system, and create commitment across the health sector to address those priorities for improved health services [7, 8]. Effective management is required to facilitate change and achieve results through ensuring the efficient mobilisation and utilisation of the health workforce and other resources [8]. As contemporary health systems operate through networks within which are ranging levels of responsibilities, they require cooperation and coordination through effective health leadership and workforce management to provide high quality care that is effective, efficient, accessible, patient-centred, equitable, and safe [9]. In this regard, health leadership and workforce management are interlinked and play critical roles in health services management [7, 8].
Along with health systems, the role of leaders and managers in health is evolving. Strategic management that is responsive to political, technological, societal and economic change is essential for health system strengthening [10]. Despite the pivotal role of health service management in the health sector, the priorities for health service management in the global health context are not well understood. This rapid review was conducted to identify the current challenges and priorities for health leadership and workforce management globally.
Methods
This review utilised a rapid evidence assessment (REA) methodology structured using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) checklist [11]. An REA uses the same methods and principles as a systematic review but makes concessions to the breadth or depth of the process to address key issues about the topic under investigation [12,13,14]. An REA provides a balanced assessment of what is already known about an issue, and the strength of evidence. The narrower research focus, relative to full systematic reviews, make REAs helpful for systematically exploring the evidence around a particular issue when there is a broad evidence base to explore [14]. In the present review, the search was limited to contemporary literature (post 2010) selected from leading health service management and global health journals identified from exploring major electronic databases.
Search strategy
Phase 1
An explorative review of three core databases in the area of public health and health services (MEDLINE®, Pubmed and Scopus) was undertaken to identify the key publication outlets for relevant content. These databases were selected as those that would be most relevant to the focus of the review and have the broadest range of relevant content. A range of text words, synonyms and subject headings were developed for the major constructs: global health, health service management and health leadership, priorities and challenges. Regarding health service management and health leadership, the following search terms were used: “healthcare manag*” OR “health manag*” OR “health services manag*” OR “health leader*”. Due to the large volume of diverse literature generated, a systematic search was then undertaken on the key journals that produced the largest number of relevant articles. The journals were selected as those identified as likely to contain highly relevant material based on an initial scoping of the literature.
Phase 2
Based on the initial database search, a systematic search for articles published in English between 1 January 2010 and 31 July 2018 was undertaken of the current issues and archives of the following journals: Asia-Pacific Journal of Health Management; BMC Health Services Research; Healthcare Management Review; International Journal of Healthcare Management; International Journal of Health Planning and Management; Journal of Healthcare Management; Journal of Health Organisation and Management; and, Journal of Health Management. Hand-searching of reference lists of identified papers were also used to ensure that major relevant material was captured.
Study selection and data extraction
Results were merged using reference-management software (Endnote) and any duplicates removed. The first author (CF) screened the titles and abstracts of articles meeting the eligibility criteria (Table 1). Full-text publications were requested for those identified as potentially relevant. The inclusion and exclusion criteria were then independently applied by two authors. Disagreements were resolved by consensus or consultation with a third person, and the following data were extracted from each publication: author(s), publication year, location, primary focus and main findings in relation to the research objective. Sixty-three articles were included in the final review. The selection process followed the PRISMA checklist [11] as shown in Fig. 1.
Data extraction and analysis
A narrative synthesis was used to explore the literature against the review objective. A narrative synthesis refers to “an approach to the systematic review and synthesis of findings from multiple studies that relies primarily on the use of words and text to summarise and explain the findings of the synthesis” [15]. Firstly, an initial description of the key findings of included studies was drafted. Findings were then organised, mapped and synthesised to explore patterns in the data.
Results
Search results
A total of 63 articles were included; Table 2 summarizes the data extraction results by region and country. Nineteen were undertaken in Europe, 16 in North America, and one in Australia, with relatively fewer studies from Asia, the Middle East, and small island developing countries. Eighteen qualitative studies that used interviews and/or focus group studies [16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32] were identified. Other studies were quantitative [33,34,35,36,37,38,39] including the use of questionnaires or survey data, or used a mixed-method approach [40,41,42,43,44]. Other articles combined different types of primary and secondary data (key informant interviews, observations, focus groups, questionnaire/survey data, and government reports). The included literature also comprised 28 review articles of various types that used mixed data and bibliographic evidence.
Key challenges and emerging trends
A set of challenges and emerging trends were identified across healthcare sectors internationally. These were grouped at three levels: 1) macro, system context (society, demography, technology, political economy, legal framework, history, culture), 2) meso, organisational context (infrastructure, resources, governance, clinical processes, management processes, suppliers, patients), and 3) micro context related to the individual healthcare manager (Table 3). This multi-levelled approach has been used in previous research to demonstrate the interplay between different factors across different levels, and their direct and indirect reciprocal influences on healthcare management policies and practices [45].
Societal and system-wide (macro)
Population growth, ageing populations, and increased disease burdens are some of the common trends health systems are facing globally. Developing and developed countries are going through demographic and epidemiological transitions; people are living longer with increasing prevalence of chronic diseases requiring health managers and leaders to adjust to shifting healthcare needs at the population level, delivering preventative and long-term care beyond acute care. Countries in Africa, Europe, the Pacific Islands, Middle East, Asia and Caribbean are seeing an increase in number of patients with non-communicable diseases and communicable diseases [21, 46,47,48,49,50,51,52].
Although many countries have similar emerging health system concerns, there are some differences in the complexities each country faces. For many small countries, outmigration, capacity building and funding from international aid agencies are affecting how their health systems operate, while in many larger countries, funding cuts, rise in private health insurance, innovations, and health system restructuring are major influences [21, 34, 50, 53, 54]. In addition, patients are increasingly health literate and, as consumers, expect high-quality healthcare [34, 53, 54]. However, hospitals and healthcare systems are lacking capacity to meet the increased demand [16, 34, 43].
Scientific advances have meant more patients are receiving care across the health system. It is imperative to have processes for communication and collaboration between different health professionals for high-quality care. However, health systems are fragmented; increasing specialisation is leading to further fragmentation and disassociation [31, 54, 55]. Adoption of technological innovations also require change management, hospital restructure, and capacity building [56,57,58].
Changes in health policies and regulations compound the challenge faced by healthcare managers and leaders to deliver high quality care [53, 54, 59]. Political reforms often lead to health system restructuring requiring change in the values, structures, processes and systems that can constrain how health managers and leaders align their organisations to new agendas [24, 28, 31, 60]. For example, the distribution of health services management to local authorities through decentralisation has a variable impact on the efficacy and efficiency of healthcare delivery [24, 27, 35, 59].
Governments’ decisions are often made focusing on cost savings, resulting in budgetary constraints within which health systems must operate [16, 19, 53, 61]. Although some health systems have delivered positive results under such constraint [53], often financial resource constraints can lead to poor human and technical resource allocation, creating a disconnect between demand and supply [23, 27, 40, 47, 57]. To reduce spending in acute care, there is also a push to deliver health services in the community and focus on social determinants of health, though this brings further complexities related to managing multiple stakeholder collaborations [27, 32, 34, 38, 40, 49, 55].
Due to an increase in demand and cost constraints, new business models are emerging, and some health systems are resorting to privatisation and corporatisation [22, 48, 62]. This has created competition in the market, increased uptake of private health insurance and increased movement of consumers between various organisations [22, 48]. Health managers and leaders need to keep abreast with continuously changing business models of care delivery and assess their impact [59, 62]. The evolving international health workforce, insufficient numbers of trained health personnel, and maintaining and improving appropriate skill mixes comprise other important challenges for managers in meeting population health needs and demands (Table 3).
Organisational level (meso)
At the organisation level, human resource management issues were a central concern. This can be understood in part within the wider global human resources for health crisis which has placed healthcare organisations under intense pressure to perform. The evidence suggests healthcare organisations are evolving to strengthen coordination between primary and secondary care; there is greater attention to population-based perspectives in disease prevention, interdisciplinary collaboration, and clinical governance. These trends are challenged by the persistence of bureaucratic and hierarchical cultures, emphasis on targets over care quality, and the intensification of front-line and middle-management work that is limiting capacity.
Healthcare managers and leaders also face operational inefficiencies in providing primary health and referral services to address highly complex and shifting needs which often result in the waste of resources [49, 63, 64]. Considering the pace of change, organisations are required to be flexible and deliver higher quality care at lower cost [21, 53, 65]. To achieve this, many organisations in developing and developed countries alike are adopting a lean model [17, 21]. However, there are challenges associated with ensuring sustainability of the lean system, adjusting organisational hierarchies, and improving knowledge of the lean model, especially in developing countries [17, 21].
Healthcare organisations require various actors with different capabilities to deliver high quality care. However, a dominant hierarchical culture and lack of collaborative and distributed culture can limit the performance of healthcare organisations [22, 36, 54]. In addition, considering high turnover of executive leadership, healthcare organisations often rely on external talent for succession management which can reduce hospital efficiency [44, 66]. Other contributors to weakened hospital performance include: the lack of allocative efficiency and transparency [24, 30, 64, 67]; poor hospital processes that hamper the development of effective systems for the prevention and control of hospital acquired infections (HAIs) [53, 68]; and, payment reforms such as value-based funding and fee-for-service that encourage volume [18, 23, 24, 61, 62, 69, 70].
Managerial work distribution within organisations is often not clearly defined, leading to extra or extreme work conditions for middle and front-line managers [29, 42, 53, 70]. Unregulated and undefined expectations at the organisation level leads to negative effects such as stress, reduced productivity, and unpredictable work hours, and long-term effects on organisational efficiency and delivery of high quality care [22, 28, 29, 37, 42, 51, 71]. Furthermore, often times front-line clinicians are also required to take the leadership role in the absence of managers without proper training [20]. Despite this, included studies indicate that the involvement of middle and front-line managers in strategic decision-making can be limited due to various reasons including lack of support from the organisation itself and misalignment of individual and organisational goals [16, 26, 31, 72].
Individual level (micro)
Worldwide, middle and front-line health managers and leaders are disproportionately affected by challenges at the system and organisational level, which has contributed to increasing and often conflicting responsibilities. Some countries are experiencing a growth in senior health managers with a clinical background, while in other countries, the converse is apparent. Indistinct organisational boundaries, increasing scope of practice, and lack of systemic support at policy level are leaving healthcare managers with undefined roles [28, 59]. Poorly defined roles contribute to reduced accountability, transparency, autonomy, and understanding of responsibilities [24, 30, 31, 67]. Studies also indicate a lack of recognition of clinical leaders in health organisations and inadequate training opportunities for them as such [20, 67].
The number of hybrid managers (performing clinical and managerial work concurrently) in developed countries is increasing, with the perception that such managers improve the clinical governance of an organization. In contrast, the number of non-clinical managers in many developing countries appears to be increasing [63, 73,74,75]. Included studies suggest this approach does not necessarily improve manager-clinical professional relationships or the willingness of clinicians becoming managers, limiting their participation in strategic decisions [28, 70, 71, 74].
Discussion
This rapid review highlights the current global climate in health service management, the key priority areas, and current health management approaches being utilised to address these. The multitude of issues emerging demonstrate the complex and evolving role of health service management in the wider complex functioning of health systems globally in a changing healthcare landscape. Key themes of achieving high quality care and sustainable service delivery were apparent, often evidenced through health reforms [5]. The influence of technological innovation in both its opportunities and complexities is evident worldwide. In the context of changing healthcare goals and delivery approaches, health management is seeking to professionalise as a strategy to build strength and capacity. In doing so, health managers are questioning role scope and the skills and knowledge they need to meet the requirements of the role.
Global challenges facing health management
Understanding how the features of the macro, meso and micro systems can create challenges for managers is critical [19]. With continual healthcare reform and increasing health expenditure as a proportion of GDP, distinct challenges are facing high-income Organisation for Economic Co-operation and Development (OECD) countries, middle-income rapidly-developing economies, and low-income, resource-limited countries. Reforms, especially in OECD countries, have been aimed at controlling costs, consolidating hospitals for greater efficiencies, and reconfiguring primary healthcare [1, 76]. The changing business models for the delivery of care have wider implications for the way in which health managers conceptualise healthcare delivery and the key stakeholders [59], for example, the emerging role of private healthcare providers and non-health actors in public health. Changes to the business model of healthcare delivery also has implications for the distribution of power amongst key actors within the system. This is evident in the evolved role of general practitioners (GPs) in the UK National Health Service as leaders of Clinical Commissioning Groups (CCGs). Commissioning requires a different skill set to clinical work, in terms of assessing financial data, the nature of statutory responsibilities, and the need to engage with a wider stakeholder group across a region to plan services [77]. With new responsibilities, GPs have been required to quickly equip themselves with new management capabilities, reflecting the range of studies included in this review around clinician managers and the associated challenges [18, 28, 53, 63, 70, 71, 74, 75].
Central to the role of healthcare managers is the ability to transition between existing and new cultures and practices within healthcare delivery [59]. Bridging this space is particularly important in the context of increasingly personalized and technologically-driven healthcare delivery [54]. While advances in knowledge and medical technologies have increased capability to tackle complex health needs, the integration of innovations into existing healthcare management practices requires strong change management [73]. Health leaders and managers need to be able to rapidly and continually assess the changes required or upon them, the implications, and to transform their analysis into a workable plan to realise change [10]. Focusing only on the clinical training of health professionals rather than incorporating managerial and leadership roles, and specifically, change management capability may limit the speed and success of innovation uptake [22].
Implications
Our findings highlight the implications of current priorities within the health sector for health management practice internationally; key issues are efficiency savings, change management and human resource management. In the context of efficiency approaches, health system and service managers are facing instances of poor human and technical resource allocation, creating a disconnect between demand and supply. At the service delivery level, this has intensified and varied the role of middle managers mediating at two main levels. The first level of middle-management is positioned between the front-line and C-suite management of an organisation. The second level of middle-management being the C-suite managers who translate regional and/or national funding decisions and policies into their organisations. Faced with increasing pace of change, and economic and resource constraints, middle managers across both levels are now more than ever exposed to high levels of stress, low morale, and unsustainable working patterns [29]. Emphasis on cost-saving has brought with it increased attention to the health services that can be delivered in the community and the social determinants of health. Connecting disparate services in order to meet efficiency goals is a now a core feature of the work of many health managers mediating this process.
Our findings also have implications for the conceptualisation of healthcare management as a profession. The scale and increasing breadth of the role of health leaders and managers is evident in the review. Clarifying the professional identity of ‘health manager’ may therefore be a critical part of building and maintaining a robust health management workforce that can fulfil these diverse roles [59]. Increasing migration of the healthcare workforce and of population, products and services between countries also brings new challenges for healthcare. In response, the notion of transnational competence among healthcare professionals has been identified [78]. Transnational competence progresses cultural competence by considering the interpersonal skills required for engaging with those from diverse cultural and social backgrounds. Thus, transnational competence may be important for health managers working across national borders. A key aspect of professionalisation is the education and training of health managers. Our findings provide a unique and useful theoretical contribution that is globally-focused and multi-level to stimulate new thinking in health management educators, and for current health leaders and managers. These findings have considerable practical utility for managers and practitioners designing graduate health management programs.
Limitations
Most of the studies in the field have focused on the Anglo-American context and health systems. Notwithstanding the importance of lessons drawn from these health systems, further research is needed in other regions, and in low- and middle-income countries in particular [79]. We acknowledge the nuanced interplay between evidence, culture, organisational factors, stakeholder interests, and population health outcomes. Terminologies and definitions to express global health, management and leadership vary across countries and cultures, creating potential for bias in the interpretation of findings. We also recognise that there is fluidity in the categorisations, and challenges arising may span multiple domains. This review considers challenges facing all types of healthcare managers and thus lacks discrete analysis of senior, middle and front-line managers. That said, managers at different levels can learn from one another. Senior managers and executives may gain an appreciation for the operational challenges that middle and front-line managers may face. Middle and front-line managers may have a heightened awareness of the more strategic decision-making of senior health managers. Whilst the findings indicate consistent challenges and needs for health managers across a range of international contexts, the study does not capture country-specific issues which may have consequences at the local level. Whilst a systematic approach was taken to the literature in undertaking this review, relevant material may have been omitted due to the limits placed on the rapid review of the vast and diverse health management literature. The inclusion of only materials in English language may have led to further omissions of relevant work.
Conclusion
Health managers within both international and national settings face complex challenges given the shortage of human resources for health worldwide and the rapid evolution of national and transnational healthcare systems. This review addresses the lack of studies taking a global perspective of the challenges and emerging needs at macro (international, national and societal), meso (organisational), and micro (individual health manager) levels. Contemporary challenges of the global health management workforce orient around demographic and epidemiological change, efficiency-saving, human resource management, changing structures, intensified management, and shifting roles and expectations. In recognising these challenges, researchers, management educators, and policy makers can establish global health service management priorities and enhance health leadership and capacities to meet these. Health managers and leaders with adaptable and relevant capabilities are critical to high quality systems of healthcare delivery.
Abbreviations
- CCGs:
-
Clinical Commissioning Groups
- GPs:
-
General practitioners
- HAIs:
-
Hospital acquired infections
- OECD:
-
Organisation for Economic Co-operation and Development
- PRISMA:
-
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- REA:
-
Rapid evidence assessment
- SDGs:
-
Sustainable Development Goals
- UHC:
-
Universal health coverage
- WHO:
-
World Health Organization
References
Senkubuge F, Modisenyane M, Bishaw T. Strengthening health systems by health sector reforms. Glob Health Action. 2014;7(1):23568.
World Health Organization, Global Health Workforce Alliance. Human resources for health: foundation for universal health coverage and the post-2015 development agenda. Report of the Third Global Forum on Human Resources for Health, 2013 November 10–13. Recife, Brazil: WHO; 2014.
Reich MR, Harris J, Ikegami N, Maeda A, Cashin C, Araujo EC, et al. Moving towards universal health coverage: lessons from 11 country studies. Lancet. 2016;387(10020):811–6.
World Health Organisation. Working together for health: the world health report 2006: policy briefs. Geneva: World Health Organisation; 2006.
West M, Dawson J. Employee engagement and NHS performance. London: King's Fund; 2012.
World Health Organization. Global strategy on human resources for health: workforce 2030. Geneva: World Health Organisation; 2016.
Reich MR, Javadi D, Ghaffar A. Introduction to the special issue on “effective leadership for health systems”. Health Syst Reform. 2016;2(3):171–5.
Waddington C, Egger D, Travis P, Hawken L, Dovlo D, World Health Organization. Towards better leadership and management in health: report of an international consultation on strengthening leadership and management in low-income countries, 29 January-1 February. Ghana: Accra; 2007.
World Health Organization. Quality of care: a process for making strategic choices in health systems. Manila: WHO Regional Office for the Western Pacific; 2006.
Ginter PM, Duncan WJ, Swayne LE. The strategic management of health care organizations: John Wiley & Sons; 2018.
Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Int Med. 2009;151(4):264–9.
Grant MJ, Booth A. A typology of reviews: an analysis of 14 review types and associated methodologies. Health Inf Libr J. 2009;26(2):91–108.
Varker T, Forbes D, Dell L, Weston A, Merlin T, Hodson S, et al. Rapid evidence assessment: increasing the transparency of an emerging methodology. J Eval Clin Pract. 2015;21(6):1199–204.
Tricco AC, Langlois EV, Straus SE. Rapid reviews to strengthen health policy and systems: a practical guide. Geneva, Switzerland: World Health Organization; 2017.
Popay J, Roberts H, Sowden A, Petticrew M, Arai L, Rodgers M, et al. Guidance on the conduct of narrative synthesis in systematic reviews. A product from the ESRC methods programme Version. 2006;1:b92.
Taylor A, Groene O. European hospital managers’ perceptions of patient-centred care: a qualitative study on implementation and context. J Health Organ Manag. 2015;29(6):711–28.
Costa LBM, Rentes AF, Bertani TM, Mardegan R. Lean healthcare in developing countries: evidence from Brazilian hospitals. Int J Health Plann Manage. 2017;32(1).
Chreim S, Williams BE, Coller KE. Radical change in healthcare organization: mapping transition between templates, enabling factors, and implementation processes. J Health Organ Manag. 2012;26(2):215–36.
Greenwald HP. Management challenges in British Columbia’s healthcare system. J Health Organ Manag. 2017;31(4):418–29.
Mercer D, Haddon A, Loughlin C. Leading on the edge: the nature of paramedic leadership at the front line of care. Health Care Manag Rev. 2018;43(1):12–20.
Reijula J, Reijula E, Reijula K. Healthcare management challenges in two university hospitals. Int J Healthc Tech Manag. 2016;15(4):308–25.
Srinivasan V, Chandwani R. HRM innovations in rapid growth contexts: the healthcare sector in India. Int J Hum Res Manage. 2014;25(10):1505–25.
Afzali HHA, Moss JR, Mahmood MA. Exploring health professionals' perspectives on factors affecting Iranian hospital efficiency and suggestions for improvement. Int J Health Plann Manag. 2011;26(1):e17–29.
Jafari M, Rashidian A, Abolhasani F, Mohammad K, Yazdani S, Parkerton P, et al. Space or no space for managing public hospitals; a qualitative study of hospital autonomy in Iran. Int J Health Plann Manag. 2011;26(3):e121–e37.
Lapão LV, Dussault G. From policy to reality: clinical managers' views of the organizational challenges of primary care reform in Portugal. Int J Health Plann Manag. 2012;27(4):295–307.
Andreasson J, Eriksson A, Dellve L. Health care managers' views on and approaches to implementing models for improving care processes. J Nurs Manag. 2016;24(2):219–27.
Maluka SO, Hurtig AK, Sebastián MS, Shayo E, Byskov J, Kamuzora P. Decentralization and health care prioritization process in Tanzania: from national rhetoric to local reality. Int J Health Plann Manag. 2011;26(2):e102–e20.
Taytiwat P, Briggs D, Fraser J, Minichiello V, Cruickshank M. Lessons from understanding the role of community hospital director in Thailand: clinician versus manager. Int J Health Plann Manag. 2011;26(2):e48–67.
Buchanan DA, Parry E, Gascoigne C, Moore C. Are healthcare middle management jobs extreme jobs? J Health Organ Manag. 2013;27(5):646–64.
Longenecker CO, Longenecker PD. Why hospital improvement efforts fail: a view from the front line. J Healthc Manag. 2014;59(2):147–57.
Reyes DJ, Bekemeier B, Issel LM. Challenges faced by public health Nurs leaders in Hyperturbulent times. Public Health Nurs. 2014;31(4):344–53.
Louis CJ, Clark JR, Gray B, Brannon D, Parker V. Service line structure and decision-maker attention in three health systems: implications for patient-centered care. Health Care Manag Rev. 2017. https://0-doi-org.brum.beds.ac.uk/10.1097/HMR.0000000000000172.
Oppel EM, Winter V, Schreyogg J. Evaluating the link between human resource management decisions and patient satisfaction with quality of care. Health Care Manag Rev. 2017;42(1):53–64.
Ramanujam P. Service quality in health care organisations: a study of corporate hospitals in Hyderabad. J Health Manag. 2011;13(2):177–202.
Diana A, Hollingworth SA, Marks GC. Effects of decentralisation and health system reform on health workforce and quality-of-care in Indonesia, 1993–2007. Int J Health Plann Manag. 2015;30(1):e16–30.
Prenestini A, Lega F. Do senior management cultures affect performance? Evidence from Italian public healthcare organizations. J Healthc Manag. 2013;58(5):336–51.
Giauque D. Stress among public middle managers dealing with reforms. J Health Organ Manag. 2016;30(8):1259–83.
Jennings JC, Landry AY, Hearld LR, Weech-Maldonado R, Snyder SW, Patrician PA. Organizational and environmental factors influencing hospital community orientation. Health Care Manag Rev. 2017. https://0-doi-org.brum.beds.ac.uk/10.1097/HMR.0000000000000180.
Tasi MC, Keswani A, Bozic KJ. Does physician leadership affect hospital quality, operational efficiency, and financial performance? Health Care Manag Rev. 2017. https://0-doi-org.brum.beds.ac.uk/10.1097/HMR.0000000000000173.
Hall W, Williams I, Smith N, Gold M, Coast J, Kapiriri L, et al. Past, present and future challenges in health care priority setting: findings from an international expert survey. J Health Organ Manag. 2018;32(3):444–62.
Nelson SA, Azevedo PR, Dias RS, de Sousa SdMA, de Carvalho LDP, Silva ACO, et al. nursing work: challenges for health management in the northeast of Brazil. J Nurs Manag 2013;21(6):838–849.
Ireri S, Walshe K, Benson L, Mwanthi MA. A qualitative and quantitative study of medical leadership and management: experiences, competencies, and development needs of doctor managers in the United Kingdom. J Manag Marketing Healthc. 2011;4(1):16–29.
Powell M. The snakes and ladders of National Health Service management in England. Int J Health Plann Manag. 2014;29(3):260–79.
Groves KS. Examining the impact of succession management practices on organizational performance: A national study of U.S. hospitals. Health Care Manage Rev. 2017; doi: https://0-doi-org.brum.beds.ac.uk/10.1097/hmr.0000000000000176.
Syed J, Özbilgin M. A relational framework for international transfer of diversity management practices. Int J Hum Res Manage. 2009;20(12):2435–53.
Adindu A. The need for effective management in African health systems. J Health Manag. 2013;15(1):1–13.
Greaves DE. Health management/leadership of Small Island developing states of the English-speaking Caribbean: a critical review. J Health Manag. 2016;18(4):595–610.
Khan MI, Banerji A. Health Care Management in India: some issues and challenges. J Health Manag. 2014;16(1):133–47.
Moghadam MN, Sadeghi V, Parva S. Weaknesses and challenges of primary healthcare system in Iran: a review. Int J Health Plann Manag. 2012;27(2):e121–e31.
Taylor R. The tyranny of size: challenges of health administration in Pacific Island states. Asia Pac J Health Manag. 2016;11(3):65.
Jooste K, Jasper M. A south African perspective: current position and challenges in health care service management and education in nursing. J Nurs Manag. 2012;20(1):56–64.
Sen K, Al-Faisal W. Reforms and emerging noncommunicable disease: some challenges facing a conflict-ridden country—the case of the Syrian Arab Republic. Int J Health Plann Manag. 2013;28(3):290–302.
Carney M. Challenges in healthcare delivery in an economic downturn, in the Republic of Ireland. J Nurs Manag. 2010;18(5):509–14.
Bowden DE, Smits SJ. Managing in the context of healthcare's escalating technology and evolving culture. J Health Organ Manag. 2012;26(2):149–57.
Meijboom BR, Bakx SJWGC, Westert GP. Continuity in health care: lessons from supply chain management. Int J Health Plann Manag. 2010;25(4):304–17.
Lega F, Calciolari S. Coevolution of patients and hospitals: how changing epidemiology and technological advances create challenges and drive organizational innovation. J Healthc Manag. 2012;57(1):17–34.
Kim Y, Kang M. The performance management system of the Korean healthcare sector: development, challenges, and future tasks. Public Perform Manag. 2016;39(2):297–315.
Hernandez SE, Conrad DA, Marcus-Smith MS, Reed P, Watts C. Patient-centered innovation in health care organizations: a conceptual framework and case study application. Health Care Manag Rev. 2013;38(2):166–75.
Briggs D, Isouard G. The language of health reform and health management: critical issues in the management of health systems. Asia Pac J Health Manag. 2016;11(3):38.
Zuckerman AM. Successful strategic planning for a reformed delivery system. J Healthc Manag. 2014;59(3):168–72.
Gantz NR, Sherman R, Jasper M, Choo CG, Herrin-Griffith D, Harris K. Global nurse leader perspectives on health systems and workforce challenges. J Nurs Manag. 2012;20(4):433–43.
Jeurissen P, Duran A, Saltman RB. Uncomfortable realities: the challenge of creating real change in Europe’s consolidating hospital sector. BMC Health Serv Res. 2016;16(2):168.
Kirkpatrick I, Kuhlmann E, Hartley K, Dent M, Lega F. Medicine and management in European hospitals: a comparative overview. BMC Health Serv Res. 2016;16(2):171.
Akbulut Y, Esatoglu AE, Yildirim T. Managerial roles of physicians in the Turkish healthcare system: current situation and future challenges. J Health Manag. 2010;12(4):539–51.
Naranjo-Gil D. The role of top management teams in hospitals facing strategic change: effects on performance. Int J Healthc Manag. 2015;8(1):34–41.
Ford EW, Lowe KB, Silvera GB, Babik D, Huerta TR. Insider versus outsider executive succession: the relationship to hospital efficiency. Health Care Manag Rev. 2018;43(1):61–8.
Leggat SG, Balding C. Achieving organisational competence for clinical leadership: the role of high performance work systems. J Health Organ Manag. 2013;27(3):312–29.
Baylina P, Moreira P. Healthcare-associated infections – on developing effective control systems under a renewed healthcare management debate. Int J Healthc Manag. 2012;5(2):74–84.
Jha R, Sahay B, Charan P. Healthcare operations management: a structured literature review. Decis. 2016;43(3):259–79.
Kuhlmann E, Rangnitt Y, von Knorring M. Medicine and management: looking inside the box of changing hospital governance. BMC Health Serv Res. 2016;16(2):159.
Spehar I, Frich JC, Kjekshus LE. Clinicians’ experiences of becoming a clinical manager: a qualitative study. BMC Health Serv Res. 2012;12(1):421.
Rodriguez CA. Challenges to effectiveness in public health organizations: the case of the Costa Rican health ministry. J Bus Res. 2016;69(9):3859–68.
Cinaroglu S. Complexity in healthcare management: why does Drucker describe healthcare organizations as a double-headed monster? Int J Healthc Manag. 2016;9(1):11–7.
Rotar A, Botje D, Klazinga N, Lombarts K, Groene O, Sunol R, et al. The involvement of medical doctors in hospital governance and implications for quality management: a quick scan in 19 and an in depth study in 7 OECD countries. BMC Health Serv Res. 2016;16(2):160.
Edmonstone JD. Whither the elephant?: the continuing development of clinical leadership in the UK National Health Services. Int J Health Plann Manag. 2014;29(3):280–91.
Naylor C, Ross S, Curry N, Holder H, Marshall L, Tait E. Clinical commissioning groups: supporting improvement in general practice? London: The King's Fund; 2013.
Holder H, Robertson R, Ross S, Bennett L, Gosling J, Curry N. Risk or reward? The changing role of CCGs in general practice. London: Kings Fund/Nuffield Trust; 2015.
Koehn PH, Rosenau JN. Transnational competence in an emergent epoch. Int Stud Perspect. 2002;3(2):105–27.
Antunes V, Moreira JP. Skill mix in healthcare: an international update for the management debate. Int J Healthc Manag. 2013;6(1):12–7.
Seitio-Kgokgwe OS, Gauld R, Hill PC, Barnett P. Understanding human resource management practices in Botswana’s public health sector. J Health Organ Manag. 2016;30(8):1284–300.
Miners C, Hundert M, Lash R. New structures for challenges in healthcare management. Healthc Manage Forum. 2015;28(3):114–7.
Hopkins J, Fassiotto M, Ku MC, Mammo D, Valantine H. Designing a physician leadership development program based on effective models of physician education. Health Care Manag Rev. 2017. https://0-doi-org.brum.beds.ac.uk/10.1097/hmr.0000000000000146.
Miranda R, Glenn SW, Leighton JA, Pasha SF, Gurudu SR, Teaford HG, et al. Using hybrid change strategies to improve the patient experience in outpatient specialty care. J Healthc Manag. 2015;60(5):363–76.
Acknowledgements
Not applicable
Funding
The rapid review is part of a larger study on global health management priorities and qualities, supported by the University of New South Wales, Sydney.
Availability of data and materials
The data that support the findings of this review are included in this published article.
Author information
Authors and Affiliations
Contributions
CF conducted the database searches and identification of relevant literature. RH and AC assessed the selected literature. RH and LM conceived the design of the review and contributed to the interpretation of the review results. CF drafted the initial manuscript while RH, AC and LM reviewed and revised subsequent drafts of the manuscript for important intellectual content. All authors read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable
Consent for publication
Not applicable
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Figueroa, C.A., Harrison, R., Chauhan, A. et al. Priorities and challenges for health leadership and workforce management globally: a rapid review. BMC Health Serv Res 19, 239 (2019). https://0-doi-org.brum.beds.ac.uk/10.1186/s12913-019-4080-7
Received:
Accepted:
Published:
DOI: https://0-doi-org.brum.beds.ac.uk/10.1186/s12913-019-4080-7