- Review
- Open access
- Published:
Strategies to measure and improve emergency department performance: a scoping review
Scandinavian Journal of Trauma, Resuscitation and Emergency Medicine volume 28, Article number: 55 (2020)
Abstract
Background
Over the last two decades, Emergency Department (ED) crowding has become an increasingly common occurrence worldwide. Crowding is a complex and challenging issue that affects EDs’ capacity to provide safe, timely and quality care. This review aims to map the research evidence provided by reviews to improve ED performance.
Methods and findings
We performed a scoping review, searching Cochrane Database of Systematic Reviews, Scopus, EMBASE, CINAHL and PubMed (from inception to July 9, 2019; prospectively registered in Open Science Framework https://osf.io/gkq4t/). Eligibility criteria were: (1) review of primary research studies, published in English; (2) discusses a) how performance is measured in the ED, b) interventions used to improve ED performance and their characteristics, c) the role(s) of patients in improving ED performance, and d) the outcomes attributed to interventions used to improve ED performance; (3) focuses on a hospital ED context in any country or healthcare system. Pairs of reviewers independently screened studies’ titles, abstracts, and full-texts for inclusion according to pre-established criteria. Discrepancies were resolved via discussion. Independent reviewers extracted data using a tool specifically designed for the review. Pairs of independent reviewers explored the quality of included reviews using the Risk of Bias in Systematic Reviews tool. Narrative synthesis was performed on the 77 included reviews. Three reviews identified 202 individual indicators of ED performance. Seventy-four reviews reported 38 different interventions to improve ED performance: 27 interventions describing changes to practice and process (e.g., triage, care transitions, technology), and a further nine interventions describing changes to team composition (e.g., advanced nursing roles, scribes, pharmacy). Two reviews reported on two interventions addressing the role of patients in ED performance, supporting patients’ decisions and providing education. The outcomes attributed to interventions used to improve ED performance were categorised into five key domains: time, proportion, process, cost, and clinical outcomes. Few interventions reported outcomes across all five outcome domains.
Conclusions
ED performance measurement is complex, involving automated information technology mechanisms and manual data collection, reflecting the multifaceted nature of ED care. Interventions to improve ED performance address a broad range of ED processes and disciplines.
Introduction
Over the last two decades, Emergency Department (ED) crowding has become an increasingly common occurrence worldwide [1]. EDs must continue to provide care during periods of crowding, and respond to expected changes (e.g., seasonal increase in demand) and unexpected changes (e.g., unanticipated events and varying demand) [2]. However, crowding impedes ED staffs’ capacity to provide timely, safe and quality care. It extends the time patients spend in ED, and threatens patient outcomes [3].
Crowding in EDs is the product of input, throughput and output factors such as the volume of patients arriving to be seen, the time taken to assess and treat patients, and the availability of beds in hospital wards [4]. Interventions (e.g., decision-making structure, resource allocation, procedures) to address these factors have been widely implemented, with mixed results [5,6,7,8]. Identifying effective interventions known to have improved care can support the uptake of those interventions in different contexts. Understanding the characteristics of those interventions and their limitations can inform the development of new strategies to address common patient flow problems.
Ideally, the design and selection of performance measures should align with the system’s purpose and improvement strategy in order to identify the extent to which the system is working effectively. It is unsurprising then that input, throughput and output measures such as wait-time, length of stay and patient satisfaction have been used to report on EDs’ performance [4, 9]. Understanding how ED performance has been measured in the past will support the selection of measures and inform the development of new measures to address gaps in performance knowledge.
The purpose of this scoping review was to map the research evidence provided by reviews on strategies to measure and improve ED performance. The review questions addressed were: (1) how is ED performance measured, (2) what are the interventions used to improve ED performance and (3) what is the role(s) of patients in improving ED performance, and (4) what are the outcomes attributed to interventions used to improve ED performance.
Methods
Study design
We conducted a scoping review of the literature from inception of bibliographic databases to July 2019 related to strategies to measure and improve ED performance. The study protocol was prospectively registered in December 2018 in the Open Science register (https://osf.io/73r4t). This protocol guided the review in adherence with the preferred reporting items for systematic reviews and meta-analyses statement (PRISMA) [10].
Inclusion criteria
Systematic reviews of primary research studies, reviews of reviews (umbrella reviews), and other research syntheses not fulfilling all criteria for systematic reviews published in the English-language peer-reviewed literature were included that met the following additional criteria: (1) review studies involving clinicians, patients, and/ or administrators in the ED or review studies that measure ED performance without involving participants (e.g., Length of Stay or patient mortality retrieved from aggregate hospital data); (2) discusses a) how performance is measured in the ED, b) interventions used to improve ED performance and their characteristics, c) the role(s) of patients in improving ED performance, and d) the outcomes attributed to interventions used to improve ED performance; (3) focuses on studies in a hospital ED context in any country or healthcare system.
Search strategy
To identify eligible studies, we developed a comprehensive search strategy using medical subject headings and text words for the general concepts of performance measures, interventions, and patient involvement. Cochrane Database of Systematic Reviews, Scopus, Embase, CINAHL and PubMed were searched on 14 January 2019. No date limits were used. English only publications were considered. An updated search was completed on 9 July 2019 and included a date filter (publications from 1 January 2019 to 31 December 2019). The full search strategy for all databases is shown in Appendix A (See Additional file 1).
An example, illustrating the search strategy for PubMed, is as follows:
((((emergency Service, Hospital [mh]) OR emergency department [tw])) AND (((((quality of health care [mh]) OR quality improvement [mh]) OR quality [tw]) OR improvement [tw]) OR performance [tw])) AND ((((((((review [ti]) OR systematic review [ti]) OR meta-analysis [ti]) OR meta-synthesis [ti]) OR scoping review [ti]) OR integrative review [ti]) OR overview [ti]) OR umbrella review [ti])
Study selection
The results of the searches were entered into EndNote citation management software (version 8.2; Thompson Reuters, New York, NY), and duplicates were removed. For each review, title, abstract, and full-text were independently screened by pairs of reviewers for inclusion according to pre-established criteria. Disagreements were resolved via discussion. Abstracts flagged as potentially relevant by reviewers underwent full-text review.
Data extraction and quality assessment
The data was extracted by independent reviewers by using an extraction tool specifically designed for the review. The data extraction form was piloted for usability prior to data extraction. The extraction form included information on Author(s), year of publication, country where review was conducted, type of review, review objectives and questions, number of studies included, types of intervention/s, intervention characteristics, type of measure used and/ or type of outcome measured.
The quality of the included papers was assessed using the Risk of Bias in Systematic Reviews (ROBIS) tool for assessing the risk of bias in systematic reviews [11]. The purpose of this assessment was only to allow for the quality of the included reviews to be mapped/ described. Prior to critical appraisal, the ROBIS was piloted on a sample of reviews. The quality of included reviews was explored by pairs of independent reviewers. Disagreements were resolved via discussion.
Data processing and analysis
A narrative synthesis was performed for this review, including numerical statistical summaries, textual commentaries, and tabular and graphical representations.
Results
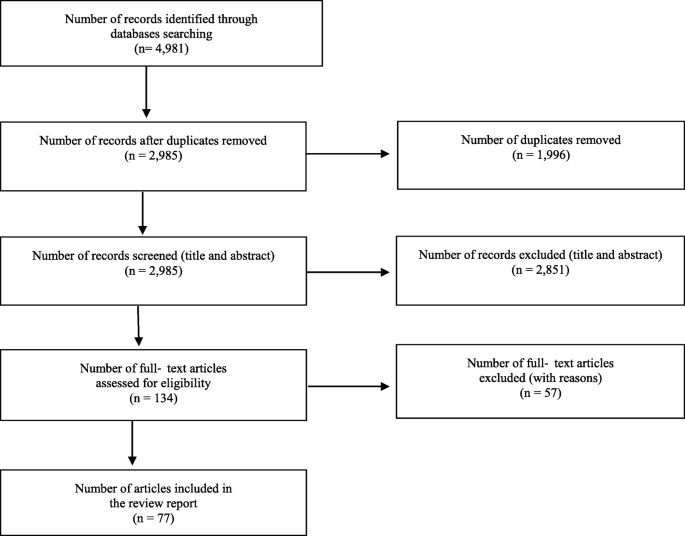
The combined searches yielded 4981 articles, including 1996 duplicate articles. Of these, 2985 abstracts and 134 full-texts were reviewed with 77 articles meeting inclusion criteria. Figure 1 illustrates the PRISMA diagram for the identification, screening, and inclusion processes.
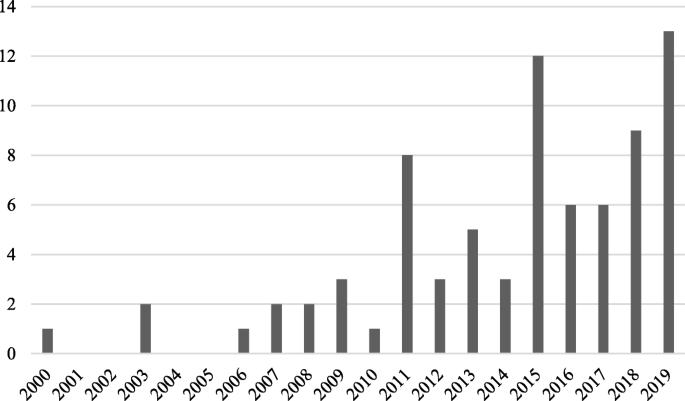
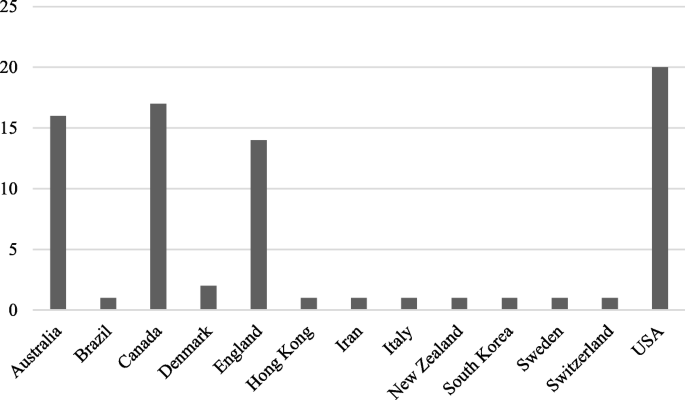
An additional table outlines the characteristics of the included articles addressing ED performance measures (See Additional file 2). An additional table outlines the characteristics of the included articles addressing interventions, and patient role in ED performance (See Additional file 3). An additional table outlines the evidence contribution of the included reviews to each review question (See Additional file 4). Distribution of included reviews published per year (2000–2019) is provided in Fig. 2. Figure 3 shows the distribution of locations where published reviews were conducted (based on the country affiliation of the first author).
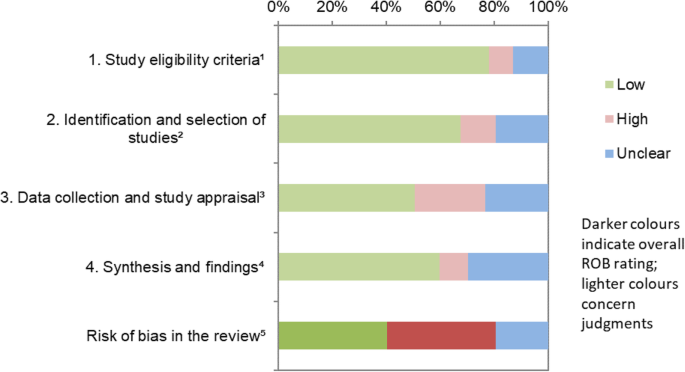
Quality assessment
Using the ROBIS tool, 31 reviews were assessed as being low bias, 31 as high bias, and 15 as unclear bias. The ROBIS risk of bias assessment results for each domain and the overall risk of bias for individual reviews are presented in an additional file (See Additional file 5). Figure 4 displays a summary ROBIS assessment across all included reviews, graphically presenting the results of the ROBIS assessment for each domain and the overall rating.
Graphical presentation for ROBIS results across all included reviews. 1 study eligibility criteria prespecified and appropriate for the review question. 2 sensitivity of the search. 3 rigour of the data collection process. 4 appropriateness of the synthesis for the review question. 5 overall risk of bias. “Low”, “high”, or “unclear” represents the rated level of concern about bias associated with each domain [11]
How ED performance is measured
Three reviews reported on ED performance measures [12,13,14]. Madsen (2015) extracted evidence for 202 individual indicators of ED performance from 127 articles, categorising them into process (e.g., time to diagnosis, physician workload), outcome (e.g., mortality, ambulance diversion), satisfaction (e.g., rate of complaints, patient participation in own care), structural/ organisational (e.g., admission rate, resources) and equity (e.g., weekday/weekend variation, sex, race, age) performance measures. Data sources used to generate the indicators are ED information technology, questionnaires, chart reviews, and multihospital databases [12]. Sørup (2013) identified 55 different performance measures and categorised ED performance measures into patient related measures focusing on safety (e.g., medication errors, unplanned reattendance), patient centeredness (e.g., complaints, left-without-being-seen), and satisfaction; employee related measures focusing on occupational profile (e.g., educational positions), and work environment; and operational performance focusing on planning (e.g., occupancy rate), utilisation (e.g., number of ECG’s taken, number of consultations), efficiency (e.g., ED admission transfer rate, length of stay), and time intervals (e.g., time to registration, triage, treatment). Stang (2015) examined crowding measures linked with quality of care including ED volume, number of patients in the waiting room, and ED length of stay.
Interventions used to improve ED performance and their characteristics
The remaining 74 articles addressed interventions used to improve ED performance. Interventions to improve ED performance address either practices and processes or team composition. Interventions addressing how tasks were performed in ED were identified as practice and process interventions. Interventions addressing the discipline or training of professionals practicing in ED were identified as team composition interventions.
Practices and processes
Six domains of clinical practice and processes have been targeted for interventions. They are: triage, care transitions, process re-design, point-of-care testing, observation units, and technology.
Triage
Designed to expedite care, triage processes sort patients according to urgency or type of service required [15]. Twelve reviews examined interventions relating to triage systems and processes. Triage based interventions included having a physician present [8, 16,17,18,19] also called a triage liaison physician [20], a triage team consisting of at least 2 medical personnel (nurse or physician) [21, 22], dedicated triage resources (e.g., ECG machine and ECG technician [23]), triage education [23], variations of basic triage [15], triage protocols [24, 25], and nurse-led triage services [26]. A description of the characteristics for each type of triage intervention is provided in Table 1.
Care transitions (handover processes)
Care transitions involved patient handover, which is the process of transferring accountability and responsibility for patient care to another person [27]. Seven reviews examined interventions relating to patient handover processes and transitions in care. Patient handover processes and transitions in care interventions include handover tools [27,28,29,30], bedside registration [19, 31], discharge planning [31], discharge communication [32], process protocols and guidelines [27, 29, 30], handover training [29], dedicated offload nurse for triaging and assessing EMS patients [30], nurse discharge coordinators [33]. A description of the characteristics for each type of care transition intervention is provided in Table 2.
Process re-design
Process re-design refers to changes in how tasks are performed. Twenty-three reviews examined interventions relating to process re-design. Processes that have been re-designed included clinical guidelines and protocols [25, 31, 34,35,36], patient assignment and referral processes [4, 31, 36,37,38], organisational processes (e.g., communication, administration) [19, 25, 35, 39, 40], nurse-initiated care processes [8, 17, 21, 41,42,43,44], clinical decision supports [45,46,47], and lean management/ lean thinking interventions [48,49,50]. A description of the characteristics for each type of process re-design intervention is provided in Table 3.
Point-of-care testing
Point-of-care testing refers to laboratory analysis located in the ED [8, 21]. Five reviews examined point of care testing in ED [8, 19, 21, 51, 52]. Point-of-care testing has been used for a range of diagnostic tests including cardiac troponin [51], metabolic [19], urinalysis, pregnancy testing, cardiac markers, glucose [19], influenza, and respiratory syncytial virus [52].
Observation units
Observation Unit interventions refer to ED-based observation units [31]. Twelve reviews examined observation units in ED [4, 8, 17,18,19, 25, 31, 39, 53,54,55,56]. ED based observation units have been developed for specific clinical needs such as Chest pain and Asthma [31, 39], for specific processes such as assessment and procedures (e.g., Rapid Assessment Zones/ Pods) [18, 55], medically stable patients likely to require admission (e.g., Medical Assessment Units) [4, 8, 17], or further investigations (e.g., Short Stay Units) [8, 17, 54, 56], management for more than 4 h (e.g., ED managed Acute Care Unit) [19], or to manage referrals from GPs (e.g., Quick Diagnostic Units) [18]. A description of the characteristics for each type of process re-design intervention is provided in Table 4.
Technology
Technology has been increasingly integrated into the ED [57]. Seven reviews examined interventions addressing technology in the ED. Technology has been introduced into EDs in the form of health information technology such as computerised clinical support systems (e.g., decision supports and provider entry forms) [45, 58], mobile devices [57], and telecommunication technology [59], computer simulation [60], and eHealth records access [61, 62]. A description of the characteristics for each type of technology intervention is provided in Table 5.
Team composition interventions
Different roles and specialties have been integrated into the ED. These included advanced nursing roles, physiotherapy, general practitioners, scribes and physician assistants, pharmacy, and mental health services, as well as the development of professional skills.
Advanced Nursing Roles. Seven reviews examined interventions relating to advancing nursing roles in the ED. Advanced nursing interventions primarily include the nurse practitioner role [17, 18, 63,64,65,66] sometimes called advanced nurse practitioner/ advanced clinical practitioner/ advanced practice nurse [66, 67], clinical nurse specialists [65], certified registered nurse anaesthetists [65], and Clinical Initiatives Nurse (CIN [17, 68];. Advanced nursing roles typically require further education and require a minimum of 2 years emergency nursing experience [68]. A description of the characteristics for each type of advanced nursing role intervention is provided in Table 6.
Physiotherapy
Three reviews examined interventions relating to physiotherapy roles in ED [69,70,71]. The role of physiotherapists in ED includes the assessment and management of acute and subacute musculoskeletal conditions, recent burns and diabetic wounds, provision of in-service training to other ED staff, liaising with nursing, medical, and allied health staff, and ensuring safe discharge from ED including arranging community services [69,70,71]. Physiotherapists have also been trained to read and request imaging and to prescribe a limited number of medications [69, 70].
General practitioners
Two reviews examined interventions relating to general practitioner roles in ED [72, 73]. There are different models in which general practitioners have been introduced into ED [72, 73]. General practitioners have been used to staff non-urgent (rather than urgent) streams when patients are triaged into separate streams [72, 73]. General practitioner services are also available onsite next to the ED and patients self-select or are redirected to these services from the ED. General practitioners have also been involved in the triage of patients presenting to the ED [72, 73]. General practitioners have also been fully integrated into ED, providing care jointly with ED staff on a range of primary care and higher acuity emergency cases [72, 73].
Scribes and physician assistants
Four reviews examined interventions relating to models of care using support staff such as scribes and physician assistant roles in ED [8, 18, 74,75,76]. A description of the characteristics for scribes and physician assistants interventions is provided in Table 7.
Pharmacy
Two reviews examined interventions relating to pharmacy roles in ED [77, 78]. The scope of pharmacy roles in the ED varied. In the ED, pharmacists conduct consultations including interpreting results and providing pharmacotherapy recommendations [77, 78]. ED pharmacy programs also included pharmacists tracking patients medication due times for repeat medications, completing medication histories, documenting patient body weight, height, and allergies [77, 78]. Pharmacists have also been involved ED patient follow-up on culture and susceptibility results, adjusting or discontinuing therapy as needed [77, 78].
Mental health services
Two reviews examined interventions relating to mental health services in ED [79, 80] including Liaison Mental Health Services [79, 80], co-located Psychiatry Liaison Personnel/ Spaces [80], Psychiatry Specialist Services [80]. A description of the characteristics for each type of mental health services intervention is provided in Table 8.
Professional development
Nine reviews examined professional development interventions in ED. Professional development interventions included eight-hour customer service training related to applying industry customer service principles to health care, benchmarks, and taught customer service skills such as negotiating agreement and resolution of expectations [31, 39]; and a 10 week medical Spanish language course [39]. The provision of audit/ feedback (from a supervisor/ colleague/ external coder) on clinical practice has been implemented in a variety of formats including weekly case specific, every 6 weeks individual feedback with group discussion; or individual feedback provided via email, written, verbal, electronic, and combination of media, one on one, group, (e.g., patient outcomes, quality of documentation [81,82,83]. Other interventions include cross-training nurses to care for patients in a designated area [25], monthly staff education/ workshops about hand hygiene with elements of targeted feedback [84], and clinical education to improve nurses’ and medical staffs’ knowledge of pain management through an education program [42, 85].
The role(s) of patients in improving ED performance
Patients are consumers of healthcare services provided by EDs. The delivery of healthcare depends on the relationship between clinicians and patients and the degree to which patients play an active or passive role [86]. Two reviews examined the role of patients in improving ED performance [42, 86]. Patients’ role in improving ED performance has been primarily addressed by involving patients in shared decision making. Shared decision-making involves active patient involvement with the clinician, sharing information and collaboratively taking steps to reach agreement about which treatment to implement [86]. Shared decision making has been addressed through decision supports [86], and education [42]. A description of the characteristics for each type of patient role intervention is provided in Table 9.
The outcomes attributed to interventions used to improve ED performance
The outcomes attributed to interventions used to improve ED performance identified by the review can be categorised into five key areas: Time, proportion, process, cost, and clinical outcomes. Time-based measures record time stamps/ intervals, and sub-cycle intervals [25]. Measures of time intervals varied, however, the most commonly used were length of stay (LOS) in ED and waiting time. Proportion-based measures record elements of ED performance rates [25]. Measures of proportion-based measures varied widely and included admissions, resource use, and treatment follow-up rate. Process-based measures document elements of ED process performance [25]. Direct and indirect measures of quality of care, including left without being seen, did not wait, as well as patient and provider satisfaction, were commonly reported ED process performance measures. Cost-based measures indicate the financial implications of health care provided. Measures of cost varied and lacked detail, and were often reported simply as “costs” [18, 51, 62]. Clinical-based measures indicate the medical outcomes for patients of the health care provided. Measures of clinical outcomes reported varied, however, and the most commonly used were adverse events and readmission.
Practices and processes
Overall, time-based and process-based outcome domains were the most widely used measures for interventions with 24 out of the 30 individual interventions reporting at least one of each of these domains. Proportion-based outcomes were similarly well reported on for interventions with 21 out of the 30 interventions reporting proportion-based measures. Cost-based and clinical-based outcomes were the least utilised domains with only 12 and 17 interventions respectively reporting at least one outcome in these domains.
Team composition
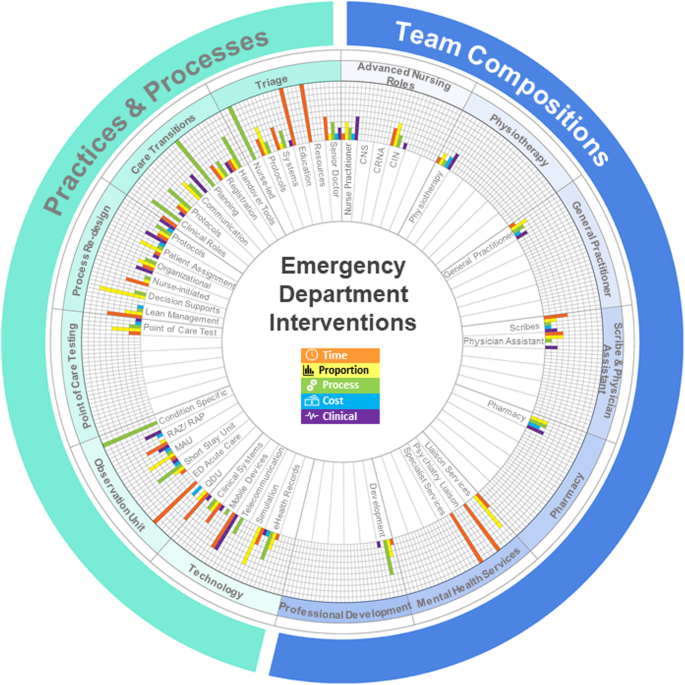
The time-based outcome was the most widely used domain for team composition interventions, with 10 of the 13 interventions reporting at least one time-based measure. Proportion-based measures were reported for nine of the 13 interventions with process-based and clinical-based measures reported for 8 of the interventions. Cost-based outcomes were the least utilised, with six interventions reporting at least one outcome in this domain. An additional file provides a full list of intervention performance measures reported for the included interventions (See Additional file 6). Figure 5 displays a summary of the types of interventions within practices and processes and team composition, as well as graphically presenting the proportion of the total number of outcome measures reported for each domain for each intervention.
Overview of the outcome measures used for ED interventions. The rich picture summarises the types of interventions identified by this review. The graphs for each intervention present the proportion of outcome measures reported for each domain for each intervention. Each proportion was calculated as the number of identified outcome measures in the domain divided by the total number of outcome measures for the intervention. CNS, clinical nurse specialist; CRNA, certified registered nurse anaesthetist; CIN, clinical initiatives nurse; RAZ/RAP, rapid assessment zone/ rapid assessment pod; MAU, medical assessment unit; ED, Emergency Department; QDU, quick diagnosis unit
Discussion
In this review we aimed to map the research evidence of strategies to measure and improve ED performance. There was strong alignment between how ED performance is measured, the types of ED interventions implemented, and the outcome measures used to assess effectiveness of those interventions.
While EDs worldwide may share a common purpose [87,88,89], the differences and complexity within each ED system is reflected in the vast number of measures used to understand different aspects of ED performance. Similarly, the different ways these measures have been categorised reflects differences in the interpretation of that common purpose. For EDs and the communities they serve, the selection of performance measures is critical to ensuring a comprehensive, accurate and precise picture of ED performance is developed. It is equally important to develop a shared understanding how ED performance data is collected to ensure that measures used for performance assessment or comparison are valid.
The results of our review show that the delivery of care in ED has evolved over the last 20 years with the implementation of a wide range of interventions to improve ED performance. The interventions identified by this review address very specific aspects of how care is provided in ED, suggesting that a systems perspective has not been applied. Crucially, EDs are complex adaptive systems and any intervention implemented to improve performance is likely influenced by existing models of care, as well as a variety of contextual factors such as funding, availability of skilled workforce, and the physical space available.
Changing patient involvement in the provision of care also plays a role in ED performance. The small number of reviews identified by this review that involved patient perspectives suggests that care delivery in the ED is likely driven by clinicians and protocols, with patients as passive consumers of care. In the crowded and frantic ED context, achieving patient-centred care is likely a challenging task [33]. Our findings suggest that achieving active participation by patients in ED care delivery is possible, but more research is needed on the implications for ED performance and patients’ clinical and psychosocial outcomes.
Intervention outcome measures allow us to determine if the intervention to improve ED performance was successful or if it had unintended outcomes. While the use of all five types of outcome measures synthesised in our review would provide clinicians, hospital administrators and researchers with the most insight into ED performance and intervention effectiveness, implementation of the full suite of measures may not be possible in some contexts. Most studies reported the use of three or fewer types of outcome measures. Measures of time were commonly combined with proportion or process measures. The use of time, proportion and process measures provides insight into the speed of healthcare provision, the quantity of resources used (e.g., diagnostic tests), and the quality of patient management (e.g., clinical documentation). However, intervention implementation decisions are often made based on department budgets or the availability of funding. As such, the inclusion of cost measures is increasingly important to inform clinicians’ and administrators’ decisions about ED performance and intervention effectiveness. Finally, measures of clinical outcomes are also important for examining the assumption that system changes in healthcare provide improved patient safety and clinical outcomes, and this is a neglected area for many interventions.
Limitations
This scoping review is the first, to our knowledge, to synthesise the many review articles to comprehensively describe the different strategies that have been used to measure and improve ED performance. Limitations of the current study include our pragmatic choice to only include reviews published in English and the potential biases of the included studies. The published reviews examining the effectiveness of interventions in the ED context might have suffered from publication bias, with negative results less likely to be published. As a result of this publication bias, it is unclear what interventions are unsuccessful or if particular context characteristics result in unsuccessful interventions, or negatively impact on patient care.
Conclusion
Over the last two decades, the way care has been delivered in ED has changed dramatically in response to increased demand and increasing complexity, and it is likely that it will continue to change over the next two decades. In turn, the way we measure ED performance has changed with our capacity to collect and analyse data. We need to think critically about the performance measures we use to define ED performance to ensure we are capturing a complete and dynamic picture that accurately reflects how an ED is performing. As shown by this review, a number of different strategies have been used to improve ED performance. As both internal and external pressures on ED continue to grow, future intervention initiatives will be needed to ensure the tragic consequences of crowding in ED are avoided. Crucially, a comprehensive range of meaningful outcome measures for interventions needs to be used to accurately establish the effectiveness of ED interventions and inform system changes and decision-making.
Availability of data and materials
All data generated or analysed during this study are included in this published article and its supplementary information files.
References
Di Somma S, Paladino L, Vaughan L, Lalle I, Magrini L, Magnanti M. Overcrowding in emergency department: an international issue. Intern Emerg Med. 2015;10(2):171–5.
Braithwaite J, Wears RL, Hollnagel E. Resilient health care: turning patient safety on its head. International J Qual Health Care. 2015;27(5):418–20.
Miró O, Antonio MT, Jiménez S, De Dios A, Sánchez M, Borrás A, et al. Decreased health care quality associated with emergency department overcrowding. Eur J Emerg Med. 1999;6(2):105–7.
Hoot NR, Aronsky D. Systematic review of emergency department crowding: causes, effects, and solutions. Ann Emerg Med. 2008;52(2):126–136.e1.
Handel DA, Ma OJ, Workman J, Fu R. Impact of an expeditor on emergency department patient throughput. West J Emerg Med. 2011;12(2):198–203.
Shetty A, Gunja N, Byth K, Vukasovic M. Senior streaming assessment further evaluation after triage zone: a novel model of care encompassing various emergency department throughput measures. EMA - Emerg Med Australas. 2012;24(4):374–82.
Karpas A, Finkelstein M, Reid S. Parental preference for rehydration method for children in the emergency department. Pediatr Emerg Care. 2009;25(5):301–6.
De Freitas L, Goodacre S, O’Hara R, Thokala P, Hariharan S. Interventions to improve patient flow in emergency departments: an umbrella review. Emerg Med J. 2018;35(10):626–37.
Schull MJ, Guttmann A, Leaver CA, Vermeulen M, Hatcher CM, Rowe BH, et al. Prioritizing performance measurement for emergency department care: consensus on evidencebased quality of care indicators. Can J Emerg Med. 2011;13(5):300–9.
Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol. 2009;62(10):1006–12.
Whiting P, Savovi J, Higgins JPT, Caldwell DM, Reeves BC, Shea B, et al. ROBIS: a new tool to assess risk of bias in systematic reviews was developed. J Clin Epidemiol. 2016;69:225–34.
Madsen M, Kiuru S, Castrèn M, Kurland L. The level of evidence for emergency department performance indicators: systematic review. Eur J Emerg Med. 2015;22(5):298–305.
Sørup CM, Jacobsen P, Forberg JL. Evaluation of emergency department performance - a systematic review on recommended performance and quality-in-care measures. Scand J Trauma Resusc Emerg Med. 2013;21(1):62.
Stang AS, Crotts J, Johnson DW, Hartling L, Guttmann A. Crowding measures associated with the quality of emergency department care: a systematic review. Acad Emerg Med. 2015;22(6):643–56.
Harding KE, Taylor NF, Leggat SG. Do triage systems in healthcare improve patient flow? A systematic review of the literature. Aust Health Rev. 2011;35(3):371–83.
Abdulwahid MA, Booth A, Kuczawski M, Mason SM. The impact of senior doctor assessment at triage on emergency department performance measures: systematic review and meta-analysis of comparative studies. Emerg Med J. 2016;33(7):504–13.
Elder E, Johnston ANB, Crilly J. Review article: systematic review of three key strategies designed to improve patient flow through the emergency department. EMA - Emerg Med Australas. 2015;27(5):394–404.
Wylie K, Crilly J, Toloo G, Fitzgerald G, Burke J, Williams G, et al. Review article: emergency department models of care in the context of care quality and cost: a systematic review. EMA - Emerg Med Australas. 2015;27(2):95–101.
Morley C, Unwin M, Peterson GM, Stankovich J, Kinsman L. Emergency department crowding: a systematic review of causes, consequences and solutions. PLoS One. 2018;13(8):e0203316.
Rowe BH, Guo X, Villa-Roel C, Schull M, Holroyd B, Bullard M, et al. The role of triage liaison physicians on mitigating overcrowding in emergency departments: a systematic review. Acad Emerg Med. 2011;18(2):111–20.
Oredsson S, Jonsson H, Rognes J, Lind L, Göransson KE, Ehrenberg A, et al. A systematic review of triage-related interventions to improve patient flow in emergency departments. Scand J Trauma Resusc Emerg Med. 2011;19(1):43.
Ming T, Lai A, Lau PM. Can team triage improve patient flow in the emergency department? A systematic review and meta-analysis. Adv Emerg Nurs J. 2016;38(3):233–50.
Chhabra S, Eagles D, Kwok ESH, Perry JJ. Interventions to reduce emergency department door-to- electrocardiogram times: a systematic review. CJEM. 2019;21(5):607–17.
Robinson DJ. An integrative review: triage protocols and the effect on ED length of stay. J Emerg Nurs. 2013;39(4):398–408.
McCaughey D, Erwin CO, DelliFraine JL. Improving capacity management in the emergency department: a review of the literature, 2000-2012. J Healthc Manag. 2015;60(1):63–75.
Rehman SA, Ali PA. A review of factors affecting patient satisfaction with nurse led triage in emergency departments. Int Emerg Nurs. 2016;29:38–44.
Dawson S, King L, Grantham H. Review article: improving the hospital clinical handover between paramedics and emergency department staff in the deteriorating patient. EMA - Emerg Med Australas. 2013;25(5):393–405.
Alimenti D, Buydos S, Cunliffe L, Hunt A. Improving perceptions of patient safety through standardizing handoffs from the emergency department to the inpatient setting: a systematic review. J Am Assoc Nurse Pract. 2019;31(6):354–63.
Flynn D, Francis R, Robalino S, Lally J, Snooks H, Rodgers H, et al. A review of enhanced paramedic roles during and after hospital handover of stroke, myocardial infarction and trauma patients. BMC Emerg Med. 2016;17(1):5.
Reay G, Norris JM, Nowell L, Hayden KA, Yokom K, Lang ES, et al. Transition in Care from EMS providers to emergency department nurses: a systematic review. Prehosp Emerg Care. 2020; 24(3):421–33.
Boudreaux ED, Cruz BL, Baumann BM. The use of performance improvement methods to enhance emergency department patient satisfaction in the United States: a critical review of the literature and suggestions for future research. Acad Emerg Med. 2006;13(7):795–802.
Curran JA, Gallant AJ, Zemek R, Newton AS, Jabbour M, Chorney J, et al. Discharge communication practices in pediatric emergency care: a systematic review and narrative synthesis. Syst Rev. 2019;8(1):83.
Shankar KN, Bhatia BK, Schuur JD. Toward patient-centered care: a systematic review of older adults’ views of quality emergency care. Ann Emerg Med. 2014;63(5):529–50.
Mieiro DB, de Oliveira ÉBC, da Fonseca REP, Mininel VA, Zem-Mascarenhas SH, Machado RC. Strategies to minimize medication errors in emergency units: an integrative review. Rev Bras Enferm. 2019;72:307–14.
Juillard CJ, Mock C, Goosen J, Joshipura M, Civil I. Establishing the evidence base for trauma quality improvement: a collaborative WHO-IATSIC review. World J Surg. 2009;33(5):1075–86.
Kirkland SW, Soleimani A, Rowe BH, Newton AS. A systematic review examining the impact of redirecting low-acuity patients seeking emergency department care: is the juice worth the squeeze? Emerg Med J. 2019;36(2):97–106.
Hughes JM, Freiermuth CE, Shepherd-Banigan M, Ragsdale L, Eucker SA, Goldstein K, et al. Emergency department interventions for older adults: a systematic review. J Am Geriatr Soc. 2019;67(7):1516–25.
Kumar GS, Klein R. Effectiveness of case management strategies in reducing emergency department visits in frequent user patient populations: a systematic review. J Emerg Med. 2013;44(3):717–29.
Boudreaux ED, O’Hea EL. Patient satisfaction in the emergency department: a review of the literature and implications for practice. J Emerg Med. 2004;26(1):13–26.
Jones P, Schimanski K. The four hour target to reduce emergency department “waiting time”: a systematic review of clinical outcomes. EMA - Emerg Med Australas. 2010;22(5):391–8.
Cabilan CJ, Boyde M. A systematic review of the impact of nurse-initiated medications in the emergency department. Australas Emerg Nurs J. 2017;20(2):53–62.
Williams S, Keogh S, Douglas C. Improving paediatric pain management in the emergency department: an integrative literature review. Int J Nurs Stud. 2019;94:9–20.
Considine J, Shaban RZ, Curtis K, Fry M. Effectiveness of nurse-initiated X-ray for emergency department patients with distal limb injuries. Eur J Emerg Med. 2019;26(5):314–22.
Rowe BH, Villa-Roel C, Guo X, Bullard MJ, Ospina M, Vandermeer B, et al. The role of triage nurse ordering on mitigating overcrowding in emergency departments: a systematic review. Acad Emerg Med. 2011;18(12):1349–57.
Bennett P, Hardiker NR. The use of computerized clinical decision support systems in emergency care: a substantive review of the literature. J Am Med Inform Assoc. 2017;24(3):655–68.
Deblois S, Chartrand-Lefebvre C, Toporowicz K, Chen Z, Lepanto L. Interventions to reduce the overuse of imaging for pulmonary embolism: a systematic review. J Hosp Med. 2018;13(1):52–61.
Desai S, Liu C, Kirkland SW, Krebs LD, Keto-Lambert D, Rowe BH. Effectiveness of implementing evidence-based interventions to reduce C-spine image ordering in the emergency department: a systematic review. Acad Emerg Med. 2018;25(6):672–83.
Bucci S, De Belvis AG, Marventano S, De Leva AC, Tanzariello M, Specchia ML, et al. Emergency department crowding and hospital bed shortage: is lean a smart answer? A systematic review. Eur Rev Med Pharmacol Sci. 2016;20(20):4209–19.
Holden RJ. Lean thinking in emergency departments: a critical review. Ann Emerg Med. 2011 Mar 1;57(3):265–78.
Isfahani HM, Tourani S, Seyedin H. Features and results of conducted studies using a lean management approach in emergency Department in Hospital: a systematic review. Bull Emerg Trauma. 2019;7(1):9.
Bingisser R, Cairns C, Christ M, Hausfater P, Lindahl B, Mair J, et al. Cardiac troponin: a critical review of the case for point-of-care testing in the ED. Am J Emerg Med. 2012;30(8):1639–49.
Doan Q, Enarson P, Kissoon N, Klassen TP, Johnson DW. Rapid viral diagnosis for acute febrile respiratory illness in children in the emergency department. Cochrane Database Syst Rev. 2014;(9):CD006452. https://0-doi-org.brum.beds.ac.uk/10.1002/14651858.CD006452.pub4.
Goodacre SW. Should we establish chest pain observation units in the UK? A systemic review and critical appraisal of the literature. J Accid Emerg Med. 2000;17(1):1–6.
Konnyu KJ, Kwok E, Skidmore B, Moher D. The effectiveness and safety of emergency department short stay units: a rapid review. Open Med. 2012;6(1):e10.
Bullard MJ, Villa-Roel C, Guo X, Holroyd BR, Innes G, Schull MJ, et al. The role of a rapid assessment zone/pod on reducing overcrowding in emergency departments: a systematic review. Emerg Med J. 2012;29(5):372–8.
Galipeau J, Pussegoda K, Stevens A, Brehaut JC, Curran J, Forster AJ, et al. Effectiveness and safety of short-stay units in the emergency department: a systematic review. Acad Emerg Med. 2015;22(8):893–907.
Dexheimer JW, Borycki EM. Use of mobile devices in the emergency department: a scoping review. Health Informatics J. 2015;21(4):306–15.
Georgiou A, Prgomet M, Paoloni R, Creswick N, Hordern A, Walter S, et al. The effect of computerized provider order entry systems on clinical care and work processes in emergency departments: a systematic review of the quantitative literature. Ann Emerg Med. 2013;61(6):644–53.
Kelton DK, Szulewski A, Howes D. Real-time video telemedicine applications in the emergency department: a scoping review of literature. Can J Emerg Med. 2018;20(6):920–8.
Mohiuddin S, Busby J, Savović J, Richards A, Northstone K, Hollingworth W, et al. Patient flow within UK emergency departments: a systematic review of the use of computer simulation modelling methods. BMJ Open. 2017;7(5):e015007.
Bowden T, Coiera E. The role and benefits of accessing primary care patient records during unscheduled care: a systematic review. BMC Med Inform Decis Mak. 2017;17(1):138.
Hersh WR, Totten AM, Eden KB, Devine B, Gorman P, Kassakian SZ, et al. Outcomes from health information exchange: systematic review and future research needs. JMIR Med Informatics. 2015;3(4):e39.
Carter AJE, Chochinov AH. A systematic review of the impact of nurse practitioners on cost, quality of care, satisfaction and wait times in the emergency department. Can J Emerg Med. 2007;9(4):286–95.
Jennings N, Clifford S, Fox AR, O’Connell J, Gardner G. The impact of nurse practitioner services on cost, quality of care, satisfaction and waiting times in the emergency department: a systematic review. Int J Nurs Stud. 2015;52(1):421–35.
Kleinpell RM, Ely EW, Grabenkort R. Nurse practitioners and physician assistants in the intensive care unit: an evidence-based review. Crit Care Med. 2008;36(10):2888–97.
Thamm C, Teleni L, Chan RJ, Stone L, Mccarthy AL. Nurse-led interventions for cancer patients in emergency departments: systematic review. Collegian. 2019;26(2):311–9.
Williams K. Advanced practitioners in emergency care: a literature review. Emerg Nurse. 2017;25(4):36–41.
Innes K, Jackson D, Plummer V, Elliott D. Care of patients in emergency department waiting rooms - an integrative review. J Adv Nurs. 2015;71(12):2702–14.
Anaf S, Sheppard LA. Physiotherapy as a clinical service in emergency departments: a narrative review. Physiotherapy. 2007;93(4):243–52.
Ferreira GE, Traeger AC, Maher CG. Review article: a scoping review of physiotherapists in the adult emergency department. Emerg Med Australas. 2019;31(1):43–57.
Kilner E. What evidence is there that a physiotherapy service in the emergency department improves health outcomes? A systematic review. J Health Serv Res Policy. 2011;16(1):51–8.
Gonçalves-Bradley D, Khangura JK, Flodgren G, Perera R, Rowe BH, Shepperd S. Primary care professionals providing non-urgent care in hospital emergency departments. Cochrane Database Syst Rev. 2018;(2):CD002097. https://0-doi-org.brum.beds.ac.uk/10.1002/14651858.CD002097.pub4.
Ramlakhan S, Mason S, O’Keeffe C, Ramtahal A, Ablard S. Primary care services located with EDs: a review of effectiveness. Emerg Med J. 2016;33(7):495–503.
Cabilan CJ, Eley RM. Review article: potential of medical scribes to allay the burden of documentation and enhance efficiency in Australian emergency departments. Emerg Med Australas. 2015;27(6):507–11.
Doan Q, Sabhaney V, Kissoon N, Sheps S, Singer J. A systematic review: the role and impact of the physician assistant in the emergency department. Emerg Med Australas. 2011;23(1):7–15.
Heaton HA, Castaneda-Guarderas A, Trotter ER, Erwin PJ, Bellolio MF. Effect of scribes on patient throughput, revenue, and patient and provider satisfaction: a systematic review and meta-analysis. Am J Emerg Med. 2016;34(10):2018–28.
Cohen V, Jellinek SP, Hatch A, Motov S. Effect of clinical pharmacists on care in the emergency department: a systematic review. Am J Heal Pharm. 2009;66(15):1353–61.
Hammond DA, Gurnani PK, Flannery AH, Smetana KS, Westrick JC, Lat I, et al. Scoping review of interventions associated with cost avoidance able to be performed in the intensive care unit and emergency department. Pharmacother J Hum Pharmacol Drug Ther. 2019;39(3):215–31.
Callaghan P, Eales S, Coates T, Bowers L. A review of research on the structure, process and outcome of liaison mental health services. J Psychiatr Ment Health Nurs. 2003;10(2):155–65.
Evans R, Connell J, Ablard S, Rimmer M, O’Keeffe C, Mason S. The impact of different liaison psychiatry models on the emergency department: a systematic review of the international evidence. J Psychosom Res. 2019;119:53–64.
Lavoie CF, Schachter H, Stewart AT, McGowan J. Does outcome feedback make you a better emergency physician? A systematic review and research framework proposal. Can J Emerg Med. 2009;11(6):545–52.
Rogers RLG, Narvaez Y, Venkatesh AK, Fleischman W, Hall MK, Taylor RA, et al. Improving emergency physician performance using audit and feedback: a systematic review. Am J Emerg Med. 2015;33(10):1505–14.
Lorenzetti DL, Quan H, Lucyk K, Cunningham C, Hennessy D, Jiang J, et al. Strategies for improving physician documentation in the emergency department: a systematic review. BMC Emerg Med. 2018;18(1):36.
Seo HJ, Sohng KY, Chang SO, Chaung SK, Won JS, Choi MJ. Interventions to improve hand hygiene compliance in emergency departments: a systematic review. J Hosp Infect. 2019;102(4):394–406.
Sampson FC, Goodacre SW, O’Cathain A. Interventions to improve the management of pain in emergency departments: systematic review and narrative synthesis. Emerg Med J. 2014;31:e9–18.
Flynn D, Knoedler MA, Hess EP, Murad MH, Erwin PJ, Montori VM, et al. Engaging patients in health care decisions in the emergency department through shared decision-making: a systematic review. Acad Emerg Med. 2012;19(8):959–67.
Fleischmann T, Fulde G. Emergency medicine in modern Europe. Emerg Med Australas. 2007;19(4):300–2.
Black JJM, Davies GD. International EMS systems: United Kingdom. Resuscitation. 2005;64(1):21–9.
Morganti KG, Bauhoff S, Blanchard JC, Abir M, Iyer N, Smith A, et al. The evolving role of emergency departments in the United States. Rand Heal Q. 2013;3(2):3.
Acknowledgements
We would like to acknowledge and thank Ms. Teresa Winata for providing support in the proof-reading process. We would also like to acknowledge and thank Mr. Drew McTavish for providing support in the development of Figures.
Funding
This project was not funded.
Author information
Authors and Affiliations
Contributions
EEA, BB, JB and RCW made substantial contributions to the conception of the work. EEA, CT and AS made substantial contributions to the acquisition, analysis and interpretation of the data. All authors approved the submitted version and have agreed both to be personally accountable for the author’s own contributions and to ensure that questions related to the accuracy or integrity of any part of the work, even ones in which the author was not personally involved, are appropriately investigated, resolved, and the resolution documented in the literature.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Additional file 1: Appendix A.
The full search strategy for all databases.
Additional file 2: Table 1.
Characteristics of the included reviews on ED performance measures.
Additional file 3: Table 2.
Characteristics of the included reviews on interventions to improve ED performance.
Additional file 4: Table 3.
The evidence contribution to the review questions of the included reviews.
Additional file 5: Table 4.
The ROBIS Risk of Bias results for each domain and the overall risk of bias for the included reviews
Additional file 6: Table 14.
The performance measures reported by the included reviews for each intervention.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Austin, E.E., Blakely, B., Tufanaru, C. et al. Strategies to measure and improve emergency department performance: a scoping review. Scand J Trauma Resusc Emerg Med 28, 55 (2020). https://0-doi-org.brum.beds.ac.uk/10.1186/s13049-020-00749-2
Received:
Accepted:
Published:
DOI: https://0-doi-org.brum.beds.ac.uk/10.1186/s13049-020-00749-2