Published online Sep 16, 2013. doi: 10.12998/wjcc.v1.i6.205
Revised: July 28, 2013
Accepted: August 5, 2013
Published online: September 16, 2013
The patient was a 1-year-and-4-mo-old boy. He had drunk about 1 L of an isotonic drink for infants daily since about 10 mo after birth. He was examined by a local doctor due to anorexia and vomiting, found to have cardiomegaly, and transported to our hospital with suspected myocarditis. After admission, the patient showed polypnea, a decreased level of consciousness, and marked metabolic acidosis and lapsed into circulatory insufficiency, requiring catecholamine administration, endotracheal intubation, and extracorporeal membrane oxygenation. Initially, low-output heart failure due to acute myocarditis was suspected, but the central venous oxygen saturation was high, at 82%. Considering high-output heart failure to be more likely, we evaluated its cause and noted, by urinary organic acid analysis, increases in lactate, pyruvate, 3-OH-butyrate, acetoacetate, metabolic products of branched-chain amino acids, 2-ketoglutarate, 2-OH-glutarate, 2-keto-adipate, and 2-OH-adipate. Since the vitamin B1 level was reduced to 12 ng/mL (normally 20-50 ng/mL), a diagnosis of cardiac beriberi due to vitamin B1 deficiency was made. When unexplained heart failure is observed in children, cardiac beriberi must be excluded as a differential diagnosis of myocarditis and cardiomyopathy. The measurement of the central venous oxygen saturation may be useful for the diagnosis.
Core tip: When unexplained heart failure is observed in children, cardiac beriberi must be excluded as a differential diagnosis of myocarditis and cardiomyopathy. The measurement of the central venous oxygen saturation may be useful for the diagnosis. Although beriberi is a rare disease today, it is necessary to remember that it may still be caused by an unbalanced diet.
- Citation: Majima N, Umegaki O, Soen M. Use of central venous saturation monitoring in a patient with pediatric cardiac beriberi. World J Clin Cases 2013; 1(6): 205-207
- URL: https://www.wjgnet.com/2307-8960/full/v1/i6/205.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v1.i6.205
The condition related to vitamin B1 deficiency is called beriberi or cardiac beriberi, which markedly decreased due to postwar improvements in the nutritional state. In the latter half of the 1970s, an unbalanced diet due to the excessive intake of instant foods in the young, alcohol intake, and overwork were recognized again as causes of beriberi. Subsequently, its incidence decreased due to improvements in the awareness of nutritional problems associated with instant foods and soft drinks and the addition of vitamins, but beriberi has yet to be eradicated[1,2].
In this report, a child with cardiac beriberi due to excessive intake of an isotonic drink for infants, in whom the measurement of the central venous oxygen saturation was useful for the diagnosis, is presented.
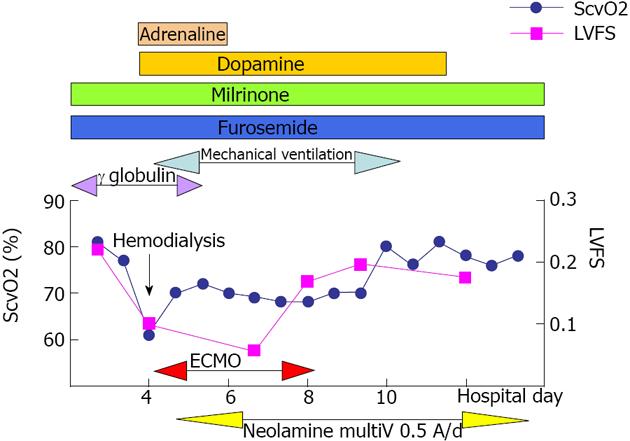
The patient was a 1-year-and-4-mo-old boy, with a height of 77 cm and a body weight of 11 kg. There was no particular history. He had had anorexia for about 1 wk before the consultation but showed no fever or cold-like symptoms. He started vomiting from 2 d before the consultation and was examined by a local doctor the next day, when he was suspected to have infectious enteritis and was prescribed an antiemetic. Since the symptoms were not alleviated, he was examined by the local doctor again, found to have cardiomegaly on a thoraco abdominal radiography, and transported to our hospital with suspected myocarditis. On admission, the body temperature was 36.8 °C, heart rate was 142/min, respiratory rate was 34/min, complexion was relatively poor, and vigor was reduced. The first and second heart sounds were both weakened, and the third heart sound or heart murmur was not heard. No hepatomegaly or splenomegaly was noted. Also, no clear generalized edema was noted. There was no clear abnormality in the sensory or motor nerves of the limbs. No decrease in the deep tendon reflex was noted. The blood test results on admission included: white blood cells: 10090/μL, C-reactive protein < 0.01, creatine kinase: 206/L, creatine kinase myoglobin band: 23/L, brain natriuretic peptied: 333 pg/mL, and rapid troponin T assay: positive (Table 1). Chest X-ray showed marked cardiomegaly with a cardio thoracic ratio of 66% (Figure 1). On electrocardiogram, negative T waves were noted in V2-V5. Echocardiography disclosed depressed left ventricular contractility with a fractional shortening of 17%, cardiomegaly, and moderate circumferential pericardial effusion. From the history, physical findings, and laboratory results, heart failure due to acute myocarditis was suspected, and the administration of a diuretic and γ-globulin was initiated. On the 4th hospital day, polypnea and a decreased level of consciousness were noted, and marked metabolic acidosis was indicated by blood gas analysis (room air: pH 7.275, pCO2: 7.5 mmHg, pO2: 131 mmHg, BE: -23.1 mEq/L, lactate: 114 mg/dL). After the initiation of hemodialysis, the patient lapsed into circulatory insufficiency, and catecholamine administration, endotracheal intubation, and extracorporeal membrane oxygenation (ECMO) became necessary. Initially, low-output heart failure due to acute myocarditis was suspected, but the central venous oxygen saturation was high at 82%. Despite circulatory insufficiency, the central venous oxygen saturation remained generally high during the course and showed no marked decrease (Figure 2). We considered high-output to be more likely than low-output heart failure and searched for its cause, but no clear abnormality was shown by various viral, endocrine function, or immunological tests. On urinary organic acid analysis, increases in the lactate and pyruvate levels, marked increases in the excretion of 3-OH-butyrate and acetoacetate, increases in metabolic products of branched-chain amino acids, and increases in 2-ketoglutarate, 2-OH-glutarate, 2-keto-adipate, and 2-OH-adipate were observed, and the vitamin B1 level was reduced to 12 ng/mL (normally 20-50 ng/mL). From these findings, a diagnosis of cardiac beriberi due to vitamin B1 deficiency was made. Careful inquiry with the patient’s family about his daily diet revealed that he had drunk about 1 L of an isotonic drink for infants daily from about 10 mo after birth. Central venous nutrition and the administration of vitamin preparations were initiated on the 5th hospital day, leading to marked improvements in the clinical condition. The patient was weaned from ECMO on the 8th hospital day, extubated on the 10th hospital day, and recovered with no sequela.
| WBC | 10090/μL | AST | 42 U/L |
| Neutro | 41.50% | ALT | 12 U/L |
| Lym | 43.60% | LDH | 399 U/L |
| Hb | 12.5 g/dL | CK | 206 U/L |
| Ht | 37.90% | CK-MB | 23 U/L |
| PLT | 726 × 103/μL | BUN | 5 mg/dL |
| Na | 134 mEq/L | Cr | 0.26 mg/dL |
| K | 4.2 mEq/L | CRP | < 0.01 mg/dL |
| Cl | 100 mEq/L | BNP | 333 pg/mL |
| Ca | 10.4 mg/dL | Rapid troponin T assay | Positive |
In children with unexplained heart failure, cardiac beriberi must be considered as a differential diagnosis of myocarditis and cardiomyopathy. In vitamin B1 deficiency, resistance vessels, particularly arterioles, are dilated due to metabolic acidosis. High-output heart failure is often observed due to increases in the peripheral vascular bed and venous return[3,4]. In adults, pulmonary artery catheterization or cardiac catheterization is performed for the differential diagnosis of heart failure, but such invasive procedures are often difficult to perform in children. The central venous oxygen saturation can be monitored continuously by placing a Pediasat™ catheter in the superior vena cava, and can be determined from the arterial oxygen saturation, hemoglobin level, cardiac output, and systemic oxygen saturation[5,6]. Since the balance of oxygen demand and supply in the body can be evaluated less invasively compared with pulmonary artery catheterization, the central venous oxygen saturation can be a useful index to differentially diagnose heart failure in children. In the case presented here, the central venous oxygen saturation showed no marked decrease and generally remained high despite heart failure, so we suspected high-output heart failure and, by searching for its cause, diagnosed the condition as cardiac beriberi.
In patients with cardiac beriberi, echocardiography has been reported to show right heart dilation by some[7] but no characteristic change by others[8], and the diagnosis of the condition by echocardiography alone is occasionally difficult. In our patient, echocardiography showed no clear right heart dilation and yielded no significant finding suggestive of cardiac beriberi, but the high central venous oxygen saturation was useful for the diagnosis. Despite high-output heart failure, the central venous oxygen saturation decreased for about 1 wk from hospital days 2-3, which may have been partly because venous return was impaired due to pericardial effusion, and the right atrial pressure increased, reducing the left ventricular contraction function[9]. With improvements in the hemodynamics after vitamin B1 administration, the central venous oxygen saturation increased.
Cardiac beriberi is a serious disease with a rapid onset and course and causes lactic acidosis and cardiogenic shock but is clinically characterized by prompt resolution by the administration of a vitamin preparation[7]. After early treatment, high-output cardiac failure rapidly improves. However, a rapid increase in systemic vascular resistance and a decrease in left ventricular contraction due to afterload mismatch occur during the course, requiring cardiotonic or diuretic administration. In this patient, milrinone and a diuretic were used during the course.
Concerning hemodynamics associated with beriberi, a marked decrease in the diagnostic pressure and an increase in cardiac output are well known. It may be difficult to diagnose as it may be accompanied by low-output[10] and not necessarily by high-output heart failure. Since the prognosis is favorable with early diagnosis and treatment, it is important to suspect the condition first by comprehensively evaluating indices including the history, echocardiography findings, and central venous oxygen saturation. Although beriberi is a rare disease today, it is necessary to remember that it may still be caused by an unbalanced diet.
In conclusion, when unexplained heart failure is observed in children, cardiac beriberi must be excluded as a differential diagnosis of myocarditis and cardiomyopathy. The measurement of the central venous oxygen saturation may be useful for the diagnosis.
P- Reviewers Durandy Y, Said S, Shen XC S- Editor Gou SX L- Editor A E- Editor Liu XM
| 1. | Fujita I, Sata T, Gondo K, Fukazawa M, Kukita J, Zaitsu A, Yoshitake J, Ueda K. Cardiac beriberi (shoshin beriberi) caused by excessive intake of isotonic drink. Acta Paediatr Jpn. 1992;34:466-468. [PubMed] [Cited in This Article: ] |
| 2. | Kawano H, Hayashi T, Koide Y, Toda G, Yano K. Histopathological changes of biopsied myocardium in Shoshin beriberi. Int Heart J. 2005;46:751-759. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 13] [Cited by in F6Publishing: 13] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 3. | Coelho LS, Hueb JC, Minicucci MF, Azevedo PS, Paiva SA, Zornoff LA. Thiamin deficiency as a cause of reversible cor pulmonale. Arq Bras Cardiol. 2008;91:e7-e9. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 13] [Cited by in F6Publishing: 15] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 4. | Motherway C. Acute pernicious (sho-shin) beri-beri: a report of three cases. Crit Care Resusc. 1999;1:69-73. [PubMed] [Cited in This Article: ] |
| 5. | Ranucci M, Isgrò G, De La Torre T, Romitti F, De Benedetti D, Carlucci C, Kandil H, Ballotta A. Continuous monitoring of central venous oxygen saturation (Pediasat) in pediatric patients undergoing cardiac surgery: a validation study of a new technology. J Cardiothorac Vasc Anesth. 2008;22:847-852. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 22] [Cited by in F6Publishing: 22] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 6. | Liakopoulos OJ, Ho JK, Yezbick A, Sanchez E, Naddell C, Buckberg GD, Crowley R, Mahajan A. An experimental and clinical evaluation of a novel central venous catheter with integrated oximetry for pediatric patients undergoing cardiac surgery. Anesth Analg. 2007;105:1598-1604, table of contents. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 20] [Cited by in F6Publishing: 21] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 7. | Sangtawesin C, Leartveravat S. Pediatric cardiac beriberi: 3 different presentations. J Med Assoc Thai. 2008;91 Suppl 3:S165-S168. [PubMed] [Cited in This Article: ] |
| 8. | Meurin P. [Shoshin beriberi. A rapidly curable hemodynamic disaster]. Presse Med. 1996;25:1115-1118. [PubMed] [Cited in This Article: ] |
| 9. | Araki T, Saitou M, Nakashima A, Takimoto H, Tofuku Y. A case of beriberi heart disease associated with high cardiac output state masked by pericardial effusion. Heart. 1996;28:935-941. [Cited in This Article: ] |
| 10. | López Gastón OD, Malvino ER, McLoughlin D, Osatnik J, Chávez Zambrano MA, Pino C. [Acute cardiovascular beriberi (shoshin-beriberi)]. Medicina (B Aires). 2002;62:331-334. [PubMed] [Cited in This Article: ] |