Digital health is a cultural transformation of traditional healthcare
Introduction
A new phenomenon we call “digital health”, and define as “the cultural transformation of how disruptive technologies that provide digital and objective data accessible to both caregivers and patients leads to an equal level doctor-patient relationship with shared decision-making and the democratization of care”, initiated changes in providing care and practicing medicine. As technological innovations become inseparable from healthcare and as healthcare systems worldwide are becoming financially unsustainable, a paradigm shift is imminent.
Since the dawn of medicine, physicians have tried to make informed decisions with a very limited set of tools and a growing amount of experience that could be transmitted to the next generation. Even in the case of the first stethoscope, a hollow wooden tube introduced by Dr. Laennec in France in the early 19th century (1), it took decades to spread the idea of improving care with an innovation. Since then, healthcare has become dependent on technologies but neither the medical curriculum nor the policies and guidelines behind care reflected upon this development (2).
By the 2010s, the digitalization of healthcare became inevitable, the amount of medical knowledge continued to grow rapidly (3); and patients started to become empowered while stakeholders were not prepared (4). Physicians burn out easily under the burden of bearing with all the responsibility (5); patients become frustrated by looking for solutions in a mess of information and decision makers hesitate to change the system.
Digital health has made a range of technologies from genome sequencing to smartphone connected ECG readily available (Table 1), although it also carries the risk of dehumanizing care. The authors of this paper argue that the use of technology only leads to better health outcomes if the related cultural challenges are acknowledged and the new needs of patients are met. This way, disruptive innovations such as deep learning algorithms, virtual reality (VR), or health sensors could contribute to value-based healthcare, and help make human skills from clinical judgement and experience to creative problem-solving determine the success of intervention and the doctor-patient relationship. As digital health makes patients the point-of-care, a new status quo and new roles for both patients and caregivers are approaching.
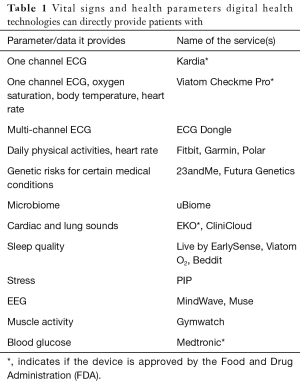
Full table
Behind the transformation
In the 19th century, practicing medicine became a profession based on natural sciences that required specific knowledge and experience, which only a handful of experts possessed. An implicit contract between the medical profession and society included provision of the financial background from the state and respect of the profession’s autonomy; while professionals guarded people’s health (6-8). Partially because of financial reasons and because of the rise of technologies giving power to patients, a new contract is timely. In that, the roles of stakeholders, their individual responsibility, their rights and transparency should be defined and clearly described.
In the 21st century, the number of patients with chronic conditions and the costs of providing modern treatments are rising, life expectancy is getting higher and the World Health Organization estimates that there is a worldwide shortage of around 4.3 million health workers in the world (9). At the same time, technology advances with an unprecedented pace. A hardware and software revolution is taking place in healthcare.
Regarding hardware, internet access, mobile phone and smartphone penetration has been increasing. Medical technologies such as artificial narrow intelligence, robotics, genomics, telemedicine, virtual and augmented reality are becoming disruptive. Regarding the software/information component, an enormous amount of medical information, peer support and open access clinical studies and guidelines are becoming widely available. It does not only lead to potentially better quality and a larger quantity of information being obtained in healthcare but also to the opportunity for self-care (10).
Another changing aspect is the shift of the human side of medicine. In the traditional settings of healthcare, patients were not involved in decision making about their own health and disease management. Medical professionals had to take the burden and all the responsibility concerning medical decisions and consequences. Patients have been completely dependent on the processes, infrastructure, information and decisions of healthcare providers and systems. This insecurity and exposure to decisions out of their control served as the primary motivation behind patient empowerment that included the use of disruptive technologies, which were also becoming available.
Dr. Tom Ferguson coined the term e-patient (11) and its awareness started to rise around 2009 (12). Empowered patients see themselves as equal, engaged and they want to take active part in making decisions about their care. They ask for second opinion and involve other caregivers and fellow patients in gathering information, making decisions and determining the impact of treatment on their lives (13).
The patriarchal hierarchy of traditional medicine has been disrupted by empowered patients who have previously unmet needs. They expect their caregivers to answer their medical and technology-related questions. The importance of patients’ right and willingness to self-determination, getting more access to information and technologies, the choice or even the rejection of treatment have been increasing. E-patients do not want to completely depend on others’ decisions. In such a world, the so-called ivory tower of medicine becomes unsustainable.
The new status quo
The evolution of medicine in recent decades, where patients are treated like products and fragmented specialists are providing care, might be best described as “clinical factories”. The paternalistic model of the doctor-patient relationship has begun to be replaced by shared decision making in the second half of the 20th century (Figure 1, Table 2).
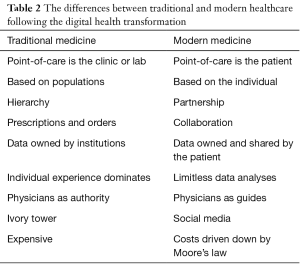
Full table
One of the core reasons behind this change was the increasing dominancy of chronic diseases: successfully curing and managing them depend on a cooperation between physicians and patients, which can span decades. Parallel to this, informed consent became the most important bioethical principle (14), which stresses the therapeutic decision making, assuming an equal, partner-like relationship and genuine communication. Another reason might be due to the technological possibilities: besides shared decision making, the active participation in treatment and the monitoring of their own physical state with sensors at home, are undeniable.
Physicians are transforming into guides for their patients in the jungle of healthcare information and technologies from being an authority, from being the one who makes all the decisions (15). As they still have the expertise and a lot of experience, they remain crucial elements in the status quo. However, instead of being the gate keepers to the ivory tower, they become collaborators in the patient’s journey in healthcare.
Such technological transitions have taken place in healthcare before but could never lead to a meaningful and cultural transformation of the status quo. When personal computers became widely available in the 1990s, e-health emerged (16). When such computers could be connected into networks, telemedical services appeared (17). The rise of social media networks gave space to medicine 2.0 and health 2.0 (18); while penetration of mobile phones and later smartphones summoned mobile health (19). But from the 2010s, the rate at which disruptive technologies appear is becoming overwhelming for both the patients and their caregivers.
Policy makers globally face the challenge of keeping up with the fast pace of innovations; innovators find it hard to integrate their solutions into the over-regulated healthcare systems. This process is disturbed by patients’ and caregivers’ reluctance to change (20). To make digital health fill the gaps and function properly, we need to build knowledge and attitude. Thus, one of the crucial tasks of the stakeholders of healthcare is to assist both patients and caregivers in implementing digital health into everyday medicine. This will only succeed if we lay down the basics of using digital health in care, which requires a fundamental change in study design too.
Digital health is a paradigm shift
In his book, The Structure of Scientific Revolutions, Thomas Kuhn described how paradigm shifts occur in science. Although healthcare and medicine are fundamentally different from physical sciences, the principle of how the sociological transition takes place is universal. He mentioned that “perhaps science does not develop by the accumulation of individual discoveries and inventions”, but that discovery commences with the awareness of anomaly, i.e., with the recognition that nature has somehow violated the paradigm-induced expectations that govern normal science” (21).
Giving a certain disruptive technology alone to a patient has not improved health outcomes. We argue that digital health represents this transformation but most medical studies dedicated to the issue have focused on the technological instead of the human component. For instance, studies that aimed at incorporating health sensors to drive behavior change for patients, did not take into consideration the importance of providing coaching with the technology.
There have been studies focusing on whether a web-based intervention or monitoring service could help manage medical conditions better, like the measuring of quantified parameters such as hemoglobin A1c levels or blood pressure. There were no significant improvements in those parameters when patients received access to a web portal without prior training (22-24); or when participants had trouble with the registration process and using tools designed to allow them to track their health and self-report health information indicating that complex portal interfaces may present a barrier to use (25).
However, where coaching was an equal element to the use of technologies in the study design, the use of disruptive technologies such as VR devices led to quantifiable, significant changes. Patients who could experience VR worlds for up to 20 minutes through wearing a headset and chose to travel to Iceland, participated in the work of an art studio or swam with whales in the ocean described the experience as pleasant and capable of reducing pain and anxiety (26).
Another study included patients suffering from gastrointestinal, cardiac, neurological, and post-surgical pain. Half of them watched a 15-minute nature video accompanied by calming music; while the other group wore VR goggles to watch a 15-minute animated game called Pain RelieVR, which was specifically designed to treat patients who have to stay in bed or have limited mobility. Use of VR in hospitalized patients significantly reduced pain versus a controlled distraction condition. These results indicate that VR is an effective and safe adjunctive therapy for pain management in the acute inpatient setting (27).
Research has shown that consistent use of continuous positive airway pressure therapy for patients with sleep apnea is associated with improved health outcomes. Importantly, giving feedback to patients improved their utilization of the treatment. Patients who had access to their data and sleep quality results on a smartphone app (myAir), used the device on average 46 minutes longer every night compared to other patients; and had higher adherence than other patients, 81% compared to 68% at week 8 (28). This illustrates that it’s ineffective to simply say “Patients should just follow doctors’ orders”. It’s more effective to give them feedback on how well their efforts are working.
The challenging questions digital health raises
With the advantages and the changing status quo, digital health leads to some ethical considerations and challenges policy makers in an unprecedented way. With the disappearance of the ivory tower, misinterpreted information obtained from digital health devices and unreliable online resources can lead to medical decisions that do not involve medical professionals and endanger the lives of patients (29).
In addition, with devices that make data accessible to both stakeholders and patients, unauthorized third parties might acquire sensitive information about patients’ health. Medical devices were shown to be hacked from a distance (30). Laws, such as the Genetic Non-Discrimination Act in the United States, are expected to defend patients from their employers and/or insurers gathering data from their direct-to-consumer genetic testing results, and might lead to disadvantages.
The lack of access to care and diminishing trust towards the healthcare system can make patients turning to inefficient therapies and online medical quackery (31). The same can happen with digital health tools, if physicians are not involved as expert partners in the process.
Also, more emphasis is needed on the validation of health sensors (32), other digital health devices and smartphone applications (33) to provide quality, reliable information to users. Comparing their accuracy to well-documented technologies is a good starting point, but double-blind studies involving large patient cohorts are also needed.
The reluctance and the lack of incentives from physicians to go through this cultural transformation make patients the leading driving force in initiating these changes. As they are not encouraged to ask their caregivers for guidance in technological questions, they increasingly turn to technological solutions as their only option. Patients with diabetes started a movement called #WeAreNotWaiting that led to a DIY artificial pancreas systems developed at home without regulatory oversight (34). This shows the lack of capability and capacity of regulatory agencies in integrating innovations into care fast enough. It also shows how in some cases patients might not need medical expertise: they may be able to self-manage, entirely on their own.
As a long-term effect of digital health, individual entrepreneurship skills should not define a patient’s health outcomes. There are examples for patients with oncological diagnoses to use crowdfunding websites for covering their healthcare costs (35). There is also an example of a patient with a deformed limb to offer advertising space on his prosthetic device (36). Digital health technologies, without the proper implementation, give rise to such efforts too.
Despite the use of digital technologies, the development of health status is also dependent on health literacy. Those with lower health literacy levels are generally in a worse state of health, visit the doctor more often, use fewer prevention techniques and on the whole, are more costly for the healthcare system (37). A 2013 WHO report revealed that health literacy is a stronger predictor of the formation of the state of health than income, education or belonging to various ethnic groups (38).
The European health literacy survey (HLS-EU) found that every second person possesses limited health literacy (39). Also, patients with lower health literacy rates are more unlikely to use the possibilities of eHealth (40). The technological boom makes it unambiguous that digital health literacy has a wider aspect than the notion of classic health literacy. Digital health adds the requirement to be technically literate about computers and media. We are standing before an enormous challenge: will technological transformation improve health literacy levels, or the contrary: will digital health deepen the already existing digital divide?
The answer might lie in design thinking to improve health literacy. A company, Mucca Design re-invented blood test results in a way that they changed the basic list of results to a colorful and easily digestible infographic (41). Text4Wellness and Mobilize4Fitness are mobile services that provide texts with health and wellness tips, reminders to exercise, inspirational quotes and information about health and wellness activities geared toward African-American women in the United States. It uses a convenient communication method and familiar language (42). The Maxillofacial Department at Radboud University in the Netherlands invited patients to help design new care facilities for them in order to improve patient satisfaction (43).
The future of digital health
Medical professionals and policy makers have a huge responsibility in involving patients as partners in designing care and decision making; and guiding them in using the myriad of digital health technologies. Otherwise, patients may either turn to non-proven services or technological solutions they might not be able to interpret alone.
By sharing responsibility, physicians could also share the burden of choosing the right therapy and bearing the consequences. Disruptive innovations also have the potentials of taking away the repetitive parts of their job, letting them spend more time with and dedicate their focus to the patient. Those skills that are hard to replace such as empathy, social care and the human touch could be the essence of providing care.
Using digital health is a teamwork, thus the era of lonely doctor heroes will end. The success of providing care depends on collaboration, empathy and shared decision making. What is needed for this is a newly defined co-operation between patients and their caregivers. The well-functioning patient-physician relationship is still an essential part of healing: a decisive study revealed that the empathy skills of physicians can influence diabetic patients’ objective laboratory parameters, development of complications and subjective well-being (44).
New approaches must be applied in modern medical education including post-graduate education to teach students skills that facilitate their job and prepare caregivers for working with technologies. We have already shown that a well-designed course, improved by constant evaluation-based feedback, can be suitable for preparing students for the massive use of the Internet, social media platforms, and digital technologies (45).
This implies a regulatory framework that understands how technological innovations work and what their weaknesses are to prevent sensitive information from leaking to unauthorized third parties and protect the patient’s privacy. Promising examples include the Patient Engagement Advisory Board, which the FDA launched and the 3D printing workshops, which the FDA organized (46).
The role of patients also needs to shift from being a passive stakeholder of care to becoming proactive with tools and information at their disposal to perform health and disease management. E-patient movements and advocacy have been assisting this transition (47,48).
Today’s generation grows up on using technologies, some of them becoming so-called “digital natives” (49). For them, it is inevitable that they turn to digital solutions when facing medical issues. If we are not able to properly and safely integrate digital health into healthcare today, we will soon pose a threat to their health.
Based on Kuhn’s theory, science progresses through a series of paradigm shifts where a new paradigm contradicts the old one, creates tensions between the stakeholders and gradually becomes the dominant model. We aimed at raising awareness about the importance of the current shift known as digital health that changes the status quo, the delivery of care and the practice of medicine. We attempted to demonstrate that digital health is not only a technological but a cultural transformation in which, besides many others, definition of the new roles is taking place today.
Acknowledgements
We are grateful to Dave deBronkart for his suggestions, comments and guidance.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Cheng TO. How Laënnec invented the stethoscope. Int J Cardiol 2007;118:281-5. [Crossref] [PubMed]
- Topol E. The Creative Destruction of Medicine: How the Digital Revolution Will Create Better Health Care. Basic Books, 2013.
- Druss BG, Marcus SC. Growth and decentralization of the medical literature: implications for evidence-based medicine. J Med Libr Assoc 2005;93:499-501. [PubMed]
- Barham V, Devlin RA, Wang X. Empowered patient or empowered physician: an analysis of the importance of the empowered patient in the health delivery system. Cah Sociol Demogr Med 2008;48:9-39. [PubMed]
- Engstrom PF. Physician burnout. J Natl Compr Canc Netw 2013;11:502-4. [Crossref] [PubMed]
- Irvine D. The changing relationship between the public and the medical profession. J R Soc Med 2001;94:162-69. [PubMed]
- Cruess RL, Cruess SR, Johnston SE. Professionalism: an ideal to be sustained. Lancet 2000;356:156-9. [Crossref] [PubMed]
- Armstrong D. Medicine as a profession: times of change. BMJ 1990;301:691-3. [Crossref] [PubMed]
- Aluttis C, Bishaw T, Frank MW. The workforce for health in a globalized context - global shortages and international migration. Glob Health Action 2014;7:23611. [Crossref]
- Lupton D. The digitally engaged patient: Self-monitoring and self-care in the digital health era. Soc Theory Heal 2013;11:256-70. [Crossref]
- Ferguson T. Doc Tom. Available online: http://www.doctom.com/
- Fox S. The Engaged E-patient Population. Pew Internet Am Life Proj 2008:1-4.
- Jadad AR, Rizo CA, Enkin MW, et al. I am a good patient, believe it or not. BMJ 2003;326:1293-5. [Crossref] [PubMed]
- Grady C. Enduring and emerging challenges of informed consent. N Engl J Med 2015;372:855-62. [Crossref] [PubMed]
- TEDxMaastricht - Bas Bloem - “From God to Guide”. 2011. Available online: https://www.youtube.com/watch?v=LnDWt10Maf8
- Eysenbach G. What is e-health? J Med Internet Res 2001;3:E20. [Crossref] [PubMed]
- Perednia DA. Telemedicine Technology and Clinical Applications. JAMA 1995;273:483. [Crossref] [PubMed]
- Van De Belt TH, Engelen LJ, Berben SA, et al. Definition of Health 2.0 and Medicine 2.0: a systematic review. J Med Internet Res 2010;12:e18. [Crossref] [PubMed]
- Steinhubl SR, Muse ED, Topol EJ. Can mobile health technologies transform health care? JAMA 2013;310:2395-6. [Crossref] [PubMed]
- Ayers DJ, Menachemi N, Ramamonjiarivelo Z, et al. Adoption of electronic medical records: the role of network effects. J Prod Brand Manag 2009;18:127-35. [Crossref]
- Kuhn TS. The structure of scientific revolutions, Vol. 57. Chicago: The University of Chicago, 1996:59-75.
- Grant RW, Wald JS, Schnipper JL, et al. Practice-linked online personal health records for type 2 diabetes mellitus: a randomized controlled trial. Arch Intern Med 2008;168:1776-82. [Crossref] [PubMed]
- Wagner PJ, Dias J, Howard S, et al. Personal health records and hypertension control: a randomized trial. J Am Med Inform Assoc 2012;19:626-34. [Crossref] [PubMed]
- Tuil WS, Verhaak CM, Braat DD, et al. Empowering patients undergoing in vitro fertilization by providing Internet access to medical data. Fertil Steril 2007;88:361-8. [Crossref] [PubMed]
- Haggstrom DA, Saleem JJ, Russ AL, et al. Lessons learned from usability testing of the VA’s personal health record. J Am Med Inform Assoc 2011;18:i13-7. [Crossref] [PubMed]
- Keefe FJ, Huling DA, Coggins MJ, et al. Virtual reality for persistent pain: A new direction for behavioral pain management. Pain 2012;153:2163-6. [Crossref] [PubMed]
- Mosadeghi S, Reid MW, Martinez B, et al. Feasibility of an Immersive Virtual Reality Intervention for Hospitalized Patients: An Observational Cohort Study. JMIR Ment Health 2016;3:e28. [Crossref] [PubMed]
- pwc. Empowering the sleep apnea patient. How online patient engagement tools improve adherence to treatment. Available online: http://www.resmed.com/epn/content/dam/resmed/global/documents/epn/pwc-report-effects-of-myair-6.pdf
- Fahy E, Hardikar R, Fox A, et al. Quality of patient health information on the internet: Reviewing a complex and evolving landscape. Australas Med J 2014;7:24-8. [Crossref] [PubMed]
- Marks P. Hacked to death. New Scientist 2014;224:19.
- Ernst E. Rise in popularity of complementary and alternative medicine: reasons and consequences for vaccination. Vaccine 2001;20 Suppl 1:S90-3; discussion S89.
- Hekler EB, Buman MP, Grieco L, et al. Validation of physical activity tracking via Android smartphones compared to ActiGraph accelerometer: Laboratory-based and free-living validation studies. JMIR mHealth uHealth 2015;3:e36. [Crossref] [PubMed]
- Plante TB, Urrea B, MacFarlane ZT, et al. Validation of the Instant Blood Pressure Smartphone App. JAMA Intern Med 2016;176:700-2. [Crossref] [PubMed]
- Lewis D, Leibrand S. Real-World Use of Open Source Artificial Pancreas Systems. J Diabetes Sci Technol 2016;10:1411. [Crossref] [PubMed]
- Telegraph Reporters. Record numbers of cancer patients using crowdfunding to pay for private treatment not available on NHS. Telegraph 2017. Available online: http://www.telegraph.co.uk/news/2017/02/04/record-numbers-cancer-patients-using-crowdfunding-pay-private/
- F1 fan receives bionic hand from Mercedes team. Telegraph 2011; Available online: http://www.telegraph.co.uk/sport/motorsport/8700621/F1-fan-receives-bionic-hand-from-Mercedes-team.html
- The European Health Literacy Project 2009-2012. Available online: https://docs.wixstatic.com/ugd/76600e_4899bb3c9c8e4a8db213d60e3a2de16f.pdf
- World Health Organization. Health Literacy [Internet]. 2013. Available online: http://www.euro.who.int/__data/assets/pdf_file/0008/190655/e96854.pdf
- Sørensen K, Pelikan JM, Rothlin F, et al. Health literacy in Europe: comparative results of the European health literacy survey (HLS-EU). Eur J Public Health 2015;25:1053-8. [Crossref] [PubMed]
- Mackert M, Mabry-Flynn A, Champlin S, et al. Health literacy and health information technology adoption: The potential for a new digital divide. J Med Internet Res 2016;18:e264. [Crossref] [PubMed]
- Leckart S. The Blood Test Gets a Makeover. Wired 2010. Available online: https://www.wired.com/2010/11/ff_bloodwork/
- Katz S. Combine design thinking and digital health to provide for the underserved. Techcrunch 2016; Available online: https://techcrunch.com/2016/07/21/combine-design-thinking-and-digital-health-to-provide-for-the-underserved/
- Mesko B. Peek into the Future of Hospitals: Smart Design, Technologies and Our Homes. The Medical Futurist 2017. Available online: http://medicalfuturist.com/peek-into-the-future-of-hospitals/
- Del Canale S, Louis DZ, Maio V, et al. The Relationship Between Physician Empathy and Disease Complications. Acad Med 2012;87:1243-9. [Crossref] [PubMed]
- Mesko B, Győrffy Z, Kollár J. Digital Literacy in the Medical Curriculum: A Course With Social Media Tools and Gamification. JMIR Med Educ 2015;1:e6. [Crossref] [PubMed]
- FDA. Patient Engagement Advisory Committee. Available online: https://www.fda.gov/advisorycommittees/committeesmeetingmaterials/patientengagementadvisorycommittee/default.htm
- Prainsack B. The Powers of Participatory Medicine. PLoS Biol 2014;12:e1001837. [Crossref] [PubMed]
- deBronkart D. How the e-patient community helped save my life: an essay by Dave deBronkart. BMJ 2013;346:f1990. [Crossref] [PubMed]
- Prensky MH. Sapiens Digital: From Digital Immigrants and Digital Natives to Digital Wisdom Digital Wisdom. Journal of Online Education 2009;5:1-9.
Cite this article as: Meskó B, Drobni Z, Bényei É, Gergely B, Győrffy Z. Digital health is a cultural transformation of traditional healthcare. mHealth 2017;3:38.



