Increased low back pain prevalence in females than in males after menopause age: evidences based on synthetic literature review
Introduction
Low back pain (LBP) is usually defined as pain, muscle tension, or stiffness localized below the costal margin and above the inferior gluteal folds, with or without leg pain (sciatica). LBP occurs in about 60–80% of people at some points in their lives, and can begin in childhood (1-7). It is a disorder with many possible etiologies, with many definitions, and occurring in many groups of populations. The vast literature available on prevalence of LBP is not only heterogeneous, but also sometimes contradictory. This variability may be due to differences among study factors such as the age of the sample, the definition of LBP, and the strategy for extracting data. The prevalence can be described in terms such as point prevalence (the number of persons in a defined population who have LBP at a particular point in time, usually the time the survey was carried out), period prevalence (the number of persons who have LBP at any time during a specified time interval), and lifetime prevalence (the number of persons who have LBP at some points in their life). LBP has also been shown to be associated with certain psychosocial factors, including presence of psychological conditions, maladaptive coping strategies, poor job satisfaction, higher physical work demands, poor general health or functional level, tobacco use, obesity, receipt of workers’ compensation or disability/sick leave, and unresolved litigation or compensation issues related to the back pain (8-10). There may be also cultural differences in the pain perception or reporting, with some ethnic minorities having the attitude that pain is to be endured without complaint (8,11).
The overall prevalence of LBP is higher in women than in men (12,13). Women are also affected by many chronic pain conditions and painful conditions of the musculoskeletal system in greater numbers than men are (14). A biopsychosocial model of chronic pain attributes sex differences in pain to interactions between biological, psychological, and sociocultural factors (15,16). The heightened pain sensitivity among women can also partially explain greater reports of pain by women compared to men (17,18). Menstrual cycle fluctuations in pain sensitivity may help to explain sex differences in pain reporting in younger adults (19). Biologic response to pregnancy and childbearing, physical stress of child-rearing, perimenopausal abdominal weight gain are additional causes for LBP (12). Population-based studies have shown that the prevalence of widespread pain increases with age, peaking in the seventh and eighth decades (20,21). Recently, it has been show that genetics also played a role in the development of LBP (1,22,23).
Lumbar disc degeneration and its associated changes such as disc space narrowing are related to LBP (24). Lumbar disc degeneration is a common musculoskeletal condition, the prevalence of which increases with age (25-29). Disc degeneration can progress to disk herniation, spinal canal stenosis, and, in conjunction with facet joint arthrosis, degenerative spondylolisthesis. In an analysis of published data of 600 autopsy specimens of young and middle-aged subjects younger than 50 years, intervertebral disc degeneration was observed in men in the second decade of life, occurring at an earlier age than in women; the severity of age matched disk degeneration was also being generally greater in men (25). In a later independent histologic study, Łebkowski (26) investigated 308 lumbar intervertebral discs at autopsy from 57 women (mean age, 41.8 years) and 79 men (mean age, 42.1 years). Disc degeneration became first readily apparent during the 2nd decade of life, though it was observed to occur in men almost a decade earlier than in women. In a MR imaging-based survey of young adults 20–22 years, lumbar disc degeneration was significantly more frequent in men (30). These results confirm the general perception that young men are more susceptible to disc degeneration than young women are, most likely due to increased mechanical stress and physical injury. However, after menopause which is around the age of 49–50 years, lumbar discs in females degenerate at a notably quicker rate than male lumbar discs in males, after later 50s, disc space narrowing become more apparent and more severe than age matched males (31-33).
Based on these backgrounds, we propose a hypothesis, i.e., while overall females have higher prevalence of LBP across all age groups, this male vs. female difference in LBP prevalence further increases after female menopause age. This is partially related to the accelerated lumbar disc degeneration and spine degeneration after female menopause (31-33). In this study we performed a literature review to look at whether this male vs. female difference in LBP prevalence exaggerated after female menopause age can be demonstrated.
Materials and methods
The literature search was performed on PubMed on January 2, 2016. The search word combination was (low back pain) AND prevalence AND [(males OR men) AND (females OR women)]. This search generated 2,897 paper titles. The titles and abstracts of these papers, and sometimes full papers when required, were screened, and the following criteria were used to include the papers for further synthetic analysis:
- Only English literatures on LBP were further analyzed. Review and meta-analysis articles were excluded.
- We only included prospective studies on general population of both males and female subjects studied using the same LBP criterion, ages-specific information available, and males and female subjects were age-matched. Patient-only studies, which tended to be retrospective, were excluded, as results from clinical groups are likely to be biased (4). The decision to seek medical care would be dependent on: (i) predisposition of the individual to use services, which is based on demographic and social characteristics as well as attitudes about medical care and efficacy of treatment; (ii) ability to obtain medical services; and (iii) subjective perception of severity of illness.
- Literatures with focus on LBP of occupational causes, such as industrial workers, drivers, athletes, were excluded. Occupational populations represent a selective group of individuals. In general, workers tend to be healthier, and state of health itself may determine entry into a specific occupation. Rates of back pain among occupational groups may differ because of not only the work itself but also because of differential selection into various occupations. However, studies on teachers of general subjects and farmers were included. Studies on teachers were usually of convenience samples, and they are likely not to have specific occupational causes for LBP. Studies on farmers were usually of large sample size, and in many societies farmers constitute a very large portion of the society members. It is known in some societies females can be more involved in household work, in this study house wife were not excluded.
- The included studies were judged to have no major flaws. The characteristics of the population adequate, the sample size and response rate adequate.
- When a study applied a longitudinal design, only the prevalence rate at end of the study was recorded, or the prevalence rate which was judged to be most relevant was used for analysis.
- Regional and ethics factors were not considered in this study.
Results
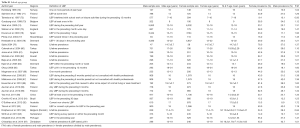
This study extracted 98 studies from PubMed for synthetic analysis, involved 772,927 participant subjects (Tables S1-S4). According to the information in the literature, participant subjects were divided into four age groups: (I) school age children group: 6–19 years; (II) young and middle age group: 20–50 years; (III) mixed age group: data from studies did not differentiate age groups; (IV) elderly group: ≥50 years old. When individual studies were not weighted by participant number and each individual study is represented as one entry regardless of their sample size, the median LBP prevalence ratio of female vs. males was 1.310, 1.140, 1.220, and 1.270 respectively for the four age groups (Figure 1). When individual studies were weighted by participant number, the LBP prevalence ratio of female vs. males was 1.360, 1.127, 1.185 and 1.280 respectively for the four groups (Figure 2).
Full table
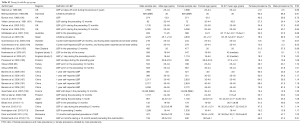
Full table
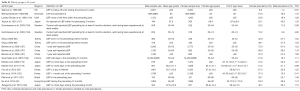
Full table
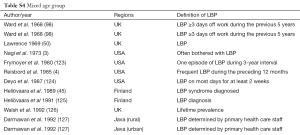
Full table
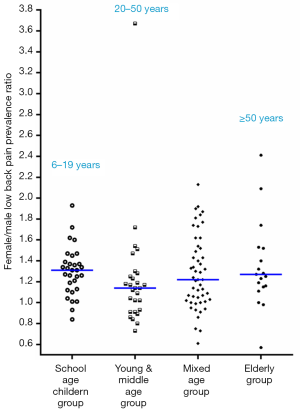
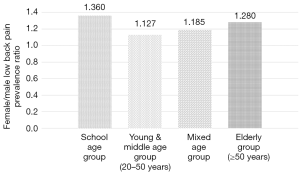
This study demonstrated females had higher prevalence of LBP across all age groups. The female vs. males LBP prevalence ratio was highest for school age girls and boys. Compared with middle aged subjects, a further increased low back pain prevalence in females than in males was noted after menopause age.
Discussion
Among all chronic pain problems and spinal pain conditions, LBP is the most common and important clinical, social, economic, and public health problem affecting the population indiscriminately across the world (8). LBP is known to be of multi-factorial causes (3,34,35). Employment and workplace factors, both physical and psychological, such as heavy lifting, pushing, pulling, vehicle driving, and prolonged walking or standing were found to be predictors of LBP and there are similar associations with stressful and monotonous work and dissatisfaction with work. Body mass index has been found to be linked to LBP in obese people (36). Associations between LBP and social class, low levels of educational and low income have been reported. Persons with greater education are more likely to be in professional, managerial, or other skilled occupations where there is more flexibility to eliminate pain-provoking job situations and physical demand (4,37). Compared with a lower or a higher frequency of exercise, a moderate frequency of exercise from one to five times a week was associated with a lower LBP risk level (4). LBP has been reported consistently in a higher proportion of females than males (3,4,12,13,38,39). Our synthetic analysis further confirmed this phenomenon. Gender prevalence ratios also revealed a higher prevalence of pain in females for headache, migraine, temporomandibular pain, burning mouth pain, neck pain, shoulder pain, back pain, knee pain, abdominal pain, and fibromyalgia (8). Women have shown to have a lower threshold of perception of pain and in reaction to it (40,41). Several authors have observed that although females are more likely to report symptoms, physician verified abnormalities are approximately equal to those of males (42,43). However, occupational LBP is seen in higher proportions in men (44,45).
Some data suggested LBP prevalence increased in the recent years (8,46). It could be that the actual prevalence has not changed but the reporting has; or it could be that the questions used to assess the prevalence have changed; or LBP prevalence really increased due to life style changes of the population. Harkness et al. showed there were significant differences in the prevalence of pain increasing from 2- to 4-fold between two surveys (47). Chronic pain is a common symptom and significant problem for older adults. Epidemiologic data in the elderly suggests that up to 50% of community-dwelling older adults and as many as 80% of residents of long-term care facilities experience persistent pain. Bressler et al. (48) undertook a systematic review of the literature from 1966 through 1998 and reported that persons over 65 years of age experience low back pain with greater frequency and have been under-represented in research, as well as in management. Further, age related prevalence of persistent pain appears to be much more common in the elderly associated with functional limitations and difficulty in performing daily life activities. In an evaluation of pain characteristics of adults 65 years of age and older referred to a tertiary pain care clinic, the older patients had relatively more physical problems concordant with their complaints, but fewer psychological factors contributing to disability than the younger pain patients (49). On the other hand, we expect the higher LBP prevalence in school age girls than in school aged boys is more likely due to psychological factors, female hormone fluctuation, and menstruation.
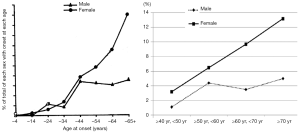
That post menopausal women has higher incidence of LBP than men has been reported distinctively in a number of studies. In 1969 Lawrence (50) surveyed 713 males and 809 females aged ≥35 years with lumbar radiograph in Manchester, UK. Back-hip-sciatic pain was present at the time of the survey in 79 (11%) of the males and in 153 (19%) of the 809 females. In those with pain at the time of the survey the incidence had raised till age 40 in males and then remained constant, but in females it continued to rise sharply up to and over the age of 65 (Figure S1A). Nagi et al. (3) in 1973 showed a greater proportion of females (21%) reported back pain as compared to males (14%). It was suggested a number of women might have experienced back pain in connection with the biological processes associated with the menses. However, when age controls were introduced, Nagi et al. noted that women over 50 years of age were more likely than men to report back pain (26% and 17%, respectively). In 1995, Papageorgiou et al. (51) reported the South Manchester Back Pain Survey with study population of 4,501 (age: 18–75 years old). The 1-month period prevalence of LBP was 31.2%, 33.1%, 38.5%, 34.9% for the age range of 18–29, 30–44, 45–59, and ≥60 years respectively for males; 32.2%, 41.5%, 49.2%, 43.7% for the age range of 18–29, 30–44, 45–59, and ≥60 years respectively for females. In our own Osteoporotic Fractures in Men (Hong Kong) and Osteoporotic Fractures in Women (Hong Kong) Studies data published in 2013 (52). A total of 2,000 Chinese men and 2,000 Chinese women, aged ≥65 years, were prospectively recruited from local communities for a prospective cohort study from August 2001 to March 2003. The LBP prevalence was 30.6% for men and 53.3% for women (P<0.001). In 2010, Cho et al. (53) published LBP data collected for 4,181 subjects from a rural farming community in Korea, with a mean age of 56.6 years. 6-month prevalence of LBP was 38.5% for men and 55.6% for women. The prevalence of LBP increased significantly with age in women (Figure S1B).
Estrogen participates in a variety of biological processes through different molecular mechanisms. The collagen wasting is commonly observed in bone and skin in the postmenopausal period due to decreased estrogen levels (54,55). Estrogen has favorable effects on the lipid profile, antioxidant activity, and enhanced fibrinolysis (56). Estrogen may reduce the risk for arteriosclerosis, which has been considered a risk factor for LBP (57). Estrogen plays an important role in the etiology and pathophysiology of a variety of musculoskeletal degenerative diseases. The prevalence of osteoarthritis (OA) is higher among women than among men, and this prevalence increases considerably after menopause (58,59). Moreover, with the same degree of radiographic damage, OA is also more symptomatic in women (58,59). After menopause women have more severe disc space narrowing than age matched men (28,29,60). This may be associated with the physiological changes caused by relatively lower level of sex hormones after menopause in women, and the accelerated lumbar disc degeneration (33).
The expert views of hormone replacement treatment (HRT) evolved during the last 10 years since the publication of WHI trials (61,62). Dose regimen, combination of estrogen with progestins versus estrogen alone, the administration route and duration of treatment such as the choice of repetitive or periodic administration simulating the menstrual cycle are some of the factors that may be involved in the benefit discrepancies. The Estrogen and Thromboembolism Risk (ESTHER) study confirmed that oral estrogens increased venous thromboembolism risk, whereas transdermal estrogens had little or no impact on the development of thrombosis (63). The presence of gene polymorphisms may also be implicated. HRT may benefit a large number of postmenopausal women, but a subset of women may have higher risk of cardiovascular and thrombotic complications (64). Estrogen receptor modulators and phytoestrogens may retain the desired effects but avoid undesirable effects (65). HRT has been shown to be protective against menopause-associated OA (66,67). However, in one study Musgrave et al. (68) reported women taking HRT reported more back pain and back pain-related disability than did those not taking HRT. An in-depth understanding of the role of the gonadal hormones in LBP modulation remains unclear; whether HRT is useful for patients with severe LBP warrants further studies.
There are a number of limitations for the current study. Only English literatures were included in this review, and only database of PubMed was used. There was a lack of a universal definition and delimitation of LBP and the absence of important specifications of LBP such as the frequency of episodes, its intensity and duration in some studies; therefore we reported the ratio of female vs. male LBP prevalence instead of absolute LBP prevalence. The LBP in survey subjects are assumed to be nonspecific. Specific LBP is due to organic diseases that include spinal fractures, cancers, infections, and cauda equina syndrome can be identified. The probability that a particular case of back pain has a specific cause identified on back radiographs is less than 1% (69). Additionally, for the a few studies the age-specific grouping could only be approximated (Tables S1-S4). This study also did not establish an exact causal role of accelerated spine degeneration in post-menopausal women for the increased LBP prevalence. Our literature review is likely not being exhaustive; however, we believe this limitation is unlikely to have impact on the conclusion of our study.
In conclusion, our synthetic literature review demonstrated females had higher prevalence of LBP across all age groups. This female vs. male difference was highest for school age children. Compared with middle aged subjects, a further increased low back pain prevalence in females than in males was noted after menopause age. Clarification of the hormonal influences on pain modulation will advance our understanding of sex differences in clinical pain conditions such as LBP. The evidence showed in this study may open a new line of further clinical researches.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Manek NJ, MacGregor AJ. Epidemiology of back disorders: prevalence, risk factors, and prognosis. Curr Opin Rheumatol 2005;17:134-40. [PubMed]
- Martin BI, Deyo RA, Mirza SK, Turner JA, Comstock BA, Hollingworth W, Sullivan SD. Expenditures and health status among adults with back and neck problems. JAMA 2008;299:656-64. [Crossref] [PubMed]
- Nagi SZ, Riley LE, Newby LG. A social epidemiology of back pain in a general population. J Chronic Dis 1973;26:769-79. [Crossref]
- Reisbord LS, Greenland S. Factors associated with self-reported back-pain prevalence: a population-based study. J Chronic Dis 1985;38:691-702. [Crossref] [PubMed]
- Burton AK, Clarke RD, McClune TD, Tillotson KM. The natural history of low back pain in adolescents. Spine 1996;21:2323-8. [Crossref] [PubMed]
- Leboeuf-Yde C, Kyvik KO. At what age does low back pain become a common problem? A study of 29,424 individuals aged 12–41 years. Spine (Phila Pa 1976) 1998;23:228-34. [Crossref] [PubMed]
- Calvo-Muñoz I, Gómez-Conesa A, Sánchez-Meca J. Prevalence of low back pain in children and adolescents: a meta-analysis. BMC Pediatr 2013;13:14. [Crossref] [PubMed]
- Manchikanti L, Singh V, Datta S, Cohen SP, Hirsch JA. American Society of Interventional Pain Physicians. Pain Physician 2009;12:E35-70. [PubMed]
- Linton SJ. A review of psychological risk factors in back and neck pain. Spine 2000;25:1148-56. [Crossref] [PubMed]
- Pincus T, Burton AK, Vogel S, Field AP. A systematic review of psychological factors as predictors of chronicity/disability in prospective cohorts of low back pain. Spine (Phila Pa 1976) 2002;27:E109-20. [Crossref] [PubMed]
- Green CR, Anderson KO, Baker TA, Campbell LC, Decker S, Fillingim RB, Kalauokalani DA, Lasch KE, Myers C, Tait RC, Todd KH, Vallerand AH. The unequal burden of pain: confronting racial and ethnic disparities in pain. Pain Med 2003;4:277-94. [Crossref] [PubMed]
- Bailey A. Risk factors for low back pain in women: still more questions to be answered. Menopause 2009;16:3-4. [Crossref] [PubMed]
- Leveille SG, Ling S, Hochberg MC, Resnick HE, Bandeen-Roche KJ, Won A, Guralnik JM. Widespread musculoskeletal pain and the progression of disability in older disabled women. Ann Intern Med 2001;135:1038-46. [Crossref] [PubMed]
- Leveille SG, Zhang Y, McMullen W, Kelly-Hayes M, Felson DT. Sex differences in musculoskeletal pain in older adults. Pain 2005;116:332-8. [Crossref] [PubMed]
- Turk DC, Okifuji A. Psychological factors in chronic pain: evolution and revolution. J Consult Clin Psychol 2002;70:678-90. [Crossref] [PubMed]
- Fillingim RB. Sex, gender and pain: the biopsychosocial Model in action XX vs. XY: The International Journal of Sex Differences in the Study of Health. Dis Aging 2003;1:98-101.
- Wolfe F, Ross K, Anderson J, Russell IJ. Aspects of fibromyalgia in the general population: sex, pain threshold, and fibromyalgia symptoms. J Rheumatol 1995;22:151-6. [PubMed]
- Rollman GB, Lautenbacher S. Sex differences in musculoskeletal pain. Clin J Pain 2001;17:20-4. [Crossref] [PubMed]
- Riley JL III, Robinson ME, Wise EA, Price DD. A meta-analytic review of pain perception across the menstrual cycle. Pain 1999;81:225-35. [Crossref] [PubMed]
- Croft P, Rigby AS, Boswell R, Schollum J, Silman A. The prevalence of chronic widespread pain in the general population. J Rheumatol 1993;20:710-3. [PubMed]
- Wolfe F, Ross K, Anderson J, Russell IJ, Hebert L. The prevalence and characteristics of fibromyalgia in the general population. Arthritis Rheum 1995;38:19-28. [Crossref] [PubMed]
- Hestbaek L, Iachine IA, Leboeuf-Yde C, Kyvik KO, Manniche C. Heredity of low back pain in a young population: a classical twin study. Twin Res 2004;7:16-26. [Crossref] [PubMed]
- Pinheiro MB, Ferreira ML, Refshauge K, Colodro-Conde L, Carrillo E, Hopper JL, Ordoñana JR, Ferreira PH. Genetics and the environment affect the relationship between depression and low back pain: a co-twin control study of Spanish twins. Pain 2015;156:496-503. [Crossref] [PubMed]
- Raastad J, Reiman M, Coeytaux R, Ledbetter L, Goode AP. The association between lumbar spine radiographic features and low back pain: a systematic review and meta-analysis. Semin Arthritis Rheum 2015;44:571-85. [Crossref] [PubMed]
- Miller JA, Schmatz C, Schultz AB. Lumbar disc degeneration: correlation with age, sex, and spine level in 600 autopsy specimens. Spine (Phila Pa 1976) 1988;13:173-8. [Crossref] [PubMed]
- Łebkowski WJ. Autopsy evaluation of the extent of degeneration of the lumbar intervertebral discs. Pol Merkur Lekarski 2002;13:188-90. [PubMed]
- Wang YX, Griffith JF, Leung JC, Yuan J. Age related reduction of T1rho and T2 magnetic resonance relaxation times of lumbar intervertebral disc. Quant Imaging Med Surg 2014;4:259-64. [PubMed]
- Wang YX, Griffith JF, Zeng XJ, Deng M, Kwok AW, Leung JC, Ahuja AT, Kwok T, Leung PC. Prevalence and sex difference of lumbar disc space narrowing in elderly chinese men and women: osteoporotic fractures in men (Hong Kong) and osteoporotic fractures in women (Hong Kong) studies. Arthritis Rheum 2013;65:1004-10. [Crossref] [PubMed]
- Wáng YX. Continued progression of lumbar disc degeneration in postmenopausal women. Climacteric 2015;18:435. [Crossref] [PubMed]
- Takatalo J, Karppinen J, Niinimäki J, Taimela S, Näyhä S, Järvelin MR, Kyllönen E, Tervonen O. Prevalence of degenerative imaging findings in lumbar magnetic resonance imaging among young adults. Spine (Phila Pa 1976) 2009;34:1716-21. [Crossref] [PubMed]
- Wang YX, Griffith JF. Effect of menopause on lumbar disk degeneration: potential etiology. Radiology 2010;257:318-20. [Crossref] [PubMed]
- Wang YX, Griffith JF, Ma HT, Kwok AW, Leung JC, Yeung DK, Ahuja AT, Leung PC. Relationship between gender, bone mineral density, and disc degeneration in the lumbar spine: a study in elderly subjects using an eight-level MRI-based disc degeneration grading system. Osteoporos Int 2011;22:91-6. [Crossref] [PubMed]
- Wáng YX. Postmenopausal Chinese women show accelerated lumbar disc degeneration compared with Chinese men. Journal of Orthopaedic Translation 2015;3:205-11. [Crossref]
- Kosiak M, Aurelius JR, Hartfiel WF. The low back problem--an evaluation. J Occup Med 1968;10:588-93. [PubMed]
- Cohen SP, Argoff CE, Carragee EJ. Management of low back pain. BMJ 2008;337:a2718. [Crossref] [PubMed]
- Leboeuf-Yde C. Body weight and low back pain: A systematic literature review of 56 journal articles reporting on 65 epidemiologic studies. Spine 2000;25:226-37. [Crossref] [PubMed]
- Haber LD. Disabling effects of chronic disease and impairment-II: Functional capacity limitations. J Chron Dis 1973;26:127-51. [Crossref] [PubMed]
- Svensson HO, Andersson GB. Low back pain in forty to forty-seven year old men. I. Frequency of occurrence and impact on medical services. Scand J Rehabil Med 1982;14:47-53. [PubMed]
- Takahashi N, Kikuchi S, Konno S, Morita S, Suzukamo Y, Green J, Fukuhara S. Discrepancy between disability and the severity of low back pain: Demographic, psychologic, and employment-related factors. Spine 2006;31:931-9. [Crossref] [PubMed]
- Hall KRL, Stride E. The varying responses to pain in psychiatric disorders. A study in abnormal psychology. Brit J Med Psychol 1954;27:48-60. [Crossref] [PubMed]
- Kennard MA. Responses to painful stimuli of patients with severe chronic conditions. J Clin Invest 1952;31:245-52. [Crossref] [PubMed]
- Cunningham LS, Kelsey JL. Epidemiology of musculoskeletal impairments and associated disability. Am J Public Health 1984;74:574-9. [Crossref] [PubMed]
- Brodman K, Erdmann AJ, Lorge I, Wolff HG. The Cornell Medical Index-Health Questionnaire. VI. The relation of patients’ complaints to age, sex, race, and education. J Gerontol 1953;8:339-42. [Crossref] [PubMed]
- Unruh AM. Gender variation in clinical pain experience. Pain 1996;65:123-67. [Crossref] [PubMed]
- Heliövaara M, Sievers K, Impivaara O, Maatela J, Knekt P, Mäkelä M, Aromaa A. Descriptive epidemiology and public health aspects of low back pain. Ann Med 1989;21:327-33. [Crossref] [PubMed]
- Freburger JK, Holmes GM, Agans RP, Jackman AM, Darter JD, Wallace AS, Castel LD, Kalsbeek WD, Carey TS. The rising prevalence of chronic low back pain. Arch Intern Med 2009;169:251-8. [Crossref] [PubMed]
- Harkness EF, Macfarlane GJ, Silman AJ, McBeth J. Is musculoskeletal pain more common now than 40 years ago?: Two population-based cross-sectional studies. Rheumatology (Oxford) 2005;44:890-5. [Crossref] [PubMed]
- Bressler HB, Keyes WJ, Rochon PA, Badley E. The prevalence of low back pain in the elderly. A systematic review of the literature. Spine 1999;24:1813-9. [Crossref] [PubMed]
- Mailis-Gagnon A, Nicholson K, Yegneswaran B, Zurowski M. Pain characteristics of adults 65 years of age and older referred to a tertiary care pain clinic. Pain Res Manag 2008;13:389-94. [Crossref] [PubMed]
- Lawrence JS. Disc degeneration. Its frequency and relationship to symptoms. Ann Rheum Dis 1969;28:121-38. [Crossref] [PubMed]
- Papageorgiou AC, Croft PR, Ferry S, Jayson MI, Silman AJ. Estimating the prevalence of low back pain in the general population. Evidence from the South Manchester Back Pain Survey. Spine 1995;20:1889-94. [Crossref] [PubMed]
- He LC, Wang YX, Gong JS, Griffith JF, Zeng XJ, Kwok AW, Leung JC, Kwok T, Ahuja AT, Leung PC. Prevalence and risk factors of lumbar spondylolisthesis in elderly Chinese men and women. Eur Radiol 2014;24:441-8. [Crossref] [PubMed]
- Cho NH, Jung YO, Lim SH, Chung CK, Kim HA. The prevalence and risk factors of low back pain in rural community residents of Korea. Spine (Phila Pa 1976) 2012;37:2001-10. [Crossref] [PubMed]
- Brincat M, Moniz CF, Studd JW, Darby AJ, Magos A, Cooper D. Sex hormones and skin collagen content in postmenopausal women. Br Med J (Clin Res Ed) 1983;287:1337-8. [Crossref] [PubMed]
- Bolognia JL, Braverman IM, Rousseau ME, Sarrel PM. Skin changes in menopause. Maturitas 1989;11:295-304. [Crossref] [PubMed]
- Tostes RC, Nigro D, Fortes ZB, Carvalho MH. Effects of estrogen on the vascular system. Braz J Med Biol Res 2003;36:1143-58. [Crossref] [PubMed]
- Kurunlahti M, Tervonen O, Vanharanta H, Ilkko E, Suramo I. Association of atherosclerosis with low back pain and the degree of disc degeneration. Spine 1999;24:2080-4. [Crossref] [PubMed]
- Srikanth VK, Fryer JL, Zhai G, Winzenberg TM, Hosmer D, Jones G. A meta-analysis of sex differences prevalence, incidence and severity of osteoarthritis. Osteoarthritis Cartilage 2005;13:769-81. [Crossref] [PubMed]
- Lawrence RC, Helmick CG, Arnett FC, Deyo RA, Felson DT, Giannini EH, Heyse SP, Hirsch R, Hochberg MC, Hunder GG, Liang MH, Pillemer SR, Steen VD, Wolfe F. Estimates of the prevalence of arthritis and selected musculoskeletal disorders in the United States. Arthritis Rheum 1998;41:778-99. [Crossref] [PubMed]
- de Schepper EI, Damen J, van Meurs JB, Ginai AZ, Popham M, Hofman A, Koes BW, Bierma-Zeinstra SM. The association between lumbar disc degeneration and low back pain: the influence of age, gender, and individual radiographic features. Spine (Phila Pa 1976) 2010;35:531e6.
- Ghazal S, Pal L. Perspective on hormone therapy 10 years after the WHI. Maturitas 2013;76:208-12. [Crossref] [PubMed]
- Lobo RA, Davis SR, De Villiers TJ, Gompel A, Henderson VW, Hodis HN, Lumsden MA, Mack WJ, Shapiro S, Baber RJ. Prevention of diseases after menopause. Climacteric 2014;17:540-56. [Crossref] [PubMed]
- Scarabin PY, Oger E, Plu-Bureau G. Differential association of oral and transdermal oestrogen-replacement therapy with venous thromboembolism risk. Lancet 2003;362:428-32. [Crossref] [PubMed]
- Herrington DM, Klein KP. Invited review: Pharmacogenetics of estrogen replacement therapy. J Appl Physiol (1985) 2001;91:2776-84. [PubMed]
- Mirkin S, Pickar JH. Selective estrogen receptor modulators (SERMs): a review of clinical data. Maturitas 2015;80:52-7. [Crossref] [PubMed]
- Wluka AE, Davis SR, Bailey M, Stuckey SL, Cicuttini FM. Users of oestrogen replacement therapy have more knee cartilage than non-users. Ann Rheum Dis 2001;60:332-6. [Crossref] [PubMed]
- Tanko LB, Christiansen C, Karsdal MA. Potentials of estrogens in the prevention of osteoarthritis: what do we know and what questions are still pending? In Lobo RA, ed. Treatment of the Postmenopausal Woman. Academic Press, 2007:393-401.
- Musgrave DS, Vogt MT, Nevitt MC, Cauley JA. Back problems among postmenopausal women taking estrogen replacement therapy: the study of Osteoporotic fractures. Spine (Phila Pa 1976) 2001;26:1606-12. [Crossref] [PubMed]
- van den Bosch MA, Hollingworth W, Kinmonth AL, Dixon AK. Evidence against the use of lumbar spine radiography for low back pain. Clin Radiol 2004;59:69-76. [Crossref] [PubMed]
- Hertzberg A. Prediction of cervical and low-back pain based on routine school health examinations. A nine- to twelve-year follow-up study. Scand J Prim Health Care 1985;3:247-53. [Crossref] [PubMed]
- Salminen JJ, Pentti J, Terho P. Low back pain and disability in 14-year-old schoolchildren. Acta Paediatr 1992;81:1035-9. [Crossref] [PubMed]
- Taimela S, Kujala UM, Salminen JJ, Viljanen T. The prevalence of low back pain among children and adolescents. A nationwide, cohort-based questionnaire survey in Finland. Spine 1997;22:1132-6. [Crossref] [PubMed]
- Gunzburg R, Balague F, Nordin M, Szpalski M, Duyck D, Bull D, Melot C. Low back pain in a population of school children. Eur Spine J 1999;8:439-43. [Crossref] [PubMed]
- Vikat A, Rimpela M, Salminen JJ, Rimpela A, Savolainen A, Virtanen SM. Neck or shoulder pain and low back pain in Finnish adolescents. Scand J Public Health 2000;28:164-73. [Crossref] [PubMed]
- Watson KD, Papageorgiou AC, Jones GT, Taylor S, Symmons DP, Silman AJ, Macfarlane GJ. Low back pain in schoolchildren: occurrence and characteristics. Pain 2002;97:87-92. [Crossref] [PubMed]
- Kovacs FM, Gestoso M, del Real MTG, Lopez J, Mufraggi N, Mendez JI. Risk factors for non-specific low back pain in schoolchildren and their parents: a population based study. Pain 2003;103:259-68. [Crossref] [PubMed]
- Prista A, Balague F, Nordin M, Skovron ML. Low back pain in Mozambican adolescents. Eur Spine J 2004;13:341-5. [Crossref] [PubMed]
- Hestbaek L, Leboeuf-Yde C, Kyvik KO, Vach W, Russell MB, Skadhauge L, Svendsen A, Manniche C. Comorbidity with low back pain: a cross-sectional population-based survey of 12- to 22-year-olds. Spine 2004;29:1483-91. [Crossref] [PubMed]
- Sjolie AN. Persistence and change in nonspecific low back pain among adolescents: a 3-year prospective study. Spine 2004;29:2452-7. [Crossref] [PubMed]
- Cakmak A, Yucel B, Ozyalcn SN, Bayraktar B, Ural HI, Duruoz MT, Genc A. The frequency and associated factors of low back pain among a younger population in Turkey. Spine 2004;29:1567-72. [Crossref] [PubMed]
- Jones MA, Stratton G, Reilly T, Unnithan VB. A school-based survey of recurrent non-specific low-back pain prevalence and consequences in children. Health Educ Res 2004;19:284-9. [Crossref] [PubMed]
- Shehab DK, Al-Jarallah KF. Nonspecific low-back pain in Kuwaiti children and adolescents: associated factors. Journal of Adolescent Health 2005;36:32-5. [Crossref] [PubMed]
- Bejia I, Abid N, Ben Salem K, Letaief M, Younes M, Touzi M, Bergaoui N. Low back pain in a cohort of 622 Tunisian schoolchildren and adolescents: an epidemiological study. Eur Spine J 2005;14:331-6. [Crossref] [PubMed]
- Kjaer P, Leboeuf-Yde C, Sorensen JS, Bendix T. An epidemiologic study of MRI and low back pain in 13-year-old children. Spine 2005;30:798-806. [Crossref] [PubMed]
- Oksuz E. Prevalence, risk factors, and preference-based health states of low back pain in a Turkish population. Spine 2006;31:E968-72. [Crossref] [PubMed]
- Mogensen AM, Gausel AM, Wedderkopp N, Kjaer P, Leboeuf-Yde C. Is active participation in specific sport activities linked with back pain? Scand J Med Sci Sports 2007;17:680-6. [Crossref] [PubMed]
- Mikkonen P, Leino-Arjas P, Remes J, Zitting P, Taimela S, Karppinen J. Is smoking a risk factor for low back pain in adolescents? A prospective cohort study. Spine 2008;33:527-32. [Crossref] [PubMed]
- Heuscher Z, Gilkey DP, Peel JL, Kennedy CA. The association of self-reported backpack use and backpack weight with low back pain among college students. J Manipulative Physiol Ther 2010;33:432-7. [Crossref] [PubMed]
- Auvinen JP, Tammelin TH, Taimela SP, Zitting PJ, Jarvelin MR, Taanila AM, Karppinen JI. Is insufficient quantity and quality of sleep a risk factor for neck, shoulder and low back pain? A longitudinal study among adolescents. Eur Spine J 2010;19:641-9. [Crossref] [PubMed]
- Yao W, Mai X, Luo C, Ai F, Chen Q. A cross-sectional survey of nonspecific low back pain among 2083 schoolchildren in China. Spine (Phila Pa 1976) 2011;36:1885-90. [Crossref] [PubMed]
- Onofrio AC, da Silva MC, Domingues MR, Rombaldi AJ. Acute low back pain in high school adolescents in Southern Brazil: prevalence and associated factors. Eur Spine J 2012;21:1234-40. [Crossref] [PubMed]
- O'Sullivan PB, Beales DJ, Smith AJ, Straker LM. Low back pain in 17 year olds has substantial impact and represents an important public health disorder: a cross-sectional study. BMC Public Health 2012;12:100. [Crossref] [PubMed]
- Tiira AH, Paananen MV, Taimela SP, Zitting PJ, Jarvelin MR, Karppinen JI. Determinants of adolescent health care use for low back pain. Eur J Pain 2012;16:1467-76. [Crossref] [PubMed]
- Dolphens M, Cagnie B, Coorevits P, Vanderstraeten G, Cardon G, D'Hooge R, Danneels L. Sagittal standing posture and its association with spinal pain: a school-based epidemiological study of 1196 Flemish adolescents before age at peak height velocity. Spine 2012;37:1657-66. [Crossref] [PubMed]
- Wirth B, Knecht C, Humphreys K. Spine Day 2012: spinal pain in Swiss school children- epidemiology and risk factors. BMC Pediatr 2013;13:159. [Crossref] [PubMed]
- Minghelli B, Oliveira R, Nunes C. Non-specific low back pain in adolescents from the south of Portugal: prevalence and associated factors. Journal of Orthopaedic Science 2014;19:883-92. [Crossref] [PubMed]
- Chiwaridzo M, Naidoo N. Prevalence and associated characteristics of recurrent non-specific low back pain in Zimbabwean adolescents: a cross-sectional study. BMC Musculoskelet Disord 2014;15:381. [Crossref] [PubMed]
- Ward T, Knowelden J, Sharrard WJ. Low back pain. J R Coll Gen Pract 1968;15:128-36. [PubMed]
- Biering-Sørensen F. A prospective study of low back pain in a general population. I. Occurrence, recurrence and aetiology. Scand J Rehabil Med 1983;15:71-9. [PubMed]
- Burton AK, Tillotson KM, Troup JD. Prediction of low-back trouble frequency in a working population. Spine 1989;14:939-46. [Crossref] [PubMed]
- Viikari-Juntura E, Vuori J, Silverstein BA, Kalimo R, Kuosma E, Videman T. A life-long prospective study on the role of psychosocial factors in neck-shoulder and low-back pain. Spine 1991;16:1056-61. [Crossref] [PubMed]
- Palmer KT, Walsh K, Bendall H, Cooper C, Coggon D. Back pain in Britain: comparison of two prevalence surveys at an interval of 10 years. BMJ 2000;320:1577-8. [Crossref] [PubMed]
- McMeeken J, Tully E, Stillman B, Nattrass C, Bygott IL, Story I. The experience of back pain in young Australians. Man Ther 2001;6:213-20. [Crossref] [PubMed]
- Gummesson C, Atroshi I, Ekdahl C, Johnsson R, Ornstein E. Chronic upper extremity pain and co-occurring symptoms in a general population. Arthritis Rheum 2003;49:697-702. [Crossref] [PubMed]
- McBride D, Begg D, Herbison P, Buckingham K. Low back pain in young New Zealanders. N Z Med J 2004;117:U1099. [PubMed]
- Poussa MS, Heliovaara MM, Seitsamo JT, Kononen MH, Hurmerinta KA, Nissinen MJ. Anthropometric measurements and growth as predictors of low-back pain: a cohort study of children followed up from the age of 11 to 22 years. Eur Spine J 2005;14:595-8. [Crossref] [PubMed]
- Barrero LH, Hsu YH, Terwedow H, Perry MJ, Dennerlein JT, Brain JD, Xu X. Prevalence and physical determinants of low back pain in a rural Chinese population. Spine (Phila Pa 1976) 2006;31:2728-34. [Crossref] [PubMed]
- Gourmelen J, Chastang JF, Ozguler A, Lanoe JL, Ravaud JF, Leclerc A. Frequency of low back pain among men and women aged 30 to 64 years in France. Results of two national surveys. Ann Readapt Med Phys 2007;50:640-4, 33-9.
- Shiri R, Solovieva S, Husgafvel-Pursiainen K, Taimela S, Saarikoski LA, Huupponen R, Viikari J, Raitakari OT, Viikari-Juntura E. The association between obesity and the prevalence of low back pain in young adults: the Cardiovascular Risk in Young Finns Study. Am J Epidemiol 2008;167:1110-9. [Crossref] [PubMed]
- Ono R, Higashi T, Takahashi O, Tokuda Y, Shimbo T, Endo H, Hinohara S, Fukui T, Fukuhara S. Sex differences in the change in health-related quality of life associated with low back pain. Qual Life Res 2012;21:1705-11. [Crossref] [PubMed]
- Birabi BN, Dienye PO, Ndukwu GU. Prevalence of low back pain among peasant farmers in a rural community in South South Nigeria. Rural Remote Health 2012;12:1920. [PubMed]
- Yue P, Liu F, Li L. Neck/shoulder pain and low back pain among school teachers in China, prevalence and risk factors. BMC Public Health 2012;12:789. [Crossref] [PubMed]
- Hartvigsen J, Davidsen M, Hestbaek L, Sogaard K, Roos EM. Patterns of musculoskeletal pain in the population: a latent class analysis using a nationally representative interviewer-based survey of 4817 Danes. Eur J Pain 2013;17:452-60. [Crossref] [PubMed]
- Erick PN, Smith DR. Low back pain among school teachers in Botswana, prevalence and risk factors. BMC Musculoskelet Disord 2014;15:359. [Crossref] [PubMed]
- Rottermund J, Knapik A, Saulicz E, Mysliwiec A, Saulicz M, Rygiel KA, Linek P. Back and neck pain among school teachers in Poland and its correlations with physical activity. Med Pr 2015;66:771-8. [PubMed]
- Lavsky-Shulan M, Wallace RB, Kohout FJ, Lemke JH, Morris MC, Smith IM. Prevalence and functional correlates of low back pain in the elderly: the Iowa 65+ Rural Health Study. J Am Geriatr Soc 1985;33:23-8. [Crossref] [PubMed]
- Tsuji T, Matsuyama Y, Sato K, Hasegawa Y, Yimin Y, Iwata H. Epidemiology of low back pain in the elderly: correlation with lumbar lordosis. J Orthop Sci 2001;6:307-11. [Crossref] [PubMed]
- Muraki S, Oka H, Akune T, Mabuchi A, En-Yo Y, Yoshida M, Saika A, Suzuki T, Yoshida H, Ishibashi H, Yamamoto S, Nakamura K, Kawaguchi H, Yoshimura N. Prevalence of radiographic lumbar spondylosis and its association with low back pain in elderly subjects of population-based cohorts: the ROAD study. Ann Rheum Dis 2009;68:1401-6. [Crossref] [PubMed]
- Muraki S, Akune T, Oka H, En-Yo Y, Yoshida M, Nakamura K, Kawaguchi H, Yoshimura N. Prevalence of falls and the association with knee osteoarthritis and lumbar spondylosis as well as knee and lower back pain in Japanese men and women. Arthritis Care Res (Hoboken) 2011;63:1425-31. [Crossref] [PubMed]
- Kim W, Jin YS, Lee CS, Hwang CJ, Lee SY, Chung SG, Choi KH. Relationship between the type and amount of physical activity and low back pain in Koreans aged 50 years and older. PM R 2014;6:893-9. [Crossref] [PubMed]
- Palma R, de Conti MH, Quintino NM, Gatti MA, Simeao SF, de Vitta A. Functional capacity and its associated factors in the elderly with low back pain. Acta Ortop Bras 2014;22:295-9. [Crossref] [PubMed]
- Teraguchi M, Yoshimura N, Hashizume H, Muraki S, Yamada H, Oka H, Minamide A, Nakagawa H, Ishimoto Y, Nagata K, Kagotani R, Tanaka S, Kawaguchi H, Nakamura K, Akune T, Yoshida M. The association of combination of disc degeneration, end plate signal change, and Schmorl node with low back pain in a large population study: the Wakayama Spine Study. Spine J 2015;15:622-8. [Crossref] [PubMed]
- Frymoyer JW, Pope MH, Costanza MC, Rosen JC, Goggin JE, Wilder DG. Epidemiologic studies of low-back pain. Spine 1980;5:419-23. [Crossref] [PubMed]
- Deyo RA, Tsui-Wu YJ. Descriptive epidemiology of low-back pain and its related medical care in the United States. Spine 1987;12:264-8. [Crossref] [PubMed]
- Heliövaara M, Mäkelä M, Knekt P, Impivaara O, Aromaa A. Determinants of sciatica and low-back pain. Spine (Phila Pa 1976) 1991;16:608-14. [Crossref] [PubMed]
- Walsh K, Cruddas M, Coggon D. Low back pain in eight areas of Britain. J Epidemiol Community Health 1992;46:227-30. [Crossref] [PubMed]
- Darmawan J, Valkenburg HA, Muirden KD, Wigley RD. Epidemiology of rheumatic diseases in rural and urban populations in Indonesia: a World Health Organisation International League Against Rheumatism COPCORD study, stage I, phase 2. Ann Rheum Dis 1992;51:525-8. [Crossref] [PubMed]
- Croft PR, Papageorgiou AC, Thomas E, Macfarlane GJ, Silman AJ. Short-term physical risk factors for new episodes of low back pain. Prospective evidence from the South Manchester Back Pain Study. Spine (Phila Pa 1976) 1999;24:1556-61. [Crossref] [PubMed]
- Santos-Eggimann B, Wietlisbach V, Rickenbach M, Paccaud F, Gutzwiller F. One-year prevalence of low back pain in two Swiss regions: estimates from the population participating in the 1992-1993 MONICA project. Spine (Phila Pa 1976) 2000;25:2473-9. [Crossref] [PubMed]
- Walker BF, Muller R, Grant WD. Low back pain in Australian adults: prevalence and associated disability. J Manipulative Physiol Ther 2004;27:238-44. [Crossref] [PubMed]
- Zeng QY, Chen R, Xiao ZY, Huang SB, Liu Y, Xu JC, Chen SL, Darmawan J, Couchman KG, Wigley RD, Muirden KD. Low prevalence of knee and back pain in southeast China; the Shantou COPCORD study. J Rheumatol 2004;31:2439-43. [PubMed]
- Gilgil E, Kacar C, Butun B, Tuncer T, Urhan S, Yildirim C, Sunbuloglu G, Arikan V, Tekeoglu I, Oksuz MC, Dundar U. Prevalence of low back pain in a developing urban setting. Spine (Phila Pa 1976) 2005;30:1093-8. [Crossref] [PubMed]
- Ihlebaek C, Hansson TH, Laerum E, Brage S, Eriksen HR, Holm SH, Svendsrod R, Indahl A. Prevalence of low back pain and sickness absence: a "borderline" study in Norway and Sweden. Scand J Public Health 2006;34:555-8. [Crossref] [PubMed]
- Schmidt CO, Raspe H, Pfingsten M, Hasenbring M, Basler HD, Eich W, Kohlmann T. Back pain in the German adult population: prevalence, severity, and sociodemographic correlates in a multiregional survey. Spine (Phila Pa 1976) 2007;32:2005-11. [Crossref] [PubMed]
- Strine TW, Hootman JM. US national prevalence and correlates of low back and neck pain among adults. Arthritis Rheum 2007;57:656-65. [Crossref] [PubMed]
- Altinel L, Kose KC, Ergan V, Isik C, Aksoy Y, Ozdemir A, Toprak D, Dogan N. The prevalence of low back pain and risk factors among adult population in Afyon region, Turkey. Acta Orthop Traumatol Turc 2008;42:328-33. [Crossref] [PubMed]
- Leclerc A, Gourmelen J, Chastang JF, Plouvier S, Niedhammer I, Lanoe JL. Level of education and back pain in France: the role of demographic, lifestyle and physical work factors. Int Arch Occup Environ Health 2009;82:643-52. [Crossref] [PubMed]
- Leboeuf-Yde C, Nielsen J, Kyvik KO, Fejer R, Hartvigsen J. Pain in the lumbar, thoracic or cervical regions: do age and gender matter? A population-based study of 34,902 Danish twins 20-71 years of age. BMC Musculoskelet Disord 2009;10:39. [Crossref] [PubMed]
- Tucer B, Yalcin BM, Ozturk A, Mazicioglu MM, Yilmaz Y, Kaya M. Risk factors for low back pain and its relation with pain related disability and depression in a Turkish sample. Turk Neurosurg 2009;19:327-32. [PubMed]
- Leijon O, Mulder M. Prevalence of low back pain and concurrent psychological distress over a 16-year period. Occup Environ Med 2009;66:137-9. [Crossref] [PubMed]
- Fernández-de-las-Peñas C, Hernández-Barrera V, Alonso-Blanco C, Palacios-Ceña D, Carrasco-Garrido P, Jiménez-Sánchez S, Jiménez-García R. Prevalence of neck and low back pain in community-dwelling adults in Spain: a population-based national study. Spine (Phila Pa 1976) 2011;36:E213-9. [Crossref] [PubMed]
- Jiménez-Sánchez S, Fernández-de-Las-Peñas C, Carrasco-Garrido P, Hernández-Barrera V, Alonso-Blanco C, Palacios-Ceña D, Jiménez-García R. Prevalence of chronic head, neck and low back pain and associated factors in women residing in the Autonomous Region of Madrid (Spain). Gac Sanit 2012;26:534-40. [Crossref] [PubMed]
- Korovessis P, Repantis T, Zacharatos S, Baikousis A. Low back pain and sciatica prevalence and intensity reported in a Mediterranean country: ordinal logistic regression analysis. Orthopedics 2012;35:e1775-84.
- Liu X, Wang L, Stallones L, Wheeler KK, Zhao W, Smith GA, Xiang H. Back pain among farmers in a northern area of China. Spine (Phila Pa 1976) 2012;37:508-14. [Crossref] [PubMed]
- Macfarlane GJ, Beasley M, Jones EA, Prescott GJ, Docking R, Keeley P, McBeth J, Jones GT, Team MS. The prevalence and management of low back pain across adulthood: results from a population-based cross-sectional study (the MUSICIAN study). Pain 2012;153:27-32. [Crossref] [PubMed]
- Björnsdóttir SV, Jónsson SH, Valdimarsdóttir UA. Functional limitations and physical symptoms of individuals with chronic pain. Scand J Rheumatol 2013;42:59-70. [Crossref] [PubMed]
- Chou YC, Shih CC, Lin JG, Chen TL, Liao CC. Low back pain associated with sociodemographic factors, lifestyle and osteoporosis: a population-based study. J Rehabil Med 2013;45:76-80. [Crossref] [PubMed]
- Fujii T, Matsudaira K. Prevalence of low back pain and factors associated with chronic disabling back pain in Japan. Eur Spine J 2013;22:432-8. [Crossref] [PubMed]
- Pedisic Z, Pranic S, Jurakic D. Relationship of back and neck pain with quality of life in the Croatian general population. J Manipulative Physiol Ther 2013;36:267-75. [Crossref] [PubMed]
- Hu HY, Chen L, Wu CY, Chou YJ, Chen RC, Huang N. Associations among low back pain, income, and body mass index in Taiwan. Spine J 2013;13:1521-6. [Crossref] [PubMed]
- Meucci RD, Fassa AG, Paniz VM, Silva MC, Wegman DH. Increase of chronic low back pain prevalence in a medium-sized city of southern Brazil. BMC Musculoskelet Disord 2013;14:155. [Crossref] [PubMed]
- Sandoughi M, Zakeri Z, Tehrani Banihashemi A, Davatchi F, Narouie B, Shikhzadeh A, Mohammadi M, Jahantigh M, Shakiba M, Moulaei NA, Yousefi S, Rezazehi B, Shirzaei Sani E, Emamdadi A, Hoseynian M, Masoodian S, Shahbakhsh S. Prevalence of musculoskeletal disorders in southeastern Iran: a WHO-ILAR COPCORD study (stage 1, urban study). International Journal of Rheumatic Diseases 2013;16:509-17. [Crossref] [PubMed]
- Heuch I, Heuch I, Hagen K, Zwart JA. Body mass index as a risk factor for developing chronic low back pain: a follow-up in the Nord-Trondelag Health Study. Spine (Phila Pa 1976) 2013;38:133-9. [Crossref] [PubMed]
- Choi K, Park JH, Cheong HK. Prevalence of musculoskeletal symptoms related with activities of daily living and contributing factors in Korean adults. J Prev Med Public Health 2013;46:39-49. [Crossref] [PubMed]
- Lee S, Nam CM, Yoon DH, Kim KN, Yi S, Shin DA, Ha Y. Association between low-back pain and lumbar spine bone density: a population-based cross-sectional study. J Neurosurg Spine 2013;19:307-13. [Crossref] [PubMed]
- Mork PJ, Vik KL, Moe B, Lier R, Bardal EM, Nilsen TI. Sleep problems, exercise and obesity and risk of chronic musculoskeletal pain: the Norwegian HUNT study. Eur J Public Health 2014;24:924-9. [Crossref] [PubMed]
- Araújo F, Lucas R, Alegrete N, Azevedo A, Barros H. Sagittal standing posture, back pain, and quality of life among adults from the general population: a sex-specific association. Spine (Phila Pa 1976) 2014;39:E782-94. [Crossref] [PubMed]
- Großschädl F, Stolz E, Mayerl H, Rásky É, Freidl W, Stronegger W. Educational inequality as a predictor of rising back pain prevalence in Austria-sex differences. Eur J Public Health 2016;26:248-53. [Crossref] [PubMed]
- Capkin E, Karkucak M, Cakırbay H, Topbas M, Karaca A, Köse MM, Gökmen F. The prevalence and risk factors of low back pain in the eastern Black Sea region of Turkey. J Back Musculoskelet Rehabil 2015;28:783-7. [Crossref] [PubMed]


