
Tumor mutational burden assessment as a predictive biomarker for immunotherapy in lung cancer patients: getting ready for prime-time or not?
Introduction
The introduction of cancer immunotherapy for the treatment of non-small cell lung cancer (NSCLC) has revolutionized treatment algorithms for advanced and metastatic patients and has massively improved survival rates for certain groups of patients. Pembrolizumab, a PD-1 blocking monoclonal antibody (mAB), has been approved by the Food and Drug Administration (FDA) for first-line treatment of NSCLC patients with a PD-L1 tumor proportion score >50% and in second-line treatment for patients with PD-L1 expression >1% (1). Additionally, it was recently shown to be beneficial in first-line treatment, irrespective of PD-L1 expression, when administered in combination with pemetrexed or carboplatin (2,3) and was consequently approved by the FDA as a first-line treatment (4). Additionally, nivolumab, another PD-1 blocking mAB, has been approved for the second line treatment of metastatic NSCLC after failed chemotherapy for patients with PD-L1 expression >1% (5). Furthermore, atezolizumab (an anti-PD-L1 mAB) has been approved for second-line treatment of metastatic NSCLC (6), and durvalumab (an anti-PD-L1 mAB) was also approved for the maintenance therapy of unresected stage III NSCLC after successful chemoradiotherapy (7). However, while the biological concept of immune checkpoint inhibition has been extensively studied, not all aspects of immunotherapy are fully understood at present (8). While many patients respond to the treatment and show stable disease over long periods (9-11), cancer immunotherapy is not effective in other patients or is even associated with tumor hyperprogression (12). The only biomarker that is currently used as surrogate marker for the selection of patients eligible for cancer immunotherapy, and FDA approved as a companion diagnostic test (CDx), is the expression of PD-L1 in tumor cells as detected by immunohistochemistry (IHC) (13). However, while all currently approved immunotherapy treatments in NSCLC target the PD1-PD-L1 interaction, the use of PD-L1 as a biomarker has its limitations (13). PD-L1 expression (>1% or >5%) has been reported in only 24–60% of NSCLC (14). Furthermore, high expression of PD-L1 (>50%) is limited to only 25–30% of all NSCLC (15-17) and the objective response rate (ORR) was for example only 44.8% in the PD-L1 >50% group in the KEYNOTE-024 trial which compared first line treatment of pembrolizumab in patients with PD-L1 >50% versus chemotherapy (17). Consequently, there are currently many challenges concerning the effective use of PD-L1 IHC as a biomarker to select patients for immunotherapy, and it is imperative that we find more robust biomarkers to be used either independently or in association with PD-L1 IHC (18,19). It has been speculated that the rise of tumor neoantigens might trigger the patients’ immune system to attack the tumor [(20,21) for review). Thus, it has been postulated that the emergence of these tumor neoantigens could serve as a predictor of response to cancer immunotherapy (22-24). For example, assessment of the tumor mutational burden (TMB), defined as the total number of nonsynonymous mutations in the coding regions of genes, including small indel variants, has recently been proposed to stratify patients for cancer immunotherapy (25).
The aim of this review is to consider the suitability of TMB as a novel and strong biomarker for the assessment of patients who could be eligible to receive cancer immunotherapy in NSCLC and to discuss whether TMB is ready for prime-time clinical use. We discuss the research supporting the suitability of TMB, as well as the opposing evidence that prevents TMB from being currently implemented in routine practice.
The pros
TMB is a biomarker of immunotherapy efficiency that is independent of PD-L1 IHC expression
TMB has proven to be an effective and independent predictive biomarker of PD-L1 expression in tumors (26,27). Response rate, progression-free survival (PFS) as well as overall survival (OS) increase with higher TMB and were independent of PD-L1 expression as assessed by IHC (28). Recent data from the CheckMate-227 trial, comparing nivolumab plus ipilimumab with nivolumab monotherapy and chemotherapy in the first-line, demonstrated that high-TMB patients (>10 mutations/Mb) received the greatest benefits in terms of OS (26). This clearly confirms the effectiveness of treatment stratification based on TMB. Additionally, improved OS (HR =0.59) was also seen in patients with low PD-L1 expression <1% (26). Simultaneously published results from the Keynote-189 trial, comparing first-line pembrolizumab treatment with pembrolizumab in combination with chemotherapy, demonstrated improved efficacy even in low PD-L1 expression patients, highlighting once more the urgent requirement for novel PD-L1 independent biomarkers (16). However, the strongest responses have been seen in patients with both high TMB and high PD-L1 expression (>50%) and it is therefore currently unclear if TMB might be a good addition to existing PD-L1 expression analyses or if it might be able to completely replace PD-L1 testing altogether (26,29,30).
TMB can be efficiently assessed using targeted sequencing panels
TMB was initially assessed using whole exome sequencing (WES) (25,27,29,31). While this might be suitable and achievable in a research setting, its regular use in routine clinical practice would certainly exceed the infrastructural capacities of most current molecular pathology laboratories. The requirements for data storage and analysis, as well as the current costs and sequencing time, would perturb the routine workflows of most of the laboratories. Moreover, the prolonged turnaround time for results could be unrealistic in a routine clinical setting. In this context, various targeted sequencing panels have recently been developed to efficiently determine TMB, and have shown strong correlation with WES (28,32,33). Rizvi et al. demonstrated a high correlation (Spearmen ρ =0.86) between WES and the Memorial Sloan Kettering-Integrated Mutation Profiling of Actionable Cancer Targets (MSK-IMPACT) targeted sequencing panel, which targets 468 individual cancer-related genes, thereby covering 1.5 Mb of the human genome (30). The MSK-IMPACT panel was developed in-house at the Memorial Sloan Kettering Cancer Center (MSKCC) in New York, USA and was later approved by the FDA (34,35). Furthermore, the FDA-approved FoundationOne CDx™ (Foundation Medicine, Cambridge, USA) targeted sequencing panel, covering 324 individual genes across 1.1 MB of the genome also highly correlates with TMB as assessed by WES (29,31). This panel was successfully used for the stratification of 1,004 patients in the CheckMate-227 trial (26). However, the correlation between WES and targeted sequencing panels appears to be limited to panels covering large genomic regions and is unfortunately lost in more focused gene panels (32). Furthermore, the MSK-IMPACT panel is a single-site assay [meeting the FDA requirements as Laboratory Developed Test (LDT)] and thus not commercially available, while the FoundationOne CDx is a service offered by Foundation Medicine (Cambridge, USA), where samples must be sent to their testing centers. Consequently, both panels preclude in-house use and assessment. Thermo Fisher Scientific (Waltham, USA) has developed the Oncomine Tumor Mutation Load Assay, a targeted sequencing panel covering 407 individual genes with 1.7 Mb of coverage, which has been developed for their Ion Torrent platforms (35). In theory this would allow the direct assessment of TMB and druggable mutations in any molecular pathology laboratory and might be more easily integrated into existing workflows. Moreover, the development of this sequencing panel might decrease the turnaround time for results and reduce costs. Therefore, it is important to determine how this panel will perform in a real-life clinical setting and how its results correlate with competing assays for the stratification of patients for cancer immunotherapy. In addition to the assays described above, further market fragmentation is to be expected due to the development of a plethora of new sequencing panels. Consequently, while the use of larger targeted sequencing panels will certainly expand labor requirements and increase costs, they remain relatively easy to implement in a routine molecular pathology workflow. Such panels could therefore be used as standard tool in the initial mutational assessment of each NSCLC patient. The implementation of TMB evaluation using targeted sequencing panels will be relatively straightforward and is expected to lead to rapid distribution and high prevalence among clinical testing centers.
The cons
While the promising results of CheckMate-227 certainly demonstrate the relevance of TMB in cancer immunotherapy, there are currently several reasons why TMB might not have been ready for prime-time clinical use until now.
Availability of tumor material might limit the use of TMB in clinical routine practice
Large sequencing panels are required for TMB assessment and these panels necessitate larger amounts of tumor material (e.g., tumor DNA). The FoundationOne CDx test requires at least 10 unstained FFPE slides with a tumor cell content greater than 20% to be submitted to the testing center (36), because at least 50 ng and >500× coverage of tumor DNA is required to get reliable results (37). Importantly, in contrast to the other sequencing panels, the FoundationOne definition of TMB includes synonymous mutations (26), which, in contrast, are filtered out in the MSK-IMPACT panel (37). Similarly, the MSK-IMPACT panel requires 5–20 unstained FFPE sections with a tumor cell content >10% (34), while the Thermo Fisher Oncomine Tumor Mutation Load Assay requires a DNA input of 20 ng (35). This is still higher than the minimal 10 ng input for the CE-IVD Oncomine Solid Tumor DNA panel and might decrease the ratio of samples that are eligible for TMB assessment. However, a minimum percentage of tumor cells had not previously been specified until now for this panel. Especially in late stage NSCLC, small biopsies are usually the main tissue source for tumor analysis. In this context, the limited amounts of tumor DNA obtained following a conventional biopsy or a fine needle biopsy might make the TMB assessment challenging or even impossible, regardless of whether it is conducted independently or in association with the assessment of the gene panel for druggable mutations (38). Additionally, it could be also very challenging to assess TMB in bronchial or transthoracic biopsies showing a low percentage of tumor cells or from large necrotic or inflamed areas (39). Interestingly, TMB assessment in ctDNA has been shown to correlate strongly with tissue-derived TMB status (40-43). However, ctDNA studies also revealed some differences in TMB between primary and metastatic tissue, which might interfere with precise TMB assessment (43). However, only preclinical studies have been published thus far, precluding its use in routine clinical assessment. Moreover, the quantity and the quality of ctDNA is certainly the main current impediment to producing systematically robust TMB results in advanced or metastatic NSCLC patients. Interestingly, the interim results for the B-F1RST study, analyzing blood-based TMB for the stratification of atezolizumab in first line therapy for NSCLC showed promising results (44). Blood-based TMB correlated well with treatment response to first-line atezolizumab therapy.
In contrast, less material is required for the assessment of PD-L1 expression in tumor cells and various sources can be used for this assessment (13,39). Only 100 tumor cells are required to meet the cutoff established for PD-L1 IHC assessment (45). In this context, even if the PD-L1 immunocytochemistry (ICC) is currently not validated as a CDx (in contrast to IHC), it can probably be used as a predictive biomarker on cell blocks containing more than 100 tumor cells (46).
TMB currently serves as a complementary diagnostic tool but it might not have yet the power to replace PD-L1 IHC testing. Thus, while TMB could improve therapeutic stratification and might help to select the right patient for the right therapy at the right time, it will certainly increase diagnostic complexity, costs and might delay time to diagnosis and patient care. Additionally, it will not be suitable for all patients and limited sample resources might prevent TMB assessment in a significant number of patients.
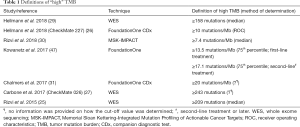
Absence of standardization prevents comparability between assays
The greatest challenge to the implementation of TMB in routine clinical practice is the absence of standardization between the different tests. While the terms “low TMB” or “high TMB” are commonly used, there is not a clear definition of either term (Table 1). Initially, TMB stratification was performed using the 50% percentile or by expanding this strategy to other percentiles, as well as other defined standards (26,30,48). However, there is no biological justification for such stratification and hypermutated patients might interfere with the percentile-based separation. Interestingly, Hellman et al. used a receiver operating characteristic curve (ROC curve) to determine the best cut-off for TMB-based stratification using the FoundationOne CDx panel (26). This approach might be superior to percentile-based stratification as it statistically justifies the cut-off point. In the Checkmate-227 trial, a cutoff of >10 mutations/Mb was determined. This is higher notably than the previously used cut-off at the 50% percentile, which was determined to be 5–7.4 mutations/Mb in NSCLC (28,30,31). Thus, the ROC curve-derived cut-off value for the FoundationOne panel must be evaluated and we must determine if and how this can be transferred to other sequencing panels and if a single value can be used across all panels.
Full table
Another important aspect to this analysis is that germline mutations must be filtered out to avoid false positive mutation calls (32). While the MSK-IMPACT panel sequences matched healthy tissue (34), computer-based methods that filter germline mutations using large databases have also been shown to work efficiently (49,50). However, it was recently shown that clonal hematopoiesis-derived mutations have been detected in many different solid tumors with a high prevalence in NSCLC patients (51). As this might overestimate the TMB in the tumor, sequencing of matched white-blood cells (WBCs) might be necessary to avoid miss-classification of patients. Additionally, all mutations are currently considered to be equal and the assessment and stratification is only performed on the quantitative assessment of mutations. However, it has been demonstrated that certain mutations, like P53 mutations or genomic alterations in the mismatch repair pathway (MMR) and homologous recombination pathway (HR) might also impact the response to immunotherapy (52-55). Furthermore, other features such as STK11 mutations are suspected to be strongly correlated with non-responding patients (29,30). Consequently, one can speculate that certain mutations might have a greater influence than others within the TMB range and that patients with fewer but potentially more relevant mutations might respond better than patients who have a higher TMB but with fewer mutations in certain crucial loci, such as MMR or HR genes. This would certainly further increase the complexity of stratification and could hinder full market penetration.
Additionally, sequencing panels for TMB assessment would require the CE-IVD certification in Europe to guarantee the highest quality and to maintain minimal inter-assay variability. This is a mandatory step to allow the implementation in accredited molecular pathology laboratories (56) and would require either external quality assessment (EQA) or validation by larger European ring studies. However, both are currently lacking and therefore it is urgent that this process has been initiated.
Conclusions
TMB has been shown to be a promising, effective and independent biomarker for the stratification of cancer immunotherapy, where it meets an important need in current routine practice in pathology. The development of novel targeted sequencing panels has been shown to efficiently replace previously performed WES. Additionally, this allows the determination of TMB for cancer immunotherapy and the search for druggable mutations at the same time and might therefore lead to its rapid implementation in current workflows.
However, TMB in targeted panels has only been assessed with the MSK-IMPACT and the FoundationOne CDx panels in clinical practice. While the first is an LDT and not a commercially available test, the latter requires the submission of each patient’s sample to external testing centers, which might not be acceptable in all countries and settings, for example, under the new data protection regulations (GDPR) in the European Union (57,58). Commercial panels for TMB have been, and will be, developed in the future, risking a complicated market fragmentation that might hinder its fast and universal implementation in daily practice. A similar situation occurred recently with the onset of multiple clones of PD-L1 for IHC, some of which have been used as an LTD while others are used as a CDx (13). Finally, only comparative studies derived from clinical trials with different TMB panels will demonstrate the relative efficiency of these panels and their capacity to act as predictive biomarkers.
The requirement for significant amounts of sample material might be another possible hurdle for routine implementation, where the amount and the quality of sample material is typically less controlled than in clinical trials. For example, only 58% of the samples in the CheckMate-227 trial met the minimum requirements for TMB assessment (26).
Finally, routine clinical TMB assessment is yet to be standardized and evidence-based stratification according to the mutational load is not yet sufficiently refined and tested. TMB is certainly a promising biomarker in cancer immunotherapy for NSCLC patients but current limitations have to be overcome to prepare it for prime-time clinical use. Further clinical trials must be performed to resolve these open questions and the technical workflow must be standardized to allow for the robust comparison of patients between laboratories and clinical centers.
Acknowledgements
We would like to thank Abby Cuttriss from the Office of International Scientific Visibility at the University Côte d’Azur for editing assistance.
Funding: This work was supported by the French Government (National Research Agency, ANR) through the “Investments for the Future” LABEX SIGNALIFE: program reference # ANR-11-LABX-0028-01, the Conseil Departemental des Alpes Maritimes, the Ligue Departementale contre le Cancer, the Canceropole PACA and the Association for Cancer Research (ARC).
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Merck. Prescribing Information - KEYTRUDA (pembrolizumab). 2017;45. Available online: https://www.merck.com/product/usa/pi_circulars/k/keytruda/keytruda_pi.pdf
- Langer CJ, Gadgeel SM, Borghaei H, et al. Carboplatin and pemetrexed with or without pembrolizumab for advanced, non-squamous non-small-cell lung cancer: a randomised, phase 2 cohort of the open-label KEYNOTE-021 study. Lancet Oncol 2016;17:1497-508. [Crossref] [PubMed]
- Gandhi L, Rodríguez-Abreu D, Gadgeel S, et al. Pembrolizumab plus Chemotherapy in Metastatic Non-Small-Cell Lung Cancer. N Engl J Med 2018;378:2078-92. [Crossref] [PubMed]
- FDA. Pembrolizumab (Keytruda) 5-10-2017 [Internet]. 2017. Available online: https://www.fda.gov/drugs/informationondrugs/approveddrugs/ucm558048.htm
- Prescribing Information - OPDIVO (nivolumab) [Internet]. 2018 [cited 2018 May 9]. Available online: https://packageinserts.bms.com/pi/pi_opdivo.pdf
- Prescribing Information - TECENTRIQ (atezolizumab) [Internet]. 2018 [cited 2018 May 9]. Available online: https://www.gene.com/download/pdf/tecentriq_prescribing.pdf
- Prescribing Information - IMFINZI (durvalumab) [Internet]. 2018 [cited 2018 May 9]. Available online: https://www.azpicentral.com/imfinzi/imfinzi.pdf#page=1
- Ilie M, Benzaquen J, Hofman V, et al. Immunotherapy in non-small cell lung cancer: Biological principles and future opportunities. Curr Mol Med 2017;17:527-40. [Crossref] [PubMed]
- Schouten R, Baas P, Van Den Heuvel M. MA14.07 Real Life Experience with Immunotherapy in the Netherlands. J Thorac Oncol 2017;12:S425. [Crossref]
- Pérez JM, Sanchez I, Gonzalez AF, et al. P3.02c-034 A Single Institution Experience with Immunotherapy as an Effective Therapy Approach of Advance Non-Small Cell Lung Cancer (NSCLC). J Thorac Oncol 2017;12:S1293-4. [Crossref]
- Brustugun OT, Sprauten M. Helland. Real-world data on nivolumab treatment of non-small cell lung cancer. Acta Oncol 2017;56:438-40. [Crossref] [PubMed]
- Champiat S, Dercle L, Ammari S, et al. Hyperprogressive disease is a new pattern of progression in cancer patients treated by anti-PD-1/PD-L1. Clin Cancer Res 2017;23:1920-8. [Crossref] [PubMed]
- Hofman P. PD-L1 immunohistochemistry for non-small cell lung carcinoma: which strategy should be adopted? Expert Rev Mol Diagn 2017;17:1097-108. [Crossref] [PubMed]
- Yu H, Boyle TA, Zhou C, et al. PD-L1 expression in lung cancer. J Thorac Oncol 2016;11:964-75. [Crossref] [PubMed]
- Sorensen SF, Zhou W, Dolled-Filhart M, et al. PD-L1 expression and survival among patients with advanced non–small cell lung cancer treated with chemotherapy. Transl Oncol 2016;9:64-9. [Crossref] [PubMed]
- Aggarwal C, Rodriguez Abreu D, Felip E, et al. Prevalence of PD-L1 expression in patients with non-small cell lung cancer screened for enrollment in KEYNOTE-001, -010, and -024. Ann Oncol 2016;27. [Crossref]
- Reck M, Rodríguez-Abreu D, Robinson AG, et al. Pembrolizumab versus Chemotherapy for PD-L1–Positive Non–Small-Cell Lung Cancer. N Engl J Med 2016;375:1823-33. [Crossref] [PubMed]
- Teng F, Meng X, Kong L, et al. Progress and challenges of predictive biomarkers of anti PD-1/PD-L1 immunotherapy: A systematic review. Cancer Lett 2018;414:166-73. [Crossref] [PubMed]
- Cesano A, Warren S. Bringing the Next Generation of Immuno-Oncology Biomarkers to the Clinic. Biomedicines 2018;6:14. [Crossref] [PubMed]
- Heemskerk B, Kvistborg P, Schumacher TN. The cancer antigenome. EMBO J 2013;32:194-203. [Crossref] [PubMed]
- Schumacher TN, Schreiber RD. Neoantigens in cancer immunotherapy. Science 2015;348:69-74. [Crossref] [PubMed]
- DuPage M, Mazumdar C, Schmidt LM, et al. Expression of tumour-specific antigens underlies cancer immunoediting. Nature 2012;482:405-9. [Crossref] [PubMed]
- Matsushita H, Vesely MD, Koboldt DC, et al. Cancer exome analysis reveals a T-cell-dependent mechanism of cancer immunoediting. Nature 2012;482:400-4. [Crossref] [PubMed]
- Castle JC, Kreiter S, Diekmann J, et al. Exploiting the mutanome for tumor vaccination. Cancer Res 2012;72:1081-91. [Crossref] [PubMed]
- Rizvi NA, Hellmann MD, Snyder A, et al. Cancer immunology. Mutational landscape determines sensitivity to PD-1 blockade in non-small cell lung cancer. Science 2015;348:124-8. [Crossref] [PubMed]
- Hellmann MD, Ciuleanu TE, Pluzanski A, et al. Nivolumab plus Ipilimumab in Lung Cancer with a High Tumor Mutational Burden. N Engl J Med 2018;378:2093-104. [Crossref] [PubMed]
- Carbone DP, Reck M, Paz-Ares L, et al. First-Line Nivolumab in Stage IV or Recurrent Non–Small-Cell Lung Cancer. N Engl J Med 2017;376:2415-26. [Crossref] [PubMed]
- Goodman AM, Kato S, Bazhenova L, et al. Tumor Mutational Burden as an Independent Predictor of Response to Immunotherapy in Diverse Cancers. Mol Cancer Ther 2017;16:2598-608. [Crossref] [PubMed]
- Hellmann MD, Nathanson T, Rizvi H, et al. Genomic Features of Response to Combination Immunotherapy in Patients with Advanced Non-Small-Cell Lung Cancer. Cancer Cell 2018;33:843-52.e4. [Crossref] [PubMed]
- Rizvi H, Sanchez-Vega F, La K, et al. Molecular determinants of response to anti-programmed cell death (PD)-1 and anti-programmed death-ligand 1 (PD-L1) blockade in patients with non-small-cell lung cancer profiled with targeted next-generation sequencing. J Clin Oncol 2018;36:633-41. [Crossref] [PubMed]
- Chalmers ZR, Connelly CF, Fabrizio D, et al. Analysis of 100,000 human cancer genomes reveals the landscape of tumor mutational burden. Genome Med 2017;9:34. [Crossref] [PubMed]
- Garofalo A, Sholl L, Reardon B, et al. The impact of tumor profiling approaches and genomic data strategies for cancer precision medicine. Genome Med 2016;8:79. [Crossref] [PubMed]
- Campesato LF, Barroso-Sousa R, Jimenez L, et al. Comprehensive cancer-gene panels can be used to estimate mutational load and predict clinical benefit to PD-1 blockade in clinical practice. Oncotarget 2015;6:34221-7. [Crossref] [PubMed]
- Evaluation of automatic class III designation for MSK - impact (Integrated Mutation Profiling of Actionable Cancer Targets) [Internet]. Available online: https://www.accessdata.fda.gov/cdrh_docs/reviews/DEN170058.pdf
- Oncomine TM Tumor Mutation Load Assay [Internet]. [cited 2018 May 9]. Available online: http://assets.thermofisher.com/TFS-Assets/CSD/Flyers/oncomine-tumor-mutation-load-assay-flyer.pdf
- Specimen Instructions. FoundationOne CDx, 2018. Available online: https://assets.ctfassets.net/vhribv12lmne/6ms7OiT5PaQgGiMWue2MAM/52d91048be64b72e73ffa0c1cab043c0/F1CDx_Specimen_Instructions.pdf
- Zehir A, Benayed R, Shah RH, et al. Mutational landscape of metastatic cancer revealed from prospective clinical sequencing of 10,000 patients. Nat Med 2017;23:703-13. [Crossref] [PubMed]
- Beattie J, Yarmus L, Wahidi M, et al. The Immune Landscape of Non-Small-Cell Lung Cancer. Utility of Cytologic and Histologic Samples Obtained through Minimally Invasive Pulmonary Procedures. Am J Respir Crit Care Med 2018;198:24-38. [Crossref] [PubMed]
- Hofman V, Lassalle S, Bence C, et al. Any Place for Immunohistochemistry within the Predictive Biomarkers of Treatment in Lung Cancer Patients? Cancers (Basel) 2018;10:70. [Crossref] [PubMed]
- Khagi Y, Kurzrock R, Patel SP. Next generation predictive biomarkers for immune checkpoint inhibition. Cancer Metastasis Rev 2017;36:179-90. [Crossref] [PubMed]
- Adalsteinsson VA, Ha G, Freeman SS, et al. Scalable whole-exome sequencing of cell-free DNA reveals high concordance with metastatic tumors. Nat Commun 2017;8:1324. [Crossref] [PubMed]
- Koeppel F, Blanchard S, Jovelet C, et al. Whole exome sequencing for determination of tumor mutation load in liquid biopsy from advanced cancer patients. PLoS One 2017;12:e0188174. [Crossref] [PubMed]
- Yang N, Li Y, Liu Z, et al. The characteristics of ctDNA reveal the high complexity in matching the corresponding tumor tissues. BMC Cancer 2018;18:319. [Crossref] [PubMed]
- Velcheti V, Kim ES, Mekhail T, et al. Prospective clinical evaluation of blood-based tumor mutational burden (bTMB) as a predictive biomarker for atezolizumab (atezo) in 1L non-small cell lung cancer (NSCLC): Interim B-F1RST results. J Clin Oncol 2018;36: abstr 12001.
- Teixidó C, Vilariño N, Reyes R, et al. PD-L1 expression testing in non-small cell lung cancer. Ther Adv Med Oncol 2018;10:1758835918763493. [Crossref] [PubMed]
- Ilie M, Juco J, Huang L, et al. Use of the 22C3 anti-programmed death-ligand 1 antibody to determine programmed death-ligand 1 expression in cytology samples obtained from non-small cell lung cancer patients. Cancer Cytopathol 2018;126:264-74. [Crossref] [PubMed]
- Kowanetz M, Zou W, Shames D, et al. OA20.01 Tumor Mutation Burden (TMB) is Associated with Improved Efficacy of Atezolizumab in 1L and 2L+ NSCLC Patients. J Thorac Oncol 2017;12:S321-2. [Crossref]
- Rizvi NA, Hellmann MD, Snyder A, et al. Mutational landscape determines sensitivity to PD-1 blockade in non–small cell lung cancer. Science 2015;348:124-8. [Crossref] [PubMed]
- Sun JX, He Y, Sanford E, et al. A computational approach to distinguish somatic vs. germline origin of genomic alterations from deep sequencing of cancer specimens without a matched normal. PLoS Comput Biol 2018;14:e1005965. [Crossref] [PubMed]
- Hiltemann S, Jenster G, Trapman J, et al. Discriminating somatic and germline mutations in tumor DNA samples without matching normals. Genome Res 2015;25:1382-90. [Crossref] [PubMed]
- Ptashkin RN, Mandelker DL, Coombs CC, et al. Prevalence of Clonal Hematopoiesis Mutations in Tumor-Only Clinical Genomic Profiling of Solid Tumors. JAMA Oncol 2018. [Epub ahead of print]. [Crossref] [PubMed]
- Chae YK, Anker JF, Bais P, et al. Mutations in DNA repair genes are associated with increased neo-antigen load and activated T cell infiltration in lung adenocarcinoma. Oncotarget 2017;9:7949-60. [PubMed]
- McGranahan N, Rosenthal R, Hiley CT, et al. Allele-Specific HLA Loss and Immune Escape in Lung Cancer Evolution. Cell 2017;171:1259-71.e11. [Crossref] [PubMed]
- Le DT, Durham JN, Smith KN, et al. Mismatch repair deficiency predicts response of solid tumors to PD-1 blockade. Science 2017;357:409-13. [Crossref] [PubMed]
- Łuksza M, Riaz N, Makarov V, et al. A neoantigen fitness model predicts tumour response to checkpoint blockade immunotherapy. Nature 2017;551:517-20. [PubMed]
- Long-Mira E, Washetine K, Hofman P. Sense and nonsense in the process of accreditation of a pathology laboratory. Virchows Arch 2016;468:43-9. [Crossref] [PubMed]
- Chassang G. The impact of the EU general data protection regulation on scientific research. Ecancermedicalscience 2017;11:709. [Crossref] [PubMed]
- Regulation (EU) 2016/679 of the European Parliament and of the Council of 27 April 2016 on the protection of natural persons with regard to the processing of personal data and on the free movement of such data, and repealing Directive 95/46/EC [Internet]. Available online: https://eur-lex.europa.eu/legal-content/EN/TXT/?uri=uriserv:OJ.L_.2016.119.01.0001.01.ENG


