Primary Cutaneous Adenoid-Cystic Carcinoma: A Case Report and Literature Review
*Corresponding Author(s):
K. OuallaDepartment Of Medical Oncology, Hassan II University, Fes, Morocco
Tel:+ 212 676610267,
Email:karimarauf@hotmail.com
Abstract
Primary Cutaneous Adenoid Cystic Carcinoma (PCACC) is a very rare adnexal skin tumor originating in the apocrine glands or modified apocrine glands but its precise histogenesis is still not well defined. It affects middle-aged and older individuals and arises usually in the head and neck area. The PCACC is considered to be an indolent disease with slow growth and rare distant metastases but with aggressive local behaviour. We report the case of 45 years old male, referred to our for a recurrent PCACC of the right axillary region.
The aim of this work is to underline the rarity of this disease, clinical, radiological and pathological features, as well as the treatment management and prognosis.
Keywords
Adenoid cystis carcinoma; Cutaneous location; Radiotherapy; Recurrence; Surgical excision
INTRODUCTION
Primary Cutaneous Adenoid-Cystic Carcinoma (PCACC) is a rare skin cancer with uncertain origin. It is characterized by slow expanding course, local aggressive behaviour, and low potential for distant metastasis and favorable survival for localized disease. Histologically it has cribriform pattern and may mimic other primary cutaneous tumors especially the adenoid basal cell carcinoma.
Wide local excision is the standard treatment and may be followed by radiation therapy in case of risk factor of recurrence.
CASE PRESENTATION
We report the case of 45 years old patient, who has in his medical history the resection of right axillary nodule in private clinic one year before. Histological examination revealed an adenoid cystic carcinoma with tumor free margins. The patient presented one year later a sub-cutaneous right axillary nodule in the same site of initial resection, growing slowly measuring 2cm, with firm consistency, unpainful, without any other symptoms. The patient was treated with wide local excision at private clinic then was referred to our department.
Histological examination showed a well-defined deep dermal nodule consisting of nests of basaloid cells with cribriform and tubular patterns and abundant mucin in the cysts in addition to perineural invasion. The margins were clear and the immunohistochemical stains proved positive for pan-cytokeratin AE1/AE3, PS100, estrogen receptors and P63 in few tumor cell nuclei, while it was negative for mammaglobin, CD117, HMB45, CK20 and CDX2.
These findings were suggestive of primary adnexal adenoid cystic carcinoma. Given the positivity of estrogen receptors, Breast MRI was peformed and showed no lesions in addition to a complete physical examination by an otolaryngologist that was normal. CT scan of the neck and thorax was performed and was normal. Pet CT-scan did not show any visible hypermetabolic lesion (Figure 1).
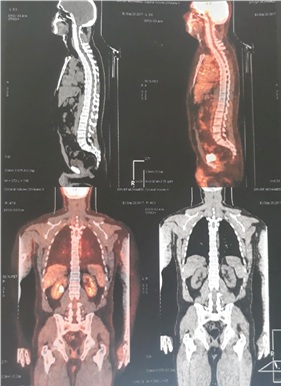
Figure 1(A, B): Pet-scan showing no evidence of hypermetabolic lesion.
Given the recurrent character of the lesion and the presence of perineural invasion, adjuvant radiotherapy was decided in the oncological multidisciplinary meeting. Patient is fully recovered without evidence of disease with a follow up of 8 months.
DISCUSSION
Primary Cutaneous Adenoid Cystic Carcinoma (PCACC) is a rare skin tumor that was classified as an adnexal skin tumor by the World Health Organization (WHO) [1]. The first case was described by Boggio in 1975 and only few cases of PCACC have been reported in the literature [2-7]. The exact origin of PCACC has not been determined if it is eccrine or apocrine, but the data were more suggestive of apocrine and modified apocrine origin.
The most common primary location of Adenoid Cystic Carcinoma (ACC) is the salivary glands in the head and neck region and may have an aggressive behaviour in this context. But other locations have been reported in the literature such as the lacrimal gland, prostate, lung, vulva, breast, external auditory canal, thymus, cervix, esophagus, and skin [8,9]. PCACC is characterized by indolent course but with frequent local recurrences within months to more than 20
years after initial diagnosis. Distant metastases are les common and have been reported to occur in 21% to 54% of cases, with predilection for lung, liver, bone, and brain respectively [10-12].
Naylor et al., reported that this tumor occurs mainly in middle-aged and older individual with a reported mean age of 59 years, and slight male predominance (57%) [13].
Histologically, PCACC is characterized by basaloid cells in the mid to deep dermis, arranged in lobules forming tubular structures giving the tumor a cribriform pattern with a lack of connection between the lobules and the epidermis [14,15]. Mucin can be found in small cystic spaces and also in the lumina of the tubular structures in addition to the surrounding stroma [14,15]. Regarding perineural invasion, they are found in approximately 50% of cases, while Mitotic figures and vascular invasion are rare [15-17]. At immunohistochemical analysis, PCACC was found to be positive for pan-cytokeratin AE1/AE2, Epithelial Membrane Antigen (EMA) and S100 in addition to amylase.
Positive staining for Carcinoembryonic Antigen (CEA) was also reported by some authors. Immunohistochemistry can help to make differential diagnosis especially with adenoid basal cell carcinoma but also with mucinous apocrine carcinoma and cribriform carcinoma [3,13]. Additional imaging explorations may be useful to exclude extracutaneous origin since the most common location of ACC is the salivary glands followed by other locations in head and neck region then other regions in the body.
The treatment management of for PCACC is mainly based on wide local excision with tumor-free margins established by permanent sections [3-14]. Adjuvant radiotherapy did not show any benefit in terms of survival and local control but it may be indicated in cases with risk factors of recurrence such as tumor-infiltrated margins and presence of perineural invasion [7]. Regarding chemotherapy, it is indicated only in patients with distant metastases [7,18,19].
For our case, he underwent a wide surgical excision followed by adjuvant radiotherapy because of the recurrent character of the tumor and the presence of perineural invasion and he is fully recovered after 8 months of follow up.
CONCLUSION
Skin is an uncommon site of Adenoid Cystic Carcinoma (ACC). The prompt recognition of PCACC is essential by integrating clinical and histopathological data for a correct diagnosis. The evolution after a wide local excision is favorable but a long-term follow-up of patients is important to establish given the long disease-free interval prior to local recurrences and metastases.
REFERENCES
- Dores GM, Huycke MM, Deversa SS, García CA (2010) Primary cutaneous adenoid cystic carcinoma in the United States: Incidence, survival, and associated cancers, 1976 to 2005. J Am Acad Dermatol 63: 71-77.
- Boggio R (1975) Adenoid cystic carcinoma of the scalp. Arch Dermatol 111: 793-794.
- van der Kwast TH, Vuzevski VD, Ramaekers F, Bousema MT, Van Joost T (1988) Primary cutaneous adenoid cystic carcinoma: case report, immunohistochemistry and review of the literature. Br J Dermatol 118: 567-577.
- Barnes J, Garcia C (2008) Primary cutaneous adenoid cystic carcinoma: a case report and review of the literature. Cutis 81: 243-246.
- Seab JA, Graham JH (1987) Primary cutaneous adenoid cystic carcinoma. J Am Acad Dermatolol 17: 113-118.
- Irvine AD, Kenny B, Walsh MY, Burrows D (1996) Primary Cutaneous Adenoid Cystic Carcinoma. Clin Exp Dermatol 21: 249-250.
- Kato N, Yasukawa K, Onozuka T (1998) Primary cutaneous adenoid cystic carcinoma with lymph node metastasis. Am J Dermatopathol 20: 571-577.
- McKee PH, Calonje E, Granter SR (2005) Pathology of the skin. 3rd ed. Philadelphia: Elsevier-Mosby; 2005. pp. 1653-1655.
- Lawrence JB, Mazur MT (1982), In: “Adenoid cystic carcinoma: a comparative pathologic study of tumors in salivary gland, breast, lung, and cervix,” Human Pathology, vol. 13, no. 10, pp. 916-924, 1982
- Fordice J, Kershaw C, El-Naggar A, Goepfert H (1999) Adenoid cystic carcinoma of the head and neck: predictors of morbidity and mortality. Arch Otolaryngol Head Neck Surg 1999 125: 149-152.
- van der Wal JE, Becking AG, Snow GB, van der Waal I (2002) Distant metastases of adenoid cystic carcinoma of the salivary glands and the value of diagnostic examinations during follow-up. Head Neck 24: 779-783.
- Spiro RH (1997) Distant metastasis in adenoid cystic carcinoma of salivary gland origin. Am J Surg 174: 495-498.
- Naylor EP, Sarkar CS, Giri PD, Gnepp DR, Robinson-Bostom L (2008) Primary cutaneous adenoid cystic carcinoma. Journal of the American Academy of Dermatology 58: 636-641.
- Headington T, Teears R, Niederhuber JE, Slinger RP (1978) Primary adenoid cystic carcinoma of skin. Archives of Dermatology 114: 421-424.
- Cooper PH, Adelson GL, Holthaus WH (1984) Primary cutaneous adenoid cystic carcinoma,” Archives of Dermatology 120: 774-777.
- Wick MR, Swanson PE (1986) Primary adenoid cystic carcinoma of the skin. a clinical, histological, and immunocytochemical comparison with adenoid cystic carcinoma of salivary glands and adenoid basal cell carcinoma. Am J Dermatopathol 8: 2-13.
- Chang SE, Ahn SJ, Choi JH, Sung KJ, Moon KC, et al. (1999) Primary adenoid cystic carcinoma of skin with lung metastasis. J Am Acad Dermatol 40: 640-642.
- Ikegawa S, Saida T, Obayashi H, Sasaki A, Esumi H, et al. (1989) Cisplatin combination chemotherapy in squamous cell carcinoma and adenoid cystic carcinoma of the skin, The Journal of Dermatology 16: 227-230.
- Lang PG Jr, Metcalf JS, Maize JC (1986) Recurrent adenoid cystic carcinoma of the skin managed by microscopically controlled surgery (Mohs surgery). The Journal of Dermatologic Surgery and Oncology 12, 395–398.
Citation: Oualla K, Acharfi N, Benbrahim Z, Arifi S, Bouhafa T, et al. (2019) Primary Cutaneous Adenoid-Cystic Carcinoma: A Case Report and Literature Review. Int J Case Rep Ther Stud 1: 008.
Copyright: © 2019 K. Oualla, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.