Health risk appraisals in Swedish occupational health services
Abstract
BACKGROUND: Health risk appraisals (HRAs) in occupational health services (OHS) in Sweden are very commonly used for health promotion issues, but not much research has explored the extent and nature of individual feedback that is provided.
OBJECTIVES: This study aimed to describe and explore HRAs in OHS regarding the content of the feedback in relation to the individual status and overall employee satisfaction.
METHODS: Feedback (evaluation and advice) and employee satisfaction with HRA were studied in employees that participated in health risk appraisals with a specific feedback session (HRA-F) (n = 272) and employees that participated in a single session (HRA-S) (n = 104). Associations between feedback and individual status concerning life style were assessed with Cohen’s kappa (k).
RESULTS: The employees received mainly information and advice for improvement on health and lifestyle issues (89–100%), while advice for improvement of working conditions was less common (15–59%). The feedback provided on life style was not based on individual status (k < 0.4), except for smoking and risky alcohol consumption (k > 0.55). A great majority of employees reported good overall satisfaction with their HRAs.
CONCLUSIONS: The evaluation and feedback given to employees after HRAs should be based more on HRA-results and advice could be focused more on work-related factors.
1Introduction
The general aims of Occupational Health Services (OHS) are to promote conditions for safe and healthy workplaces, health, well-being and work ability, as well as for prevention of ill-health and accidents [1, 2]. OHS has expertise concerning the interaction between work and health and plays a central role in public health, given that a large proportion of the working population has access to them. In some countries, OHS is (partly) financed by the social health care system, while in other countries they are privately financed, based on arguments that sustainable production is dependent on workers’ health and that an investment in OHS is cost-effective [1]. The activities of the OHS can be summarized into “surveillance of worker’s health and safety risks”, “information and education”, “preventive actions for management of health and safety hazards risks”, “diagnosis of occupational work-related diseases”, “general health care, curative and rehabilitation”, and “evaluation” [2]. One of the common services consists of health risk appraisals (HRAs) for the purpose of detecting early signs of illness and adverse lifestyle factors. Other purposes of HRAs are pre-employment surveillance [3], screening for the occurrence of stress in a company [4] or assessing the general health status in a special occupation [5]. HRAs are commonly performed as part of general health care as well, but OHS can also include working conditions in the assessment, thus adding an important dimension to health promotion in an occupational setting. These HRAs are initiated by the employer and seek to improve an employee’s health and work ability. HRAs should not be confused with health examinations required by occupational laws. Most OHS in Sweden use commercialized HRA methods consisting of self-administered questionnaires to monitor signs of illness, lifestyle factors (such as physical activity, tobacco and alcohol consumption, and nutritional habits), sleep, stress and physical and psychosocial working conditions [6, 7]. In addition to monitoring health and lifestyle factors with questionnaires, measurements of height, weight, and girth are often performed along with various laboratory tests (cholesterol levels, blood glucose, cardiopulmonary fitness, etc.). From these tests, OHS evaluate health, lifestyle and working conditions and employees receive advice and suggestions for improving one or more of the above factors. In this paper, such feedback is also referred to as ‘advice’ and ‘evaluation’. In Sweden, some OHS have a special feedback session one or two weeks after the HRA during which the results are reported to and discussed with the employee. This method is also referred to as an HRA with a feedback session (HRA-F), while HRAs that include assessment and evaluation during a single session are referred to as HRA-S.
It is important that there is congruence between individual status and the evaluation and advice that employees receive, if employees are to be guided more by facts about their condition than general beliefs. Employee satisfaction with OHS is important if a behavior change is warranted and has been proposed as a an important instrument for evaluating quality of OHS [8]. To the best of our knowledge, no studies have explored the extent and nature of individual feedback (evaluation and suggestions for improvement) by OHS and what is perceived by the receiver of such feedback. In a best case scenario, suggestions for improvement should be based on evidence and national guidelines, but the extent to which these guidelines are used remains unclear. Moreover, the degree of satisfaction with Swedish OHS efforts in the area of HRA is unknown.
1.1Aim
The aim of the study was to explore the content of the evaluation and advice that employees were given by OHS after their HRAs and as perceived by the employees, either with or without a special feedback session. Moreover, we wanted to analyze the congruence between individual status and the evaluations and advice concerning life style given by HRAs and factors associated with overall employee satisfaction with HRAs.
2Methods
2.1Study design
This is a explorative study concerning OHS efforts in the area of HRA. HRAs with or without feedback sessions (referred to as HRA-F and HRA-S) were examined. A questionnaire before an HRA was used to collect data concerning individual status with respect to health, lifestyle and working conditions. A second questionnaire was used after the HRA-F feedback session and immediately after the HRA-S to study the evaluation and advice that had been provided, along with overall satisfaction.
2.2Health Risk Appraisal with a Feedback Session (HRA-F)
The data was collected at one provider of OHS in the Stockholm area that was strategically selected out of an OHS network for research and education. The data collection was performed between 10 October 2011 and 22 January 2012, and included employees from more than 30 companies connected to this OHS. Employees were invited to participate in an HRA and a special feedback session 7–10 days later. During the feedback session, the OHS professional (occupational nurse, doctor or physical therapist) discussed the results of the HRAs with employees. Data were collected before the HRA by means of a questionnaire (Q1) filled out in the waiting room of the OHS, as well as a second questionnaire (Q2) after the specific feedback session. Both questionnaires were provided by the OHS. Moreover, data on the feedback provided by the OHS were obtained from their database (the employee’s medical records), in which OHS personnel had entered whether any advice had been given. These data were collected for all subjects who responded to Q1.
At the first session of the HRA-F, a one-hour health examination was performed, including a blood sample test on Hb, LDL cholesterol, HDL cholesterol, glucose and blood pressure. Moreover, a ‘health discussion’ was conducted that covered topics such as nutrition, physical activity and stress. Health status was recorded as a medical report. At the second session, health status, lifestyle factors and working conditions were evaluated and, if deemed necessary, specific advice for improvement in one or more of these areas was given. Notes about such advice were included in the medical report.
2.3Health Risk Appraisal with assessment and evaluation in one session (HRA-S)
Based on a strategic selection from our network, healthcare workers at six primary care units in the east central region of Sweden were asked to participate in an HRA-S during the October–December 2012 study period. The HRA-S was conducted by a provider of OHS at the workplace. Q1 was given to the employees by the researchers at an informational session 7–14 days before the HRA-S, while Q2 was provided by the OHS immediately after the HRA-S.
The HRA-S contained a standardized, self-administered questionnaire concerning physical and mental health (pain, medication and stress) and lifestyle factors (physical activity, smoking, alcohol consumption and sleeping habits), as well as a number of physical variables, such as BMI, percentage of fat-free mass and cardiopulmonary fitness (Åstrand test). At the end of the HRA-S, the results were discussed and individuals received oral feedback (evaluations and advice for improvement). The content of the HRA-S (the “health profile”) is described in previous reports [7, 6].
2.4Questionnaires
The questionnaires were given to participants at the OHS and returned in stamped, self-addressed envelopes to the researchers without involving the OHS. Q1 asked about current health status, lifestyle factors and working conditions of each employee. The various areas were assigned to three different sections in order to clarify the distinctions between them. Included was also a demographic section about individual factors such as age, gender, height and weight, number of years in the current occupation, educational level, marital status and children younger than 18. Q2 included similar sections that asked whether employees had received evaluations and advice for improvement in each area (health, lifestyle and working conditions) by the OHS at the second session of the HRA-F or during the HRA-S. Employees who responded affirmatively were asked to state whether they perceived the evaluations as positive (good health, healthy lifestyle and good working conditions) or negative (poor health, unhealthy lifestyle or poor working conditions). Q2 also asked about employee satisfaction with the feedback provided, as well as overall satisfaction with their HRAs.
2.5Subjects
During the study period, 524 employees had appointments at the OHS for an HRA-F. Before participating in the HRA-F, they received an invitation to fill out Q1 and participate in our study. Q1 was completed by 272 employees (52%), for whom medical data were collected. A total of 188 employees (69%) completed Q2. Of the 234 employees who were invited to an HRA-S, 150 participated and 104 choose to participate in the study by completing Q1 (69%). Due to logistical problems, not all of them were invited to fill out Q2. A total of 51 employees (49%) completed Q2. Logistical analyses using available demographic data concerning dropouts from Q1 and Q2 did not reveal any significant differences between participants and nonparticipants for either HRA-F or HRA-S.
2.6Variables and data treatment
Employees indicated whether the OHS had provided evaluations and advice for improvements in health, lifestyle factors and working conditions (Q2). The overall question concerning evaluations was worded as followed: “In relation to your health risk appraisal, did you receive any evaluation about 1) your health at present (physical status, weight, blood counts, etc.), or 2) your lifestyle (physical activity, nutrition, alcohol and tobacco consumption, etc.) or 3) working conditions (stress, ergonomics, organization, etc.). The employees were asked to choose between ‘no’, ‘yes, my health/lifestyle/working conditions were good,’ or ‘yes, my health/lifestyle/working conditions were not very good.’ If one of the latter alternatives was indicated, employees were asked to choose among several pre-formulated alternatives or enter their own. Multiple responses were allowed and subsequently assigned to subcategories. The overall question concerning advice for improvement was worded: “Did you receive any advice (suggestions) for improvement concerning your health, lifestyle or working conditions?” Employees were asked to choose between ‘yes’ and ‘no’ and state the advice or suggestions that they had received in their own words. These responses were subsequently assigned to various subcategories. Those who indicated that they had received an evaluation of their status or advice for improvement were asked to state whether they perceived the feedback as positive (‘Good’) or negative (‘Not Very Good’). Data in the medical records of employees about advice and suggestions for improvement were also assigned to these categories.
To assess lifestyle status, employees responded to several frequently used questions about tobacco and alcohol consumption, physical activity, nutritional habits and stress. The individual status for each area was subsequently classified as ‘Good’ or ‘Not Very Good’ based on previous cutoffs. Employees were asked whether they smoked tobacco or used snuff. They were classified as ‘smokers’ or ‘snuff users’ if they responded affirmatively about daily or irregular smoking/snuff use. Risky drinking was assessed based on three questions concerning alcohol consumption (AUDIT-C), a reliable short form of the Alcohol Use Disorders Identification Test (AUDIT), which includes frequency over the past 12 months, typical quantity and binge drinking, for a maximum score of 12 (responses ranging from 0–4, a higher score indicating a greater risk) [9–11]. The cutoffs for risky drinking were set at 6 for men and 4 for women in accordance with a recent validation study of AUDIT-C compared to full AUDIT in occupational health care [11]. As defined by Swedish recommendations, the employees were classified as being ‘physical inactive’ if they responded ‘less than 1 hour a week’ or ‘between 1 and 3 hours per week’ to the questions regarding the amount of hours with moderate or vigorous activity per week [12]. Based on an index of 0.07–6 that has previously been used in Swedish public health research, two questions explored nutritional habits in terms of vegetable, fruit and berry consumption, assessed as ‘inadequate’ (index <1.3) or ‘adequate’ (>1.3) [13]. The Shirom-Melamed Burnout Measure, consisting of 14 questions, was used to rate employees as ‘stressed out’ if they scored 4.0 or higher and ‘non-stressed out’ for ‘little’ or ‘not at all’ [14]. Finally, all employees were asked to rate their overall satisfaction with the HRA as ‘Good’, ‘Neither Good Nor Poor’ or ‘Poor.’
2.7Statistical analyses
The percentage of respondents who received evaluations or advice was calculated separately for each area (health, lifestyle and working conditions) by dividing the number of employees who responded in the affirmative by the total number of responses to that particular question. A test of proportions (Chi2) was used to determine whether there were any significant (p < 0.05) differences between the various areas with respect to received evaluation or advice in accordance with self-reporting (HRA-F and HRA-S) and documentation by the OHS in medical records (HRA-F). The degree of congruence between the current status of lifestyle factors (‘Good’ vs. ‘Not Very Good’) and an affirmative or negative response to the question of whether advice for improvement of lifestyle factors had been received was calculated with Cohen’s kappa [15] based on cross-tabulations (2×2 tables). A Cohen’s Kappa coefficient (κ) > 0.8 was interpreted as a ‘very strong association,’ while a κ> 0.6 was interpreted as a ‘strong association’ and a κ> 0.4 as an ‘acceptable association.’ Cohen’s Kappa coefficients < 0.4 were interpreted as ‘no association’ [15]. Moreover, the percentage of respondents who indicated good overall satisfaction was calculated for both HRA-F and HRA-S and an analysis was performed as to study whether good overall satisfaction was associated to evaluation or advice in the various areas of interest, or related to ‘positive or negative’ feedback, using Chi2 tests. SPSS statistical software (IBM Corp, release 22.0.0 for Windows) was used to analyze the data.
2.8Ethics
Consent was obtained from all employees and OHS personnel who participated, and the regional ethics committee in Stockholm approved the study in advance (DNR: 2011/417- 31/5).
3Results
The participation and demographics of the subjects participating in HRA-F and HRA-S and answering Q1 and Q2 is presented in Table 1. HRA participants were typically women of around 45 years of age with steady jobs. Subjects participating in HRA-F were employees from more than 30 private companies (64% women), while the subjects participating in HRA-S were employees (94% women) working in public health care.
3.1Reported evaluation of health, lifestyle and working conditions
Almost all employees reported that their health (99–100%) and lifestyle factors (99% and 98% for HRA-F and HRA-S respectively) had been evaluated (Figs. 1 and 2), and this was significantly higher than the evaluation of working conditions (72% and 51% for HRA-F and HRA-S respectively) (p < 0.05). According to the medical records, for nearly all employees there were records that the employees received evaluations of health and lifestyle factors after their HRA-F, but there were in total only two evaluations of working conditions identified: one on the occurrence of dust and one on the occurrence of whole body vibrations.
Approximately three out of every four employees who received evaluations reported after the feedback session (HRA-F) that the evaluation of their health (74%) and working conditions (75%) had been positive, indicating low risk for future health and job-related problems. However, only 50% of the employees who received evaluations reported after HRA-F that lifestyle factors had been positive, and this was significantly lower than the evaluations of health and working conditions (p < 0.001). The corresponding proportions for HRA-S were 31% positive evaluation of health, 25% positive evaluation of lifestyle factors and 58% positive evaluation of working conditions.
3.2Reported advice for improvement of health, lifestyle and working conditions
Approximately four out of every five employees received advice for improvement of health after a negative evaluation during HRA-F and HRA-S (Figs. 1 and 2). Somewhat higher proportions were found concerning advice for lifestyle improvement after a negative evaluation. For working conditions, these proportions were 63% for HRA-F and 91% for HRA-S. When calculating proportions of employees who received an evaluation, advice was given to 26%, 50%, and 17% for health, lifestyle and working conditions respectively during HRA-F (Fig. 1), and 55%, 65% and 38% respectively during HRA-S (Fig. 2).
3.3Content of evaluation and advice for improvement of health, lifestyle and working conditions
The content of evaluations of health, lifestyle and working conditions is shown in Table 2. For HRA-F, the two most frequent categories in the domain health were weight and blood counts. In the lifestyle domain, the two most frequently mentioned categories were physical activity and nutritional habits, and the most frequently mentioned category concerning working conditions was ergonomics. The employees at HRA-S reported that the evaluation of physical activity and nutritional habits were most frequent for the domains health and lifestyle. In terms of working conditions, the most frequent evaluation after an HRA-F and HRA-S considered aspects of stress on the job.
The two most frequent kinds of advice and suggestions for improvement concerning health issues were nutritional counseling and physical activity. They were also mentioned in connection with advice and suggestions for improvement of lifestyle factors. When it came to working conditions, the primary advice for improvement involved ergonomics (Table 2).
3.4Evaluation and advice concerning lifestyle factors in relation to individual status
For employees who participated in HRA-F, there was a good (acceptable) association between self-reporting of having risky drinking behavior and the behavior having been evaluated, both self-reported and as documented by the OHS in the medical records, as well as having received alcohol counseling (0.56 < κ< 0.58) (Table 3). For those who participated in HRA-S, there was a strong association between self-reported tobacco consumption and its having been evaluated (Cohen’s kappa coefficient κ= 0.76), as well as for having received advice on tobacco cessation (κ= 0.67) (Table 3). For other self-reported lifestyle factors, Cohens’ kappa coefficients were below 0.4, indicating that there was no association between individual status and corresponding evaluations during HRAs as reported by employees (Q2) or documented in the medical records. Similarly, there were no associations between individual status and corresponding advice for lifestyle improvements (κ< 0.4).
3.5Satisfaction with health risk appraisals
A great majority of employees reported good overall satisfaction with their HRAs. A total of 91% reported good overall satisfaction after an HRA-F, while 73% reported good overall satisfaction after an HRA-S. None of the employees indicated dissatisfaction with their HRAs. Additional analyses (Chi2) showed that overall satisfaction was unrelated to whether the HRA-F/HRA-S results were ‘positive’ or ‘negative’ (p > 0.05).
4Discussion
A general aim of the study was to describe and explore health risk appraisals (HRAs) at occupational services (OHS) in Sweden. More specifically, we wanted to examine the content of the evaluation and advice in relation to the individual status, as well as overall employee satisfaction.
4.1Summary of main results
Almost all employees reported that their health status and lifestyle had been evaluated, but they were less likely to report that they had received an evaluation of their working conditions. Advice for improvements of health and lifestyle was given to the majority of respondents with a negative evaluation, mainly concerning nutrition and physical activity. Fewer employees reported that they had received advice for improvement of working conditions. In general, advice for improvement was not related to individual status, with the exception of alcohol and tobacco consumption. Employees were highly satisfied with their HRAs.
4.2Evaluation and advice
Most individual evaluation and advice for improvement in health and lifestyle factors concerned physical activity and nutritional habits. Responses to the open-ended questions were categorized manually; the results showed that employees had difficulty making distinctions between evaluation and advice on health and lifestyle despite the use of different sections in the questionnaires. This inability might be due to the fact that most suggestions for improving health involved lifestyle factors. As Table 3 shows, these suggestions were provided independently of whether health had been evaluated positively or negatively. In other words, the OHS seems to fail to give specific individual adapted advice, but leaves it at a general level. Previously, the effects of this kind of individual general advice about lifestyle had been called into question [16].
Review studies revealed that HRA results can be effectively used to adapt specific workplace interventions to the individual status of the employee, as opposed to interventions that are intended for all employees without a prior health examination [17–19]. For example, the use of workplace-based group counseling and educational programs [20–22], as well as policy and environmental modifications [22, 23] after a workplace-based health examination, has been shown to be effective in changing risky behavior (nutrition and physical activity) and health outcomes (body fat, etc.). Providing information about health, lifestyle and working conditions to the individual could increase motivation to change adverse lifestyles, but using this information to initiate individualized interventions seems to be a more effective strategy. In accordance with our results, a recent critical review showed that the OHS focused primarily on preventing disease rather than promoting positive measures of health [19]. In addition, most studies in this review found that the OHS interventions were not directed to change the workplace, but rather used the workplace as a convenient setting for reaching people to change their behavior related to lifestyles and disease prevention [19]. High kappa values were identified for alcohol (HRA-F) and tobacco (HRA-S) consumption, indicating that advice had been properly adapted to those who needed suggestions for improvement; this could serve as an example to help OHS implement their HRA efforts.
4.3Satisfaction
Similar to a previous literature study by Hulshoff (1999), this study found a high proportion of satisfied employees [8]. It is important that employees are confident about their HRAs since high satisfaction promotes compliance with therapy and advice for behavioral changes [24]. In this study, the employees received more information and advice for improvement than expected (data not shown), which might be one reason for the high level of satisfaction. However, satisfaction was unrelated to the areas of interest (health, lifestyle and working conditions) or the outcome of the HRA (‘positive’ or ‘negative’). Thus, OHS do not have to alter their evaluation and advice in order to please employees.
4.4Strengths and limitations of the study
One strength of the present study is that two different HRAs and two different study populations were examined: employees who participated in an HRA-F were mainly a ‘mixed’ study population with regard to gender and profession, while those who participated in an HRA-S were women employed in primary health care. The present data offered the opportunity of providing direct feedback to OHS personnel about understanding the evaluation and advice given, thereby highlighting some of the communication difficulties associated with the HRA methods used by the OHS.
One limitation of the present study is that primarily self-reported data on health, lifestyle habits and working conditions was used. However, data from medical records after the HRA-F were also taken into account and the results did not differ from self-reported evaluation and advice on health and lifestyle. However, not much was written down about working conditions. Another limitation of the study is the validity of the questionnaires, even though many of the items and cutoffs are commonly used and have been validated in other populations [7, 6, 13, 14]. An important methodological issue that needs to be discussed when studying OHS efforts in the area of HRA is that participation is a highly selective process. In the present study, several types of ‘drop-outs’ were identified at various stages. Several employees did not respond to the initial invitation to participate in their HRAs. According to the OHS, around 15% and 36% of them did not participate in their HRA-F and HRA-S respectively. Previous studies have shown that nonparticipants are overrepresented by males, ‘poor health’ and ‘poor lifestyle habits’, as well as lower work ability than those who participate in HRAs [25]. We were unable to explore whether these previous predictors of nonparticipation were present in the present study, but that would appear to have been the case, given that the percentage of participants with a ‘negative’ evaluation of health-related factors was low. Moreover, a relatively high percentage of employees who participated in an HRA did not choose to be involved in the present study (Q1). There were, however, no systematic differences between participants and nonparticipants. Thus, it appears unlikely that the results were skewed due to these non-respondents. Finally, a large number of employees in the HRA-S group who participated in Q1 were unable to participate in Q2. As the OHS changed their routines during the study-period, some of the subjects were not invited to participate in Q2, but there was no systematic drop-out and the nonparticipants did not differ from participants in any of the variables that were available from Q1. Since the general aim of the study was to explore and describe the OHS effort in the area of HRA, nonsystematic loss of data could not have influenced the results to a very great extent.
In accordance with previous studies, this study showed that OHS survey employees concerning health and lifestyle factors, but with a limited focus on working conditions, despite their specific knowledge about conditions at the companies involved [19]. An important lesson for OHS from this study is that they should try to relate their knowledge about the employees’ working conditions to the results of HRS in order to initiate workplace interventions. Future studies should focus on the effects of workplace interventions that are more closely related and adapted to evaluation reports from HRAs.
4.5Conclusions
This study showed that employees state that evaluation and advice after an HRA in an occupational setting mainly concerns health and lifestyle issues, and that working conditions are given less consideration. Evaluation and advice after an HRA were not only based on individual status, suggesting that there is room for improvement to the efforts of Swedish OHS in the area of HRAs. As OHS are experts on the interaction between work and health, we believe that the OHS could use the results of HRAs to initiate individualized interventions that emphasize working conditions.
Conflict of interest
The authors declare that they have no competing interests.
Authors’ contributions
WG, MF, KK, AT and MS have been involved in the conception and design of the study. WG performed the acquisition of data. MM and BOÄ performed the analysis and interpretation of data. All authors have contributed with intellectual content in the study. All authors have read and approved the final manuscript.
Acknowledgments
This study was funded by AFA and Karolinska Institutet. Special thanks to Jacob Sejersen and Felicia Fixell for their help. The authors declare that they have no competing interests with any of the OHS studied.
References
[1] | Torp S , Eklund L , Thorpenberg S . Research on workplace health promotion in the Nordic countries: A literature review, 1986-2008. Glob Health Promot (2011) ;18: (3):15–22. doi: 10.1177/1757975911412401 |
[2] | Rantanen J . Basic occupational health services - their structure, content and objectives. Scand J Work Env Hea (2005) :5–15. |
[3] | McHugh C , Gibson L . Pre-placement screenings: An exploratory study of their use in a sample of New South Wales workplaces. Work-a Journal of Prevention Assessment & Rehabilitation (2011) ;40: (2):187-94. doi: 10.3233/Wor-2011-1219 |
[4] | Holton MK , Barry AE , Chaney JD . Employee stress management: An examination of adaptive and maladaptive coping strategies on employee health. Work (2015) . doi: 10.3233/WOR-152145 |
[5] | Apostolopoulos Y , Sonmez S , Shattell MM , Gonzales C , Fehrenbacher C . Health survey of U.S. long-haul truck drivers: Work environment, physical health, and healthcare access. Work (2013) ;46: (1):113–23. doi: 10.3233/WOR-121553 |
[6] | Malmgren S . A health information campaign and Health Profile Assessment as revelatory Communication. Medical Dissertations. Linköping University: (1987) . |
[7] | Andersson G . Betydelsen av regelbunden motion för sjukfrånvaro och upplevd hälsa. Linköping University: (1989) . |
[8] | Hulshof CT , Verbeek JH , van Dijk FJ , van der Weide WE , Braam IT . Evaluation research in occupational health services: General principles and a systematic review of empirical studies. Occup Environ Med (1999) ;56: (6):361–77. |
[9] | Bradley KA , McDonell MB , Bush K , Kivlahan DR , Diehr P , Fihn SD . The AUDIT alcohol consumption questions: Reliability, validity, and responsiveness to change in older male primary care patients. Alcohol Clin Exp Res (1998) ;22: (8):1842–9. doi:00000374-199811000-00034 [pii]. |
[10] | Bush K , Kivlahan DR , McDonell MB , Fihn SD , Bradley KA . The AUDIT alcohol consumption questions (AUDIT-C): An effective brief screening test for problem drinking. Ambulatory Care Quality Improvement Project (ACQUIP). Alcohol Use Disorders Identification Test. Arch Intern Med (1998) ;158: (16):1789–95. |
[11] | Kaarne T , Aalto M , Kuokkanen M , Seppa K . AUDIT-C, AUDIT-3 and AUDIT-QF in screening risky drinking among Finnish occupational health-care patients. Drug Alcohol Rev (2010) ;29: (5):563–7. doi: DAR172 [pii] 10.1111/j.1465-3362.2010.00172.x |
[12] | Jansson E , Anderssen SA . Kapitel 2. Allmänna rekommendationer om fysisk aktivitet. In: Agneta Ståhle, Yrkesföreningar_för_fysisk_aktivitet, editors. FYSS 2008 - Fysisk aktivitet i sjukdomsprevention och sjukdomsbehandling. Stockholm: Elander; 2008. pp. 38–46. |
[13] | Boström G , Nyqvist K . Questionnaires about physical activity and diet (in Swedish). Health in equal terms - objective and background of the questions in the national public health survey. Vol. 02. Gothenburg: Swedish National Institute of Public Health; (2010) . |
[14] | Lundgren-Nilsson A , Jonsdottir IH , Pallant J , Ahlborg G . Internal construct validity of the Shirom-Melamed Burnout Questionnaire (SMBQ). BMC Public Health (2012) ;12. doi: Artn 1, Doi; 10.1186/1471-2458-12-1 |
[15] | Cohen J . Weighted kappa: Nominal scale agreement with provision for scaled disagreement or partial credit. Psychol Bull (1968) ;70: (4):213–20. |
[16] | Socialstyrelsen. Nationella riktlinjer för sjukdomsförebyggande metoder 2011 (in Swedish) http://www.socialstyrelsen.se/publikationer2011/2011-11-11. (2011) . Accessed 21-01-2016. |
[17] | Cashman CM , Ruotsalainen JH , Greiner BA , Beirne PV , Verbeek JH . Alcohol and drug screening of occupational drivers for preventing injury. The Cochrane Database of Systematic Reviews (2009) ;(2):CD006566. doi:10.1002/14651858.CD006566.pub2 |
[18] | Soler RE , Leeks KD , Razi S , Hopkins DP , Griffith M , Aten A , et al . A systematic review of selected interventions for worksite health promotion. The assessment of health risks with feedback. American Journal of Preventive Medicine (2010) ;38: (2 Suppl):S237–62. doi:S0749-3797(09)00752-1 [pii] 10.1016/j.amepre.2009.10.030 |
[19] | Torp S , Vinje HF . Is workplace health promotion research in the Nordic countries really on the right track? Scand J Public Healt (2014) ;42: :74–81. doi: 10.1177/1403494814545106 |
[20] | Cancelliere C , Cassidy JD , Ammendolia C , Cote P . Are workplace health promotion programs effective at improving presenteeism in workers? A systematic review and best evidence synthesis of the literature. BMC Public Health (2011) ;11: :395. doi: 1471-2458-11-395 [pii] 10.1186/1471-2458-11-395 |
[21] | Groeneveld IF , Proper KI , van der Beek AJ , Hildebrandt VH , van Mechelen W . Lifestyle-focused interventions at the workplace to reduce the risk of cardiovascular disease–a systematic review. Scand J Work Environ Health (2010) ;36: (3):202–15. doi:2891 [pii] |
[22] | Maes L , Van Cauwenberghe E , Van Lippevelde W , Spittaels H , De Pauw E , Oppert JM , et al. Effectiveness of workplace interventions in Europe promoting healthy eating: A systematic review. Eur J Public Health (2011) ;22: (5): 677–83. doi:ckr098 [pii] 10.1093/eurpub/ckr098 |
[23] | To QG , Chen TT , Magnussen CG , To KG . Workplace physical activity interventions: A systematic review. American journal of health promotion: AJHP (2013) ;27: (6):e113–23. doi:10.4278/ajh120425-LIT-222 |
[24] | Jin J , Sklar GE , Min Sen Oh V , Chuen Li S . Factors affecting therapeutic compliance: A review from the patient’s perspective. Ther Clin Risk Manag (2008) ;4: (1):269–86. |
[25] | Robroek SJ , van Lenthe FJ , van Empelen P , Burdorf A . Determinants of participation in worksite health promotion programmes: A systematic review. Int J Behav Nutr Phys Act (2009) ;6: :26. doi:1479-5868-6-26 [pii] 10.1186/1479-5868-6-26 |
Figures and Tables
Fig.1
Evaluation and Advice. Number of employees who indicated that they had received a ‘positive’ or ‘negative’ evaluation and advice for improvement after an HRA including a specific feedback session 7–10 days later (HRA-F).
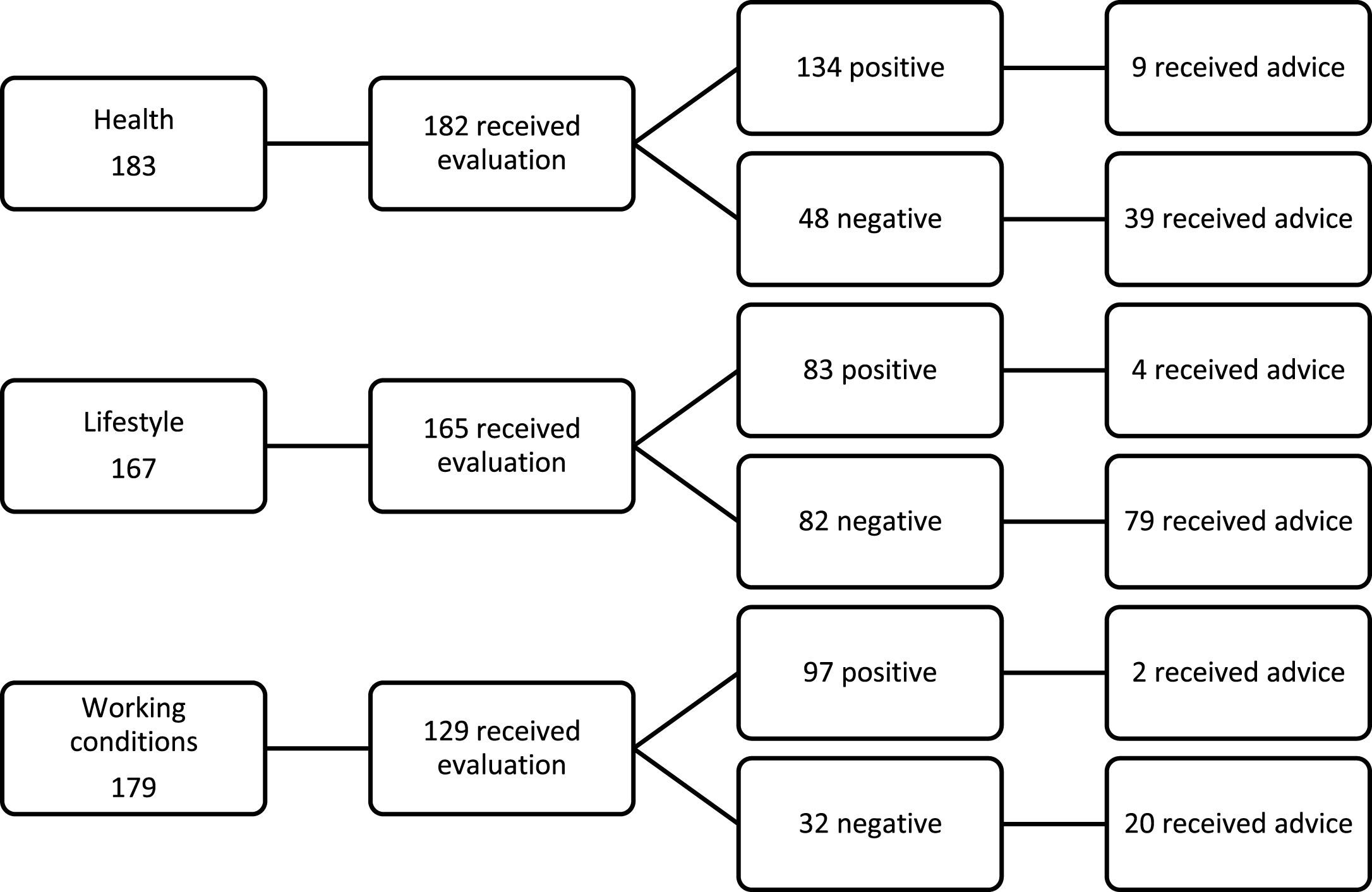
Fig.2
Number of employees who indicated that they had received a ‘positive’ or ‘negative’ evaluation and advice for improvement after a single-session HRA (HRA-S).
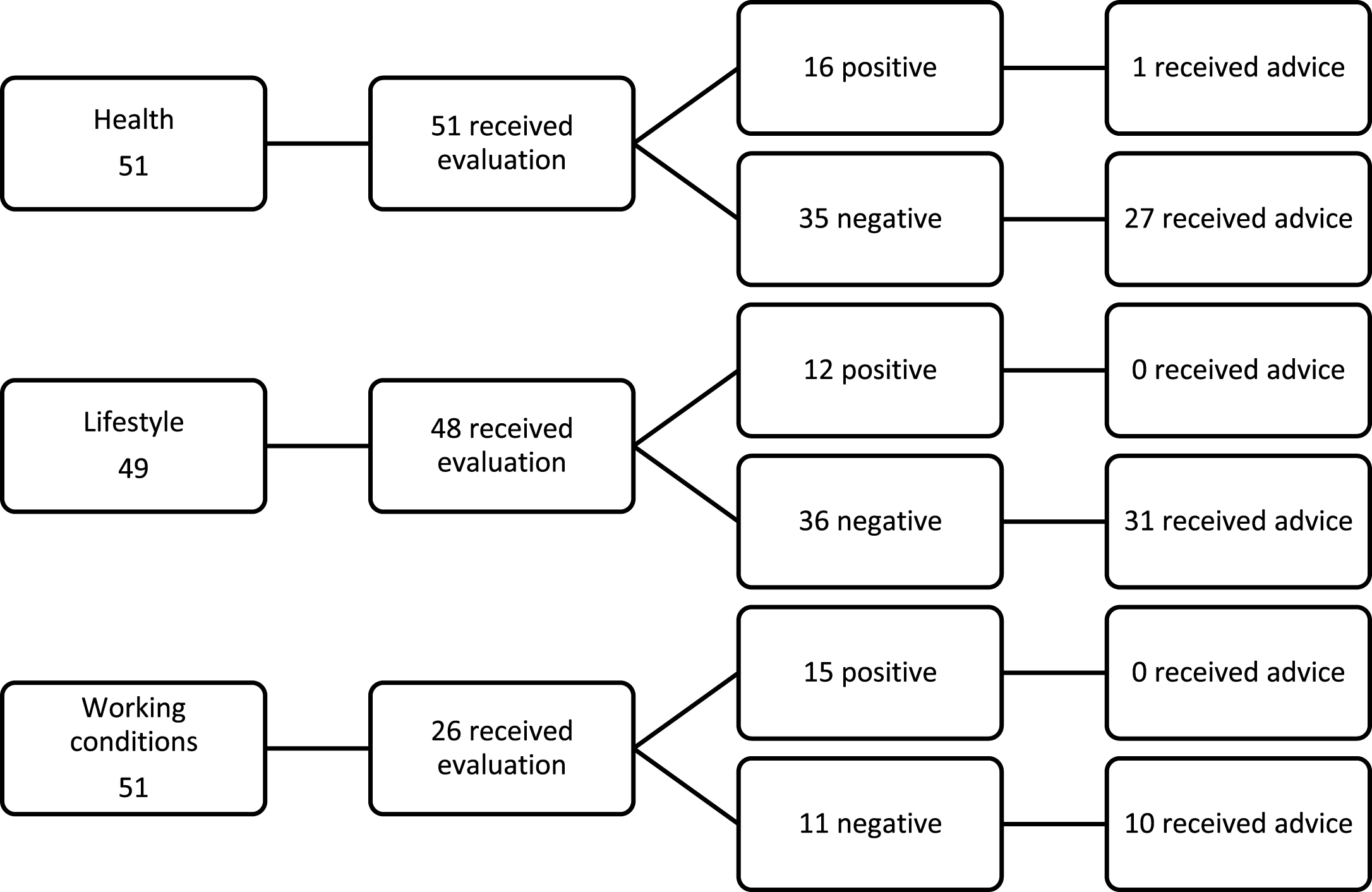
Table 1
Participation and demographics of the subjects. Expectations of evaluations and advice. Evaluations: The number (n) and percentage of employees (%) who expected that their health, lifestyle and/or working conditions would be evaluated. Advice: The number and percentage of employees who expected that they would receive advice and suggestions to improve their health, lifestyle and/or working conditions
| HRA-F | HRA-S | ||
| Number of participants | Unknown number of | 234 were asked to | |
| invited to HRA | participants that were | participate in the HRA-S | |
| asked to participate in | |||
| the HRA-F | |||
| Number of participants asked to fill | 524 came to the OHS | 150 participated and | |
| in the questionnaires | and were asked to | were asked to answer the | |
| answer the | questionnaires | ||
| questionnaires | |||
| Q1 | N | 272 | 104 |
| Female (%) | 64% | 94% | |
| Age | Mean and Standard deviation (SD) | 44.5 (11.5) | 46.8 (10.5) |
| Years in same profession | Mean and Standard deviation (SD) | 13.5 (10.2) | 19.1 (12.9) |
| Married (%) | 78% | 85% | |
| Q2 | N | 188 | 51 d |
| Female (%) | 62% | 100% | |
| Age | Mean and Standard deviation (SD) | 45.8 (12.0) | 46.0 (10.4) |
| Years in same profession | Mean and Standard deviation (SD) | 15.1 (12.2) | 18.7 (13.3) |
| Married (%) | 77% | 87% |
Q1: Questionnaire 1. Q2: Questionnaire 2.
Table 2
Evaluation and advice for improvement – areas of interest. The number of employees (n) and corresponding percentage (%) out of the total number of employees who responded to questions about evaluations received in the various areas of health, lifestyle and working conditions on Q2 after an HRA-F and HRA-S. The content of advice in the various areas of health, lifestyle and working conditions, and the corresponding percentages of the total amount of advice reported by employees on Q2 after an HRA-F and HRA-S. Questions about the specific content of advice provided during HRAs were open-ended. Responses to these questions were categorized. One employee could report multiple pieces of advice such that the total amount of advice in the area of lifestyle exceeded the number of employees
| EVALUATION | ADVICE1) | ||||||||||||
| HRA-F | HRA-S | HRA-F | HRA-S | ||||||||||
| n | % | Tot | n | % | Tot | n | % | Tot | n | % | Tot | ||
| Health | Health | ||||||||||||
| Weight | 31 | 17 | 185 | 22 | 48 | 46 | Weight counseling | 5 | 6 | 84 | 7 | 17 | 42 |
| Blood2) | 24 | 13 | 185 | 17 | 37 | 46 | Blood parameter advice | – | 84 | 6 | 14 | 42 | |
| Physical status3) | 5 | 3 | 185 | 15 | 33 | 46 | Physical activity advice | 25 | 30 | 84 | 11 | 26 | 42 |
| Sleep | – | – | – | – | 46 | Nutrition counselling | 30 | 36 | 84 | 14 | 33 | 42 | |
| Hearing/eyesight | – | – | – | – | 46 | Referral to medical center | 17 | 20 | 84 | 4 | 10 | 42 | |
| Specific diseases4) | – | – | – | – | 46 | Stress management | 2 | 2 | 84 | – | – | 42 | |
| Stress-related symptoms | – | – | 185 | 3 | 7 | 46 | Tobacco cessation | 1 | 1 | 84 | – | – | 42 |
| Musculoskeletal symptoms | 4 | 2 | 185 | 7 | 15 | 46 | Alcohol detox | 3 | 4 | 84 | – | – | 42 |
| Other | 10 | 5 | 185 | 17 | 37 | 46 | Other | 1 | 1 | 84 | – | – | 42 |
| Lifestyle | Lifestyle | ||||||||||||
| Physical Activity | 58 | 31 | 185 | 21 | 46 | 46 | Physical activity advice | 62 | 38 | 164 | 24 | 46 | 52 |
| Tobacco use5) | 15 | 8 | 185 | 7 | 15 | 46 | Tobacco cessation5) | 15 | 9 | 164 | 5 | 10 | 52 |
| Alcohol consumption | 12 | 6 | 185 | 0 | 0 | 46 | Alcohol detox | 13 | 8 | 164 | – | 52 | |
| Stress | 17 | 9 | 185 | 17 | 37 | 46 | Stress management | 13 | 8 | 164 | 6 | 12 | 52 |
| Nutritional habits | 58 | 31 | 185 | 10 | 22 | 46 | Counselling for reduced | 8 | 5 | 164 | 6 | 12 | 52 |
| musculoskeletal symptoms | |||||||||||||
| Nutrition counseling | 53 | 32 | 164 | 11 | 21 | 52 | |||||||
| Working conditions | Working conditions | ||||||||||||
| Ergonomics6) | 11 | 6 | 185 | – | 46 | Ergonomic advisory6) | 9 | 38 | 24 | 7 | 37 | 19 | |
| Stress7) | 8 | 4 | 185 | 8 | 17 | 46 | Stress management7) | 4 | 17 | 24 | 3 | 16 | 19 |
| Physical environment8) | 6 | 3 | 185 | 4 | 9 | 46 | Physical environment advice8) | 4 | 17 | 24 | 2 | 11 | 19 |
| Organizational issues9) | 6 | 3 | 185 | – | – | 46 | Organizational management consultance9) | 6 | 25 | 24 | 3 | 16 | 19 |
| Threats and violence10) | – | – | 185 | – | – | 46 | Threats and violence10) | – | – | 24 | – | – | 19 |
| Other | 1 | 1 | 185 | 1 | 2 | 46 | Other | 1 | 4 | 24 | 4 | 21 | 19 |
1) Questions about the specific content of advice provided during HRAs were open-ended. Responses to these questions were categorized accordingly. One employee could report multiple pieces of advice such that the total amount of advice in the area of lifestyle exceeded the number of employees; 2) Systolic/diastolic blood pressure, glucose and/cholesterol levels; 3) e.g. VO2max estimated with Åstrand sub-maximal cycle test; 4) e.g. diabetes mellitus; 5) Smoking and/or snuff use; 6) Physical workload, static muscle activity, sedentary work; 7) Work-related psychosocial factors and concerns; 8) Climate, noise; 9) Enough personnel or time to perform duties; 10) Bullying.
Table 3
Cross-tabulations between life style factors and evaluation and advice received. Cohen’s Kappa coefficients (κ) for associations between life style factors (‘Good’, and ‘Not Very Good’) according to self-reporting before HRA-F and HRA-S (using Q1) and evaluation and advice received for improvement in variables of lifestyle (Q2), and evaluation and advice for improvement as documented in the medical records after an HRA-F
| HRA-F | HRA-S | ||||||||||
| Lifestyle factors: | Good | Not Very | Good | Not Very | |||||||
| Good | Good | ||||||||||
| Yes | No | Yes | No | Kappa | Yes | No | Yes | No | Kappa | ||
| Physical | Q2: Indiv. evaluation | 20 | 78 | 34 | 40 | 0.264 | 9 | 21 | 10 | 6 | 0.311 |
| activity (Q1) | Q2: Advice | 23 | 75 | 35 | 39 | 0.245 | 12 | 18 | 21 | 25 | 0.151 |
| Medical record: Advice | 15 | 75 | 22 | 50 | 0.146 | – | – | – | – | – | |
| Tobacco (Q1) | Q2: Indiv. evaluation | 0 | 113 | 14 | 46 | 0.284 | 0 | 37 | 6 | 3 | 0.763 |
| Q2: Advice | 0 | 113 | 14 | 46 | 0.284 | 0 | 37 | 5 | 4 | 0.668 | |
| Medical record: Advice | – | – | – | – | – | – | – | – | – | – | |
| Alcohol (Q1) | Q2: Indiv. evaluation | 2 | 154 | 8 | 4 | 0.708 | 0 | 44 | 0 | 1 | 0 |
| Q2: Advice | 4 | 152 | 7 | 5 | 0.58 | 0 | 44 | 0 | 1 | 0 | |
| Medical record: Advice | 2 | 143 | 6 | 6 | 0.574 | – | – | – | – | – | |
| Stress (Q1) | Q2: Indiv. evaluation | 14 | 149 | 2 | 7 | 0.1 | 16 | 29 | 0 | 1 | 0.043 |
| Q2: Advice | 11 | 152 | 2 | 7 | 0.128 | 6 | 39 | 0 | 1 | –0.04 | |
| Medical record: Advice | 10 | 143 | 1 | 8 | 0.041 | – | – | – | – | – | |
| Smoking (Q1) | Q2: Indiv. evaluation | 2 | 131 | 12 | 27 | 0.378 | 1 | 39 | 5 | 1 | 0.808 |
| Q2: Advice | 2 | 131 | 12 | 27 | 0.378 | 0 | 40 | 5 | 1 | 0.897 | |
| Medical record: Advice | 0 | 126 | 4 | 31 | 0.168 | – | – | – | – | – | |
| Nutrition (Q1) | Q2: Indiv. evaluation | 30 | 95 | 27 | 20 | 0.314 | 9 | 33 | 1 | 3 | 0.021 |
| Q2: Advice | 29 | 96 | 23 | 24 | 0.249 | 10 | 32 | 1 | 3 | 0.007 | |
| Medical record: Advice | 38 | 77 | 28 | 18 | 0.246 | – | – | – | – | – | |
Q1: Questionnaire 1. Q2: Questionnaire 2.



