Addition of TyG index to the GRACE score improves prediction of adverse cardiovascular outcomes in patients with non-ST-segment elevation acute coronary syndrome undergoing percutaneous coronary intervention: A retrospective study
- Department of Cardiology, The First Affiliated Hospital of Zhengzhou University, Zhengzhou, China
Background: The Global Registry of Acute Coronary Events (GRACE) score is a widely recognized tool for predicting adverse cardiovascular events in patients with non-ST-segment elevation acute coronary syndrome (NSTE-ACS). The triglyceride-glucose index (TyG index) is a new biomarker of insulin resistance and has a close association with the occurrence of adverse cardiovascular events. We investigated whether the addition of the TyG index to the GRACE score could improve prognosis prediction in patients with NSTE-ACS undergoing percutaneous coronary intervention (PCI).
Methods: In total, 515 patients with NSTE-ACS undergoing PCI were included in this retrospective study. Kaplan-Meier analysis was performed to describe the cumulative incidence of the primary endpoint based on the median TyG index. The relationship between the TyG index and GRACE score was analyzed using Spearman's rank correlation. Univariate and multivariate Cox proportional hazards analyses were used to identify independent risk factors. Based on the receiver operating characteristic curve, net reclassification improvement (NRI), integrated differentiation improvement (IDI), and decision curve analysis, the TyG index was evaluated for its predictive value when added to the GRACE score. ROC curve analyses, NRI, and IDI were used to compare the gain effect of the TyG index and the levels of HbA1C, FBG, TG, and LDL-C on the GRACE score for predicting adverse cardiovascular events.
Results: The TyG index was an independent predictor of 2-year adverse cardiovascular events in patients with NSTE-ACS undergoing PCI. The addition of the TyG index to the GRACE score demonstrated an improved ability to predict 2-year adverse cardiovascular events compared with the GRACE score alone (AUCs: GRACE score 0.798 vs. GRACE score+TyG index 0.849, P = 0.043; NRI = 0.718, P < 0.001; IDI = 0.086, P < 0.001). The decision curve analysis suggested that the clinical net benefit of the new model (GRACE score+TyG index) was superior to that of the GRACE score alone, with a probability range of 0.04 to 0.32. When including the TyG index, HbA1C, FBG, TG, and LDL-C in the GRACE score system, we found that the TyG index had a greater incremental impact on risk prediction and stratification compared to the other parameters.
Conclusion: Combining the TyG index and GRACE score could improve the prediction of 2-year adverse cardiovascular events. This new risk model could identify patients with NSTE-ACS at higher risk of adverse events following PCI so that they can be monitored more carefully.
Introduction
Insulin resistance (IR) can induce disorders of glucose and lipid metabolism, which are important risk factors for the incidence and prognosis of cardiovascular diseases (1, 2). The hyperinsulinemia-glucose clamp test and homeostatic model assessment for insulin resistance (HOMA-IR) are recognized as accurate and reliable methods for evaluating IR; however, they are costly and complicated to perform. Epidemiological studies and clinical practice require easy-to-use markers of IR. The triglyceride-glucose index (TyG index) (composed of fasting glucose and triglycerides) not only has high sensitivity and specificity for IR identification but also correlates closely with the hyperinsulinemia-normal glucose clamp test and HOMA-IR and has been suggested to be a reliable alternative marker of IR (3). In addition, the TyG index has been proven to be closely associated with predicting the occurrence, progression, and prognosis of coronary heart disease (CHD) (4–6).
Even with percutaneous coronary intervention (PCI) and adequate antiplatelet drugs, the prognosis of some patients with non-ST-segment elevation acute coronary syndrome (NSTE-ACS) remains poor (7). Early risk stratification is important for clinical decision-making and prognostic assessment. The Global Registry of Acute Coronary Events (GRACE) risk score is currently the most widely used method for prognostic determination of patients with NSTE-ACS (8). Studies have shown that the GRACE risk score exhibits high predictive accuracy in both the inpatient phase and during long-term follow-up of major adverse cardiovascular events (MACEs) in patients with NSTE-ACS and guides clinicians in adjusting treatment regimens to reduce long-term cardiovascular risk (9). However, the TyG index, a new and powerful predictor of cardiovascular disease, has not been considered in the GRACE risk scoring system, which may result in a proportion of patients at high risk of adverse cardiovascular events being overlooked. Studies on the application of the TyG index in the GRACE score are limited; thus, the aim of this study was to investigate whether the predictive ability of the GRACE risk score improves when combined with the TyG index for 2-year adverse cardiovascular events in patients with NSTE-ACS and PCI.
Materials and methods
Study cohort
This was a single-center, retrospective study of patients with NSTE-ACS undergoing PCI at the First Affiliated Hospital of Zhengzhou University from April 2018 to December 2019, including those with unstable angina (UA) and non-ST-segment elevation myocardial infarction (NSTEMI).
The inclusion criteria were as follows: (1) diagnosis of UA or NSTEMI according to relevant guidelines (7); (2) PCI performed during hospitalization; and (3) integrated medical documentation. The exclusion criteria were as follows: (1) primary cardiomyopathy, valvular heart disease, and history of coronary artery bypass grafting; (2) severe liver or kidney dysfunction; (3) autoimmune diseases and hematologic disorders; (4) malignant diseases; and (5) use of triglyceride-lowering medications. Finally, a cohort of 515 patients with NSTE-ACS was included in the analysis (Supplementary Figure 1). This study was conducted in compliance with the Helsinki Declaration of Human Rights and was approved by the Clinical Research Ethics Committee of the First Affiliated Hospital of Zhengzhou University.
Demographic and clinical data
Clinical data at admission, including demographic data, medical history, laboratory test results, and angiographic and echocardiographic data, were collected from the First Affiliated Hospital of Zhengzhou University Medical Information Recording System. Laboratory parameters were analyzed by standard techniques using fasting venous blood samples collected after overnight fasting (>8 h) before the baseline coronary procedure. Calculation of the GRACE score was based on the clinical data obtained at admission (age, heart rate, systolic blood pressure, Killip class, creatinine level, ST-segment deviation, elevated cardiac enzymes, and cardiac arrest) (Supplementary Table 1).
Definitions
NSTE-ACS was defined according to the current guidelines of the European Society of Cardiology (10). A score of ≥140 was defined as high risk. Obesity was defined as a body mass index of >25 kg/m2. An estimated glomerular filtration rate <60 ml/min/1.73 m2 was considered to indicate the presence of chronic kidney disease. The TyG index was calculated as ln[fasting triglyceride (TG) (mg/dl) × fasting blood glucose (FBG) (mg/dl)/2].
Outcomes and follow-up
The primary endpoint was defined as a composite of adverse cardiovascular events including all-cause death, non-fatal myocardial infarction, non-fatal ischemic stroke, and ischemia-driven revascularization. All-cause mortality was defined as death due to any reason. Reviews of electronic medical records and follow-up telephonic interviews were conducted to assess 2-year clinical outcomes.
Statistical analyses
Continuous variables are expressed as mean ± standard deviation or median (interquartile range) according to the presence or absence of normal distribution. Comparisons between two groups were performed using Student's t-test or the Mann-Whitney U test. Categorical variables were expressed as numbers and percentages, and comparisons between groups were made using Pearson's chi-square test or Fisher's exact test. Kaplan–Meier analysis was performed to describe the cumulative incidence of the primary endpoint based on the median TyG index, and the groups were compared using the log-rank test. The correlation between the GRACE risk score and the TyG index was evaluated using Spearman's correlation analysis. Univariate and multivariate Cox regression analyses were used to identify whether the TyG index and GRACE risk score were independent predictors of the primary endpoint. C-statistics were calculated using receiver operating characteristic (ROC) analysis curves, which reflect the discrimination of the model. The areas under the curves (AUCs) of the two models were compared using the Delong test. The net reclassification improvement (NRI) and integrated differentiation improvement (IDI) risk models were used to compare the GRACE score model with the new risk model to identify which can correctly reclassify 2-year adverse cardiovascular disease. The clinical values of the new risk model and GRACE score alone were assessed using decision curve analysis (DCA). Data were analyzed using R (version 4.1.2; R Foundation for Statistical Computing, Vienna, Austria) and MedCalc (version 19.1; MedCalc Software Ltd., Ostend, Belgium). A two-sided P-value of <0.05 was considered to indicate statistical significance.
Results
Baseline characteristics of patients
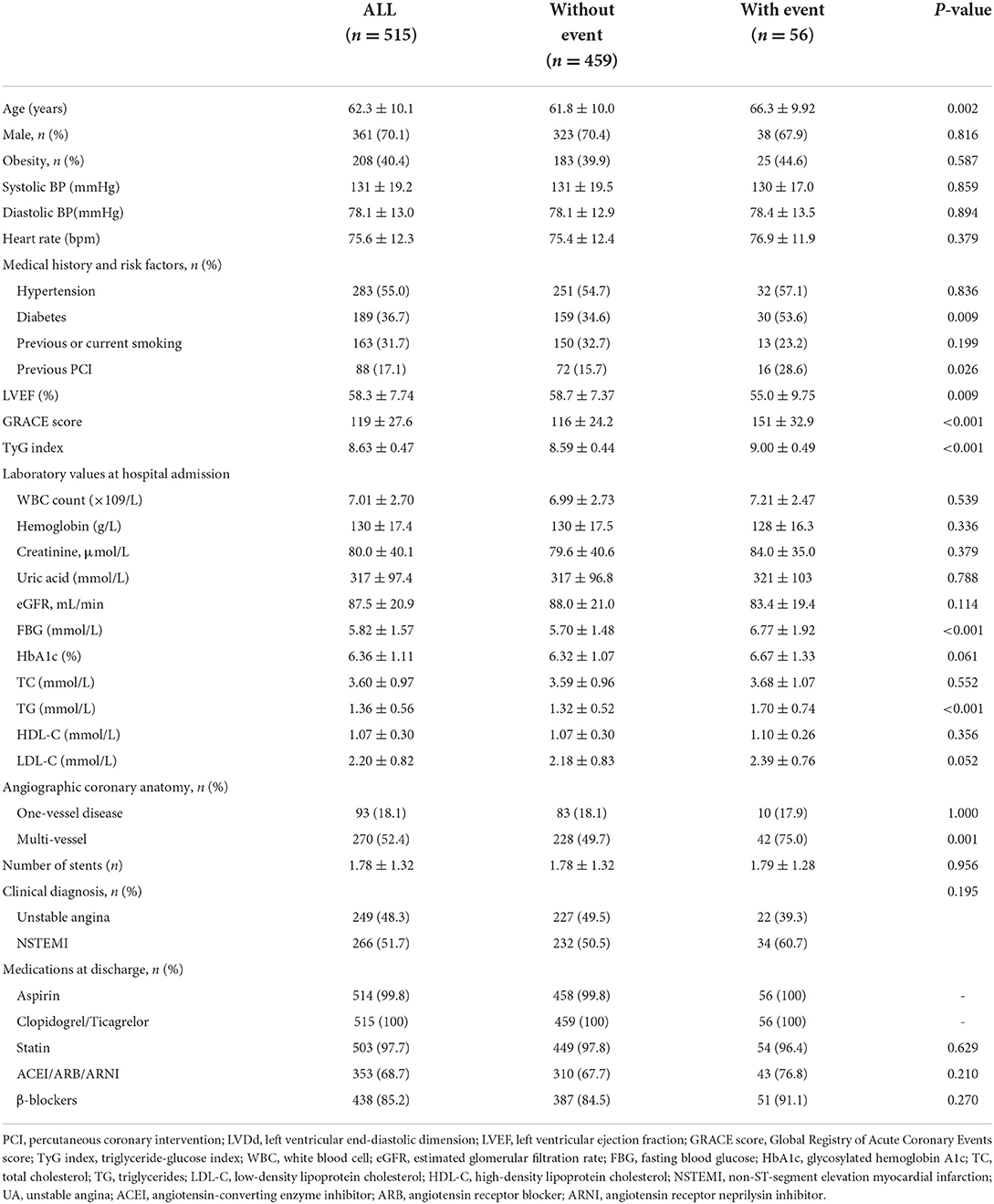
This study included 515 patients with NSTE-ACS undergoing PCI, with a mean age of 62.3 ± 10.1 years and a male proportion of 70.1%. During the 24-month follow-up period, 56 patients (10.9% of the total population) experienced primary endpoint events, which consisted of 17 (3.3%) all-cause deaths, 15 (2.9%) non-fatal myocardial infarctions, 7 (1.4%) non-fatal ischemic strokes, and 17 (3.3%) ischemia-driven revascularizations. The baseline characteristics of the study population are shown in Table 1.
Patients were divided into two groups according to the occurrence of primary endpoint events. Patients with a primary endpoint event had a higher rate of smoking and prior histories of PCI and multivessel disease and a higher GRACE score, TyG index, age, FBG, glycated hemoglobin (HbA1c), TG, low-density lipoprotein cholesterol (LDL-C), and lower left ventricular ejection fraction (LVEF) than those without a primary endpoint event. We performed a correlation analysis and found a weak correlation between the TyG index and the GRACE score (r = 0.120, P = 0.006) (Supplementary Table 2).
TyG index as an independent predictor of major endpoint events
Kaplan-Meier curves stratified by the median TyG index are shown in Figure 1. Major endpoint events occurred more frequently in patients with a high TyG index (log-rank test, P < 0.001) (Figure 1). Univariate Cox analysis showed that the significant predictors of major endpoint events were smoking, multivessel disease, diabetes, history of PCI, lower LVEF, older age, higher HbA1C levels, higher LDL-C levels, higher FBG levels, higher TG levels, higher GRACE score, and higher TyG index (Supplementary Table 3). The results of the collinearity analysis of the TyG index and other predictors are displayed in Supplementary Table 4. TG, LDL-C, and HbA1C levels had high co-linearity with the TyG index. Therefore, the TG, LDL-C, and HbA1c levels were not included in the multivariate Cox analysis (Table 2). Multivariate Cox regression analysis revealed that the TyG index [hazard ratio (HR) 5.31; 95% confidence interval (CI) 2.75–10.24; P < 0.001] and GRACE score (HR 1.03; 95% CI 1.03–1.04; P < 0.001) were both independent predictors of major endpoints (Figure 2).
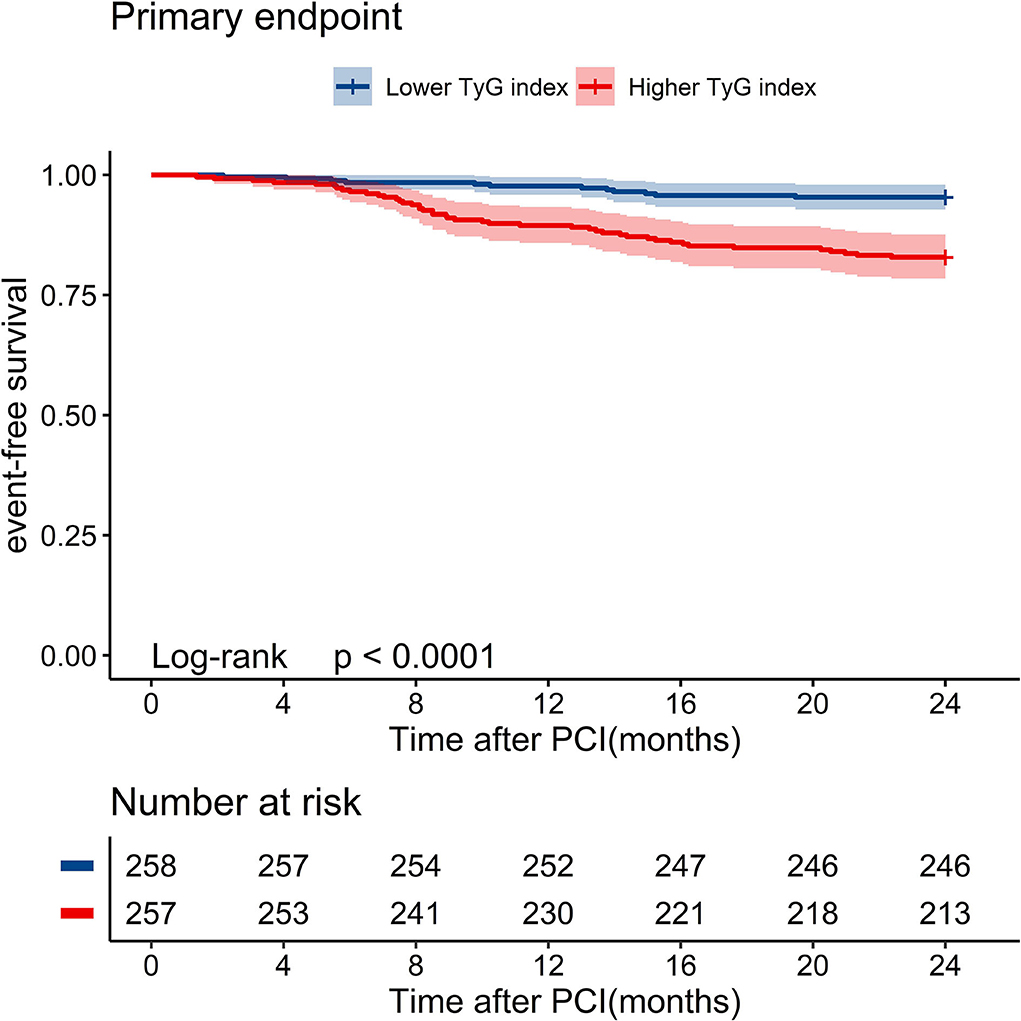
Figure 1. Kaplan–Meier survival curves of event-free survival stratified by the median level of TyG index for 2-year primary endpoint events. PCI, percutaneous coronary intervention; TyG index, triglyceride-glucose index.
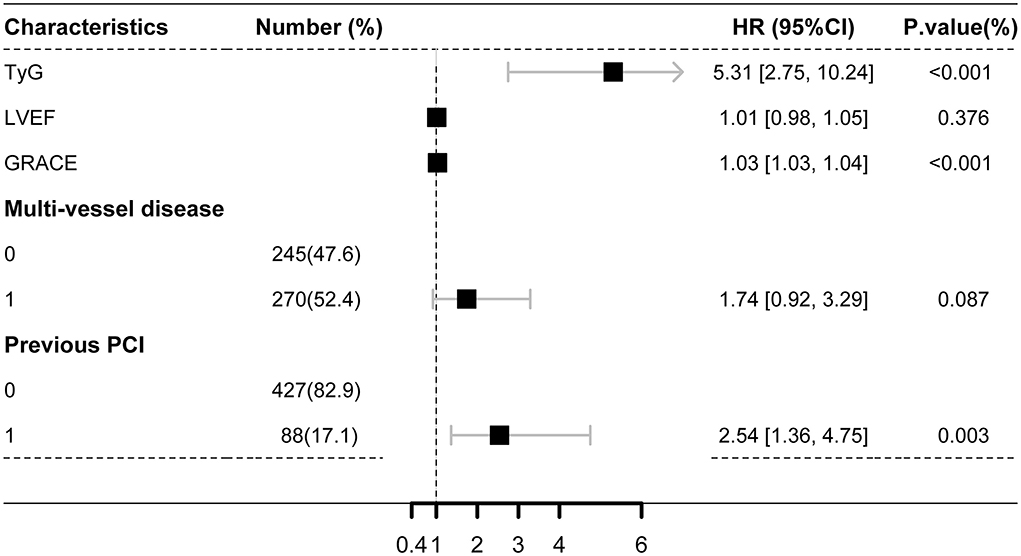
Figure 2. Multivariate cox analysis for the predictors of the primary endpoint. GRACE score, Global Registry of Acute Coronary Events score; TyG index, triglyceride-glucose index; LVEF, left ventricular ejection fraction; HR, hazard ratio; CI, confidence interval.
Predictive value of combining TyG index and GRACE score for primary endpoint events
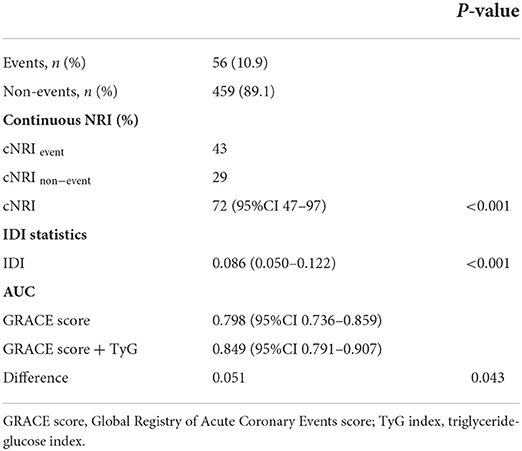
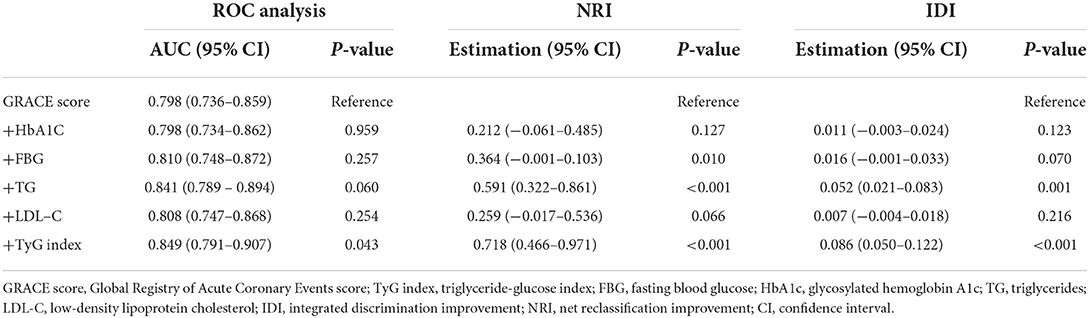
In contrast with other parameters, adding the TyG index to the GRACE score resulted in the most significant improvement in the AUC for predicting primary endpoint events (AUCs: GRACE score 0.798 vs. +TyG index 0.849, P = 0.043; GRACE score 0.798 vs. +HbA1C 0.798, P = 0.959; GRACE score 0.798 vs. +FBG 0.810, P = 0.257; GRACE score 0.798 vs. +TG 0.841, P = 0.060; GRACE score 0.798 vs. +LDL-C 0.808, P = 0.254). Furthermore, adding the TyG index to the GRACE score resulted in a greater improvement in risk reclassification and discrimination (NRI = 0.718, P < 0.001; IDI = 0.086, P < 0.001) compared with HbA1C (NRI = 0.212, P = 0.127; IDI = 0.011, P = 0.123), FBG (NRI = 0.364, P = 0.010; IDI = 0.016, P = 0.070), TG (NRI = 0.591, P < 0.001; IDI = 0.052, P = 0.001), and LDL-C (NRI = 0.259, P = 0.066; IDI = 0.007, P = 0.216) (Tables 2, 3). DCA suggested that both the GRACE score and the new model (GRACE score+TyG index) had good clinical application value for predicting the 2-year primary endpoint. The net benefit of the new model was superior to the GRACE score alone, with a probability range of 0.04 to 0.32 (Figure 3).
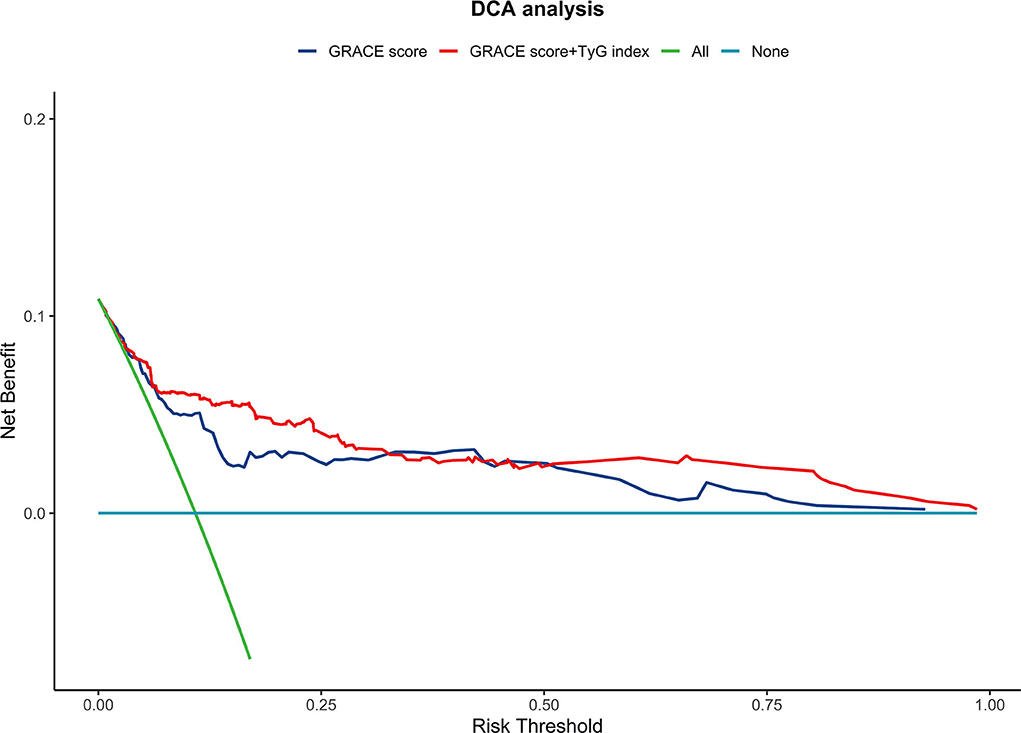
Figure 3. The decision curve analysis (DCA) comparing the GRACE risk score and its combination with the TyG index. GRACE score, Global Registry of Acute Coronary Events score; TyG index, triglyceride-glucose index.
Discussion
In this study, we examined the prognostic and predictive effects of the GRACE score combined with the TyG index on 2-year adverse cardiovascular events in patients with NSTE-ACS who underwent elective PCI. The major findings of this study are as follows: (1) The GRACE score and TyG index could independently predict adverse cardiovascular events in patients with NSTE-ACS undergoing PCI; (2) the TyG index was weakly correlated with the GRACE score; and (3) in contrast to other glucose- and lipid-related parameters, adding the TyG index to the GRACE score showed the best performance in predicting adverse cardiovascular events.
Patients with IR are susceptible to a variety of metabolic disorders, such as hyperglycemia, dyslipidemia, and hypertension, which are closely related to a poor prognosis of CVD (cardiovascular disease) (11). The hyperinsulinemia-glucose clamp test and HOMA-IR are well-established methods for assessing IR but are difficult to implement in clinical practice because of their high cost, time requirement, and complexity (12). The TyG index is a newly discovered alternative marker for IR, which is simple, inexpensive, and convenient for clinicians. In addition, the TyG index shows a direct correlation with the hyperinsulinemia-glucose clamp test and HOMA-IR (3). At present, the TyG index is widely used in the assessment of CVD risk, and a clear correlation has been confirmed in various CVDs such as acute coronary syndrome, arteriosclerosis, heart failure, and coronary artery calcification (13–15).
However, the mechanisms responsible for the association between the TyG index and CVD remain uncertain. The potential relationship between the TyG index and CVD is as follows. First, IR can induce blood glucose and lipid metabolism disorders, leading to inflammation and oxidative stress, and these changes further aggravate the progression of CVD (16). Second, IR can induce increased production of glycosylated products and free radicals, resulting in NO inactivation and impaired vascular diastolic function (17). Moreover, IR can mediate the relevant signaling that sensitizes platelets to the anti-aggregation effects of prostaglandin I2 (PGI2) and NO, which, in turn, can lead to thrombosis (18). In addition, IR can induce excessive glycosylation, which promotes smooth muscle cell proliferation and collagen deposition, leading to increased ventricular stiffness, cardiac fibrosis, and ultimately, heart failure (11, 19). Finally, IR also plays an important role in hyperlipidemia. Increased TG levels can increase free fatty acid (FFA) levels and promote FFA flux from adipose tissue to non-adipose tissue (20). Furthermore, the retention of cholesterol- and TG-rich remnants of Apo B in coronary artery walls may play a role in the pathogenesis of atherosclerosis (21).
Owing to its ease of use, the convenience of data acquisition, and high accuracy, most of the current guidelines recommend the GRACE score to evaluate the prognosis of patients with NSTE-ACS. However, the biochemical indicators of the GRACE score include only myocardial necrosis markers and creatinine, leaving room for improvement in predicting adverse cardiovascular events. According to current research, pro-brain natriuretic peptides, C-reactive protein, and other biomarkers can contribute to the predictive power of the GRACE score (22, 23). The TyG index can reflect disorders of glucose and lipid metabolism and predict the prognosis of patients with ACS (4, 6, 24); however, the effect of the TyG index on the predictive ability of the GRACE scoring system for the occurrence of adverse cardiovascular events in patients with NSTE-ACS undergoing PCI remains unknown. Among our patients, we found that the GRACE score increased with an increasing TyG index, and a correlation was found between the two variables. Similar to previous studies, we found that an elevated TyG index and GRACE score were significantly associated with 2-year adverse cardiovascular events in patients with NSTE-ACS who underwent PCI. We found that the predictive ability can be significantly improved by including the TyG index in the GRACE score since the AUC went from 0.798 to 0.845 when the TyG index was combined with the GRACE score. Moreover, multiple novel methods were used to evaluate the improvement in discrimination and clinical usage of the TyG index when added to the GRACE score, including the IDI, NRI, and DCA curves. Using a continuous, category-free NRI, 29% of patients without events were reclassified as low risk and 43% of patients with events were reclassified as high risk. Furthermore, IDI analysis showed that incorporation of the TyG index with the GRACE scores significantly improved the discriminatory accuracy for adverse cardiovascular events with an IDI of 8.6% (p < 0.001). Finally, by plotting DCA curves, we found that the predictive value of the new model with the combined TyG index was higher than that of the traditional GRACE model, with a probability range of 0.04 to 0.32 for endpoint events. Therefore, with the assistance of this new model (GRACE score combined with TyG index), major endpoint events can be predicted more accurately and better clinical decisions can be made for patients with NSTE-ACS.
We then further compared the gain effect of the Tyg index and the levels of HbA1C, FBG, TG, and LDL-C on the GRACE score for predicting adverse cardiovascular events, considering that the TyG index is closely associated with lipid and glucose metabolism. We found that the TyG index was strongly correlated with TG levels and moderately correlated with FBG, TG, LDL-C, and HbA1C levels. Given the relatively small number of patients with diabetes in our study cohort and the small range of glycemic fluctuations, the TyG index and TG levels correlated more strongly. ROC curve analyses, NRI, and IDI were used to quantify the improvement in the different prediction models. Although previous studies have shown that HbA1C is an independent risk factor for cardiovascular events (25, 26), HbA1C did not significantly improve the predictive power of the GRACE score in this study. Since HbA1C reflects blood glucose levels over the past 3 months, and most hospitalized patients in this study did not have diabetes, there was less difference in HbA1C values. Patients with the acute coronary syndrome often have stress hyperglycemia. Acute elevated blood glucose levels can induce oxidative stress, leading to direct injury of myocardial cells, endothelial dysfunction, and activation of clotting pathways, which can lead to enlarged infarct size, restenosis, and adverse cardiac remodeling (27–30). Numerous studies have shown a strong association between hyperglycemia and poor outcomes in patients with ACS (31–33). In this study, fasting glucose improved the ability of the GRACE score to distinguish patients at high risk of major adverse cardiovascular events (MACE) (NRI: P = 0.010). In previous studies, low-density lipoprotein was a very important indicator of the prognosis of patients with AMI (34), but this study showed a limited additional effect on the GRACE score. This may be because patients had been treated with statins before hospitalization for CHD-related symptoms with or without PCI. Surprisingly, in this study, triglycerides played a significant role in enhancing the ability of the GRACE score to predict MACE. Studies have shown that in addition to LDL, hypertriglyceridemia plays an important role in the development of coronary artery disease (35–38). In a large cohort study by Ambrosy et al. elevated triglyceride levels were associated with an increased risk of atherosclerotic cardiovascular disease events and a reduced risk of death in a cohort treated with statins (39). Hypertriglyceridemia is closely related to patients' eating habits (40), so a healthy diet after discharge is essential. The TyG index reflects the status of insulin resistance and has a good predictive effect on the occurrence of MACE. Including these parameters into the GRACE score system, we found that the TyG index had a greater incremental impact on risk prediction and stratification than the other parameters. Thus, the TyG index may provide more information on recurrent adverse cardiovascular events.
Patients with multivessel coronary artery disease have a high risk of MACE (41). We found that patients with NSTE-ACS and a high TyG index were more likely to have the multivessel disease. Similar to our research, a recent study found that a high TyG was significantly associated with the risk of multivessel coronary artery disease regardless of confounders, such as age, sex, SBP, DBP, history of smoking and alcohol consumption, and drug therapy (42). This may be another reason the TyG index can predict primary endpoints independent of the GRACE score in some patients. Unfortunately, there are few studies on the relationship between TyG and multivessel coronary artery disease at present, and further large-sample studies are needed.
Limitations
Our study has three limitations. First, it was a single-center retrospective study; therefore, the findings should be interpreted with caution. Second, because patient information was insufficient, we did not specify the cardiovascular deaths that were commonly used as endpoint events. Finally, as the study involved only Chinese patients, generalizing the findings to other ethnic groups might not be appropriate.
Conclusion
Combining the TyG index and GRACE score could improve the prediction of the occurrence of 2-year adverse cardiovascular events. This new risk model could identify patients with NSTE-ACS at higher risk of adverse events following PCI so that they can be monitored more carefully.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author/s.
Ethics statement
The studies involving human participants were reviewed and approved by the First Affiliated Hospital of Zhengzhou University. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Author contributions
SP, GM, and XZ contributed to the conception and design of the study. SP, GM, YZ, and ZR collected the clinical information. SP wrote the first draft of the manuscript. SP, GM, and YD wrote sections of the manuscript. All authors have revised, read, and approved the final version of the manuscript.
Funding
This study was supported by the Science and Technology Development of Henan Province (Grant No. 212102310210).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcvm.2022.957626/full#supplementary-material
Abbreviations
AUC, area under the curve; CI, confidence interval; DCA, decision curve analysis; FBG, fasting blood glucose; GRACE, Global Registry of Acute Coronary Events; HbA1c, glycated hemoglobin; HOMA-IR, homeostatic model assessment for insulin resistance; HR, hazard ratio; IDI, integrated differentiation improvement; IR, insulin resistance; LDL-C, low-density lipoprotein cholesterol; LVEF, left ventricular ejection fraction; NRI, net reclassification improvement; NSTE-ACS, non-ST-segment elevation acute coronary syndrome; NSTEMI, non-ST-segment elevation myocardial infarction; PCI, percutaneous coronary intervention; ROC, receiver operating characteristic; TG, triglycerides; TyG index, triglyceride-glucose index; UA, unstable angina.
References
1. Eddy D, Schlessinger L, Kahn R, Peskin B, Schiebinger R. Relationship of insulin resistance and related metabolic variables to coronary artery disease: a mathematical analysis. Diabetes Care. (2009) 32:361–6. doi: 10.2337/dc08-0854
2. Ormazabal V, Nair S, Elfeky O, Aguayo C, Salomon C, Zuniga FA. Association between insulin resistance and the development of cardiovascular disease. Cardiovasc Diabetol. (2018) 17:122. doi: 10.1186/s12933-018-0762-4
3. Guerrero-Romero F, Simental-Mendia LE, Gonzalez-Ortiz M, Martinez-Abundis E, Ramos-Zavala MG, Hernandez-Gonzalez SO, et al. The product of triglycerides and glucose, a simple measure of insulin sensitivity. Comparison with the euglycemic-hyperinsulinemic. Clamp J Clin Endocrinol Metab. (2010) 95:3347–51. doi: 10.1210/jc.2010-0288
4. Hong S, Han K, Park CY. The triglyceride glucose index is a simple and low-cost marker associated with atherosclerotic cardiovascular disease: a population-based study. BMC Med. (2020) 18:361. doi: 10.1186/s12916-020-01824-2
5. Li M, Zhan A, Huang X, Hu L, Zhou W, Wang T, et al. Positive association between triglyceride glucose index and arterial stiffness in hypertensive patients: the china h-type hypertension registry study. Cardiovasc Diabetol. (2020) 19:139. doi: 10.1186/s12933-020-01124-2
6. Wang L, Cong HL, Zhang JX, Hu YC, Wei A, Zhang YY, et al. Triglyceride-glucose index predicts adverse cardiovascular events in patients with diabetes and acute coronary syndrome. Cardiovasc Diabetol. (2020) 19:80. doi: 10.1186/s12933-020-01054-z
7. Amsterdam EA, Wenger NK, Brindis RG, Casey DE, Ganiats TG, Holmes DR, et al. Aha/Acc guideline for the management of patients with non-st-elevation acute coronary syndromes: a report of the American college of cardiology/American heart association task force on practice guidelines. J Am Coll Cardiol. (2014) 64:e139–e228. doi: 10.1016/j.jacc.2014.09.017
8. Hamm CW, Bassand JP, Agewall S, Bax J, Boersma E, Bueno H, et al. Esc guidelines for the management of acute coronary syndromes in patients presenting without persistent st-segment elevation: the task force for the management of acute coronary syndromes (Acs) in patients presenting without persistent st-segment elevation of the european society of cardiology (Esc). Eur Heart J. (2011) 32:2999–3054. doi: 10.1093/eurheartj/ehr236
9. Fox KA, Carruthers KF, Dunbar DR, Graham C, Manning JR, De Raedt H, et al. Underestimated and under-recognized: the late consequences of acute coronary syndrome (Grace Uk-Belgian Study). Eur Heart J. (2010) 31:2755–64. doi: 10.1093/eurheartj/ehq326
10. Collet J, Thiele H, Barbato E, Barthélémy O, Bauersachs J, Bhatt D, et al. 2020 Esc guidelines for the management of acute coronary syndromes in patients presenting without persistent st-segment elevation. Eur Heart J. (2021) 42:1289–367. doi: 10.1093/eurheartj/ehaa909
11. Tao LC, Xu JN, Wang TT, Hua F, Li JJ. Triglyceride-glucose index as a marker in cardiovascular diseases: landscape and limitations. Cardiovasc Diabetol. (2022) 21:68. doi: 10.1186/s12933-022-01511-x
12. Irace C, Carallo C, Scavelli FB, De Franceschi MS, Esposito T, Tripolino C, et al. Markers of insulin resistance and carotid atherosclerosis. A comparison of the homeostasis model assessment and triglyceride glucose index. Int J Clin Pract. (2013) 67:665–72. doi: 10.1111/ijcp.12124
13. Luo E, Wang D, Yan G, Qiao Y, Liu B, Hou J, et al. High triglyceride-glucose index is associated with poor prognosis in patients with acute st-elevation myocardial infarction after percutaneous coronary intervention. Cardiovasc Diabetol. (2019) 18:150. doi: 10.1186/s12933-019-0957-3
14. Guo W, Zhao L, Mo F, Peng C, Li L, Xu Y, et al. The prognostic value of the triglyceride glucose index in patients with chronic heart failure and type 2 diabetes: a retrospective cohort study. Diabetes Res Clin Pract. (2021) 177:108786. doi: 10.1016/j.diabres.2021.108786
15. Won KB, Park EJ, Han D, Lee JH, Choi SY, Chun EJ, et al. Triglyceride glucose index is an independent predictor for the progression of coronary artery calcification in the absence of heavy coronary artery calcification at baseline. Cardiovasc Diabetol. (2020) 19:34. doi: 10.1186/s12933-020-01008-5
16. Yang Q, Vijayakumar A, Kahn BB. Metabolites as regulators of insulin sensitivity and metabolism. Nat Rev Mol Cell Biol. (2018) 19:654–72. doi: 10.1038/s41580-018-0044-8
17. Molina MN, Ferder L, Manucha W. Emerging role of nitric oxide and heat shock proteins in insulin resistance. Curr Hypertens Rep. (2016) 18:1. doi: 10.1007/s11906-015-0615-4
18. Gerrits AJ, Koekman CA, van Haeften TW, Akkerman JW. Platelet tissue factor synthesis in type 2 diabetic patients is resistant to inhibition by insulin. Diabetes. (2010) 59:1487–95. doi: 10.2337/db09-1008
19. Hill MA, Yang Y, Zhang L, Sun Z, Jia G, Parrish AR, et al. Insulin resistance, cardiovascular stiffening and cardiovascular disease. Metabolism. (2021) 119:154766. doi: 10.1016/j.metabol.2021.154766
20. Samuel VT, Shulman GI. The pathogenesis of insulin resistance: integrating signaling pathways and substrate flux. J Clin Invest. (2016) 126:12–22. doi: 10.1172/JCI77812
21. Ala-Korpela M. The culprit is the carrier, not the loads: cholesterol, triglycerides and apolipoprotein B in atherosclerosis and coronary heart disease. Int J Epidemiol. (2019) 48:1389–92. doi: 10.1093/ije/dyz068
22. Ang DS, Wei L, Kao MP, Lang CC, Struthers AD. A Comparison between B-type natriuretic peptide, global registry of acute coronary events (grace) score and their combination in acs risk stratification. Heart. (2009) 95:1836–42. doi: 10.1136/hrt.2008.160234
23. Persampieri S, Castini D, Valli F, Sabatelli L, Carugo S. Additional predictive value of C-reactive protein to grace score in patients with acute coronary syndrome. Eur J Int Med. (2019) 69:e1–2. doi: 10.1016/j.ejim.2019.07.036
24. Park GM, Cho YR, Won KB, Yang YJ, Park S, Ann SH, et al. Triglyceride glucose index is a useful marker for predicting subclinical coronary artery disease in the absence of traditional risk factors. Lipids Health Dis. (2020) 19:7. doi: 10.1186/s12944-020-1187-0
25. Stratton IM, Adler AI, Neil HA, Matthews DR, Manley SE, Cull CA, et al. Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes (Ukpds 35): prospective observational study. BMJ Clin Res Ed. (2000) 321:405–12. doi: 10.1136/bmj.321.7258.405
26. Corpus RA, O'Neill WW, Dixon SR, Timmis GC, Devlin WH. Relation of hemoglobin a1c to rate of major adverse cardiac events in nondiabetic patients undergoing percutaneous coronary revascularization. Am J Cardiol. (2003) 92:1282–6. doi: 10.1016/j.amjcard.2003.08.008
27. Li M, Chen G, Feng Y, He X. Stress induced hyperglycemia in the context of acute coronary syndrome: definitions, interventions, and underlying mechanisms. Front Cardiovasc Med. (2021) 8:676892. doi: 10.3389/fcvm.2021.676892
28. Kloner RA, Przyklenk K, Whittaker P. Deleterious effects of oxygen radicals in ischemia/reperfusion. Resolved Unresolved Issues Circ. (1989) 80:1115–27. doi: 10.1161/01.CIR.80.5.1115
29. Jensen CJ, Eberle HC, Nassenstein K, Schlosser T, Farazandeh M, Naber CK, et al. Impact of hyperglycemia at admission in patients with acute st-segment elevation myocardial infarction as assessed by contrast-enhanced mri. Clin Res Cardiol. (2011) 100:649–59. doi: 10.1007/s00392-011-0290-7
30. Nian M, Lee P, Khaper N, Liu P. Inflammatory cytokines and postmyocardial infarction remodeling. Circ Res. (2004) 94:1543–53. doi: 10.1161/01.RES.0000130526.20854.fa
31. Cui CY, Zhou MG, Cheng LC, Ye T, Zhang YM, Zhu F, et al. Admission hyperglycemia as an independent predictor of long-term prognosis in acute myocardial infarction patients without diabetes: a retrospective study. J Diabetes Investig. (2021) 12:1244–51. doi: 10.1111/jdi.13468
32. Hao Y, Lu Q, Li T, Yang G, Hu P, Ma A. Admission hyperglycemia and adverse outcomes in diabetic and non-diabetic patients with non-st-elevation myocardial infarction undergoing percutaneous coronary intervention. BMC Cardiovasc Disord. (2017) 17:6. doi: 10.1186/s12872-016-0441-x
33. Kim EJ, Jeong MH, Kim JH, Ahn TH, Seung KB, Oh DJ, et al. Clinical impact of admission hyperglycemia on in-hospital mortality in acute myocardial infarction patients. Int J Cardiol. (2017) 236:9–15. doi: 10.1016/j.ijcard.2017.01.095
34. Cicero AFG, Fogacci F, Hernandez AV, Banach M. Efficacy and safety of bempedoic acid for the treatment of hypercholesterolemia: a systematic review and meta-analysis. PLoS Med. (2020) 17:e1003121. doi: 10.1371/journal.pmed.1003121
35. Nordestgaard BG, Varbo A. Triglycerides and cardiovascular disease. Lancet. (2014) 384:626–35. doi: 10.1016/S0140-6736(14)61177-6
36. Peng J, Luo F, Ruan G, Peng R, Li X. Hypertriglyceridemia and atherosclerosis. Lipids Health Dis. (2017) 16:233. doi: 10.1186/s12944-017-0625-0
37. Matsumoto S, Gotoh N, Hishinuma S, Abe Y, Shimizu Y, Katano Y, et al. The role of hypertriglyceridemia in the development of atherosclerosis and endothelial dysfunction. Nutrients. (2014) 6:1236–50. doi: 10.3390/nu6031236
38. Ginsberg HN, Packard CJ, Chapman MJ, Borén J, Aguilar-Salinas CA, Averna M, et al. Triglyceride-rich lipoproteins and their remnants: metabolic insights, role in atherosclerotic cardiovascular disease, and emerging therapeutic strategies-a consensus statement from the European atherosclerosis society. Eur Heart J. (2021) 42:4791–806. doi: 10.1093/eurheartj/ehab551
39. Ambrosy AP, Yang J, Sung SH, Allen AR, Fitzpatrick JK, Rana JS, et al. Triglyceride levels and residual risk of atherosclerotic cardiovascular disease events and death in adults receiving statin therapy for primary or secondary prevention: insights from the Kp reach study. J Am Heart Assoc. (2021) 10:e020377. doi: 10.1161/JAHA.120.020377
40. Yamanaka M, Sakuma M, Matsushita A, Tanaka S, Yamamoto Y, Asai T, et al. The effects of long-term dietary therapy on patients with hypertriglyceridemia. J Atheroscler Thromb. (2019) 26:39–49. doi: 10.5551/jat.42440
41. Özcan C, Deleskog A, Schjerning Olsen AM, Nordahl Christensen H, Lock Hansen M, Hilmar Gislason G. Coronary artery disease severity and long-term cardiovascular risk in patients with myocardial infarction: a danish nationwide register-based cohort study. Europ Heart J Cardiovas Pharmacother. (2018) 4:25–35. doi: 10.1093/ehjcvp/pvx009
42. Su J, Li Z, Huang M, Wang Y, Yang T, Ma M, et al. Triglyceride glucose index for the detection of the severity of coronary artery disease in different glucose metabolic states in patients with coronary heart disease: a Rcscd-Tcm study in China. Cardiovasc Diabetol. (2022) 21:96. doi: 10.1186/s12933-022-01523-7
Keywords: acute coronary syndrome, percutaneous coronary intervention, insulin resistance, biomarkers, prognosis
Citation: Pang S, Miao G, Zhou Y, Du Y, Rui Z and Zhao X (2022) Addition of TyG index to the GRACE score improves prediction of adverse cardiovascular outcomes in patients with non-ST-segment elevation acute coronary syndrome undergoing percutaneous coronary intervention: A retrospective study. Front. Cardiovasc. Med. 9:957626. doi: 10.3389/fcvm.2022.957626
Received: 31 May 2022; Accepted: 01 August 2022;
Published: 25 August 2022.
Edited by:
Christoph Sinning, University Medical Center Hamburg-Eppendorf, GermanyReviewed by:
Hui Gao, Affiliated Beijing Friendship Hospital, Capital Medical University, ChinaQi Zhao, Beijing Anzhen Hospital, Capital Medical University, China
Copyright © 2022 Pang, Miao, Zhou, Du, Rui and Zhao. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xiaoyan Zhao, fcczhaoxy8@zzu.edu.cn
 Shuo Pang
Shuo Pang Guangrui Miao
Guangrui Miao  Xiaoyan Zhao
Xiaoyan Zhao