- 1Psycho-Oncology Unit, Istituto Scientifico Romagnolo per lo Studio e la Cura dei Tumori (IRST), IRCCS, Meldola, Italy
- 2Medical Oncology Department, Istituto Scientifico Romagnolo per lo Studio e la Cura dei Tumori (IRST), IRCCS, Meldola, Italy
- 3Medical Oncology Department, Campus Bio-Medico University, Rome, Italy
- 42nd Department of Oncology, Faculty of Medicine, Comenius University and National Cancer Institute, Bratislava, Slovakia
- 5Division of Medical Oncology, Cannizzaro Hospital, Catania, Italy
- 6University Hospital Psychiatry Unit, Integrated Department of Mental Health and Addictive Behavior, St. Anna University Hospital and NHS Community Health Trusts, Ferrara, Italy
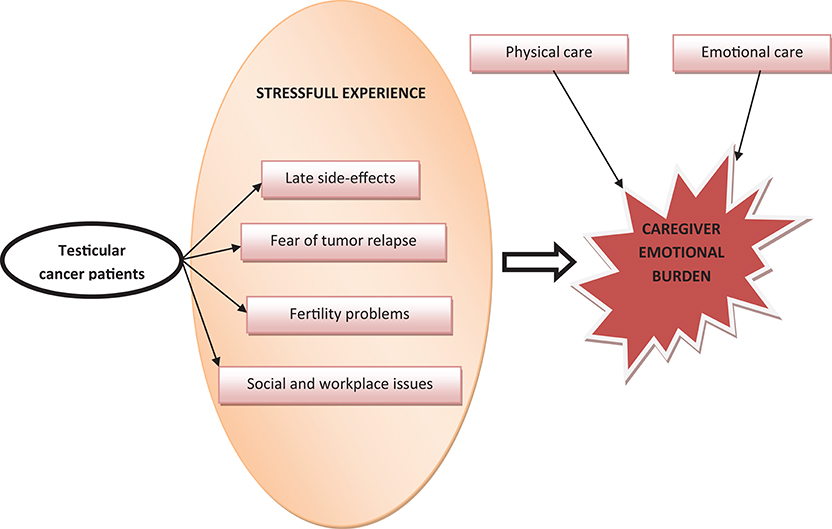
Testicular cancer is the most common tumor in young males aged 15–40 years. The overall cure rate for men with testicular cancer is >90%, so a huge number of these patients will become testicular cancer survivors. These people may feel some stress in the experience of diagnosis, treatment, and consequences that affects the quality of life, and during follow-up, especially when new issues and emotional distresses appear over time, such as late side-effects of treatments and emotional challenges including fear of tumor relapse, fertility and sexuality concerns, and social and workplace issues. The cancer experience has an impact not only on patients, but also on their relatives (e.g., spouses, parents, or siblings), who often have to assume a caregiving role for the duration of and following treatment for cancer. Moreover, the caregiver plays an important role in supporting a man with a testicular cancer, providing physical and emotional care. This review presents a summary of existing knowledge regarding the impact and the burden of testicular cancer on caregivers.
Introduction
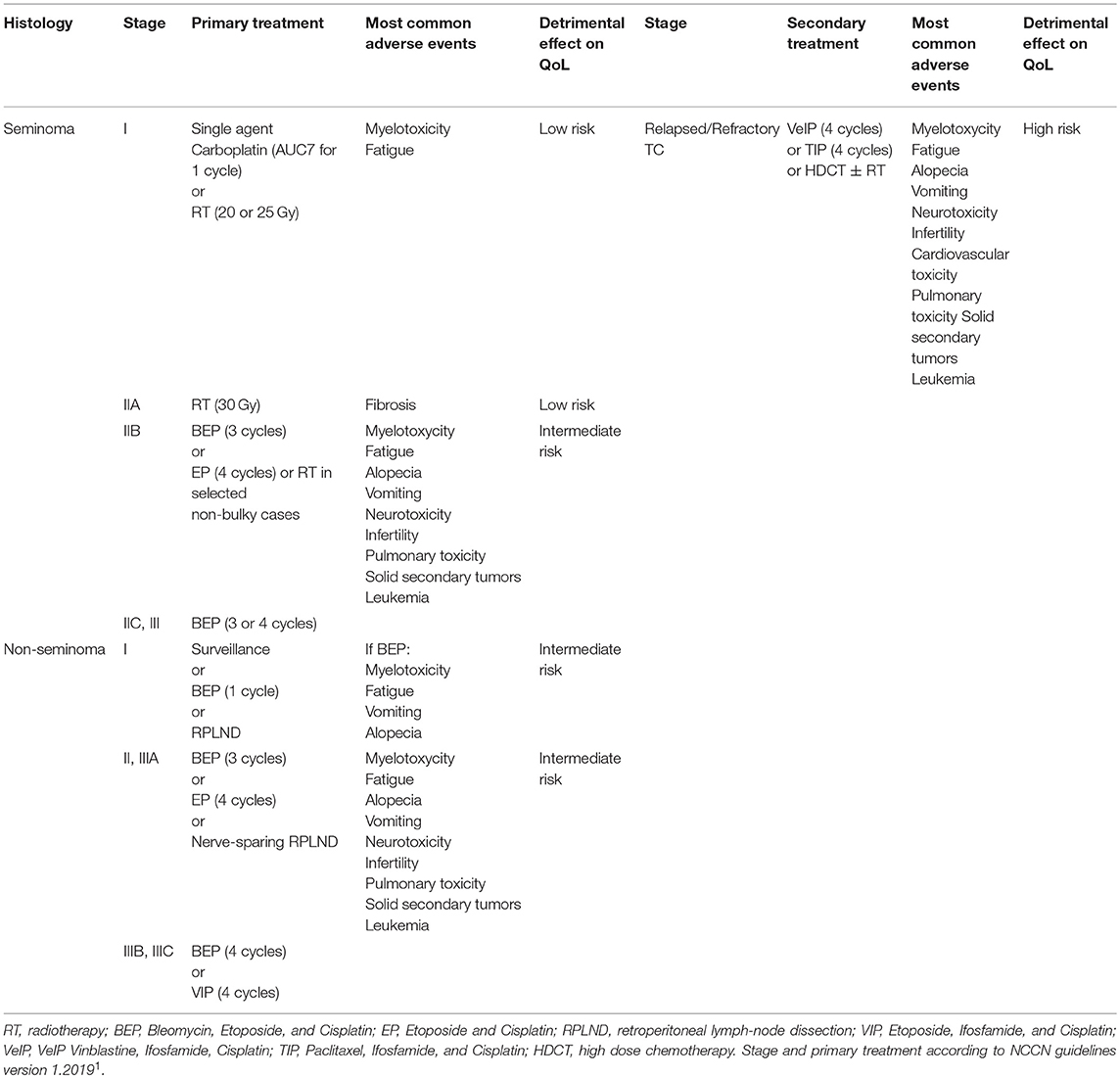
Testicular cancer (TC) is the most frequent solid tumor in young adult men aged between 15 and 35 years, and is a highly curable cancer with survival rates close to 99% for stage I disease cases (localized tumor) and 80–90% for cases with metastatic disease treated with cisplatin-based chemotherapy and surgery on residual masses, when indicated (1). In addition, the 10–20% of metastatic patients who are not cured with first-line cisplatin-based chemotherapy, increase their chances of long-term remission in nearly 50% of cases treated with second-line treatments, such as high-dose chemotherapy (HDCT) or standard-dose chemotherapeutic regimens, and in nearly 15–30% of cases treated in the following lines with other salvage regimens (2–5). A young age at diagnosis and excellent prognosis, physical, psychological and social well-being represent a significant indicator for follow-up and survivorship of these people. In fact, despite the excellent prognosis, cured patients may experience long-term somatic sequelae and psychosocial distress according to the tumor and treatment burden (6, 7). However, type and duration of each treatment depends on initial stage of the disease (Table 1). As a consequence, different physical and psychological loads correlate with different treatment loads. Both tumor diagnosis and tumor treatment are usually stressful events affecting not only patients but the whole family system (Graphical Abstract) (8).
Role of Caregiver
Caregivers are individuals, usually family members or relatives (e.g., partner, parents, but also close friends), who have a significant relationship with the patient suffering from a life-threatening illness and provide assistance (9, 10). Along the whole process of the disease and its treatments, they are engaged in the practical help and psychological support for coping with the situation, including the emotions of uncertainty and fear (11). This role requires many abilities that may be physically, emotionally and financially demanding. The burden of caregiving has been defined a “multidimensional biopsychosocial reaction resulting from an imbalance of care demands relative to caregivers' personal time, social roles, physical and emotional states, financial resources, and formal care resources given the other multiple roles they fulfill” (12).
Cancer could determine major effects both on caregivers and patients, with literature clearly indicating that cancer affects the emotional, social, physical, and spiritual well-being of patients and their family members (13).
Most studies in family caregivers of cancer patients reported diverse problems as a consequence of their role, ranging from diminished physical health and psychological distress to an adverse impact on their work (14). The most prevalent physical problems included sleep disturbance, fatigue, pain, loss of physical strength, loss of appetite, and weight loss.
Cancer is a family experience that exerts a change in family's system, balance and identity, redefines the rules, changes the lives of all its members, brings an immense amount of stress, and presents many challenging situations. Cancer and the approaches used to treat it can introduce a complex array of lifestyle changes and emotional responses, which can be difficult for family members to handle. The diagnosis of cancer, its treatment and symptoms both of the illness and of the chemotherapy have an influence on how patients and their caregivers experience distress. A review on psychological impact of cancer on patients' partners and other relatives affirmed that an important minority of carers become highly distressed, clinically depressed and anxious: in particular, prevalence of clinically significant distress among caregivers was reported to be 20–30% in studies using self-report questionnaires, whereas in studies that used diagnostic interviews rates are approximately 10% (15). However, data concerning caregivers' distress are sparse. This review analyzes TC-related distress and burden of caregivers.
Caregiver Burden
The experience of illness perceived by the caregiver depends on some specific aspects of the disease such as the type of cancer and the stage of life in which it is diagnosed.
TC has a profound effect on body image and on the personal image of oneself and, and often occurs in adolescence and young adulthood, times characterized by significant life changes and psychosocial challenges. These men are in the prime of their lives, when health is often taken for granted, while interpersonal relationships and the desire to start a family may be major interests (16–19).
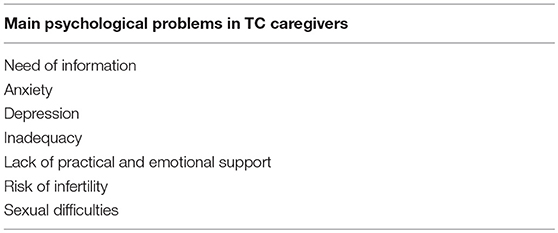
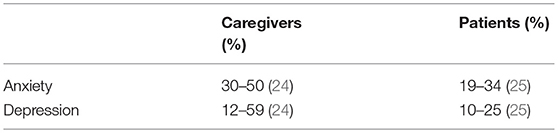
Diagnosis of TC causes a sort of emotional earthquake which involves relatives, partners and close friends. Cancer patients during treatment and also during the follow-up period experience many needs, and caregivers are often unprepared to respond to this important burden (20). Main psychological problems experienced by TC caregivers are summarized in Table 2. Of note is that the physical and mental health of patients and their caregivers are often related. In this contest, improving knowledge and social support to caregivers could help to ameliorate patients' global health. Confirming this, depression symptoms are less frequent in patients living in couples (21). Taking care of a patient with cancer is described as a full-time job (22) and caregivers themselves often are in great need of psychological support. Caregivers of TC patients usually are parents or partners, typically young females and it is recognized that the highest predisposition to symptoms of distress have been showed by female caregivers of young age and lower social status (19). Therefore, for female partners of cancer patients, there is a risk of developing psychological and psychiatric morbidity and lower quality-of-life (QoL) than women in healthy couples (15, 23). In this contest, TC survivors' caregivers are a high risk population. Several studies reported rates of anxiety of between 30 and 50% (24) among family caregivers in comparison to rates of anxiety of between 19 and 34% (25) in patient samples. Likewise, rates of depression are reported to be between 10 and 25% (25) in patients samples compared to between 12 and 59% (24) among family caregivers. This underlines that, in many cases, the psychological burden on caregivers is even greater than in patients (Table 3). Caregivers receive less practical and emotional support from friends and professionals than patients (26). However, their high self-efficacy can improve their own mental state and also the mental well-being of patients.
In their caregiver role, partners of TC patients have a social task: commonly they give information to family members and friends while her husband is in the hospital (27). Another considerable aspect of these women's burden is emotional experiences connected to the illness and to the period of life in which it occurs. Often the diagnosis of TC happens in an important period of life, characterized by major life changes and specific developmental tasks, when forming intimate and long-term emotional and sexual relationships, and starting families may be major concerns (28). Each member of the couple, both the patient and the partner, is faced with the possibility of treatment-related infertility and sexual difficulties in a period of life where partners are often focused on starting a family (27). However, only a minority of the couples experienced more serious and long lasting testicular cancer-induced disturbances in sexual and marital relationships. In general, couples felt their relationship became more tightly bonded and stronger following the confrontation with TC (29, 30).
Both psychosocial and QoL consequences occur years after the experience of the tumor and the end of treatments. Tuinman et al. (31) showed that spouses who experienced the diagnosis and treatment process had better physical QoL than the average woman. Their stress response levels were low and were related to the stress response level of TC survivors and to the duration of treatments received. However, these women, even years after the completion of treatment, were experiencing more stress response symptoms than the TC survivors.
Relevant components of the caregiver's burden consist of the support, assistance and information needs that, if not unmet, leads to reduced QoL and high levels of distress (32). Kim et al. (33) demonstrated that caregivers of cancer patients frequently have a variety of unmet needs and that unmet needs strongly predicted their QoL.
Patients, caregivers and care providers had different expectations about TC survivorship: psychological distress was considered as highly relevant by 35% of patients and caregivers and 93% of care providers; the couple's relationship was quite or very difficult for 12% of patients and caregivers in comparison to 64% in the perception of care providers (34). A different perception of the illness experience could affect the recognition and ability to respond to the needs of patients and caregivers. In another study, close relatives of men suffering from TC highlight four themes: the disease and its course, normalization, the long-term consequences, and the social network (35). The results showed that relatives suffer from social isolation (35).
Another source of caregiver burden could be the fertility issue: the paternity rates among men who attempted to conceive a child after treatment were 71% at 15 years and 76% at 20 years after orchiectomy, but this rate ranged from 48% in the HDCT group to 92% in the surveillance group (36). Sandén and Söderhamn (37) reported a conversational interview to a young woman whose partner had TC using a semistructured guide with open-ended questions. Caring became primary for female partner, and she focused less on her own needs in order to support the patient; everyday life changed, as more time was spent at the hospital, the home, and the parent's home. The third keypoint was the shortness of time: from the discovery of the disease and the start of chemotherapy, time was reported as passing very quickly, and the felt like they spent a lot of time with their physicians.
In literature, little data exists about the role of mothers as caregiver of TC patients and the dramatic changes in their lives. Unlike their healthy peers, young TC patients often face greater challenges in life: they may experience delays in developmental milestones, difficulties in employment and interpersonal relationships, and medical and institutional problems (e.g., economy, education, transport). These challenges can hinder their transition to independence, which is not favored by mothers who continue to take care even when their sons progress to adulthood (38).
Caregiver Therapy
Caregivers need a large volume of information, including: diagnosis-related information, prognosis-related information, treatment-related information, information on homecare, and information about impact on the family or on relationship with partner. Therefore, psychoeducational interventions have been conceived to increase their knowledge. Bultz et al. (39) reported that this sort of intervention had a positive impact on caregivers' ability to provide care and also improve marital satisfaction of patients. Pelusi et al. (40) revealed that caregivers sharing their cancer experience with others in storytelling is essential to offer educational information and emotional support to those who hear it, but also care for self is an important component of managing the course of these events. A Chinese study explored the relationship between family resilience and the post-traumatic growth, and the quality of life of survivors of breast cancer, demonstrating that family resilience decreased caregivers' and patients' burden (41). One intervention used telephone interpersonal counseling, which was delivered to patients and their caregivers separately to improve cancer education and resulted in significant decreases in depression and anxiety levels in the caregivers group (42). Kozachik et al. (43) conducted a quasi-experimental study to describe the use of complementary therapy (such as reflexology, guided imagery, and reminiscence therapy) to cancer patients undergoing chemotherapy and their family caregivers. The authors were unable to draw conclusions regarding the impact of complementary therapy on caregiver burden, however they suggest that one complementary therapy may be incorporated into patients' and caregivers' courses of cancer treatment (43).
According to the different stage of the disease at diagnosis, several treatment strategies are recommended (Table 1). These modalities are associated with different complications and late toxicities and a negative impact on QoL. TC survivors have a high risk of leukemia; the relative risk, associated with the previous use of etoposide, ranges between 3.5 and 4.5 and appears often within 10 years following the end of treatment (44). Younger age at radiotherapy and/or chemotherapy increases risk for solid secondary tumors and remains elevated for at least 35 years (45). In long-term setting pulmonary toxicity, infections and cardiovascular events are higher compared with the general population (46, 47). For TC survivors and their caregivers, preserved fertility is a fundamental subject which has an important impact on their QoL (48). The prospect of paternity improves with the decreasing number of cycles of chemotherapy, therefore the correct management of TC requires a careful balance between the intensity of treatment and burden of disease, in order to limit short and long term adverse events (49). In sight of this, the correct management of late toxicities is essential in order to preserve the higher QoL of patients and their caregivers. A recent multidisciplinary consensus conference by the Italian Germ cell cancer Group (IGG) and the Associazione Italiana di Oncologia Medica (AIOM) has provided recommendations for surveillance and follow-up appointments of men with TC, suggesting a visit with caregiver at the beginning of follow-up and, eventually, a psychological consultation (50).
To date there are no evidence about the importance of the role of nurse in supporting caregivers of TC-patients. In our opinion, it is important to develop educational programs with the aim of creating a cancer clinical nurse specialist role, who could support patients and their families during the course of disease. This program could guarantee personalized nursing assistance and aid (both psychological and practical), leaving from the psychosocial contest of the patients. The role of nurse is expressed before, during and after the identification and the monitoring of signs and symptoms of the disease and the treatment, in order to promote the well-being of the patients and their caregivers.
TC patients and their families have to be included; they should have the opportunity to be involved in the planning of the assistance and in the decision making process through individualized services which could adapt to the changing psychophysical status of the patients (51).
Conclusions
Cancer treatment is not an individual experience, but induces deep effects on patients' families. Couples who achieve the survivorship phase often have to change life plans, deal with TC and treatment-related effects, and manage worries about future health (52). Patients partnered at diagnosis experience a better emotional and physical adaptation to disease (53, 54) and the majority of follow-up studies reported that the rate of divorce or broken relationship was 5% to 10% (55). The impact of disease on caregivers depends also on patients' story. TC patients who undergo, after orchiectomy, one cycle of chemotherapy probably have a lower burden of distress compared with patients who complete four standard cycles of chemotherapy, due to the reduced treatment load. Moreover, some patients are not cured with first-line chemotherapy and have to be treated with further intensified chemotherapeutic regimens, including standard dose chemotherapy supported by granulocyte-colony stimulating factor (G-CSF) (3) and/or HDCT with support of autologous peripheral-blood stem-cell (56, 57). HDCT is a stressful program both for patients and their family, due to long hospitalization periods and a high risk of treatment-related toxicity that requires the adoption of specific precautionary measures. These therapeutic options are able to lead to long-term remission of disease, but leave a stressful emotional burden on the patient and his caregivers. There is some data available about stressful burden of caregivers of elderly persons with physical dependence (58), but there are little evidence about young patients' caregivers, though often they are young people at risk of psychological distress which could have an impact on long-term effects (59, 60).
Unfortunately, there are little data available in literature concerning the role of caregiver in TC patients, probably because of the lower number of persons involved compared with breast cancer, for example. However, in our opinion, according to the young age of patients and the very good prognosis, it is important to consider a more integrated system of the patient and his social support, with the purpose of improving QoL not only during active treatment, but also in the follow-up period, and to encourage a less traumatic return to the everyday life.
Author Contributions
SD, CC, and UD collaborated in the conception, in the data retrieval, and in the drafting of the text. CC, GS, and MC collaborated in the revision of the text and in the completion of the bibliographic research. AB, TB, AF, CM, SB, AA, SP, SM, MC, GB, LG, and MM revised the manuscript.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Footnotes
References
1. Fizazi K, Oldenburg J, Dunant A, Chen I, Salvioni R, Hartmann JT, et al. Assessing prognosis and optimizing treatment in patients with postchemotherapy viable nonseminomatous germ-cell tumors (NSGCT): results of the sCR2 international study. Ann Oncol. (2008) 19:259–64. doi: 10.1093/annonc/mdm472
2. De Giorgi U, Demirer T, Wandt H, Taverna C, Siegert W, Bornhauser M, et al. Second-line high-dose chemotherapy in patients with mediastinal and retroperitoneal primary non-seminomatous germ cell tumors: the EBMT experience. Ann Oncol. (2005) 16:146–51. doi: 10.1093/annonc/mdi017
3. Kondagunta GV, Bacik J, Donadio A, Bajorin D, Marion S, Sheinfeld J, et al. Combination of paclitaxel, ifosfamide, and cisplatin is an effective second-line therapy for patients with relapsed testicular germ cell tumors. J Clin Oncol. (2005) 23:6549–55. doi: 10.1200/JCO.2005.19.638
4. Oing C, Seidel C, Bokemeyer C. Therapeutic approaches for refractory germ cell cancer. Expert Rev Anticancer Ther. (2018) 18:389–97. doi: 10.1080/14737140.2018.1450630
5. De Giorgi U, Rosti G, Aieta M, Testore F, Burattini L, Fornarini G, et al. Phase II study of oxaliplatin and gemcitabine salvage chemotherapy in patients with cisplatin-refractory nonseminomatous germ cell tumor. Eur Urol. (2006) 50:1032–8. doi: 10.1016/j.eururo.2006.05.011
6. Rossen PB, Pedersen AF, Zachariae R, Von Der Maase H. Health-related quality of life in long-term survivors of testicular cancer. J Clin Oncol. (2009) 27:5993–9. doi: 10.1200/JCO.2008.19.6931
7. Shinn EH, Swartz RJ, Thornton BB, Spiess PE, Pisters LL, Basen-Engquist KM. Testis cancer survivors' health behaviors: comparison with age-matched relative and demographically matched population controls. J Clin Oncol. (2010) 28:2274–9. doi: 10.1200/JCO.2009.23.9608
8. Rolland JS. Cancer and the family: an integrative model. Cancer. (2005) 104 (Suppl. 11):2584–95. doi: 10.1002/cncr.21489
9. Hudson P, Payne S. Family caregivers and palliative care: current status and agenda for the future. J Palliat Med. (2011) 14:864–9. doi: 10.1089/jpm.2010.0413
10. Hudson P, Payne S. The future of family caregiving: research, social policy and clinical practice. In: Hudson P, Payne S, editors. Family Carers in Palliative Care: A Guide for Health and Social Care Professionals. Oxford: Oxford University Press (2009). p. 277–303.
11. Romito F, Goldzweig G, Cormio C, Hagedoorn M, Andersen BL. Informal caregiving for cancer patients. Cancer. (2013) 119 (Suppl. 11):2160–9. doi: 10.1002/cncr.28057
12. Given CW, Stommel M, Given BA, Osuch J, Kurtz ME, Kurtz JC. The influence of cancer patients' symptoms and functional status on patients' depression and family caregivers' reaction and depression. Health Psychol. (1993) 12:277–85.
13. Northouse LL. Helping families of patients with cancer. Oncol Nurs Forum. (2005) 32 743–50. doi: 10.1188/04.ONF.743-750
14. Stenberg U, Ruland CM, Miaskowski C. Review of the literature on the effects of caring for a patient with cancer. Psychooncology. (2010) 19:1013–25. doi: 10.1002/pon.1670
15. Pitceathly C, Maguire P. The psychological impact of cancer on patients' partners and other key relatives: a review. Eur J Cancer. (2003) 39:1517–24. doi: 10.1016/s0959-8049(03)00309-5
16. Fleer J, Hoekstra HJ, Sleijfer DT, Tuinman MA, Klip EC, Hoekstra-Weebers JE. Quality of life of testicular cancer survivors and the relationship with sociodemographics, cancer-related variables, and life events. Support Care Cancer. (2006) 14:251–9. doi: 10.1007/s00520-005-0879-3
17. Arai Y, Kawakita M, Hida S, Terachi T, Okada Y, Yoshida O. Psychosocial aspects in long-term survivors of testicular cancer. J Urol. (1996) 155:574–8. doi: 10.1016/S0022-5347(01)66452-8
18. Jones GY, Payne S. Searching for safety signals: the experience of medical surveillance amongst men with testicular teratomas. Psychooncology. (2000) 9:385–94. doi: 10.1002/1099-1611(200009/10)9:5<385::AID-PON467>3.0.CO;2-B
19. Chovanec M, Vasilkova L, Setteyova L, Obertova J, Palacka P, Rejlekova K, et al. Long-term cognitive functioning in testicular germ-cell tumor survivors. Oncologist. (2018) 23:617–23. doi: 10.1634/theoncologist.2017-0457
20. Kent EE, Rowland JH, Northouse L, Litzelman K, Chou WYS, Shelburne N, et al. Caring for caregivers and patients: research and clinical priorities for informal cancer caregiving. Cancer. (2016) 122:1987–95. doi: 10.1002/cncr.29939
21. Gil T, Sideris S, Aoun F, van Velthoven R, Sirtaine N, Paesmans M, et al. Testicular germ cell tumor: short and long-term side effects of treatment among survivors. Mol Clin Oncol. (2016) 5:258–64. doi: 10.3892/mco.2016.960
22. Rabow MW, Hauser JM, Adams J. Supporting family caregivers at the end of life: “they don't know what they don't know.” J Am Med Assoc. (2004) 291:483–91. doi: 10.1001/jama.291.4.483
23. Hagedoorn M, Buunk B, Kuijer R, Wobbes T, Sanderman R. Couples dealing with cancer: role and gender differences regarding psychological distress and quality of life. Psychooncology. (2000) 9:232–42. doi: 10.1002/1099-1611(200005/06)9:3<232::aid-pon458>3.0.co;2-j
24. Grunfeld E, Coyle D, Whelan T, Clinch J, Reyno L, Earle CC, et al. Family caregiver burden: results of a longitudinal study of breast cancer patients and their principal caregivers. CMAJ. (2004) 170:1795–801. doi: 10.1503/cmaj.1031205
25. Traeger L, Greer JA, Fernandez-Robles C, Temel JS, Pirl WF. Evidence-based treatment of anxiety in patients with cancer. J Clin Oncol. (2012) 30:1197–205. doi: 10.1200/JCO.2011.39.5632
26. Gröpper S, van der Meer E, Landes T, Bucher H, Stickel A, Goerling U. Assessing cancer-related distress in cancer patients and caregivers receiving outpatient psycho-oncological counseling. Support Care Cancer. (2016) 24:2351–7. doi: 10.1007/s00520-015-3042-9
27. Tuinman MA, Hoekstra HJ, Sleijfer DT, Fleer J, Vidrine DJ, Gritz ER, et al. Testicular cancer: a longitudinal pilot study on stress response symptoms and quality of life in couples before and after chemotherapy. Support Care Cancer. (2007), 15:279–86. doi: 10.1007/s00520-006-0119-5
28. Warner EL, Kent EE, Trevino KM, Parsons HM, Zebrack BJ, Kirchhoff AC. Social well-being among adolescents and young adults with cancer: a systematic review. Cancer. (2016) 122:1029–37. doi: 10.1002/cncr.29866
29. Gritz ER, Wellisch DK, Siau J, Wang HJ. Long-term effects of testicular cancer on sexual functioning in married couples. Cancer. (1989) 64: 1560–7.
30. Hannah MT, Gritz ER, Wellisch DK, Fobair P, Hoppe RT, Bloom JR, et al. Changes in marital and sexual functioning in long-term survivors and their spouses: testicular cancer versus Hodgkin's disease. Psychooncology. (1992) 1:89–103.
31. Tuinman MA, Fleer J, Hoekstra HJ, Sleijfer DT, Hoekstra-Weebers JE. Quality of life and stress response symptoms in long-term and recent spouses of testicular cancer survivors. Eur J Cancer. (2004) 40:1696–703. doi: 10.1016/j.ejca.2004.03.020
32. Printz C. Cancer caregivers still have many unmet needs. Cancer. (2011) 117:1331. doi: 10.1002/cncr.26075
33. Kim H, Yi M. Unmet needs and quality of life of family caregivers of cancer patients in south korea. Asia Pac J Oncol Nurs. (2015) 2:152–9. doi: 10.4103/2347-5625.158019
34. De Padova S, Rosti G, Scarpi E, Salvioni R, Amadori D, De Giorgi U. Expectations of survivors, caregivers and healthcare providers for testicular cancer survivorship and quality of life. Tumori. (2011) 97:367–73. doi: 10.1700/912.10036
35. Sanden I, Hyden LC. How everyday life is affected: an interview study of relatives of men suffering from testicular cancer. J Psychosoc Oncol. (2002) 20:27–44. doi: 10.1300/J077v20n02_02
36. Brydøy M, Fosså SD, Klepp O, Bremnes RM, Wist EA, Wentzel-Larsen T, et al. Paternity following treatment for testicular cancer. J Natl Cancer Inst. (2005) 97:1580–8. doi: 10.1093/jnci/dji339
37. Sandén I, Söderhamn O. Experience of living in a disrupted situation as partner to a men with testicular cancer. Am J Mens Health. (2009) 3:126–33. doi: 10.1177/1557988307311289
38. Deatrick JA, Hobbie W, Ogle S, et al. Competence in caregivers of adolescent and young adult childhood brain tumor survivors. Health Psychol. (2013) 33:1103–12. doi: 10.1037/a0033756
39. Bultz BD, Speca M, Brasher PM, Geggie PH, Page SA. A randomized controlled trial of a brief psychoeducational support group for partners of early stage breast cancer patients. Psychooncology. (2000) 9:303–13. doi: 10.1002/1099-1611(200007/08)9:4<303::AID-PON462>3.0.CO;2-M
40. Pelusi J, Krebs LU, Castro L. Understanding cancer—understanding the stories of life and living. J Cancer Edu. (2005) 20 (Suppl. 1):12–6. doi: 10.1207/s15430154jce2001s_04
41. Liu Y, Li Y, Chen L, Li Y, Qi W, Yu L. Relationships between family resilience and posttraumatic growth in breast cancer survivors and caregiver burden. Psychooncology. (2018) 27:1284–90. doi: 10.1002/pon.4668
42. Badger T, Segrin C, Meek P, Lopez AM, Bonham E, Sieger A. Telephone interpersonal counseling with women with breast cancer: symptom management and quality of life. Oncol Nurs Forum. (2005) 32:273–9. doi: 10.1188/05.ONF.273-279
43. Kozachik SL, Wyatt G, Given CW, Given BA. Patterns of use of complementary therapies among cancer patients and their family caregivers. Cancer Nurs. (2006) 29:84–94. doi: 10.1097/00002820-200603000-00002
44. Richiardi L, Scélo G, Boffetta P, Hemminki K, Pukkala E, Olsen JH, et al. Second malignancies among survivors of germ-cell testicular cancer: a pooled analysis between 13 cancer registries. Int J Cancer. (2007) 120:623–31. doi: 10.1002/ijc.22345
45. Ng AK, Kenney LB, Gilbert ES, Travis LB. Secondary malignancies across the age spectrum. Semin Radiat Oncol. (2010) 20:67–78. doi: 10.1016/j.semradonc.2009.09.002
46. Travis LB, Beard C, Allan JM, Dahl AA, Feldman DR, Oldenburg J, et al. Testicular cancer survivorship: research strategies and recommendations. J Natl Cancer Inst. (2010) 102:1114–30. doi: 10.1093/jnci/djq216
47. Huddart RA, Norman A, Shahidi M, Horwich A, Coward D, Nicholls J, et al. Cardiovascular disease as a long-term complication of treatment for testicular cancer. J Clin Oncol. (2003) 21:1513–23. doi: 10.1200/JCO.2003.04.173
48. Stoehr B, Schachtner L, Pichler R, Holzner B, Giesinger J, Oberguggenberger A, et al. Influence of achieved paternity on quality of life in testicular cancer survivors. BJU Int. (2013) 111 (4 Pt B):E207–12. doi: 10.1111/j.1464-410X.2012.11579.x
49. Brydøy M, Fosså SD, Klepp O, Bremnes RM, Wist EA, Wentzel-Larsen T, et al. Paternity and testicular function among testicular cancer survivors treated with two to four cycles of cisplatin-based chemotherapy. Eur Urol. (2010) 58:134–40. doi: 10.1016/j.eururo.2010.03.041
50. Banna GL, Nicolai N, Palmieri G, Ottaviano M, Balzarini L, Barone D, et al. Recommendations for surveillance and follow-up of men with testicular germ cell tumors: a multidisciplinary consensus conference by the Italian Germ cell cancer Group and the Associazione Italiana di Oncologia Medica. Crit Rev Oncol Hematol. (2019) 137:154–64. doi: 10.1016/j.critrevonc.2019.03.006
51. Dreyer B, Macfarlane K, Hendry D. The testicular cancer nurse specialist: a pivotal role in patient care. Br J Nurs. (2018) 27:S26–7. doi: 10.12968/bjon.2018.27.18.S26
52. Carpentier MY, Fortenberry JD. Romantic and sexual relationships, body image, and fertility in adolescent and young adult testicular cancer survivors: a review of the literature. J Adolesc Health. (2010) 47:115–25. doi: 10.1016/j.jadohealth.2010.04.005
53. Brodsky MS. Testicular Cancer Survivors' Impressions of the Impact of the Disease on their Lives. Qual Health Res. (1995) 5:78–96. doi: 10.1177/104973239500500106
54. Sheppard C, Wylie KR. An assessment of sexual difficulties in men after treatment for testicular cancer. Sex Relatsh Ther. (2001) 16:47–58. doi: 10.1080/14681990124325
55. Fosså SD, Travis LB, Dahl AA. Medical and psychosocial issues in testicular cancer survivors. In: Oncology: An Evidence-Based Approach. New York, NY: Springer (2006). p. 1825–37.
56. Adra N, Abonour R, Althouse SK, Albany C, Hanna NH, Einhorn LH. High-dose chemotherapy and autologous peripheral-blood stem-cell transplantation for relapsed metastatic germ cell tumors: the Indiana university experience. J Clin Oncol. (2017) 35:1096–102. doi: 10.1200/JCO.2016.69.5395
57. Pedrazzoli P, Ferrante P, Kulekci A, Schiavo R, De Giorgi U, Carminati O, et al. Autologous hematopoietic stem cell transplantation for breast cancer in Europe: critical evaluation of data from the European Group for Blood and Marrow Transplantation (EBMT) Registry 1990–1999. Bone Marrow Transplant. (2003) 32:489–94. doi: 10.1038/sj.bmt.1704153
58. Navarro-Sandoval C, Uriostegui-Espìritu LC, Delgado-Quinones EG, Sahagùn-Cuevas MN. Depression and burden on primary caregivers of elderly persons with physical dependence of the UMF 171. Rev Med Inst Mex Seguro Soc. (2017) 55:25–31.
59. Kenney LB, Antal Z, Ginsberg JP, Hoppe BS, Bober SL, Yu RN, et al. Improving male reproductive health after childhood, adolescent, and young adult cancer: progress and future directions for survivorship research. J Clin Oncol. (2018) 36:2160–8. doi: 10.1200/JCO.2017.76.3839
Keywords: caregiver, testicular, cancer, patients, long-term survivors
Citation: De Padova S, Casadei C, Berardi A, Bertelli T, Filograna A, Cursano MC, Menna C, Burgio SL, Altavilla A, Schepisi G, Prati S, Montalti S, Chovanec M, Banna GL, Grassi L, Mego M and De Giorgi U (2019) Caregiver Emotional Burden in Testicular Cancer Patients: From Patient to Caregiver Support. Front. Endocrinol. 10:318. doi: 10.3389/fendo.2019.00318
Received: 26 February 2019; Accepted: 01 May 2019;
Published: 28 May 2019.
Edited by:
Gabriella Castoria, Second University of Naples, ItalyReviewed by:
Silvio Naviglio, Università degli Studi della Campania Luigi Vanvitelli Caserta, ItalyErika Di Zazzo, Università degli Studi della Campania Luigi Vanvitelli Caserta, Italy
Copyright © 2019 De Padova, Casadei, Berardi, Bertelli, Filograna, Cursano, Menna, Burgio, Altavilla, Schepisi, Prati, Montalti, Chovanec, Banna, Grassi, Mego and De Giorgi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ugo De Giorgi, ugo.degiorgi@irst.emr.it
 Silvia De Padova
Silvia De Padova Chiara Casadei
Chiara Casadei Alejandra Berardi1
Alejandra Berardi1 Maria Concetta Cursano
Maria Concetta Cursano Giuseppe Schepisi
Giuseppe Schepisi Michal Chovanec
Michal Chovanec Giuseppe Luigi Banna
Giuseppe Luigi Banna Luigi Grassi
Luigi Grassi Michal Mego
Michal Mego Ugo De Giorgi
Ugo De Giorgi