A Systematic Review and Meta-Analysis of the Prevalence and Risk Factors of Depression in Type 2 Diabetes Patients in China
- 1School of Health Preservation and Rehabilitation, Chengdu University of Traditional Chinese Medicine, Chengdu, China
- 2Department of Rehabilitation, Fushun County People's Hospital, Zigong, China
- 3Affiliated Rehabilitation Hospital of Chengdu University of Traditional Chinese Medicine /Sichuan Province Rehabilitation Hospital, Chengdu, China
Background: The prevalence of type 2 diabetes mellitus (T2DM) is increasing in China. Depression in patients with T2DM interferes with blood glucose management, leads to poor treatment outcomes, and has a high risk of dementia and cardiovascular event. We conducted this systematic review and meta-analysis to evaluate the prevalence of depression in patients with T2DM in China and explore potential risk factors associated with depression in T2DM.
Methods: We conducted a literature search in MEDLINE/PubMed, EMBASE, the Cochrane Library, the Chinese Biomedical Literature Database (CBM), the China National Knowledge Infrastructure (CNKI), the Chinese Science and Technology Periodical Database (VIP), and the Wanfang Database from their inception to February 25, 2022 to include population-based, cross-sectional surveys that investigated the prevalence of depression in Chinese T2DM patients and studied possible risk factors. Gray literature and reference lists were also manually searched. We used the Agency for Healthcare Research and Quality methodology checklist to assess the risk of bias in the included studies. Two reviewers screened studies, extracted data, and evaluated the risk of bias independently. The primary outcome was the pooled prevalence of depression in Chinese T2DM patients, and the secondary outcomes included potential risk factors for depression in T2DM patients. R (version 3.6.1) and Stata (version 12.0) software were used for data synthesis.
Results: We included 48 reports that identified 108,678 subjects. Among the included reports, 4 were rated as low risk of bias, 40 moderate risks of bias, and 4 high risks of bias. The prevalence of depression in T2DM patients in China was 25.9% (95% CI 20.6%−31.6%). The prevalence of depression was higher in women (OR = 1.36, 95% CI 1.19–1.54), subjects ≥60 years (OR = 1.56, 95% CI 1.14–2.14), with a primary school or lower education (vs. middle or high school education (OR = 1.49, 95% CI 1.16 – 1.92); vs. college degree or higher education (OR = 1.84, 95% CI 1.16 – 2.92), with a duration of T2DM ≥ 10 years (OR = 1.68, 95% CI 1.11–2.54), with complications (OR = 1.90, 95% CI 1.53–2.36), insulin users (OR = 1.46, 95% CI 1.09–1.96) and individuals living alone (OR = 2.26, 95% CI 1.71–2.98). T2DM patients with current alcohol use had a lower prevalence of depression (OR = 0.70, 95% CI 0.58–0.86). Prevalence varied from 0.8 to 52.6% according to different instruments used to detect depression.
Conclusion: The prevalence of depression in T2DM patients is remarkable in China. Potential risk factors of depression in T2DM patients included women, age ≥ 60 years, low educational level, complications, duration of diabetes ≥ 10 years, insulin use, and living alone. High-quality epidemiological investigations on the prevalence of depression in Chinese T2DM patients are needed to better understand the status of depression in T2DM.
Systematic Review Registration: https://www.crd.york.ac.uk/PROSPERO/, identifier: CRD42020182979.
Introduction
Type 2 diabetes mellitus (T2DM) is a common chronic metabolic disease, accounting for 90%−95% of all cases (1). The highest proportions occur in low- and middle-income countries (2). According to the International Diabetes Federation (IDF) (3) and summary data by Ma (4), China has the largest diabetes population and is one of the countries with a sharp increase in diabetes prevalence worldwide, which is mainly attributed to T2DM (4). The latest statistics show that the overall prevalence of T2DM in China is 9.1% (5).
Depression refers to persistent sadness and a loss of interest or pleasure in previously rewarding or enjoyable activities (6). It prevails in T2DM patients, and numerous studies have suggested a bidirectional relationship between T2DM and depression (7–9). The association between the two conditions may cause a shared etiology, including alterations of the hypothalamic-pituitary-adrenal axis, inflammation, hippocampal structural alterations, and weight gain (7, 10). Nouwen et al. (11) report that T2DM patients have a 24% increased risk of developing depression compared to healthy individuals based on global data. Comorbid depression and T2DM appear to have an additive impact on patients, which results in poor compliance (12), worse quality of life (13), higher risk of dementia (14), and cardiovascular events (15, 16).
Globally, 28% of T2DM patients have depression of different degrees (17), and 14.5% have major depressive disorder (18). In developing countries, epidemiological studies show that depression in patients with T2DM ranges from 34 to 54% (19–21). Since China has a large T2DM population, the number of patients with T2DM and comorbid depression could be huge. Numerous cross-sectional surveys have investigated the prevalence of depression in Chinese T2DM patients, but the results vary. Although several studies have reported diverse risk factors associated with the prevalence of depression in T2DM patients, such as gender, age, educational level, complications, and lifestyle, the risk factors are inconsistent (22–24). A systematic review (SR) of the prevalence of depression in Chinese patients with T2DM has been conducted. This SR included 26 studies published up to 2016 (25). Since more surveys have been carried out in recent years, we conducted this SR and meta-analysis to update the current epidemiological data about the prevalence of depression in patients with T2DM in China and explore the potential risk factors associated with depression in patients with T2DM.
Materials and Methods
Study Registration
This SR adhered to the Preferred Reporting Items for Systematic reviews and Meta-Analysis (PRISMA) (26) and the Meta-analysis Of Observational Studies in Epidemiology (MOOSE) guidelines (27) (Supplementary File 1). The protocol was registered at the International Prospective Register of Systematic Reviews https://www.crd.york.ac.uk/PROSPERO/ (registration ID: CRD42020182979) and had been published (28).
Search Strategy
We searched MEDLINE/PubMed, EMBASE, the Cochrane Library, the Chinese Biomedical Literature Database (CBM), the China National Knowledge Infrastructure (CNKI), the Chinese Science and Technology Periodical Database (VIP), and Wanfang Database from their inception to February 25, 2022, to collect the studies that reported the prevalence of depression in patients with T2DM in China. We combined Medical Subject Headings and free text words related to China, diabetes, and depression, to search the aforementioned electronic databases. Supplementary File 2 shows the search strategies of all databases. We manually searched gray literature, reference lists of included articles and relevant SRs for additional eligible studies. Relevant websites were also searched for useful data and we consulted experts for possible relevant studies.
Study Selection
After filtering duplicate records, two independent reviewers (HLZ and JZ) screened the titles and abstracts of the remaining records for potentially eligible studies. Then, full texts were obtained and checked independently by two reviewers (XBL and XH). The studies were eligible if they met the following criteria:
Study characteristics: (1) Cross-sectional studies selecting subjects from the general population or community; (2) Reported the prevalence of depression in Chinese T2DM patients or/and investigated possible risk factors associated with depression in T2DM, regardless of sample size; (3) Published in English or Chinese.
Participant characteristics: (1) Chinese adults (≥18 years) diagnosed with T2DM with no restrictions on gender; (2) Diagnosis of T2DM based on self-reported physician's diagnosis, medical records, or glucose testing (fasting plasma glucose ≥ 7.0 mmol/L and/or 2-hour postprandial plasma glucose ≥ 11.1 mmol/L)(29); (3) Depression was evaluated with scales that have been verified with good validity and reliability in the Chinese population, or patients diagnosed as major depressive disorder by operationalized criteria such as the Diagnostic and Statistical Manual of Mental Disorders (DSM) or the International Statistical Classification of Diseases and Related Health Problems 10th Revision (ICD-10).
Type of outcome measurements: (1) The primary outcome was the pooled prevalence of depression in Chinese patients with T2DM; (2) Secondary outcomes contained potential risk factors of depression in patients with T2DM in China, such as gender, age, educational level, duration of T2DM, complications, insulin use, lifestyle, etc.
Hospital-based studies, randomized controlled trials, case studies, qualitative studies, systematic reviews, protocols, editorials, and conference abstracts were excluded. We also excluded duplicates. Studies were also excluded when the full text or data were unavailable by all useful approach.
Data Extraction
Two reviewers (XBL and XH) independently extracted data using a predefined data extraction Microsoft Excel spreadsheet. The extracted data were:
(1) Study characteristics: title, journal, published year(s), survey period, geographical region, method of data collection, diagnostic criteria of diabetes, and instruments used to define depression, source of funding, and information regarding the risk of bias assessment.
(2) Participants' information at study level: mean age, gender, duration of diabetes, educational level, lifestyle (smoking status, alcohol use, living status), complications, insulin use, marital status (normal/abnormal [separated, divorced, widowed]).
(3) Critical data: sample size, the total number of subjects with depression, the number of subjects with depression according to age, gender, educational level, lifestyle, and other risk factors affecting prevalence.
We contacted the corresponding authors by e-mail for any incomplete information and data. The extracted data were cross-checked, and a third reviewer (JL) was invited to arbitrate disagreements.
Risk of Bias Assessment
Two reviewers (YXL and DLZ) assessed the risk of bias of the included studies independently by the Agency for Healthcare Research and Quality (AHRQ) methodology checklist, which is devised for cross-sectional/prevalence studies (30). The AHRQ methodology checklist consists of 11 items. Each item is scored as “1” when answered “Yes” and “0” when answered “Unclear” or “No.” Studies are rated as high, moderate, and low risk of bias when quality is scored 0–3, 4–7, and 8–11, respectively. The results of the AHRQ methodology checklist were cross-checked, and disagreements were resolved by team discussion.
Statistical Analysis
All statistical analyses were performed using R (vision 3.6.1) and Stata (vision 12.0) software. The pooled prevalence of depression in T2DM patients was calculated by the metaprop command in R (vision 3.6.1) software, with a 95% confidence interval (CI). We used odds ratio (OR) for categorical data (e.g., female and male, smoker and non-smoker) to explore potential risk factors. The statistical heterogeneity among studies was assessed by Cochran's Q test and the I2 statistic. A P-value <0.1 for the Q test and I2 >50% was set as the threshold for statistically significant heterogeneity. Since heterogeneity was expected, the random-effect model was used to pool all outcomes to give a more conservative estimate of prevalence. We used Kappa statistics to assess inter-rater agreement between reviewers for study inclusion and assessment of the risk of bias (31).
Subgroup Analysis
Subgroup analyses were conducted according to age, residence, duration of T2DM, educational level, complications, insulin use, current smoking status, alcohol use, marital status, living status, and instruments used to detect depression.
Publication Bias
Funnel plots and Egger's test were used to assessed the publication bias for primary outcome.
Sensitivity Analysis
Sensitivity analysis was performed by excluding studies one by one to investigate the robustness of the results and pooling the studies' prevalence with a low, moderate, and high risk of bias, respectively, to explore the impact of studies' risk of bias on results. When asymmetric funnel plots indicated publication bias, we used the trim and fill method by metatrim packages of Stata (vision 12.0) software to quantify the impact of publication bias on results.
Meta-Regression Analysis
Univariable meta-regression analysis was conducted to investigate potential sources of heterogeneity based on characteristics of study level (instruments used to detect depression, risk of bias, publication year, and sample size). Metareg command in R (vision 3.6.1) software was used for analyses.
Results
Included Studies and Characteristics
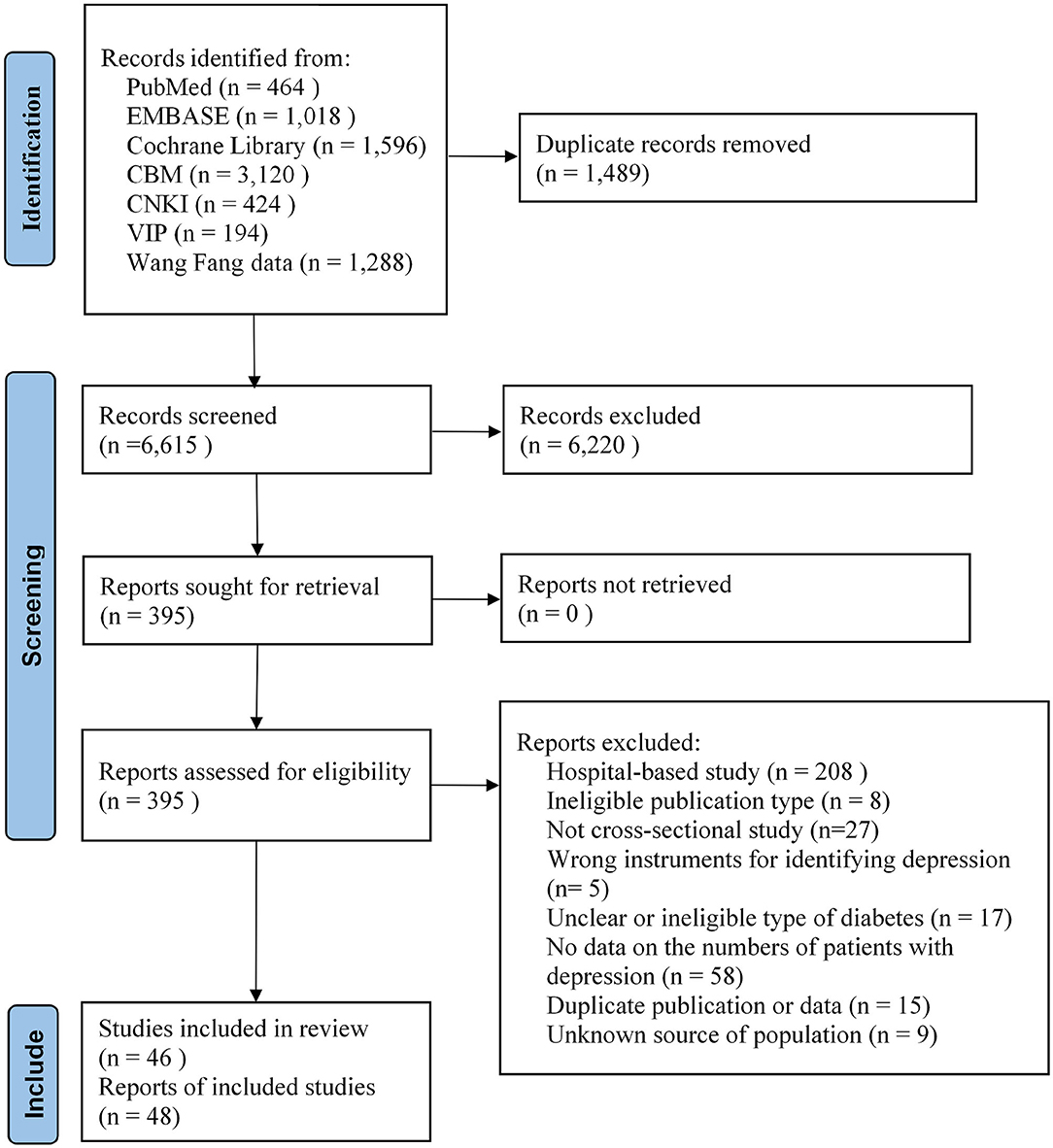
A total of 8,104 articles were identified from the database and gray literature searches. After filtering 1,489 duplicates, we reviewed the titles and abstracts and identified 395 possible eligible records. Then, we checked the full texts and reference lists, and 48 reports (22–24, 32–76) fulfilled the eligible criteria. The list of excluded records with justification are provided in Supplementary File 3. Among the included reports, the sample of Sun et al. (22) and Zheng et al. (47) was a separate part of the sample of Zhang et al. (52) and Sun et al. (49). We used these as supplemental data for subgroup analysis. Inter-rater agreement between reviewers for study selection was excellent (Kappa statistics = 0.78). A PRISMA flow diagram of the selection process is presented in Figure 1.
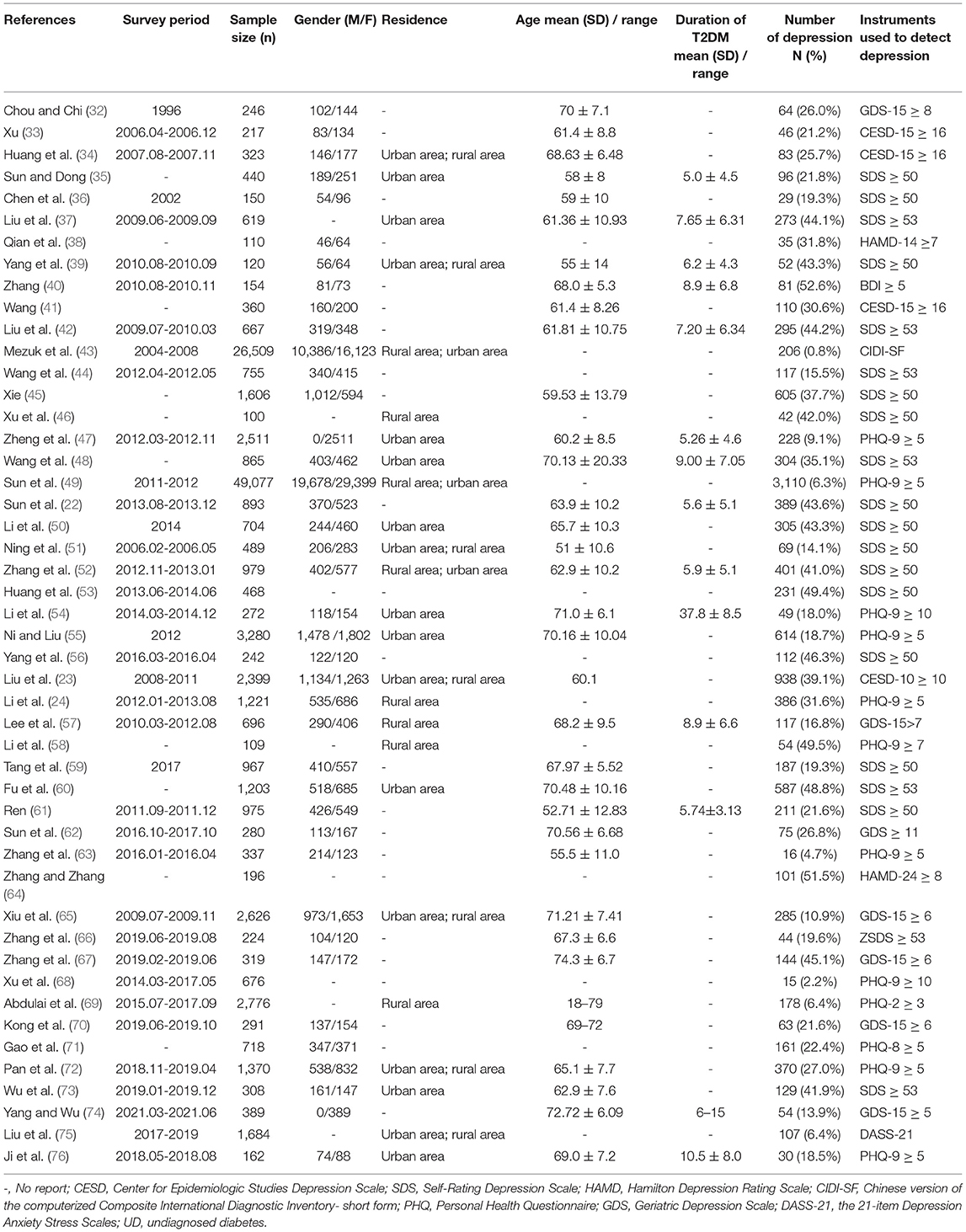
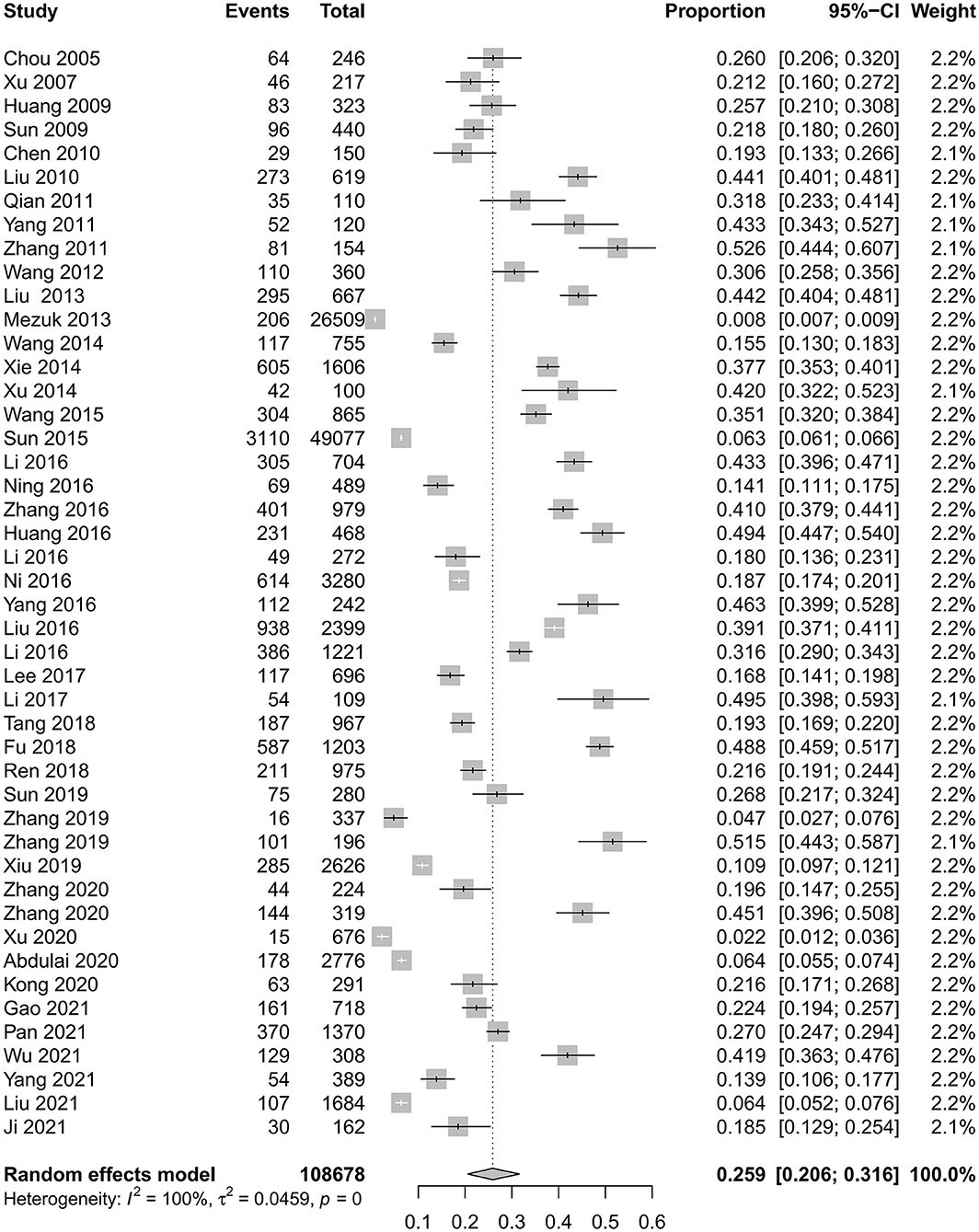
The included studies contained 108,678 adult subjects. The ages of subjects ranged from 18 to 79 years. Three studies (23, 43, 49) were analyzed based on cross-sectional data from large national survey, and the rest were based on the population of different provinces and cities. Most of the studies evaluated depression status with the Self-rating Depression Scale, the Center for Epidemiologic Studies Depression Scale, the Patient Health Questionnaire-9, and the Geriatric Depression Scale. The prevalence of depression in T2DM patients reported in these studies ranged from 0.8% to 52.6%. Mezuk et al. (43) reported the lowest prevalence (0.8%), which included both diagnosed and undiagnosed T2DM in 10 provinces in China and those diagnosed with depression according to the DSM-IV. Zhang et al. (40) reported the highest prevalence (52.6%), which included elderly (≥60 years) T2DM patients and evaluated depression with the Beck depression inventory. Detailed characteristics of the included studies are shown in Table 1.
Risk of Bias
Among the included reports, the AHRQ scores ranged from two to nine. Four reports were rated as low risk of bias, 40 moderate risks of bias, and 4 high risks of bias. Agreement of the risk of bias assessment was excellent (Kappa statistics = 0.8). Supplementary File 4 provides detailed scores of all included studies.
Meta-Analysis
Prevalence of Depression in Patients With T2DM in China
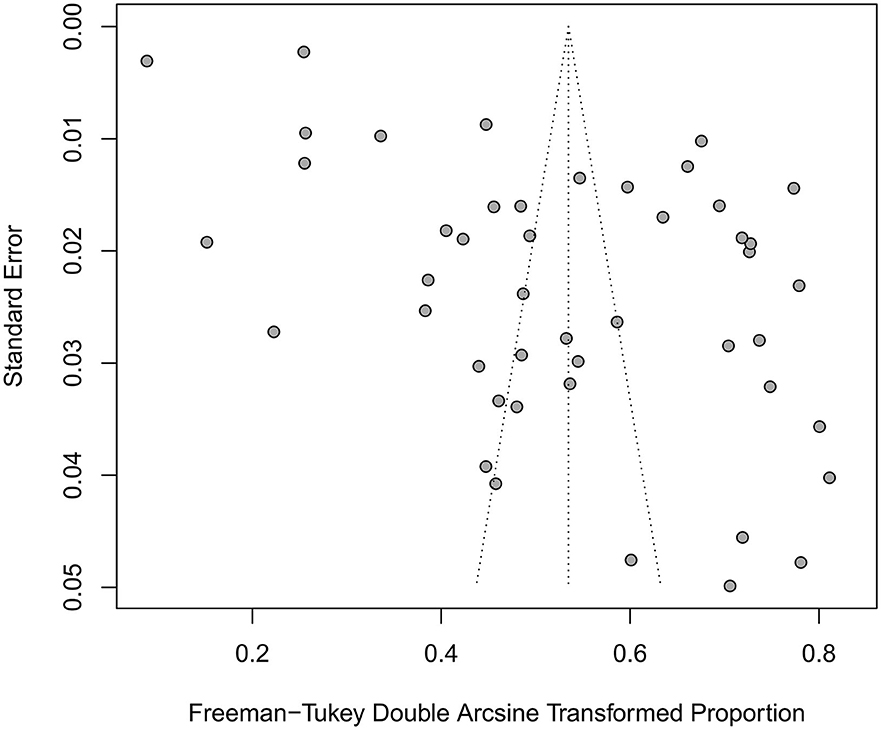
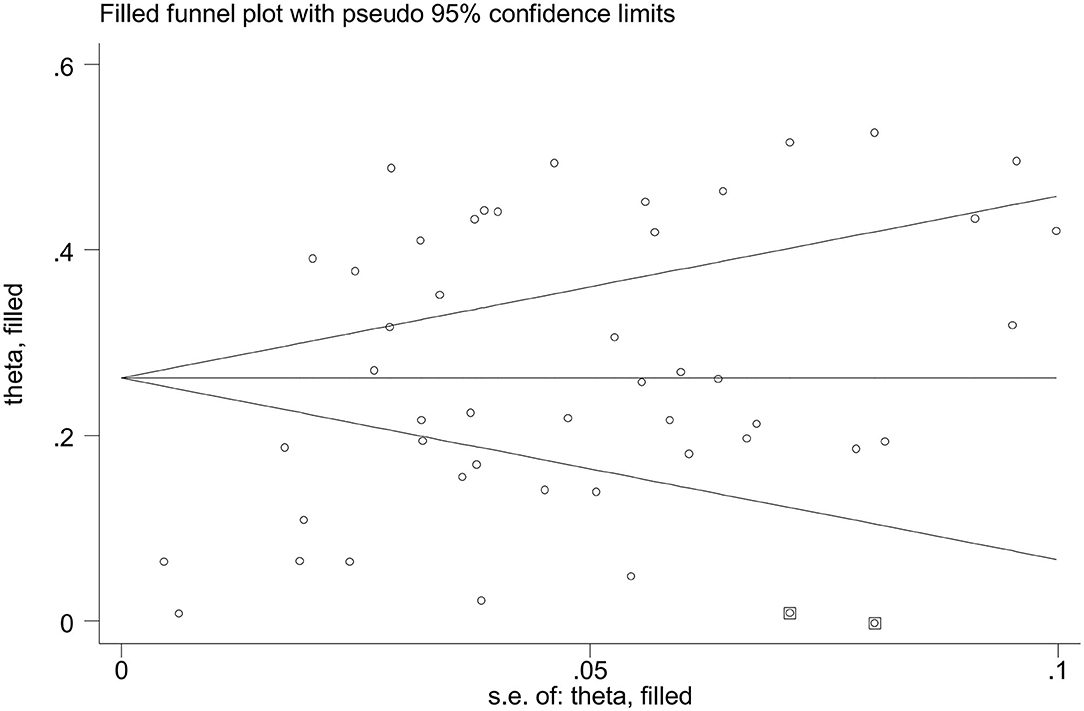
The prevalence of depression in patients with T2DM in China was 25.9% (95% CI 20.6%−31.6%), with statistically significant heterogeneity between studies (I2 = 99.7%, P < 0.0001) (Figure 2). Asymmetric funnel plot indicated publication bias might exist (Figure 3) (Egger's test, P < 0.0001).
Prevalence of Depression in Patients With T2DM According to Gender
Nineteen studies reported the prevalence of depression in patients with T2DM according to gender. Overall, the pooled prevalence of depression in women with T2DM was higher than in men (33.4% [95% CI 24.6%−42.2%; I2 = 99.2%, P < 0.0001] vs. 28.0% [95% CI 18.0%−39.1%; I2 = 99.3%, P < 0.0001]). The OR in women compared with men was 1.36 (95% CI 1.19–1.54; I2 = 64.3%, P < 0.0001).
Prevalence of Depression in Patients With T2DM According to Age
We dichotomized the reported age groups into <60 years and ≥60 years. Overall, the data of subjects ≥60 years was extracted from 18 studies, and <60 years from 7 studies. The pooled prevalence of depression in patients with T2DM was higher in subjects aged ≥60 years compared with those aged <60 years (29.5% [95% CI 24.6%−35.4%; I2 = 96.1%, P < 0.0001] vs.23.7% [95% CI 15.7%−31.8%; I2 = 95.2%, P < 0.0001]). The prevalence of depression in patients with T2DM aged ≥60 years was significantly higher than those aged <60 years (OR = 1.56; 95% CI 1.14–2.14; I2 = 78.5%, P < 0.0001).
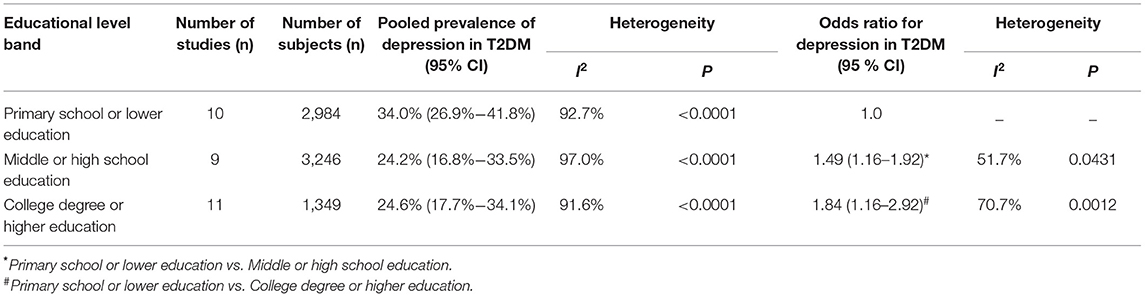
Prevalence of Depression in Patients With T2DM According to Educational Level
We divided education into three levels (primary school or lower education level; middle or high school; a college degree or higher education level). The prevalence of depression in patients with T2DM with primary school or lower education level was 34.0%, middle or high school education 24.2%, and a college degree or above education level 24.6%. In these studies, the prevalence of depression in patients with T2DM increased significantly with low education level (Table 2).
Prevalence of Depression in Patients With T2DM According to Residence
Eleven studies included urban residence. The pooled prevalence of depression in patients with T2DM in urban residents was 27.6% (95% CI 20.2%−36.4%; I2 = 99.0%, P < 0.0001). Six studies included rural residents. The pooled prevalence of depression in patients with T2DM in rural residents was 33.3% (95% CI 15.6%−50.9%; I2 = 99.6%, P < 0.0001). Due to incomparable data, the OR was not calculated.
Prevalence of Depression Between Undiagnosed and Diagnosed T2DM Patients
Seven studies included undiagnosed T2DM patients (those without a history of physician-diagnosed diabetes or use of an antidiabetic drug but with a fasting plasma glucose of 7.0 mmol/L or higher, or a 2-hour postprandial plasma glucose of 11.1 mmol/L or higher). The prevalence of depression in undiagnosed T2DM was 7.3% (95% CI 2.6%−19.1%; I2 = 99.7%, P < 0.0001). The pooled results from 44 included studies showed prevalence of depression in diagnosed patients with T2DM was 27.1% (95%CI 21.4–33.1%; I2 = 99.6%, P < 0.0001).
Prevalence of Depression in T2DM Patients According to the Duration of T2DM
Seven studies reported the prevalence of depression in patients with T2DM according to the duration of diabetes. The duration of diabetes from these studies was divided into three groups: <5 years, 5–10 years, ≥10 years. The prevalence of depression in T2DM with <5 years was 26.3%; in T2DM with 5–10 years was 28.9%; in T2DM with ≥10 years was 29.2%. The prevalence of depression in T2DM patients increased significantly with longer duration of T2DM in these studies (Table 3).
Prevalence of Depression in Patients With T2DM According to Insulin Use
The pooled prevalence of depression in patients with T2DM was higher in subjects using insulin compared with those not using insulin (49.5% [95% CI 44.0 %−55.0%; I2 = 51.8%, P = 0.0654] vs. 38.6% [95% CI 30.4%−46.7%; I2 = 91.9%, P < 0.0001). The OR in insulin users compared with non-insulin users was 1.46 (95% CI 1.09–1.96; I2 = 51.4%, P = 0.0673).
Prevalence of Depression in Patients With T2DM According to Complications
The pooled prevalence of depression in patients with T2DM with complications was higher in subjects without complications (47.3% [95% CI 39.8%−54.8%; I2 = 84.7%, P < 0.0001] vs. 31.1% [95% CI 23.2%−38.9%; I2 = 92.8%, P < 0.0001]), with an OR of 1.90 (95% CI 1.53–2.36; I2 = 39.4%, P = 0.1429).
Prevalence of Depression in Patients With T2DM According to Current Smoking Status
The pooled prevalence of depression in patients with T2DM with current smoking status was 24.4% (95% CI 16.4%−34.8%; I2 = 91.4%, P < 0.0001) and in non-smokers 25.8% (95% CI 16.7%−37.6%; I2 = 99.1%, P < 0.0001). There was no difference in prevalence of depression between current smoking T2DM and non-smoker (OR=0.85, 95% CI 0.60–1.20; I2 = 78.0%, P = 0.0001).
Prevalence of Depression in Patients With T2DM According to Current Alcohol Use
The pooled prevalence of depression in patients with T2DM with current alcohol use was 21.6% (95% CI 13.8%−30.4%; I2 = 86.2%, P < 0.0001), while prevalence of depression in non-drinkers was 23.5% (95% CI 14.9%−35.1%; I2 = 99.1%, P < 0.0001). The OR for T2DM with current alcohol use vs. non-drinkers was significantly lower (OR=0.70, 95% CI 0.58–0.86; I2 = 15.7%, P = 0.3129).
Prevalence of Depression in Patients With T2DM According to Marital Status
The pooled prevalence of depression in patients with T2DM who had abnormal marital status (separated, divorced, widowed) was 38.5% (95% CI 27.4%−49.6%; I2 = 91.4%, P < 0.0001); for normal marital status was 31.4% (95% CI 23.6%−39.1%; I2 = 97.2%, P < 0.0001). The OR in T2DM with abnormal marital status compared with normal marital status was 1.39 (95% CI 0.90–2.14; I2 = 83.5%, P < 0.0001).
Prevalence of Depression in Patients With T2DM According to Living Status
The pooled studies prevalence of depression in patients with T2DM who were living alone was higher compared to those not living alone (50.3% [95% CI 40.1%−60.5%; I2 = 62.1%, P = 0.0418] vs.29.4% [95% CI 19.7%−41.3%; I2 = 94.8%, P < 0.0001]). There was significant difference in prevalence of depression between patients with T2DM who were living alone and those not living alone (OR = 2.26, 95% CI 1.71–2.98; I2 = 0.0%, P = 0.7581).
Prevalence of Depression in Patients With T2DM According to Different Instruments Used to Detect Depression
The included studies used various instruments to detect depression; there were different cut-off points even for the same instrument. Table 4 presents the pooled prevalence of depression in patients with T2DM according to the various instruments and cut-off points.
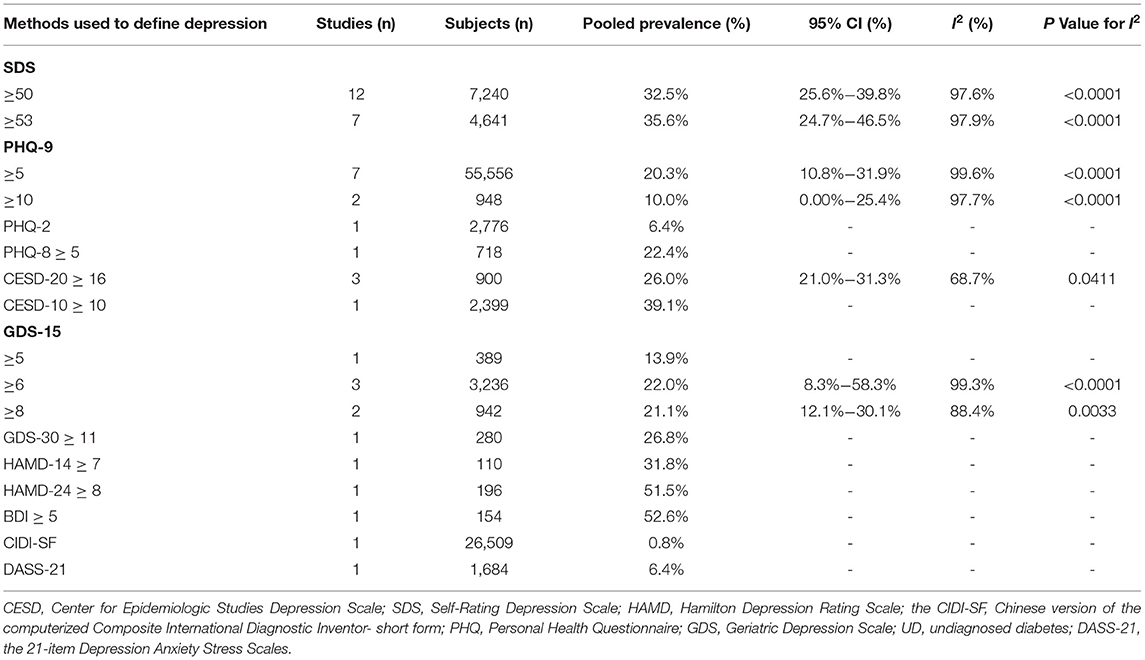
Table 4. Pooled prevalence of depression in patients with T2DM according to instruments used to evaluated depression.
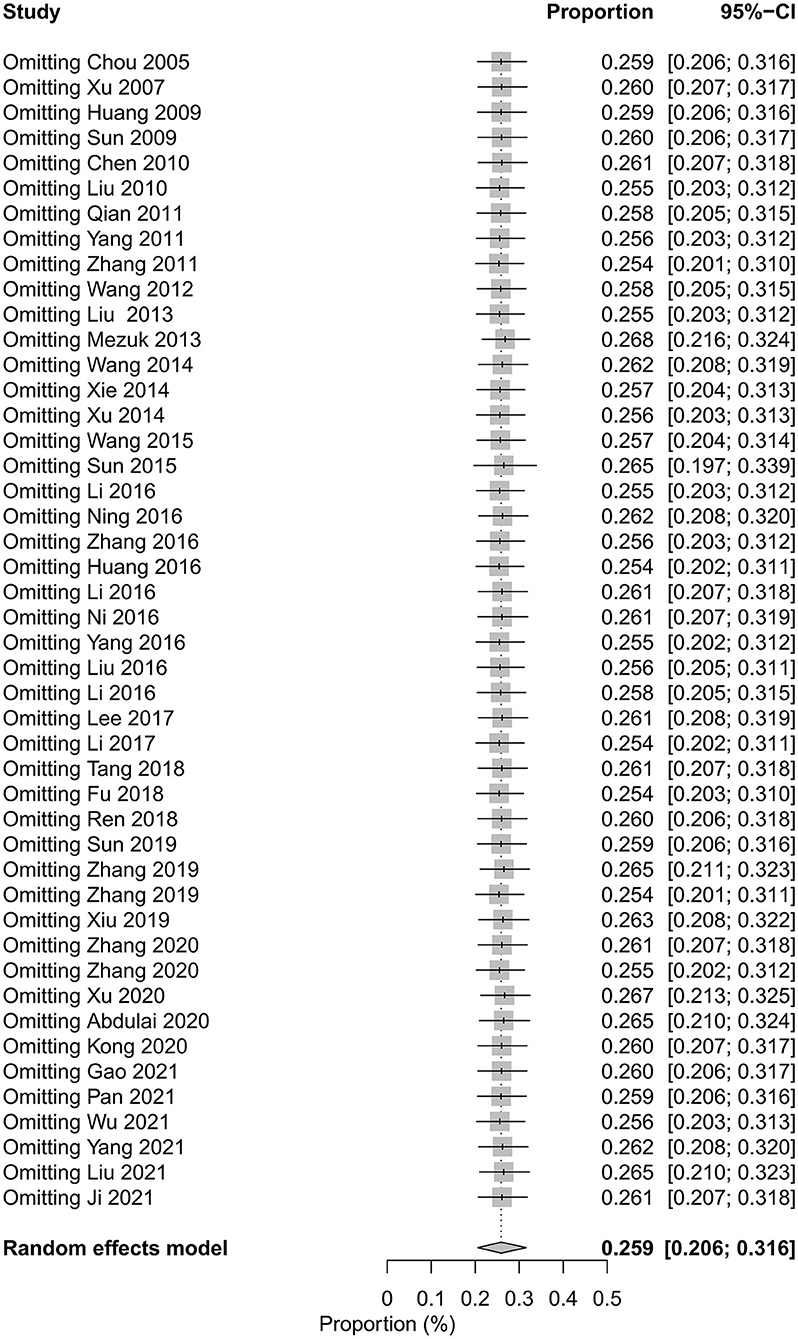
Sensitivity Analysis
The pooled prevalence of depression in patients with T2DM varied from 25.4%−26.8% after excluding studies one by one (Figure 4). We applied the trim and fill method, after filling 2 estimated missing studies, the funnel plot was symmetrical around the adjusted effect size (Figure 5). The adjusted results showed that the prevalence of depression in T2DM patients was 26.2% (95% CI 21.9%−30.5%).
We categorized the prevalence of studies with low, moderate, and high risk of bias, respectively, and the results showed that the prevalence of depression in patients with T2DM was 6.9% (95% CI 2.3%−13.6%; I2 = 99.9%, P < 0.0001), 27.0% (95% CI 22.5%−31.8%; I2 = 98.7%, P < 0.0001), and 40.4% (95% CI 23.9%−56.9%; I2 = 97.6%, P < 0.0001).
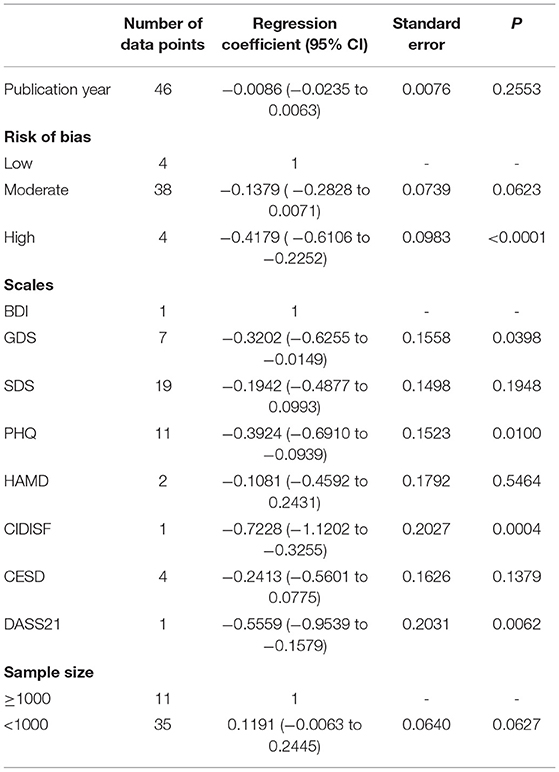
Meta-Regression Analysis
The results of univariate meta-regression showed the risk of bias of included studies and instruments used to define depression were the source of heterogeneity (Table 5).
Discussion
This SR and meta-analysis synthesized data from 48 population-based cross-sectional surveys that reported the prevalence of depression in T2DM patients in China. The results showed that 25.9% of T2DM patients in China suffered from different degrees of depression. Prevalence varied strikingly, from 7.3% to 50.3%, according to the demographic features in the study. A higher prevalence of depression existed in patients with T2DM who were women, aged ≥60 years, with primary school or lower education level and duration of diabetes ≥10 years, using insulin, with complications, living alone and living in rural areas. The prevalence of depression in undiagnosed T2DM was distinctly low. Alcohol users with T2DM had a lower prevalence of depression; other demographic features, like current smoking status and abnormal marriage, were unrelated to depression in patients with T2DM.
A global statistic calculated by Khaledi et al. (17) pooled 248 studies up to 2018. They reported that the global prevalence of depression in patients with T2DM was 28%. In their report, they included patients identified with depression through self-report or validated instruments. Another meta-analysis (18) showed that 14.5% patients with T2DM globally were diagnosed as major depressive disorder based on operationalized criteria, such as the DSM and ICD-10. Wang et al. (25) included 26 studies published up to 2016, 66,475 subjects, and reported that 28.9% of T2DM patients in China suffered from depression. In our study, we included 48 sudies with 108,678 T2DM subjects. The prevalence of depression in patients with T2DM was 25.9% in China. For the reason of such high prevalence of depression in T2DM, the researchers inferred that the link between depression and diabetes was associated with Gene-Environment interaction. The patients may share biological pathways contributing to pathogenesis of depression and T2DM, such as dysregulation of hypothalamic–pituitary–adrenal axis, overactivation of innate immunity, and inflammatory response (10, 77, 78).
Our study showed that the prevalence of depression in patients with undiagnosed T2DM (7.3%) was notably lower than diagnosed T2DM (27.1%), which was consistent with previous studies. A meta-analysis (79) found, compared with individuals without diabetes, undiagnosed diabetes have a slight risk of depression (OR = 1.27), while diagnosed diabetes have a higher risk of depression (OR = 1.80). Another study showed that the risk of depression does not differ between individuals with undiagnosed diabetes and individuals with normal glucose metabolism (80). The evidence mentioned above suggested awareness of diabetes may induce depression in patients with T2DM; therefore, early psychosomatic management is necessary.
We found that women with T2DM had a higher prevalence of depression than men. Many epidemiological studies pointed out the gender gap in the prevalence of depression—women are about twice as likely to suffer from depression than men during their lifetime (81, 82), which may be contributed to environmental, hormonal, genetic factors. In addition, among patients with T2DM, depressive symptoms are related to higher HbA1c levels (83), and the depressive symptoms was positively associated with HbA1c levels in female patients with T2DM (84). The above factors might lead to the gender difference in the prevalence of depression in T2DM patients observed in our and some other relevant meta-analyses (17, 19, 20, 25).
Few meta-analyses focus on the influence of educational characteristics on depression in patients with T2DM. Several large observational studies discovered the same trend with our study (85, 86) that a low educational level was a risk factor for depression in T2DM patients. A low educational level may lead to a low socioeconomic status (87), such as insufficient social support and medical resources, and poor perception of health, which may further lead to poor blood glucose control and a high risk of depression in patients with T2DM.
We found the risk of depression in elderly patients ≥60 years was 1.56 times higher than those <60 years. However, Khaledi et al. (17) reported that depression was more common in T2DM patients under 65 years than in the elderly. Their study pooled global data from cross-sectional, case-control, and cohort studies that reported the current or lifetime prevalence of depression. In our study, we included cross-sectional studies and reported the current prevalence of depression. The epidemiological data of China showed that the middle-aged and elderly patients were the mainstream population with T2DM, and the prevalence of T2DM increased rapidly with age (65-74 years old, 14.1%; 55–64 years old, 11.0%; over 75 years old, 11.0%) (5, 88). Therefore, the majority of patients with T2DM included in our studies were around 60 years old, though our inclusion criterion was population with T2DM aged over 18 years. We presumed that, with the decline of health level and prolonged duration of T2DM, elderly patients with T2DM are more likely to suffer from multiple diseases and diabetes complications, which may contribute to a high risk of depression.
Our studies found that patients with a duration of T2DM more than 10 years had a higher prevalence of depression. Wang et al. (25) reported that a one-year increment in diabetes duration led to a 1.1-fold increase in the risk of depression. Previous studies found long duration of diabetes was associated with a high risk of microvascular diseases (89, 90), such as nephropathy, retinopathy, neuropathy, and macrovascular complications (91). Meanwhile, the duration of T2DM varies inversely with quality of life, especially in patients with diabetes duration of more than 10 years (13).
Complications cause a greater medical burden and worse health for T2DM patients. Together with Wang et al. (25) (RR = 2·08), and Hussain et al. (19) (OR = 2.33), we (OR = 1.90) found that diabetes complications increased almost two-fold risk of depression. Rees et al. (92) reported that severe non-proliferative or proliferative diabetic retinopathy was independently associated with depressive symptoms. Due to inadequate raw data, we failed to investigate the association between types and numbers of complications and depression. More studies are needed to explore the relationship between diabetes complications and depression.
Our results showed that T2DM using insulin had higher risk of depression than non-insulin user. Consistent with our result, a previous meta-analysis (93) confirmed that insulin therapy increased the risk of depression in T2DM patients comparing with non-insulin users or oral antidiabetic drug users. Insulin is usually prescribed to treat diabetic patients with poor glycemic control, especially those with advanced diabetes (94). Besides, T2DM patients with insulin therapy commonly suffered from negative physical side effects, including hypoglycaemia, weight gain and pain. Some patients even experienced psychological barriers associated with insulin injections, such as they felt that insulin injections made their life less flexible and symbolized a worsening condition, and they concerned about other people's negative reactions (95). In other words, due to insufficient physical and psychological adjustment, T2DM patients using insulin are more likely to suffer from depression (96).
Regarding lifestyle, we found several notable factors that affected depressive symptoms in T2DM patients. We observed that T2DM patients living alone had a more than two-fold higher risk for depression. Researchers concluded that living alone was supposed to be an independent risk factor for depression (97–99). Subjects living alone were more likely to experience insomnia (100), have low social support, and social isolation. Besides, due to the one-child policy during 1980–2016, and the rapidly aging population in China, living alone in the elderly, also called empty-nest, became prevalent (101). Besides, we found that alcohol users had a significantly lower prevalence of depression among T2DM patients. Previous studies have shown that moderate alcohol consumption brought better mental health conditions and lower levels of depression (102, 103). A recent pooled analysis also suggested that (104) low-to-moderate alcohol intake was associated with a significantly reduced risk of long-term depressive symptoms. However, due to limited data in our studies and difference in patients' health conditions, we should be cautious about this finding. Future studies are needed to investigate the relationship between moderate alcohol consumption and the mental condition of T2DM patients.
The results of sensitivity analysis and meta-regression in our study showed that the risk of bias might be the source of heterogeneity, and studies with low risk of bias were associated with lower prevalence. We noticed that most of included studies were rated as high risk of bias on items involving explanation of patient exclusions, assessments undertaken for quality assurance purposes, handling of missing data, and assessment and control of confounding. Thus, researchers should pay attention to these issues to reduce the risk of bias of cross-sectional studies. In addition, results of subgroup analysis suggested that the prevalence were varied according to different instruments used to detect depression, and sensitivity analysis showed that instruments were the source of heterogeneity. Researchers found that most of depression screening instruments showed moderate–good sensitivity and specificity in detecting depression in patients with T2DM, but often produced high false positive rate (105). The symptoms of T2DM and its long-term complications including tiredness, lethargy, lack of energy, sleeping difficulties and appetite changes, may overlap with symptoms in depression. Therefore, the specific depression screening tools for patients with T2DM should be developed, which may provide more accurate prevalence of depression in patients with T2DM.
Limitations
There are some limitations existed in the present study. Firstly, various identification instruments of depression were used in cross-sectional studies, and the results of subgroup analysis showed that the prevalence were varied from different instruments, which may have impact on the pooled prevalence. Second, we calculated ORs using raw data from the studies rather than adjusting for potential underlying differences among study participants, the residual confounding was inevitable. Third, we found significant heterogeneity existed, to explore the source of heterogeneity, we conducted the meta-regression, and the results showed that different instruments used to detect depression and the risk of bias were the source of heterogeneity. Fourth, since we included the cross-sectional studies, and extracted the characteristics at study level to explored the potential risk factors, the ecological fallacy may exist.
Conclusion
In conclusion, this SR and meta-analysis suggested a pooled prevalence of depression in patients with T2DM in China was 25.9%. Potential risk factors of depression in patients with T2DM might include female gender, age ≥60 years, low educational level, complications, diabetes duration ≥10 years, insulin use, and living alone. High-quality epidemiological surveys of the prevalence of depression in T2DM in China are needed to better understand the status of depression for T2DM.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
Author Contributions
XL, YL, and LG wrote the manuscript. RJ, JL, and DZ conceptualized the study and provide methodological support. YL and LG designed the search strategy and performed searches. HZ, JZ, XL, and XH selected studies. XL and XH extracted the data. YL and DZ assessed the risk of bias of included studies. All authors contributed to the article and approved the submitted version.
Funding
This work was supported by the National Natural Science Foundation of China (Number: 81873356), National Key R&D Program of China (Number: 2019YFC1710302), and Sichuan Province Science and Technology Support Program in Sichuan (Number: 2014SZ0154).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
The authors acknowledge the editorial suggestions of Smart Study Education and Technology Group.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2022.759499/full#supplementary-material
Supplementary File 1. PRISMA and MOOSE checklist.
Supplementary File 2. Search strategy of all databases.
Supplementary File 3. List of excluded records by screening full text.
Supplementary File 4. Risk of bias assessment results of included studies.
Supplementary File 5. Forest plot and funnel plot of subgroup analysis.
References
1. The International Diabetes Federation. Type 2 Diabetes. (2020). Available online at: https://www.idf.org/aboutdiabetes/type-2-diabetes.html (accessed March, 2022).
2. World Health Organization. Classification of Diabetes Mellitus. (2019). Available online at: https://www.who.int/publications/i/item/classification-of-diabetes-mellitus (accessed March, 2022).
3. The International Diabetes Federation. Idf Diabetes Atlas 2019. (2019). Available online at: https://diabetesatlas.org/en/resources/ (accessed March, 2022).
4. Ma RCW. Epidemiology of diabetes and diabetic complications in China. Diabetologia. (2018) 61:1249–60. doi: 10.1007/s00125-018-4557-7
5. Yang L, Shao J, Bian Y, Wu H, Shi L, Zeng L, et al. Prevalence of type 2 diabetes mellitus among inland residents in China (2000-2014): a meta-analysis. J Diabetes Invest. (2016) 7:845–52. doi: 10.1111/jdi.12514
6. World Health Organization. Depression. (2022). Available online at: https://www.who.int/health-topics/depression#tab=tab_1 (accessed March, 2022).
7. Semenkovich K, Brown ME, Svrakic DM, Lustman PJ. Depression in type 2 diabetes mellitus: prevalence, impact, and treatment. Drugs. (2015) 75:577–87. doi: 10.1007/s40265-015-0347-4
8. Mezuk B, Eaton WW, Albrecht S, Golden SH. Depression and type 2 diabetes over the lifespan: a meta-analysis. Diabetes Care. (2008) 31:2383–90. doi: 10.2337/dc08-0985
9. Yu M, Zhang X, Lu F, Fang L. Depression and risk for diabetes: a meta-analysis. Can J Diabetes. (2015) 39:266–72. doi: 10.1016/j.jcjd.2014.11.006
10. Moulton CD, Pickup JC, Ismail K. The link between depression and diabetes: the search for shared mechanisms. Lancet Diabetes endocrinol. (2015) 3:461–71. doi: 10.1016/S2213-8587(15)00134-5
11. Nouwen A, Winkley K, Twisk J, Lloyd CE, Peyrot M, Ismail K, et al. Type 2 diabetes mellitus as a risk factor for the onset of depression: a systematic review and meta-analysis. Diabetologia. (2010) 53:2480–6. doi: 10.1007/s00125-010-1874-x
12. Gonzalez JS, Peyrot M, McCarl LA, Collins EM, Serpa L, Mimiaga MJ, et al. Depression and diabetes treatment nonadherence: a meta-analysis. Diabetes Care. (2008) 31:2398–403. doi: 10.2337/dc08-1341
13. Jing X, Chen J, Dong Y, Han D, Zhao H, Wang X, et al. Related factors of quality of life of type 2 diabetes patients: a systematic review and meta-analysis. Health Qual Life Outcomes. (2018) 16:189. doi: 10.1186/s12955-018-1021-9
14. Katon W, Pedersen HS, Ribe AR, Fenger-Grøn M, Davydow D, Waldorff FB, et al. Effect of depression and diabetes mellitus on the risk for dementia: a national population-based cohort study. JAMA psychiatry. (2015) 72:612–9. doi: 10.1001/jamapsychiatry.2015.0082
15. Farooqi A, Khunti K, Abner S, Gillies C, Morriss R, Seidu S. Comorbid depression and risk of cardiac events and cardiac mortality in people with diabetes: a systematic review and meta-analysis. Diabetes Res Clin Pract. (2019) 156:107816. doi: 10.1016/j.diabres.2019.107816
16. Hazuda HP, Gaussoin SA, Wing RR, Yanovski SZ, Johnson KC, Coday M, et al. Long-Term association of depression symptoms and antidepressant medication use with incident cardiovascular events in the look ahead (action for health in diabetes) clinical trial of weight loss in type 2 diabetes. Diabetes Care. (2019) 42:910–8. doi: 10.2337/dc18-0575
17. Khaledi M, Haghighatdoost F, Feizi A, Aminorroaya A. The Prevalence of comorbid depression in patients with type 2 diabetes: an updated systematic review and meta-analysis on huge number of observational studies. Acta Diabetol. (2019) 56:631–50. doi: 10.1007/s00592-019-01295-9
18. Wang F, Wang S, Zong QQ, Zhang Q, Ng CH, Ungvari GS, et al. Prevalence of comorbid major depressive disorder in type 2 diabetes: a meta-analysis of comparative and epidemiological studies. Diabet Med. (2019) 36:961–9. doi: 10.1111/dme.14042
19. Hussain S, Habib A, Singh A, Akhtar M, Najmi AK. Prevalence of depression among type 2 diabetes mellitus patients in India: a meta-Aanalysis. Psychiatry Res. (2018) 270:264–73. doi: 10.1016/j.psychres.2018.09.037
20. Pashaki MS, Mezel JA, Mokhtari Z, Gheshlagh RG, Hesabi PS, Nematifard T, et al. The prevalence of comorbid depression in patients with diabetes: a meta-analysis of observational studies. Diabetes Metab Syndr. (2019) 13:3113–9. doi: 10.1016/j.dsx.2019.11.003
21. Roy T, Lloyd CE, Parvin M, Mohiuddin KG, Rahman M. Prevalence of co-morbid depression in out-patients with type 2 diabetes mellitus in Bangladesh. BMC Psychiatry. (2012) 12:123. doi: 10.1186/1471-244X-12-123
22. Sun N, Lou P, Shang Y, Zhang P, Wang J, Chang G, et al. Prevalence and determinants of depressive and anxiety symptoms in adults with type 2 diabetes in China: a cross-sectional study. BMJ Open. (2016) 6:e012540. doi: 10.1136/bmjopen-2016-012540
23. Liu H, Xu X, Hall JJ, Wu X, Zhang M. Differences in depression between unknown diabetes and known diabetes: results from China health and retirement longitudinal study. Int Psychogeriatr. (2016) 28:1191–9. doi: 10.1017/S104161021600020X
24. Li Z, Guo X, Jiang H, Sun G, Sun Y, Abraham MR. Diagnosed but not undiagnosed diabetes is associated with depression in rural areas. Int J Environ Res Public Health. (2016) 13:1136. doi: 10.3390/ijerph13111136
25. Wang B, Yuan J, Yao Q, Li L, Yan N, Song R, et al. Prevalence and independent risk factors of depression in Chinese patients with type 2 diabetes: a systematic review and meta-analysis. Lancet Diabetes Endocrinol. (2016) 4:S36. doi: 10.1016/S2213-8587(16)30391-6
26. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The prisma 2020 statement: an updated guideline for reporting systematic reviews. Bmj. (2021) 372:n71. doi: 10.1136/bmj.n71
27. Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D, et al. Meta-Analysis of observational studies in epidemiology: a proposal for reporting. meta-analysis of observational studies in epidemiology (Moose) group. Jama. (2000) 283:2008–12. doi: 10.1001/jama.283.15.2008
28. Liu X, Dong C, Jiang H, Zhong D, Li Y, Zhang H, et al. Prevalence and risk factors of depression in Chinese patients with type 2 diabetes mellitus: a protocol of systematic review and meta-analysis. Syst Rev. (2021) 10:302. doi: 10.1186/s13643-021-01855-7
29. World Health Organization. Hearts D: Diagnosis and Management of Type 2 Diabetes. (2020). Available online at: https://www.who.int/publications/i/item/who-ucn-ncd-20.1 (accessed March, 2022).
30. Rostom A, Dubé C, Cranney A, et al. Agency for Healthcare Research and Quality (Us). (2014). Available online at: https://www.ncbi.nlm.nih.gov/books/NBK35156/ (accessed March 01, 2022).
31. Higgins J, Green S, , editors. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0: The Cochrane Collaboration. (2011). Available online at: www.handbook.cochrane.org (accessed March 2011).
32. Chou KL, Chi I. Prevalence of depression among elderly chinese with diabetes. Int J Geriatr Psychiatry. (2005) 20:570–5. doi: 10.1002/gps.1328
33. Xu N. Risk Factors for Depression in Patients with Type 2 Diabetes Mellitus. Master Dissertation, TianJin Medical University (2007).
34. Huang H, Li H, Zhao H. Wang M. Investigation of depression disorders and its influencing factors among senile patients with type 2 diabetes mellitus in rural-urban fringe. Chinese J Pract Nurs. (2009) 25:62–5. doi: 10.3760/cma.j.issn.1672-7088.2009.04.030
35. Sun S, Dong X. Investigation and analysis of the prevalence of depression in T2dm patients. Med Philosophy. (2009) 30:75–6.
36. Chen C, Dong Y, Guo Y. The prevalence and its related factors of depression in patients with igr and newly diagnosed T2dm. Chinese J Diabetes. (2010) 18:384–6. doi: 10.3969/j.issn.1006-6187.2010.05.022
37. Liu Y, He G, Qin Y, Hou R. Influencing factors to quality of life in patients with type2 diabetes mellitus complicated by depression. Chinese General Pract. (2010) 13:2829–33. doi: 10.3969/j.issn.1007-9572.2010.25.018
38. Qian X, Wang H, Wei X. Epidemiological survey on risk factors of depression and anxiety in type 2 diabetes patients in community. Chinese J Modern Drug Application. (2011) 5:132–4. doi: 10.14164/j.cnki.cn11-5581/r.2011.22.005
39. Yang C, Cai W, Huang H, Jin Y. Risk factors of comorbid depression and diabetes mellitus. Chinese General Pract. (2011) 14:2956–8. doi: 10.3969/j.issn.1007-9572.2011.26.003
40. Zhang J. Prevalence of depression and its risk factors in elderly patients with type 2 diabetes mellitus. World Health Digest. (2011) 08:91–2. doi: 10.3969/j.issn.1672-5085.2011.09.075
41. Wang G, A Large-Scale survey for risk factors of type 2 diabetes with mental illness. J Chengdu Med Coll. (2012) 07:118–20. doi: 10.3969/j.issn.1674-2257.2012.01.039
42. Liu Y, Maier M, Wu J, Li W, Chen Y, Qin Y, et al. A descriptive and comparative study from China on patients with type-2 diabetes with and without depressive symptoms. J Community Health Nurs. (2013) 30:106–15. doi: 10.1080/07370016.2013.778734
43. Mezuk B, Chen Y, Yu C, Guo Y, Bian Z, Collins R, et al. Depression, anxiety, and prevalent diabetes in the Chinese population: findings from the China Kadoorie biobank of 05 million people. J Psychosom Res. (2013) 75:511–7. doi: 10.1016/j.jpsychores.2013.09.008
44. Wang C, Jin J, Chao X, Tian H, Zhou F, Zhang Q. Analysis on influencing factors of depression in community patients with diabetes in Suzhou city. Occupation Health. (2014) 30:681–3. doi: 10.13329/j.cnki.zyyjk.2014.05.039
45. Xie K. Analysis on the current situation in type 2 diabetes accompanying with depression and influence factors in Hefei City, Master Dissertation, Anhui Medical University (2014).
46. Xu W, Liu W, Zeng H. Study on psychological status and intervention strategy of rural patients with type 2 diabetes. Chinese Manipulation Rehabilitation Med. (2014) 5:224–6.
47. Zheng Y, Sun Q, Chen K, Yan W, Pan C, Lu J, et al. Waist-to-Hip Ratio, dyslipidemia, glycemic levels, blood pressure and depressive symptoms among diabetic and non-diabetic Chinese women: a cross-sectional study. PLoS ONE. (2014) 9:e109765. doi: 10.1371/journal.pone.0109765
48. Wang L, Song R, Chen Z, Wang J, Ling F. Prevalence of depressive symptoms and factors associated with it in type 2 diabetic patients: a cross-sectional study in China. BMC Public Health. (2015) 15:188. doi: 10.1186/s12889-015-1567-y
49. Sun JC, Xu M, Lu JL Bi YF, Mu YM, Zhao JJ, et al. Associations of depression with impaired glucose regulation, newly diagnosed diabetes and previously diagnosed diabetes in Chinese adults. Diabet Med. (2015) 32:935–43. doi: 10.1111/dme.12649
50. Li Y, Jia R, Li X. Community based cross-sectional survey on patients with type 2 diabetes complicated with depression. Chinese Health Service Management. (2016) 33:94–6.
51. Ning F, Wang Y, Sun X, Zhang D, Xin H, Nan H, et al. Bi-Direction association on the increased prevalence of depression and type 2 diabetes among adults in Qingdao. Chinese J Dis Control Prevention. (2016) 20:357–61. doi: 10.16462/j.cnki.zhjbkz.2016.04.009
52. Zhang P, Tang S, Lou P, Lou H, Zhao J, Chen P, et al. Correlation of sleep quality and depression symptom in patients with type 2 diabetes mellitus in communities. Chinese J Psychiatry. (2016) 49:107–12. doi: 10.1186/s12875-016-0435-x
53. Huang J, Hu J, Zhu X, Zhang Y, Wang L, Lai B, et al. Status and influencing factors for the cognitive function of patients with type 2 diabetes mellitus. Chinese General Pract. (2016) 19:135–41. doi: 10.3969/j.issn.1007-9572.2016.02.003
54. Li C, Zhang H, Gao W, Chen S, Li J. Study on the depression and related factors of elderly patients with hypertension complicated with type 2 diabetes mellitus in a community of Shanghai. J Neuroscience and Ment Health. (2016) 16:540–3. doi: 10.3969/j.issn.1009-6574.2016.05.013
55. Ni J, Liu W. Analysis of the life ouality of patients with diabetes registered in the community and the influence factors. Shanghai Medical & Pharmaceutical Journal. (2016) 37:34–6.
56. Yang J, Feng J, Luo J, Lv J, Sha L. Investigation and analysis of depression in patients with type 2 diabetes mellitus in community of Zhuzhou city. Nurs Pract Res. (2016) 13:109–10. doi: 10.3969/j.issn.1672-9676.2016.22.043
57. Lee CM, Chang CF, Pan MY, Hsu TH, Chen MY. Depression and its associated factors among rural diabetic residents. J Nurs Res. (2017) 25:31–40. doi: 10.1097/jnr.0000000000000143
58. Li L, Yang J, Yang Y, Zhang Y. A survey and analysis on depression of patients with hypertension or type 2 diabetes mellitus in rural community. Ningxia Med J. (2017) 39:430–3. doi: 10.13621/j.1001-5949.2017.05.0430
59. Tang J, Yang Q, Li X, Wu W, Li Q, Niu D, et al. Assessment of mood and family function in elderly patients with type 2 diabetes mellitus in community. J Front Med. (2018) 8:381–2. doi: 10.3969/j.issn.2095-1752.2018.23.329
60. Fu W, He X, Cao R, Wang W, Liu Q. Study on emotion, coping and locus of control in patients with type 2 diabetes mellitus. Modern Preventive Med. (2018) 45:1149–52.
61. Ren L. Epidemiological Analysis of depression in patients with type 2 diabetes mellitus in Zhengzhou, doctoral thesis, ZhengZhou University (2018).
62. Sun Y, Jia J, Zhang H, Deng H. Correlation between depression and quality of life in elderly type 2 diabetic patients. Med Information(XiAn). (2019) 32:93–5. doi: 10.3969/j.issn.1006-1959.2019.12.028
63. Zhang Y, Lin Y, Zhang J, Li L, Liu X, Wang T, et al. Association between insomnia and type 2 diabetes mellitus in Han chinese individuals in shandong province, China. Sleep Breath. (2019) 23:349–54. doi: 10.1007/s11325-018-1687-6
64. Zhang S, Zhang H. Relationship between depression and anxiety and quality of life in elderly patients with type 2 diabetes. Chinese J Gerontology. (2019) 39:938–40. doi: 10.3969/j.issn.1005-9202.2019.04.056
65. Xiu S, Zheng Z, Liao Q, Chan P. Different risk factors for cognitive impairment among community-dwelling elderly, with impaired fasting glucose or diabetes. Diabetes Metab Syndr Obes. (2019) 12:121–30. doi: 10.2147/DMSO.S180781
66. Zhang M, Zhao C, Fu Y. Stress response and influencing factors among community patients with type 2 diabetes mellitus. Chinese J General Practitioners. (2020) 19:537–40. doi: 10.3760/cma.j.cn114798-20200119-00065
67. Zhang X, Zhang X, Liang X, Cheng Y, Lin Q, Liu L, et al. Study on the correlation between stigma and depressive symptoms in community elderly patients with type 2 diabetes in Chengdu. Medicine and Society. (2020) 33:95–8. doi: 10.13723/j.yxysh.2020.06.023.
68. Xu J, Bian Z, Zhang Y, Pan J, Gao F, Wang C, et al. Depressive symptoms in chinese adults with risk factors for diabetes: the shanghai high-risk diabetic screen (Shids) Study. Diabet Med. (2020) 38:e14375. doi: 10.1111/dme.14375
69. Abdulai T, Runqi T, Lou Z, Amponsem-Boateng C, Zhang H, Liu X, et al. Depressive symptoms are not associated with type 2 diabetes in a rural population in China: findings from the henan rural cohort: diabetes and depression. J Affect Disord. (2020) 274:841–7. doi: 10.1016/j.jad.2020.05.018
70. Kong LL, Zhao HM, Liu YT, Fan JY, Wang Q, Li J, et al. Cognitive frailty and its influencing factors among the elderly with type 2 diabetes in community. J Nurs Science. (2020) 35:89–92. doi: 10.3870/j.issn.1001-4152.2020.07.089
71. Gao M, Chen XY, Sun X, Fan LS, Wang FB, Shen Y, et al. Relation of Depressive Symptoms to Personality Traits and Exercise Behavior in Patients with Type 2 Diabetes. Chinese Mental Health Journal. (2021) 35:271–6. doi: 10.3969/j.issn.1000-6729.2021.04.002.
72. Pan XQ, Wan YN, Lv SR, Hong X, Zhen CZ, Wang HY, et al. Analysis of life quality, depressive status among patients with type 2 diabetes mellitus in the community disease management of Jiangsu province. Chinese J Prevention Control Chronic Dis. (2021) 29:665–8. doi: 10.16386/j.cjpccd.issn.1004-6194.2021.09.006.
73. Wu JS, Yu SM, Li RP. Prevalence of depression in patients with type 2 diabetes mellitus in community of Guangzhou and its risk factors. Heilongjiang Med J. (2021) 34:20–2. doi: 10.14035/j.cnki.hljyy.2021.01.007
74. Yang L, Wu DM. Relationships between grip strength, monthly household income level, and depression in community-dwelling elderly female patients with type 2 diabetes. West China Med J. (2021) 36:877–81. doi: 10.7507/1002-0179.202106212.
75. Liu X, Cao H, Zhu H, Zhang H, Niu K, Tang N, et al. Association of chronic diseases with depression, anxiety and stress in chinese general population: the Chcn-Bth cohort study. J Affect Disord. (2021) 282:1278–87. doi: 10.1016/j.jad.2021.01.040
76. Ji L, Zhang Y, Zhang Q, Zheng H, Sun W, Zhu X, et al. Self-Reported Depressive Symptoms Might Be Associated with Sudomotor Dysfunction in Chinese T2dm Patients. Experimental and Clinical Endocrinology and Diabetes. (2021) 129:689–94. doi: 10.1055/a-1025-3724
77. Gragnoli C. Hypothesis of the neuroendocrine cortisol pathway gene role in the comorbidity of depression, type 2 diabetes, and metabolic syndrome. Appl Clin Genet. (2014) 7:43–53. doi: 10.2147/TACG.S39993
78. Tabák AG, Akbaraly TN, Batty GD, Kivimäki M. Depression and type 2 diabetes: a causal sssociation? lancet Diabetes endocrinol. (2014) 2:236–45. doi: 10.1016/S2213-8587(13)70139-6
79. Chen S, Zhang Q, Dai G, Hu J, Zhu C, Su L, et al. Association of depression with pre-diabetes, undiagnosed diabetes, and previously diagnosed diabetes: a meta-analysis. Endocrine. (2016) 53:35–46. doi: 10.1007/s12020-016-0869-x
80. Nouwen A, Nefs G, Caramlau I, Connock M, Winkley K, Lloyd CE, et al. Prevalence of depression in individuals with impaired glucose metabolism or undiagnosed diabetes: a systematic review and meta-analysis of the European depression in diabetes (Edid) research consortium. Diabetes Care. (2011) 34:752–62. doi: 10.2337/dc10-1414
81. Kuehner C. Gender differences in unipolar depression: an update of epidemiological findings and possible explanations. Acta Psychiatr Scand. (2003) 108:163–74. doi: 10.1034/j.1600-0447.2003.00204.x
82. Kuehner C. Why Is Depression More Common among Women Than among Men? Lancet Psychiatry. (2017) 4:146–58. doi: 10.1016/S2215-0366(16)30263-2
83. Bot M, Pouwer F, de Jonge P, Tack CJ, Geelhoed-Duijvestijn PH, Snoek FJ. Differential associations between depressive symptoms and glycaemic control in outpatients with diabetes. Diabet Med. (2013) 30:e115–22. doi: 10.1111/dme.12082
84. Pouwer F, Snoek FJ. Association between symptoms of depression and glycaemic control may be unstable across gender. Diabet Med. (2001) 18:595–8. doi: 10.1046/j.1464-5491.2001.00499.x
85. Lloyd CE, Nouwen A, Sartorius N, Ahmed HU, Alvarez A, Bahendeka S, et al. Prevalence and correlates of depressive disorders in people with type 2 diabetes: results from the international prevalence and treatment of diabetes and depression (Interpret-Dd) study, a collaborative study carried out in 14 countries. Diabet Med. (2018) 35:760–9. doi: 10.1111/dme.13611
86. Nefs G, Pouwer F, Denollet J, Pop V. The course of depressive symptoms in primary care patients with type 2 diabetes: results from the diabetes, depression, type D personality Zuidoost-Brabant (Diaddzob) Study. Diabetologia. (2012) 55:608–16. doi: 10.1007/s00125-011-2411-2
87. Chan J, Nan H, Ting R. “Depression and diabetes: sociodemographic and cultural aspects and public health implications,” In: Katon W, Maj M, Sartorius N, editor. Depression and Diabetes. Hoboken, NJ: John Wiley & Sons (2010). p. 143–171.
88. Wang L, Gao P, Zhang M, Huang Z, Zhang D, Deng Q, et al. Prevalence and ethnic pattern of diabetes and prediabetes in China in 2013. Jama. (2017) 317:2515–23. doi: 10.1001/jama.2017.7596
89. Teliti M, Cogni G, Sacchi L, Dagliati A, Marini S, Tibollo V, et al. Risk factors for the development of micro-vascular complications of type 2 diabetes in a single-centre cohort of patients. Diab Vasc Dis Res. (2018) 15:424–32. doi: 10.1177/1479164118780808
90. Pan Q, Li Q, Deng W, Zhao D, Qi L, Huang W, et al. Prevalence of and risk factors for peripheral neuropathy in Chinese patients with diabetes: a multicenter cross-sectional study. Front Endocrinol (Lausanne). (2018) 9:617. doi: 10.3389/fendo.2018.00617
91. Reis JP, Allen NB, Bancks MP, Carr JJ, Lewis CE, Lima JA, et al. Duration of diabetes and prediabetes during adulthood and subclinical atherosclerosis and cardiac dysfunction in middle age: the cardia study. Diabetes Care. (2018) 41:731–8. doi: 10.2337/dc17-2233
92. Rees G, Xie J, Fenwick EK, Sturrock BA, Finger R, Rogers SL, et al. Association between diabetes-related eye complications and symptoms of anxiety and depression. JAMA Ophthalmol. (2016) 134:1007–14. doi: 10.1001/jamaophthalmol.2016.2213
93. Bai X, Liu Z, Li Z, Yan D. The association between insulin therapy and depression in patients with type 2 diabetes mellitus: a meta-analysis. BMJ Open. (2018) 8:e020062. doi: 10.1136/bmjopen-2017-020062
94. Sorli C, Heile MK. Identifying and Meeting the challenges of insulin therapy in type 2 diabetes. J Multidiscip Healthc. (2014) 7:267–82. doi: 10.2147/JMDH.S64084
95. Holmes-Truscott E, Browne JL, Speight J. The impact of insulin therapy and attitudes towards insulin intensification among adults with type 2 diabetes: a qualitative study. J Diabetes Complications. (2016) 30:1151–7. doi: 10.1016/j.jdiacomp.2016.03.027
96. Holmes-Truscott E, Skinner TC, Pouwer F, Speight J. Negative appraisals of insulin therapy are common among adults with type 2 diabetes using insulin: results from diabetes miles - Australia cross-sectional survey. Diabet Med. (2015) 32:1297–303. doi: 10.1111/dme.12729
97. Huang G, Duan Y, Guo F, Chen G. Prevalence and related influencing factors of depression symptoms among empty-nest older adults in China. Arch Gerontol Geriatr. (2020) 91:104183. doi: 10.1016/j.archger.2020.104183
98. Chou KL, Ho AH, Chi I. Living alone and depression in Chinese older adults. Aging Ment Health. (2006) 10:583–91. doi: 10.1080/13607860600641150
99. Chen Y, Bennett D, Clarke R, Guo Y, Yu C, Bian Z. et al. Patterns and correlates of major depression in chinese adults: a cross-sectional study of 05 million men and women. Psychol Med. (2017) 47:958–70. doi: 10.1017/S0033291716002889
100. Chen Y, Kartsonaki C, Clarke R, Guo Y, Yu C, Bian Z. et al. Characteristics and correlates of sleep duration, daytime napping, snoring and insomnia symptoms among 05 million chinese men and women. Sleep Med. (2018) 44:67–75. doi: 10.1016/j.sleep.2017.11.1131
101. Zhai Y, Yi H, Shen W, Xiao Y, Fan H, He F, et al. Association of empty nest with depressive symptom in a Chinese elderly population: a cross-sectional study. J Affect Disord. (2015) 187:218–23. doi: 10.1016/j.jad.2015.08.031
102. Paschall MJ, Freisthler B, Lipton RI. Moderate alcohol use and depression in young adults: findings from a national longitudinal study. Am J Public Health. (2005) 95:453–7. doi: 10.2105/AJPH.2003.030700
103. Zhu C, Chen Q, Si W, Li Y, Chen G, Zhao Q. Alcohol use and depression: a mendelian randomization study from China. Front Genet. (2020) 11:585351. doi: 10.3389/fgene.2020.585351
104. Liang L, Hua R, Tang S, Li C, Xie W. Low-to-Moderate alcohol intake associated with lower risk of incidental depressive symptoms: a pooled analysis of three intercontinental cohort studies. J Affect Disord. (2021) 286:49–57. doi: 10.1016/j.jad.2021.02.050
Keywords: type 2 diabetes mellitus, depression, prevalence, risk factors, China
Citation: Liu X, Li Y, Guan L, He X, Zhang H, Zhang J, Li J, Zhong D and Jin R (2022) A Systematic Review and Meta-Analysis of the Prevalence and Risk Factors of Depression in Type 2 Diabetes Patients in China. Front. Med. 9:759499. doi: 10.3389/fmed.2022.759499
Received: 16 August 2021; Accepted: 21 March 2022;
Published: 10 May 2022.
Edited by:
Kevin Lu, University of South Carolina, United StatesReviewed by:
Eron Grant Manusov, The University of Texas Rio Grande Valley, United StatesOrvalho Augusto, University of Washington, United States
Copyright © 2022 Liu, Li, Guan, He, Zhang, Zhang, Li, Zhong and Jin. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Dongling Zhong, 417934055@qq.com; Juan Li, 785939016@qq.com; Rongjiang Jin, cdzyydxjrj@126.com
†These authors have contributed equally to this work and share first authorship
 Xiaobo Liu
Xiaobo Liu Yuxi Li
Yuxi Li Li Guan2†
Li Guan2†  Jun Zhang
Jun Zhang Juan Li
Juan Li Dongling Zhong
Dongling Zhong Rongjiang Jin
Rongjiang Jin