- Iverson Health Innovation Research Institute, Swinburne University of Technology, Hawthorn, VIC, Australia
Objectives: In current study, we aim to extend previous research by investigating the unique impact of loneliness on health literacy and health-related factors of young adults, after controlling for social isolation, depressive symptomology, and social anxiety, as well as evaluate how social isolation and loneliness differ in their impact on health literacy, and health-related factors among young adults, after accounting for abovementioned concomitant variables.
Methods: Using a cross-sectional study design, 521 young adults completed an online survey in 2020, where they self-reported their loneliness, social isolation, health-related factors, and health literacy data.
Results: Increased loneliness was associated with decrease in several health literacy domains (e.g., poorer social support for health, lower appraisal of health information, among others) and increase in some health-related factors (e.g., higher perceived stress, higher negative affect), among young adults, even after controlling for social anxiety, depressive symptomology, and social isolation. Contrastingly, increase in social isolation was associated with changes in some health-related factors - more somatic health complaints, higher alcohol use, poorer cognitive and physical functioning, and lower scores for only one health literacy domain (i.e., social support for health) among young adults, after adjusting for the influence of social anxiety, depressive symptomology, and loneliness.
Conclusion: Even after accounting for the influence of several co-occurring social and mental health symptoms, higher loneliness was associated poorer health literacy and health-related factors in young adults. We also found loneliness and social isolation may differ in the mechanisms through which they impact health literacy and health-related factors in young adults.
Introduction
Young adulthood is a critical and transitional period marked with psychosocial challenges (e.g., striving for independence, holding increased responsibilities, and moving away from familial relationships and gravitating toward peer-based relationships; Heinrich and Gullone, 2006). As such, young adults (<35 years old) are susceptible to adverse mental health experiences, particularly feelings of loneliness (Lim et al., 2019; Cigna, 2020; Negosanu and Reid, 2021; Varga et al., 2021). Loneliness is a subjective and adverse experience which arises due to differences between an individual’s actual and desired quality of social relationships (Peplau, 1982). It is more closely associated with the quality of social interactions rather than the quantity or number of social contacts of an individual (de Jong and Havens, 2004). Loneliness is a relatively common experience. Indeed, a 2018 survey found 51 percent of Australian adults felt lonely at least one day a week (Abbott et al., 2018). Most researchers tend to focus on understanding the impact of loneliness on older adults [i.e., >65 years old; (Pinquart and Sorensen, 2001; Routasalo and Pitkala, 2003; Cohen-Mansfield et al., 2016; Kemperman et al., 2019)]. Nonetheless, recent studies show loneliness follows a bi-modal, U-shaped distribution (Yang and Victor, 2011; Pyle and Evans, 2018), where feelings of loneliness peak during adolescence and young adulthood (<35 years), recede in middle adulthood, and increase again in older adulthood [>70 years; (Hawkley et al., 2010; Lasgaard et al., 2016)]. Findings from these studies clearly demonstrate that young adults are just as susceptible to loneliness as older adults (Lim et al., 2019; Cigna, 2020; Negosanu and Reid, 2021; Varga et al., 2021).
Loneliness has been globally recognized as a growing public health concern with a detrimental impact on health (Hunter, 2012; Lim et al., 2020). Findings from Holt-Lunstad et al. (2015) meta-analytic review argues experience of loneliness increases the likelihood of mortality by 26%. Robust evidence from cross sectional and longitudinal research demonstrates the negative impact loneliness can have on physical health [i.e., higher incidences of cardiovascular issues (Grant et al., 2009; Thurston and Kubzansky, 2009)], cognitive health (Shankar et al., 2013), and mental health [i.e., associated with anxiety disorders (Beutel et al., 2017)], psychosis (Sündermann et al., 2014; Lim et al., 2018), schizophrenia (Trémeau et al., 2016), suicidality (Stickley and Koyanagi, 2016), paranoia (Sündermann et al., 2014), social anxiety (Lim et al., 2016), and depression (Cacioppo et al., 2010). For comprehensive review on the impact of loneliness on health, (see Hawkley and Cacioppo, 2010; Lim et al., 2020).
There are several pathways through which loneliness may affect health of young adults, including health literacy and health-related factors. Health literacy refers to the application of social and cognitive skills needed to access, assess, and engage with health-related information to support and sustain good health, and make informed health-related decisions (Nutbeam, 1998). An extensive literature documents the association between lower health literacy and poorer health outcomes (Marvanova et al., 2011; Mitchell et al., 2012; Geboers et al., 2016; Miller, 2016). Further, limited research indicates an inverse relationship between loneliness and health (Bennett et al., 2012; Geboers et al., 2016; Vasan et al., 2022). In the current study, health-related factors are comprised of several physical health factors (e.g., body mass index (BMI), weight, diet, sleep, somatic health complaints, alcohol use, physical activity, perceived general health, cognitive and physical functioning), and psychosocial factors (e.g., quality of life, perceived stress, positive affect, and negative affect). There is some evidence to suggest a negative relationship between loneliness and some of these health-related factors. Higher loneliness is associated with higher obesity (Fernández-Alonso et al., 2012; Hajek and König, 2019), elevated BMI (Fernández-Alonso et al., 2012), lower quality of life (Ong et al., 2016; Khalaila and Vitman-Schorr, 2018) among older adults. Loneliness is associated with increased sleep difficulties [e.g., poor sleep quality, sleep fragmentation/disturbances, poor day time functioning; (Hawkley et al., 2010; Kurina et al., 2011; Eccles et al., 2020; Griffin et al., 2020; Shankar, 2020)], and overall poorer self-rated health (Richard et al., 2017; Counts and John-Henderson, 2020; Eccles et al., 2020; Marziali et al., 2020; Christiansen et al., 2021). Researchers have found mixed results for the effect of loneliness on physical activity, with Hawkley and colleagues (Hawkley et al., 2009; Luo and Waite, 2014) demonstrating higher loneliness to be associated with lower levels of physical activity. Conversely, studies have found no impact of loneliness on physical activity levels (McKee et al., 2015). There is some evidence to suggest a positive relationship between loneliness and somatic health issues (e.g., asthma, allergy, diabetes, migraine, osteoarthritis) in adolescence and young adults (Stickley et al., 2016; Christiansen et al., 2021). Increased experience of loneliness is positively correlated with perceived stress and positive affect among college students (Counts and John-Henderson, 2020). Likewise, negative relationships have been reported between loneliness and negative affect across different age groups (Kurina et al., 2011; Ijzerman et al., 2012; Counts and John-Henderson, 2020). Taken together, these findings demonstrate the detrimental impact feelings of loneliness can have on various health-related factors and to some extent, health literacy. Nonetheless, aforementioned studies are not without limitations. The main issues identified in existing literature are, as mentioned previously, limited focus on the impact of loneliness on health literacy and health-related factors in young adults, especially in Australia, and the oversight to account for the influence of other co-occurring social and mental health symptoms such as, social isolation, depressive symptomology, and social anxiety.
The relationship between loneliness and several social and mental health issues (i.e., social isolation, depressive symptomology, and social anxiety) is nuanced and multifaceted (Christiansen et al., 2021). It is well established that depression has a detrimental impact on health in general (Belvederi Murri et al., 2018). However, recent research has identified loneliness as a potential antecedent for depression (Cacioppo et al., 2010). Further, loneliness has a more reciprocal or bidirectional relationship with social anxiety. Lim et al., (2016) found baseline loneliness predicted social anxiety, paranoia, and depression when measured over a six-month period in a community sample. However, only social anxiety predicted loneliness above and beyond paranoia and depression (Lim et al., 2016) [for a review, (see Maes et al., 2019)]. Further, in the present study, we have given special attention to the influence of social isolation and its relationship with loneliness. Often, the construct of social isolation is interchangeably and synonymously used with the term loneliness (de Jong and Havens, 2004) [for examples, (see Caspi et al., 2006; Banerjee and Rai, 2020)]. It is important to understand that while related, social isolation and loneliness are distinct concepts (Cornwell and Waite, 2009). Loneliness is a subjective emotional experience where one feels their current relationships do not meet their desired social need, conversely, social isolation is an objective, quantifiable variable which measures the number of an individual’s social interactions and social contacts (Asher and Paquette, 2003; de Jong and Havens, 2004). Indeed, in a recent study Beller and Wagner, (2018) found loneliness and social isolation differ significantly in how they impact mortality among older adults. Therefore, to capture the unique influence of loneliness on health literacy and health-related factors, especially in a less researched population such as young adults, it is crucial to consider the role of these co-occurring social and mental health issues.
The aims of the present cross-sectional study are: (1) to extend previous research by investigating the unique influence of loneliness on health literacy and health-related factors among young adults (<35 years old), after controlling for social isolation, depressive symptomology, and social anxiety. It is hypothesized that higher loneliness in young adults would predict lower health literacy and poorer responses on health-related factors, after controlling for social isolation, depressive symptomology, and social anxiety. (2) to evaluate how social isolation (a term sometimes used interchangeably with loneliness), and loneliness may differ in their impact on health-related factors and health literacy of young adults. It is hypothesized that loneliness and social isolation would differ in their associations with health- related factors and health literacy domains in young adults.
Methods
Ethical approval was granted by local Australian University’s ethics committee. The data used in the current study was a subset of a larger study. Participants completed a self-report survey hosted on Qualtrics (survey platform). Survey was distributed through word of mouth, advertisements on social networks, online forums, and via research training program for undergraduate first year students. Participation was voluntary, explanatory statement was included in the survey, and informed consent was obtained prior to participants completing the survey. All data was deidentified to maintain participants privacy and confidentiality. Data were collected between June 2020 and November 2020. A total of 521 Australian young adults were included in the final dataset. The online survey included demographic questions, comprehensive measures for loneliness, social isolation, social anxiety, and depressive symptomology. Further, a health literacy scale, and measures for different health-related factors were also included. Details for all scales and materials used in the current study are as follows.
Materials
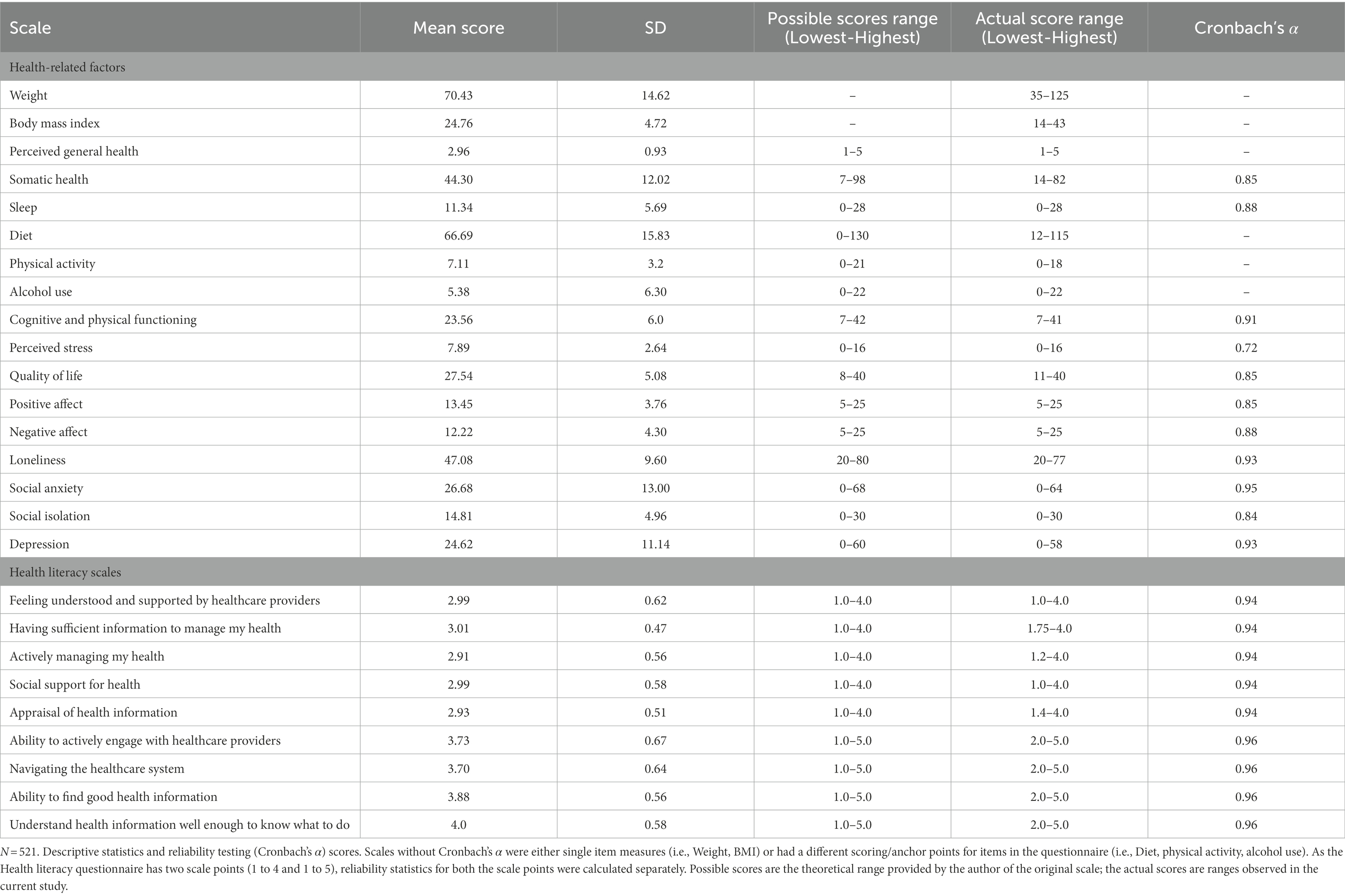
Demographic information including age, gender, use of English as primary language, marital status, ethnicity, sexual orientation, education level, living status, chronic conditions, and smoking status were obtained. Participants self-reported their weight and height measurements as well as number of diagnosed chronic conditions. BMI scores were calculated from the self-reported weight and height measurements. Scores for physical activity and alcohol use were calculated using participant’s responses for frequency and intensity of use. Additional information on how these abovementioned health-related outcomes were measured is provided in Supplementary material. The internal reliability values (Cronbach’s α) for the data and scales used in the present study are included in Table 1.
University of California Los Angeles (UCLA) loneliness scale
The UCLA is a 20-question questionnaire using a 1 (Never) to 4 (Always) Likert-type scale. UCLA assesses levels of loneliness over a one-month period (Russell, 1996). It includes both positively worded items (e.g., “How often do you feel that you are “in tune” with the people around you?”) and negatively worded (e.g., “How often do you feel that people are around you but not with you?”) questions (Russell, 1996). Total scores are calculated by reverse coding the positively worded questions and then summing the scores for all the questions, scores range from 20 to 80 with higher scores indicating higher levels of loneliness. The UCLA has been researched extensively across different populations and has demonstrated excellent reliability and convergent validity with related constructs (Russell, 1996).
Lubben social network scale
The Lubben social network scale (LSNS) is a 6 item self-reported scale that assesses the frequency and quality of social contact or engagement with friends and family members. LSNS uses a 0 (none) to 5 (nine or more) Likert-type scale. An example from the questionnaire includes “How many of your friends do you see or hear from at least once a month?” (Lubben, 1998). Composite scores are calculated by summing the scores for all six questions, scores range from 0 to 30. Higher scores indicate more social engagement and lower social isolation. LSNS has demonstrated adequate levels of reliability (Lubben, 1998).
Social interaction anxiety scale
In the present study, straightforward version of the Social interaction anxiety scale (SIAS) was used. In the straightforward version as opposed to the original 20-item SIAS, only the straightforward (negatively worded) items are used. Rodebaugh et al., (2007) advise using only the straightforward 17-items as they are the better indicators of social interaction anxiety, whereas the three reverse-coded (positively worded) questions fall more closely into the category of extraversion. SIAS uses a 0 (Not at all characteristic of me) to 4 (Extremely characteristic of me) Likert-type scale (Brown et al., 1997). The scale assesses an individual’s thoughts, emotions, and behaviors in social settings. An example item includes “When mixing socially, I am uncomfortable.” Composite scores are calculated by adding the scores for all 17 questions, total scores range from 0 to 68. Higher scores suggest higher social interaction anxiety. Previous research has shown excellent reliability and construct validity for the straightforward SIAS (Brown et al., 1997).
Centre for epidemiological studies – depression
The Centre for epidemiological studies – depression (CES-D) is a 20-question measure of depressive symptomology. It uses a 0 (rare or none of the time) to 3 (Most or all of the time) Likert-type scale (Radloff, 1977). CES-D assesses how an individual may have felt or behaved over the past week (e.g., I felt that I could not shake off the blues even with help from my family or friends). Total scores are calculated by reverse coding the positively worded items and summing the scores for all individual items. Composite scores span from 0 to 60, with higher score indicating higher depressive symptomology over the last week. Previous studies demonstrate excellent internal reliability (Radloff, 1977).
Health literacy scale
Health literacy questionnaire
Health literacy questionnaire (HLQ) has 44 questions and includes nine independent and conceptually different domains or scales. Together these nine scales offer insight into the individual’s knowledge of, engagement with, and application of health-related information and services (Osborne et al., 2013). The nine distinct domains are as follows: (1) Feeling understood and supported by healthcare providers; (2) Having sufficient information to manage my health; (3) Actively managing my health; (4) Social support for health; (5) Appraisal of health information; (6) Ability to actively engage with healthcare providers; (7) Navigating the healthcare system; (8) Ability to find good health information; and (9) Understanding health information well enough to know what to do.
Each scale consists of four to six questions. Domains one to five use a 1 (strongly disagree) to 4 (strongly agree) Likert-type scale. The remaining four scales employ a 1 (cannot do) to 5 (very easy) anchor type. Nine separate scores for each domain are calculated by averaging the values (responses) for questions within each of the scales, possible scores for the first five scales are 1 to 4, for domains six to nine, scores can range from 1 to 5. Higher domain scores are indicative of superior understanding and use of health-related services and information (i.e., higher health literacy) for that particular scale. There are no aggregate or total scores for the nine scales as doing so could under- or over-estimate an individual’s particular needs in specific health literacy domains (Osborne et al., 2013). HLQ has demonstrated strong psychometric properties and has been validated for use across diverse settings and populations [e.g., clinical, home, community care, adults 18 to 64 years and over; (Osborne et al., 2013; Elsworth et al., 2016; Kolarcik et al., 2017; Richtering et al., 2017)].
Measures for health-related factors
Insomnia severity index
Insomnia severity index (ISI) is self-report scale measuring symptoms of insomnia or poor sleep over a fortnight. ISI includes seven items and employs a 0 (no problem) to 4 (very severe problem) Likert-type scale. An example includes “To what extent do you consider your sleep problem to INTERFERE with your daily functioning?” (Morin et al., 2011). Total scores are calculated by adding the scores individual items, scores range from 0 to 28. Higher scores are indicative of more sleeping difficulties. Previous studies demonstrated very strong internal consistency [Cronbach’s α ranging from 0.90 to 0.91; (Morin et al., 2011)].
Physical health questionnaire
The Physical health questionnaire (PHQ) is a brief self-report measure of somatic health symptoms. The PHQ is a revised version of the health scale created by Spence et al., (1987). PHQ includes 14 questions and four subscales (Schat et al., 2005). The four subscales represent the following four facets of physical health symptoms: sleep difficulties, headaches, gastrointestinal and respiratory tract issues. PHQ employs a 7-point frequency scale, an example includes “How often have you suffered from an upset stomach (indigestion)?.” Individual scores can either be calculated for four physical health symptom scales by summing the scores for the corresponding scale questions. Otherwise, as performed in this study, a total somatic health score can be calculated by summing the scores for all four physical health symptom scales. Scores ranged from 7 to 98 with higher scores indicating more somatic health issues. The scale has good psychometric properties (Schat et al., 2005).
Diet quality tool
The Diet quality tool (DQT) includes 13 questions which evaluate quality of respondent’s dietary habits (e.g., vegetable and fruit intake, saturated or total fat intake). DQT employs a 0 to 10 type anchor, where a score of 10 is indicative of higher diet quality (i.e., the participant is satisfactorily following the nutritional guidelines to prevent cardiovascular disease) (O’Reilly and McCann, 2012). Nine questions of the DQT include category/quality of food groups consumed, such as types of bread, spreads, pasta/noodles/rice, fish, fat on meats, breakfast foods, milk, salt use in cooking and meals. The four remaining questions assess the quantity of food consumed (e.g., fruit and vegetable intake, quantity of high-fat sweet and savory foods products consumed). Composite scores are calculated by adding answers for each item, total scores span from 0 to 130, higher scores suggesting a higher quality of diet (O’Reilly and McCann, 2012).
The Massachusetts general hospital cognitive and physical functioning questionnaire
Cognitive and physical functioning questionnaire (CPFQ) was developed to be a brief measure of cognitive and executive dysfunction in mood and anxiety disorders (Fava et al., 2009). It assesses cognitive and physical functioning over a one-month period. Each CPFQ item is answered with a 6-point Likert-type scale, ranging from 1 (greater than normal) to 6 (totally absent) (Fava et al., 2009). An example includes “How has your ability to focus/sustain attention been over the past month?.” CPFQ has previously shown good test–retest reliability and other psychometric properties (Fava et al., 2009).
Perceived general health
Perceived general health was measured using a single question “In general would you say that your health is excellent, very good, good, fair or poor?” on a 1 to 5 (poor to excellent) scale. Higher scores are indicative of higher perceived general health.
EUROHIS – Quality of life scale
Quality of life scale (QOL) is an 8-item scale which assess overall quality of life, general health, energy, daily living activity, self-esteem, social relationships, home life, and finances of an individual over a two-week period. QOL is derived from the WHOQOL-BREF and employs a 1 to 5 Likert-type scale. Previous research has demonstrated good internal consistency (Cronbach’s α = 0.83) and satisfactory convergent and discriminant validity for QOL (Schmidt et al., 2005).
Perceived stress scale-4
This four-item scale of stress was derived from the original 14-item perceived stress scale (PSS). PSS uses a 5-point Liker-type anchor, ranging from 0 (never) to 4 (very often). It includes both positively and negatively worded questions which evaluate a individuals experience of stressful events over the last month (e.g., “In the last month, how often have you felt that you were unable to control the important things in your life?”). PSS is negatively correlated perceived health, social support, being male, and older age (Warttig et al., 2013). Research has demonstrated good reliability and psychometric properties for PSS (Warttig et al., 2013).
Positive and negative affect scale
The Positive and negative affect scale (PANAS) short form measures positive (e.g., excited) and negative (e.g., scared) affect over a one-week period. Affect is assessed through 10 items on a 5-point Likert-type scale, ranging from 1 (very slightly or not at all) to 5 (extremely). PANAS has demonstrated good internal consistency, convergent, and discriminant validity in previous literature (Watson et al., 1988).
Statistical technique
The data were analyzed using IBM Statistical Package for Social Sciences (SPSS) Version 27.0. A total of 521 participants were included in this study. The data cleaning, screening, and assumption testing information for the statistical techniques used in present study are included in Supplementary material. In the present study, an alpha value less than or equal to 0.05 is used as a cut-off for statistical significance.
To investigate the first aim - the unique contribution of loneliness on health literacy and health-related factors among young adults, we used Hierarchical Multiple Regression, where the predictor variable was loneliness. Outcome variables included nine health literacy scales and various health-related factors (i.e., weight, BMI, somatic health, perceived general health, sleep, diet, alcohol use, physical activity, cognitive and physical functioning, perceived stress, quality of life, positive affect, negative affect). Further, guided by previous empirical research, several covariates were included – age, gender, chronic conditions, scores for social anxiety [covaries with loneliness; (Cacioppo et al., 2010; Trémeau et al., 2016; Abbott et al., 2018)], scores for depressive symptomology [loneliness is often a precursor for depression; (Cacioppo et al., 2010; Stickley and Koyanagi, 2016)], and scores for social isolation [construct oftentimes interchangeably and synonymously used with the term loneliness; (Abbott et al., 2018)]. For all models, in the first step (Model 1) – age, gender, chronic conditions were entered. In step two (Model 2) social anxiety scores were included. In step three (Model 3), depressive symptomology scores were entered. Step four included social isolation scores (Model 4). In the final step (Model 5) loneliness scores were entered to ascertain its unique contribution to various health-related factors and health literacy outcomes among young adults.
To examine our second aim - how social isolation may differ from loneliness in its impact on health literacy and health-related factors of young adults, we utilized Hierarchical Multiple Regression. For these analyzes, the predictor variable was social isolation, outcome variables included nine health literacy scales and various health-related factors. Covariates included age, gender, chronic conditions, depressive symptomology, social anxiety, and loneliness. For all models, in the first step (Model 1) - age, gender, chronic conditions were entered. In step two (Model 2) social anxiety scores were included. In step three (Model 3), depressive symptomology scores were entered. Step four included loneliness scores (Model 4). In the final step (Model 5) social isolation scores were entered to ascertain how it may differ from loneliness in regards to its impact on health literacy and different health-related factors of young adults.
Results
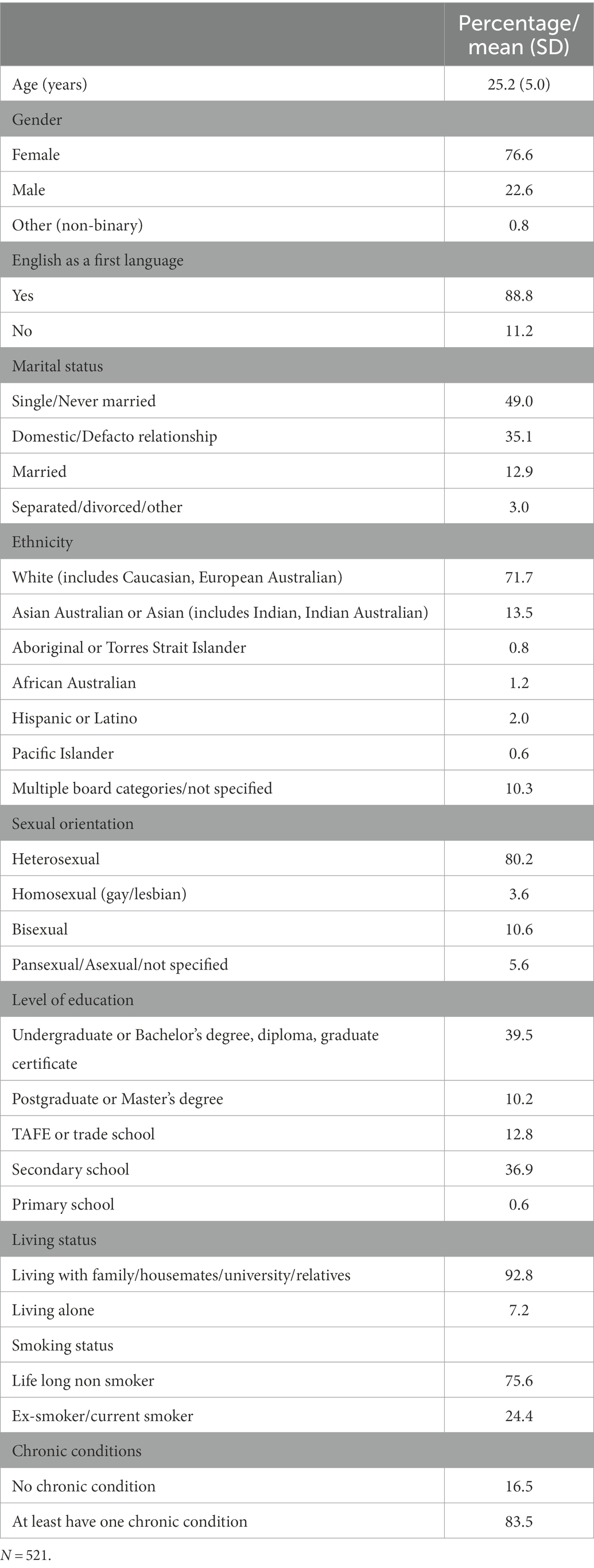
A complete breakdown of sample characteristics is presented in Table 2. Percentages are included for categorical variables, mean and standard deviation (SD) are included for continuous variables. The Chi squared goodness of fit test for gender was non-significant, suggesting that the sample was not biased (test details and results are included in the Supplementary material).
The descriptive statistics and internal reliability values (Cronbach’s α) for all scales used in current study are presented in Table 1.
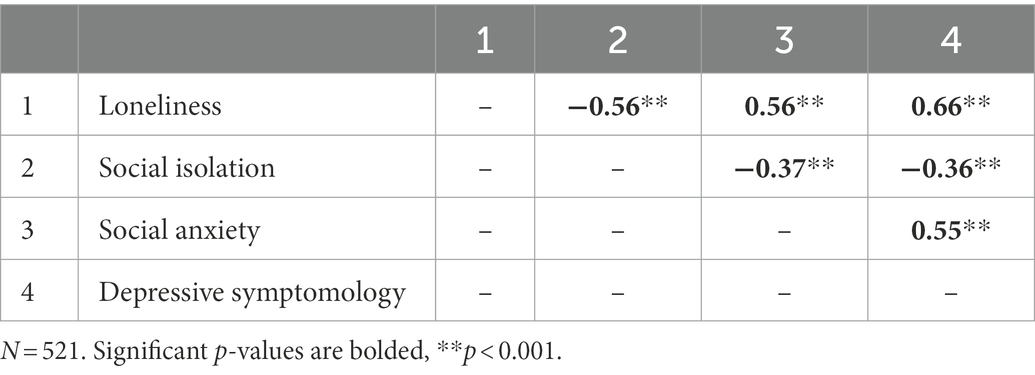
Correlation matrix for predictors variables and covariates (loneliness, social isolation, depressive symptomology, social anxiety) are displayed in Table 3. There were significant and large associations between loneliness, and social isolation, social anxiety, depressive symptomology, these directions were as expected.
For the first aim, hierarchical regression results, including the R2 change values (i.e., unique variance accounted by loneliness in the dependent variable) for all outcome variables are presented in Table 4. After controlling for age, gender, chronic conditions, social anxiety, depressive symptomology, and social isolation, increased loneliness was associated with increase in several health literacy domains and health-related factors. Higher loneliness was associated with poorer health literacy among young adults. For examples, those with increased feelings of loneliness also reported lower scores for feeling understood and supported by healthcare providers, poorer social support for health, lower appraisal of health information, poorer ability to find good health information, and lower understanding of health information among young adults. Further, higher loneliness was associated with higher perceived stress and increased negative affect. Increase in loneliness also predicted poorer quality of life among young adults.
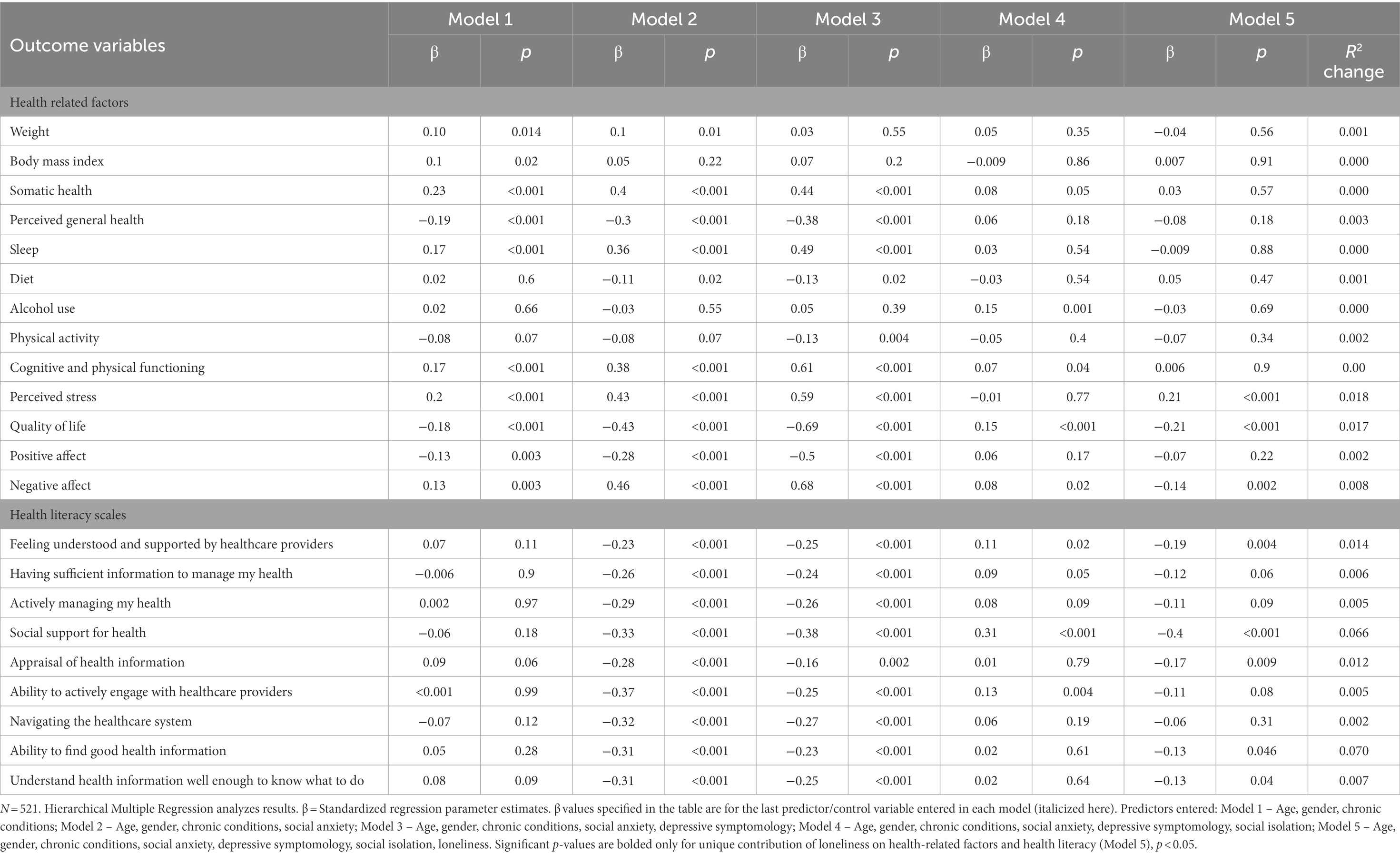
Table 4. Hierarchical multiple regression models for unique association between loneliness and health-related factors and health literacy in young adults.
For the second aim, hierarchical regression results, including the R2change values (i.e., unique variance accounted by social isolation in the dependent variable) for all outcome variables are presented in Table 5. After controlling for age, gender, chronic conditions, social anxiety, depressive symptomology, and loneliness, increase in social isolation was associated with increase in somatic health complaints and alcohol use among young adults. Increased social isolation was associated with lower cognitive and physical functioning. However, note this association was only marginally statistically significant (p = 0.058). Those with higher experience of social isolation also reported lower quality of life and lower health literacy in one domain (i.e., social support for health).
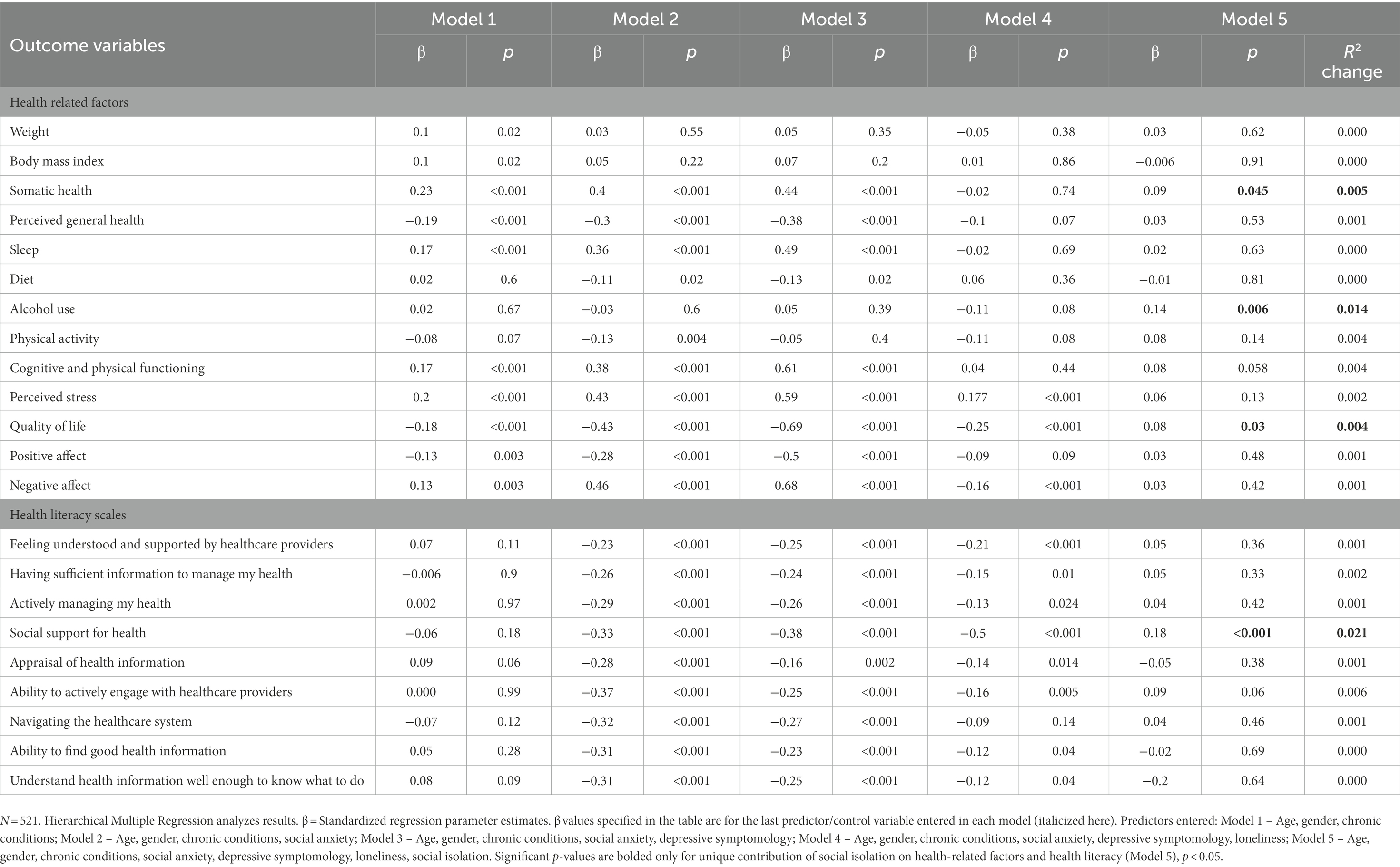
Table 5. Hierarchical multiple regression models for how social isolation may differ from loneliness in its impact on health-related factors and health literacy among young adults.
Discussion
Results from the present study extent previous empirical literature on unique influence of loneliness on health literacy and health-related factors in young adults, after controlling for co-occurring social and mental health symptoms. The present study also examined how the constructs of social isolation and loneliness may differ in their impact on different health-related factors and health literacy of young adults.
Similar to previous literature regarding the negative influence of loneliness on health literacy among older adults (Bennett et al., 2012; Geboers et al., 2016), we found higher levels of loneliness to be associated with lower scores on several health literacy domains in young adults, after controlling for social isolation, depressive symptomology, and social anxiety. For example, young adults with higher loneliness reported lower scores for feeling understood and supported by healthcare providers, poorer social support for health, lower appraisal of health information, poorer ability to find good health information, and lower understanding of health information. These results indicate higher loneliness to be associated with overall lower health literacy among young adults. These findings are particularly concerning as results from the Australian Bureau of Statistics health literacy survey using the HLQ shows over 70 percent of all young adults reported higher scores across all nine health literacy scales (Australian Bureau of Statistics, 2018). In other words, young adults, in general, indicated they were adept at understanding, evaluating, and utilizing health information to promote and maintain good health (Australian Bureau of Statistics, 2018). Collectively, these findings suggest that unlike individuals with lower loneliness, young adults with higher loneliness may be at a disadvantage when it comes to understating, appraising, and using health information and health services. This negative relationship between loneliness and health literacy is especially troubling, given the association between lower health literacy and overall poorer health outcomes [i.e., higher hospital re-admission rates; (Mitchell et al., 2012), misunderstanding of medication instructions; (Marvanova et al., 2011), lower adherence to medical treatment; (Miller, 2016), and lower ability to self-managed care; (Geboers et al., 2016)].
Consistent with prior research (Kurina et al., 2011; Ijzerman et al., 2012; Ong et al., 2016; Khalaila and Vitman-Schorr, 2018; Counts and John-Henderson, 2020), and after controlling for concomitant social and mental health factors, we found higher loneliness was associated with higher perceived stress and negative affect, and lower quality of life, this was evident in the adjusted hierarchical regression analysis results included in Table 4. However, contrary to some of the previous research (Hawkley et al., 2009, 2010; Kurina et al., 2011; Fernández-Alonso et al., 2012; Luo and Waite, 2014; Ong et al., 2016; Stickley et al., 2016; Richard et al., 2017; Khalaila and Vitman-Schorr, 2018; Hajek and König, 2019; Counts and John-Henderson, 2020; Griffin et al., 2020; Marziali et al., 2020; Shankar, 2020; Christiansen et al., 2021), we did not find significant relationships between loneliness and several health-related factors including, weight, BMI, somatic health complaints, perceived general health, sleep, diet, alcohol use, physical activity, cognitive and physical functioning, and positive affect, after controlling for the influence of social isolation, depressive symptomology, and social anxiety among young adults. A plausible explanation for the lack of significant relationships between these health-related factors and loneliness could be that some of the predictive and explanatory power attributed to loneliness, in relation to poor health in previous research, may in fact be the influence of social isolation, depressive symptomology, or social anxiety. This premise is supported by the hierarchal regression results presented Table 4 as well as additional analyzes included in Supplementary material, which showcase significant relationships between social anxiety, depressive symptomology, and social isolation, and various health-related factors (e.g., diet quality, somatic health complaints, sleep). Further, as shown in the correlation matrix presented in Table 3, we found strong associations between loneliness, and social anxiety, depressive symptomology, and social isolation, further highlighting the need to adjust for the influence of these social and mental health indicators, when examining the impact of loneliness on health-related factors among young adults.
The findings from present study also shed more light on how loneliness and social isolation may differ in their impact on health-related factors and health literacy of young adults. After controlling for age, gender, chronic conditions, social anxiety, depressive symptomology, and loneliness, higher social isolation was associated with increase in somatic health complaints, namely more respiratory (e.g., cold, flu, bronchitis symptoms) and gastrointestinal tract (e.g., indigestion, nausea, diarrhea) issues, as well as increased complaints of headaches and sleep difficulties. Likewise, higher experience of social isolation was associated with higher alcohol use, lower quality of life, and lower cognitive and physical functioning (marginally significant) among young adults. However, unlike loneliness, increased social isolation was only associated with lower score in one health literacy domain (i.e., social support for health). Together, these findings indicate higher loneliness may more closely affect psychosocial health-related factors (e.g., lower perceived stress, higher negative affect) and health literacy issues, as per associations presented in Table 4. Social isolation on the other hand may influence physical health-related factors of an individual (e.g., somatic health complaints as per associations presented in Table 4), similar to the findings from Beller and Wagner, (2018). Together, these associations suggest that while loneliness and social isolation may be interrelated and share a few superficial characteristics, the mechanisms (psychosocial health and health literacy issues as opposed to physical health issues respectively) in which they influence health literacy and poorer health-related factors of young adults may be different.
Limitations and future directions for research
Nonetheless, present study was not without limitations. The generalizability of our findings is limited. First, the data collection for this study occurred during the novel coronavirus pandemic when several physical and social distancing restrictions were in place in Australia, especially in the state of Victoria (Department of Health and Human Services Victoria, 2020), where majority of our sample reside. The psychological and social changes associated with the pandemic restrictions may have impacted our findings. Indeed, several studies demonstrate pandemic and its associated social and physical distancing restrictions may have negatively affected the health of many Australians (i.e., psychosocial, physical, and mental health; (Australian Medical Association, 2020; Holmes et al., 2020). Second, a substantial proportion of our sample consisted of first year undergraduate university students, predominantly those who spoke English as a primary language, resided in the state of Victoria, were living with other people, and were Caucasian, and identified as heterosexual females. University student populations are often utilized in psychosocial research as they are an efficient, user-friendly convenience population with lower response bias, administrative cost, and easily recruited (Lucas, 2003; Arnett, 2008). However, it is vital to acknowledge that use of such a sample may not be representative of the general young adult population of Australia, which could result in a more homogenous sample, consequently impacting the generalizability, and by extension, the external validity (McTavish and Loether, 2002) of our findings.
Another limitation of this study was the cross-sectional design used. Use of cross-sectional study design limits our ability to draw causal inferences or ascertain directionality between loneliness and its association with health literacy and various health-related factors among young adults. Future research with longitudinal data and a more heterogeneous young adult population could provide a deeper insight into the strength, causality, and directionality of the unique relationship between loneliness and health literacy and different health-related factors among young adults. Despite these limitations, findings from the current study highlight an information gap and investigate the impact of loneliness on health literacy and various health-related factors among young adults, after accounting for the influence of other concomitant variables. We also demonstrate how loneliness and related constructs such as social isolation may differ in their impact on heath literacy and health-related factors of young adults.
Conclusion
Loneliness is a relatively common experience which has universally been identified as a growing public health concern with a detrimental impact on health. While traditional research focused on the impact of loneliness on older adults, recent studies demonstrate younger adults are equally as susceptible to the ill effects of loneliness. Our findings show increased loneliness is associated with decrease in several health literacy domains (e.g., poorer social support for health, lower appraisal of health information) and health-related factors among young adults, even after controlling for co-occurring social and mental health symptoms. Additionally, we highlight the importance of controlling for concomitant social and mental health symptoms such as social anxiety, depressive symptomology, and social isolation when investigating the impact of loneliness on health-related factors. Further, we found loneliness and social isolation may in fact differ in the way they impact health literacy and various health-related factors in young adults. However, some considerations need to be made when interpreting our findings, use of cross-sectional study design and primarily female student population limits our ability to make causal inference and generalize our findings across different populations. Nevertheless, findings from the current study contribute to the growing literature on the impact of loneliness on health literacy and various health-related factors among young adults. A better understanding of the impact of loneliness on these health-related issues can inform the development of appropriate public health strategies to facilitate access to health services and health-related information among young adults.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by Ethical approval was granted by Swinburne University Human Research Ethics Committee (approval number 20202950-4247). The patients/participants provided their written informed consent to participate in this study.
Author contributions
SV collected the data, performed data analysis, and wrote the manuscript as part of their PhD dissertation. NE, ML, and EL conceptualized and developed the study as well as provided supervision to SV throughout recruitment, data analysis, and manuscript writing. All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyg.2023.996611/full#supplementary-material
References
Abbott, J., Lim, M. H., Eres, R., Long, K., and Mattews, R.. (2018). The impact of loneliness on the health and wellbeing of Australians. Available at: https://psychology.org.au/for-members/publications/inpsych/2018/december-issue-6/the-impact-of-loneliness-on-the-health-and-wellbei (Accessed January 20, 2022).
Arnett, J. J. (2008). The neglected 95%: why American psychology needs to become less American. Am. Psychol. 63, 602–614. doi: 10.1037/0003-066x.63.7.602
Asher, S. R., and Paquette, J. A. (2003). Loneliness and peer relations in childhood. Curr. Dir. Psychol. Sci. 12, 75–78. doi: 10.1111/1467-8721.01233
Australian Bureau of Statistics (2018). National health survey: health literacy. Australian Government. Available at: https://www.abs.gov.au/statistics/health/health-conditions-and-risks/national-health-survey-health-literacy/2018 (Accessed January 20, 2022).
Australian Medical Association (2020). COVID-19 impact likely to lead to increased rates of suicide and mental illness. Australian Government. Available at: https://www.ama.com.au/media/joint-statement-covid-19-impact-likely-lead-increased-rates-suicide-and-mental-illness (Accessed January 20, 2022).
Banerjee, D., and Rai, M. (2020). Social isolation in Covid-19: the impact of loneliness. Int. J. Soc. Psychiatry 66, 525–527. doi: 10.1177/0020764020922269
Beller, J., and Wagner, A. (2018). Loneliness, social isolation, their synergistic interaction, and mortality. Health Psychol. 37, 808–813. doi: 10.1037/hea0000605
Belvederi Murri, M., Ekkekakis, P., Magagnoli, M., Zampogna, D., Cattedra, S., Capobianco, L., et al. (2018). Physical exercise in major depression: reducing the mortality gap while improving clinical outcomes. Front. Psychiatry 9:762. doi: 10.3389/fpsyt.2018.00762
Bennett, J. S., Boyle, P. A., James, B. D., and Bennett, D. A. (2012). Correlates of health and financial literacy in older adults without dementia. BMC Geriatr. 12:30. doi: 10.1186/1471-2318-12-30
Beutel, M. E., Klein, E. M., Brähler, E., Reiner, I., Jünger, C., Michal, M., et al. (2017). Loneliness in the general population: prevalence, determinants and relations to mental health. BMC Psychiatry 17:97. doi: 10.1186/s12888-017-1262-x
Brown, E. J., Turovsky, J., Heimberg, R. G., Juster, H. R., Brown, T. A., and Barlow, D. H. (1997). Validation of the social interaction anxiety scale and the social phobia scale across the anxiety disorders. Psychol. Assess. 9, 21–27. doi: 10.1037/1040-3590.9.1.21
Cacioppo, J. T., Hawkley, L. C., and Thisted, R. A. (2010). Perceived social isolation makes me sad: 5-year cross-lagged analyses of loneliness and depressive symptomatology in the Chicago health, aging, and social relations study. Psychol. Aging 25, 453–463. doi: 10.1037/a0017216
Caspi, A., Harrington, H., Moffitt, T. E., Milne, B. J., and Poulton, R. (2006). Socially isolated children 20 years later: risk of cardiovascular disease. JAMA Pediatr. 160, 805–811. doi: 10.1001/archpedi.160.8.805
Christiansen, J., Qualter, P., Friis, K., Pedersen, S. S., Lund, R., Andersen, C. M., et al. (2021). Associations of loneliness and social isolation with physical and mental health among adolescents and young adults. Perspect. Public Health 141, 226–236. doi: 10.1177/17579139211016077
Cigna (2020). Loneliness and the workplace: 2020 U.S. Report. Available at: https://www.cigna.com/static/www-cigna-com/docs/about-us/newsroom/studies-and-reports/combatting-loneliness/cigna-2020-loneliness-factsheet.pdf (Accessed January 20, 2022).
Cohen-Mansfield, J., Hazan, H., Lerman, Y., and Shalom, V. (2016). Correlates and predictors of loneliness in older-adults: a review of quantitative results informed by qualitative insights. Int. Psychogeriatr. 28, 557–576. doi: 10.1017/S1041610215001532
Cornwell, E. Y., and Waite, L. J. (2009). Measuring social isolation among older adults using multiple indicators from the NSHAP study. J. Gerontol. B Psychol. Sci. Soc. Sci. 64, i38–i46. doi: 10.1093/geronb/gbp037
Counts, C. J., and John-Henderson, N. A. (2020). Risk in childhood family environments and loneliness in college students: implications for health. J. Am. Coll. Heal. 68, 381–386. doi: 10.1080/07448481.2018.1557198
de Jong, G. J., and Havens, B. (2004). Cross-national comparisons of social isolation and loneliness: introduction and overview. Can. J. Aging 23, 109–113. doi: 10.1353/cja.2004.0021
Department of Health and Human Services Victoria (2020). Updates about the outbreak of the coronavirus disease (COVID-19). Australian Government. Available at: https://www.dhhs.vic.gov.au/coronavirus/updates (Accessed January 20, 2022).
Eccles, A. M., Qualter, P., Madsen, K. R., and Holstein, B. E. (2020). Loneliness in the lives of Danish adolescents: associations with health and sleep. Scand. J. Public Health 48, 877–887. doi: 10.1177/1403494819865429
Elsworth, G. R., Beauchamp, A., and Osborne, R. H. (2016). Measuring health literacy in community agencies: a Bayesian study of the factor structure and measurement invariance of the health literacy questionnaire (HLQ). BMC Health Serv. Res. 16:508. doi: 10.1186/s12913-016-1754-2
Fava, M., Iosifescu, D. V., Pedrelli, P., and Baer, L. (2009). Reliability and validity of the Massachusetts general hospital cognitive and physical functioning questionnaire. Psychother. Psychosom. 78, 91–97. doi: 10.1159/000201934
Fernández-Alonso, A. M., Trabalón-Pastor, M., Vara, C., Chedraui, P., and Pérez-López, F. R. (2012). Life satisfaction, loneliness and related factors during female midlife. Maturitas 72, 88–92. doi: 10.1016/j.maturitas.2012.02.001
Geboers, B., Reijneveld, S. A., Jansen, C. J. M., and de Winter, A. F. (2016). Health literacy is associated with health behaviors and social factors among older adults: results from the LifeLines cohort study. J. Commun. Health 21, 45–53. doi: 10.1080/10810730.2016.1201174
Grant, N., Hamer, M., and Steptoe, A. (2009). Social isolation and stress-related cardiovascular, lipid, and cortisol responses. Ann. Behav. Med. 37, 29–37. doi: 10.1007/s12160-009-9081-z
Griffin, S. C., Williams, A. B., Ravyts, S. G., Mladen, S. N., and Rybarczyk, B. D. (2020). Loneliness and sleep: a systematic review and meta-analysis. Health Psychol Open. 7:2055102920913235. doi: 10.1177/2055102920913235
Hajek, A., and König, H. H. (2019). Obesity and loneliness. Findings from a longitudinal population-based study in the second half of life in Germany. Psychogeriatrics 19, 135–140. doi: 10.1111/psyg.12375
Hawkley, L. C., and Cacioppo, J. T. (2010). Loneliness matters: a theoretical and empirical review of consequences and mechanisms. Ann. Behav. Med. 40, 218–227. doi: 10.1007/s12160-010-9210-8
Hawkley, L. C., Preacher, K. J., and Cacioppo, J. T. (2010). Loneliness impairs daytime functioning but not sleep duration. Health Psychol. 29, 124–129. doi: 10.1037/a0018646
Hawkley, L. C., Thisted, R. A., and Cacioppo, J. T. (2009). Loneliness predicts reduced physical activity: cross-sectional & longitudinal analyses. Health Psychol. 28, 354–363. doi: 10.1037/a0014400
Hawkley, L. C., Thisted, R. A., Masi, C. M., and Cacioppo, J. T. (2010). Loneliness predicts increased blood pressure: 5-year cross-lagged analyses in middle-aged and older adults. Psychol. Aging 25, 132–141. doi: 10.1037/a0017805
Heinrich, L. M., and Gullone, E. (2006). The clinical significance of loneliness: a literature review. Clin. Psychol. Rev. 26, 695–718. doi: 10.1016/j.cpr.2006.04.002
Holmes, E. A., O’Connor, R. C., Perry, V. H., Tracey, I., Wessely, S., Arseneault, L., et al. (2020). Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatry 7, 547–560. doi: 10.1016/s2215-0366(20)30168-1
Holt-Lunstad, J., Smith, T. B., Baker, M., Harris, T., and Stephenson, D. (2015). Loneliness and social isolation as risk factors for mortality: a meta-analytic review. Perspect. Psychol. Sci. 10, 227–237. doi: 10.1177/1745691614568352
Hunter, D. (2012). Loneliness: a public health issue. Perspect. Public Health 132:153. doi: 10.1177/1757913912449564
Ijzerman, H., Gallucci, M., Pouw, W. T. J. L., Weiβgerber, S. C., Van Doesum, N. J., and Williams, K. D. (2012). Cold-blooded loneliness: social exclusion leads to lower skin temperatures. Acta Psychol. 140, 283–288. doi: 10.1016/j.actpsy.2012.05.002
Kemperman, A., van den Berg, P., Weijs-Perrée, M., and Uijtdewillegen, K. (2019). Loneliness of older adults: social network and the living environment. Int. J. Environ. Res. Public Health 16:406. doi: 10.3390/ijerph16030406
Khalaila, R., and Vitman-Schorr, A. (2018). Internet use, social networks, loneliness, and quality of life among adults aged 50 and older: mediating and moderating effects. Qual. Life Res. 27, 479–489. doi: 10.1007/s11136-017-1749-4
Kolarcik, P., Cepova, E., Madarasova Geckova, A., Elsworth, G. R., Batterham, R. W., and Osborne, R. H. (2017). Structural properties and psychometric improvements of the Health literacy questionnaire in a Slovak population. Int. J. Public Health 62, 591–604. doi: 10.1007/s00038-017-0945-x
Kurina, L. M., Knutson, K. L., Hawkley, L. C., Cacioppo, J. T., Lauderdale, D. S., and Ober, C. (2011). Loneliness is associated with sleep fragmentation in a communal society. Sleep 34, 1519–1526. doi: 10.5665/sleep.1390
Lasgaard, M., Friis, K., and Shevlin, M. (2016). “where are all the lonely people?” a population-based study of high-risk groups across the life span. Soc. Psychiatry Psychiatr. Epidemiol. 51, 1373–1384. doi: 10.1007/s00127-016-1279-3
Lim, M. H., Eres, R., and Peck, C. (2019). The young Australian loneliness survey: Understanding loneliness in adolescents and young adults: Swinburne University of Technology VicHealth. Available at: https://www.vichealth.vic.gov.au/-/media/ResourceCentre/PublicationsandResources/Social-connection/The-young-Australian-loneliness-survey- (Accessed January 20, 2022).
Lim, M. H., Eres, R., and Vasan, S. (2020). Understanding loneliness in the twenty-first century: an update on correlates, risk factors, and potential solutions. Soc. Psychiatry Psychiatr. Epidemiol. 55, 793–810. doi: 10.1007/s00127-020-01889-7
Lim, M. H., Gleeson, J. F., Alvarez-Jimenez, M., and Penn, D. L. (2018). Loneliness in psychosis: a systematic review. Soc. Psychiatry Psychiatr. Epidemiol. 53, 221–238. doi: 10.1007/s00127-018-1482-5
Lim, M. H., Holt-Lunstad, J., and Badcock, J. C. (2020). Loneliness: contemporary insights into causes, correlates, and consequences. Soc. Psychiatry Psychiatr. Epidemiol. 55, 789–791. doi: 10.1007/s00127-020-01891-z
Lim, M. H., Rodebaugh, T. L., Zyphur, M. J., and Gleeson, J. F. (2016). Loneliness over time: the crucial role of social anxiety. J. Abnorm. Psychol. 125, 620–630. doi: 10.1037/abn0000162
Lubben, J. E. (1998). Assessing social networks among elderly populations. Fam. Community Health 11, 42–52. doi: 10.1097/00003727-198811000-00008
Lucas, J. W. (2003). Theory-testing, generalization, and the problem of external validity. Soc. Theory 21, 236–253. doi: 10.1111/1467-9558.00187
Luo, Y., and Waite, L. J. (2014). Loneliness and mortality among older adults in China. J. Gerontol. B Psychol. Sci. Soc. Sci. 69, 633–645. doi: 10.1093/geronb/gbu007
Maes, M., Nelemans, S. A., Danneel, S., Fernández-Castilla, B., Van den Noortgate, W., Goossens, L., et al. (2019). Loneliness and social anxiety across childhood and adolescence: multilevel meta-analyses of cross-sectional and longitudinal associations. Dev. Psychol. 55, 1548–1565. doi: 10.1037/dev0000719
Marvanova, M., Roumie, C. L., Eden, S. K., Cawthon, C., Schnipper, J. L., and Kripalani, S. (2011). Health literacy and medication understanding among hospitalized adults. J. Hosp. Med. 6, 488–493. doi: 10.1002/jhm.925
Marziali, M. E., Armstrong, H. L., Closson, K., McLinden, T., Wang, L., Barath, J., et al. (2020). Loneliness and self-rated physical health among gay, bisexual and other men who have sex with men in Vancouver, Canada. J. Epidemiol. Community Health 74, 553–559. doi: 10.1136/jech-2019-213566
McKee, G., Kearney, P. M., and Kenny, R. A. (2015). The factors associated with self-reported physical activity in older adults living in the community. Age Ageing 44, 586–592. doi: 10.1093/ageing/afv042
McTavish, D. G., and Loether, H. J. (2002). Social Research: An Evolving Process. Boston: Allyn and Bacon.
Miller, T. A. (2016). Health literacy and adherence to medical treatment in chronic and acute illness: a meta-analysis. Patient Educ. Couns. 99, 1079–1086. doi: 10.1016/j.pec.2016.01.020
Mitchell, S. E., Sadikova, E., Jack, B. W., and Paasche-Orlow, M. K. (2012). Health literacy and 30-day post discharge hospital utilization. J. Health Commun. 17, 325–338. doi: 10.1080/10810730.2012.715233
Morin, C. M., Belleville, G., Belanger, L., and Ivers, H. (2011). The insomnia severity index: psychometric indicators to detect insomnia cases and evaluate treatment response. Sleep 34, 601–608. doi: 10.1093/sleep/34.5.601
Negosanu, C., and Reid, T. (2021). Loneliness in times of COVID-19 - prevalence, severity and correlates of loneliness with anxiety and depression in younger populations during the novel coronavirus pandemic - a systematic review and meta-analysis. [Prepint]. Available at: https://www.researchgate.net/publication/355175185_Loneliness_in_Times_of_COVID-19_ (Accessed January 20, 2022).
Nutbeam, D. (1998). Health Promotion Glossary. Health Promot. Int. 13, 349–364. doi: 10.1093/heapro/13.4.349
Ong, A. D., Uchino, B. N., and Wethington, E. (2016). Loneliness and health in older adults: a mini-review and synthesis. Gerontology 62, 443–449. doi: 10.1159/000441651
O’Reilly, S. L., and McCann, L. R. (2012). Development and validation of the diet quality tool for use in cardiovascular disease prevention settings. Aust J prim. Health 18, 138–147. doi: 10.1071/py11005
Osborne, R. H., Batterham, R. W., Elsworth, G. R., Hawkins, M., and Buchbinder, R. (2013). The grounded psychometric development and initial validation of the Health literacy questionnaire (HLQ). BMC Public Health 13:658. doi: 10.1186/1471-2458-13-658
Peplau, L. A. (1982). “Perlman D perspective on loneliness” in Loneliness: A Sourcebook of Current Theory, Research and Therapy. eds. L. A. Peplau and D. Perlman (New York: Wiley), 1–18.
Pinquart, M., and Sorensen, S. (2001). Influences on loneliness in older adults: a meta-analysis. Basic Appl. Soc. Psych. 23, 245–266. doi: 10.1207/s15324834basp2304_2
Pyle, E., and Evans, D.. (2018). Loneliness-What Characteristics and Circumstances are Associated with Feeling Lonely. Newport: Office for National Statistics.
Radloff, L. S. (1977). The CES-D scale: a self-report depression scale for research in the general population. Appl. Psychol. Meas. 1, 385–401. doi: 10.1177/014662167700100306
Richard, A., Rohrmann, S., Vandeleur, C. L., Schmid, M., Barth, J., and Eichholzer, M. (2017). Loneliness is adversely associated with physical and mental health and lifestyle factors: results from a Swiss national survey. PLoS One 12:e0181442. doi: 10.1371/journal.pone.0181442
Richtering, S. S., Morris, R., Soh, S. E., Barker, A., Bampi, F., Neubeck, L., et al. (2017). Examination of an eHealth literacy scale and a health literacy scale in a population with moderate to high cardiovascular risk: Rasch analyses. PLoS One 12:e0175372. doi: 10.1371/journal.pone.0175372
Rodebaugh, T. L., Woods, C. M., and Heimberg, R. G. (2007). The reverse of social anxiety is not always the opposite: the reverse-scored items of the social interaction anxiety scale do not belong. Behav. Ther. 38, 192–206. doi: 10.1016/j.beth.2006.08.001
Routasalo, P., and Pitkala, K. H. (2003). Loneliness among older people. Rev. Clin. Gerontol. 13, 303–311. doi: 10.1017/s095925980400111x
Russell, D. W. (1996). UCLA loneliness scale (version 3): reliability, validity, and factor structure. J. Pers. Assess. 66, 20–40. doi: 10.1207/s15327752jpa6601_2
Schat, A. C., Kelloway, E. K., and Desmarais, S. (2005). The physical Health questionnaire (PHQ): construct validation of a self-report scale of somatic symptoms. J. Occup. Health Psychol. 10, 363–381. doi: 10.1037/1076-8998.10.4.363
Schmidt, S., Mühlan, H., and Power, M. (2005). The EUROHIS-QOL 8-item index: psychometric results of a cross-cultural field study. Eur. J. Pub. Health 16, 420–428. doi: 10.1093/eurpub/cki155
Shankar, A. (2020). Loneliness and sleep in older adults. Soc. Psychiatry Psychiatr. Epidemiol. 55, 269–272. doi: 10.1007/s00127-019-01805-8
Shankar, A., Hamer, M., McMunn, A., and Steptoe, A. (2013). Social isolation and loneliness: relationships with cognitive function during 4 years of follow-up in the English longitudinal study of ageing. Psychosom. Med. 75, 161–170. doi: 10.1097/psy.0b013e31827f09cd
Spence, J. T., Helmreich, R. L., and Pred, R. S. (1987). Impatience versus achievement strivings in the type a pattern: differential effects on students’ health and academic achievement. J. Appl. Psychol. 72, 522–528. doi: 10.1037/0021-9010.72.4.522
Stickley, A., and Koyanagi, A. (2016). Loneliness, common mental disorders and suicidal behavior: findings from a general population survey. J. Affect. Disord. 197, 81–87. doi: 10.1016/j.jad.2016.02.054
Stickley, A., Koyanagi, A., Koposov, R., Blatny, M., Hrdlicka, M., Schwab-Stone, M., et al. (2016). Loneliness and its association with psychological and somatic health problems among Czech, Russian and U.S. adolescents. BMC Psychiatry 16:128. doi: 10.1186/s12888-016-0829-2
Sündermann, O., Onwumere, J., Kane, F., Morgan, C., and Kuipers, E. (2014). Social networks and support in first-episode psychosis: exploring the role of loneliness and anxiety. Soc. Psychiatry Psychiatr. Epidemiol. 49, 359–366. doi: 10.1007/s00127-013-0754-3
Thurston, R. C., and Kubzansky, L. D. (2009). Women, Loneliness, and incident coronary heart disease. Psychosom. Med. 71:836. doi: 10.1097/psy.0b013e3181b40efc
Trémeau, F., Antonius, D., Malaspina, D., Goff, D. C., and Javitt, D. C. (2016). Loneliness in schizophrenia and its possible correlates. An exploratory study. Psychiatry Res. 246, 211–217. doi: 10.1016/j.psychres.2016.09.043
Varga, T. V., Bu, F., Dissing, A. S., Elsenburg, L. K., Bustamante, J. J. H., Matta, J., et al. (2021). Loneliness, worries, anxiety, and precautionary behaviours in response to the COVID-19 pandemic: a longitudinal analysis of 200,000 Western and northern Europeans. Lancet Reg. Health Eur. 2:100020. doi: 10.1016/j.lanepe.2020.100020
Vasan, S., Lambert, E., Eikelis, N., and Lim, M. H. (2022). Impact of loneliness on health-related factors in Australia during the COVID-19 pandemic: a retrospective study. Health Soc. Care Community 30, e5293–e5304. doi: 10.1111/hsc.13948
Warttig, S. L., Forshaw, M. J., South, J., and White, A. K. (2013). New, normative, English-sample data for the short form perceived stress scale (PSS-4). J. Health Psychol. 18, 1617–1628. doi: 10.1177/1359105313508346
Watson, D., Clark, L. A., and Tellegen, A. (1988). Development and validation of brief measures of positive and negative affect: the PANAS scales. J. Pers. Soc. Psychol. 54, 1063–1070. doi: 10.1037/0022-3514.54.6.1063
Keywords: loneliness, health-related factors, health literacy, social isolation, young adults
Citation: Vasan S, Eikelis N, Lim MH and Lambert E (2023) Evaluating the impact of loneliness and social isolation on health literacy and health-related factors in young adults. Front. Psychol. 14:996611. doi: 10.3389/fpsyg.2023.996611
Edited by:
Lukasz Mokros, Medical University of Lodz, PolandReviewed by:
Carlo Lazzari, South West Yorkshire Partnership NHS Foundation Trust, United KingdomGianluca Serafini, Department of Neuroscience, San Martino Hospital (IRCCS), Italy
Marjan Mardani-Hamooleh, Iran University of Medical Sciences, Iran
Copyright © 2023 Vasan, Eikelis, Lim and Lambert. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Shradha Vasan, ✉ svasan@swin.edu.au
 Shradha Vasan
Shradha Vasan Nina Eikelis
Nina Eikelis Michelle H. Lim
Michelle H. Lim Elisabeth Lambert
Elisabeth Lambert