Corrigendum: Prevalence and Influencing Factors of Anxiety and Depression Symptoms in the First-Line Medical Staff Fighting Against COVID-19 in Gansu
- 1Department of Psychiatry, Lanzhou University Second Hospital, Lanzhou, China
- 2Department of Geriatric Psychiatry, Shanghai Mental Health Center, Shanghai Jiao Tong University School of Medicine, Shanghai, China
- 3Alzheimer's Disease and Related Disorders Center, Shanghai Jiao Tong University, Shanghai, China
Background: The outbreak of novel coronavirus pneumonia (COVID-19) has brought enormous physical and psychological pressure on Chinese medical staff. It is extremely important to understand the prevalence and influencing factors of anxiety and depression symptoms in first-line anti-epidemic medical staff and their coping styles for these negative emotions.
Methods: A cross-sectional survey was conducted in Gansu (China), with a questionnaire packet which consisted of the self-rating anxiety scale (SAS), self-rating depression scale (SDS), and the simplified coping style questionnaire (SCSQ). A total of 79 doctors and 86 nurses participated in the survey. Correlation analysis was performed to explore the relationship between SAS, SDS, and SCSQ score. A linear regression model was used to determine the influencing factors for anxiety or depression symptoms.
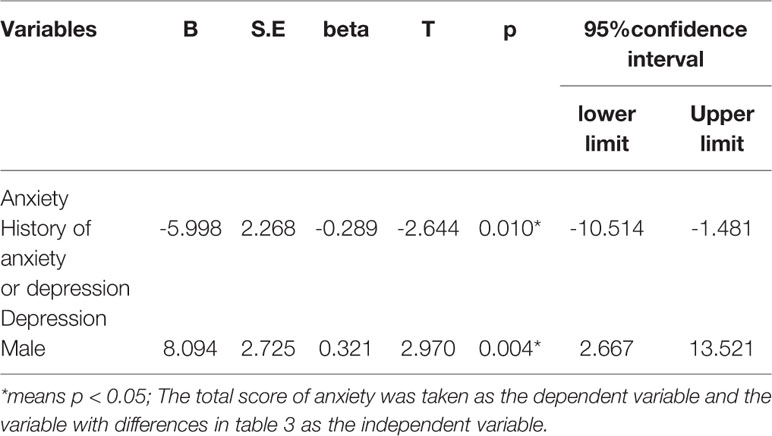
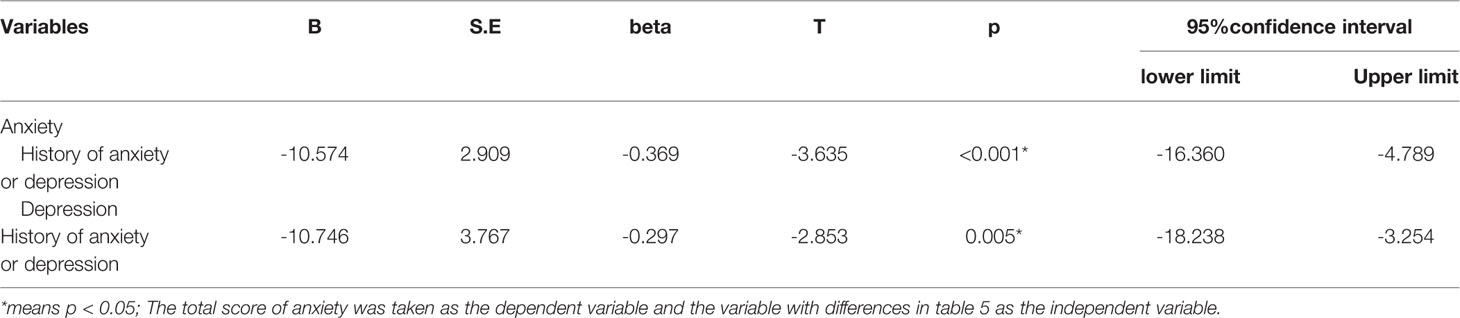
Results: The prevalence rates of anxiety and depression symptoms among doctors was 11.4% and 45.6%, respectively. History of depression or anxiety (T=-2.644, p= 0.010, 95%CI: -10.514~-1.481) was shown to be a risk factor for anxiety symptoms in doctors, while being male (T=2.970, p=0.004, 95%CI: 2.667~13.521) was a protective factor for depression. The prevalence rate of anxiety and depression symptoms among nurses was 27.9% and 43.0%, respectively. History of depression or anxiety was a common risk factor for anxiety symptoms (T=-3.635, p=0.000, 95%CI: -16.360~-4.789) and depression symptoms (T=-2.835, p=0.005, 95%CI:-18.238~-3.254) in nurses. The results of partial correlation analysis (controlled for gender and history of depression or anxiety) indicated that the total score of positive coping was negatively correlated with the total score of anxiety (r=-0.182, p=0.002) and depression (r=-0.253, p=0.001).
Conclusions: The first-line anti-epidemic medical staff have high anxiety and depression symptoms and adopting positive coping styles will help to improve their negative emotions.
Introduction
Since mid-December of 2019, coronavirus disease 2019 (COVID-19) has been identified in many countries (1). As of February 24th, 41600 medical staff in China have been fighting in the front line of the anti-epidemic campaign. Of these medical staff, 3387 of them were infected with the novel coronavirus pneumonia, accounting for 4% of all confirmed cases, while 22 died and accounted for 0.8% of the deaths. The front-line medical staff will not only bear the work pressure of overload, but also face the huge risk of infection (2). Stress represents the main environmental risk factor for psychiatric illnesses, and in a long-term stress state, people can be more prone to depression or other mental disease (3), which will also increase the risk of infection (4–6). Therefore, it is necessary to investigate the psychological state of the first-line anti-epidemic medical staff and give them necessary psychological interventions if they have anxiety or depression.
Materials and Methods
Participants
This cross-sectional study was conducted between February 1, 2020 and February 29, 2020. The research objects were the first line medical staff in the designated hospitals and fever clinics of novel coronavirus pneumonia in Gansu Province. The inclusion criteria were as follows: 1) 18 years or older; 2) doctor or nurse; 3) first-line to COVID-19; 4) without serious mental illness, such as schizophrenia or an intellectual disability; 5) without physical disease affecting anxiety or depression, such as hypothyroidism or coronary heart disease; and 6) willing to be investigated. Exclusion criteria were as follows: 1) less than 18 years old, 2) non-frontline medical or administrative staff, 3) not in Gansu, 4) serious mental illness or a combination of disorders that may affect anxiety or depression, and 5) refused to be investigated. Finally, 165 front-line medical staff working in Gansu were enrolled in the study.
Ethical approval was issued by the Ethics Committee of the Second Clinical Medical College of Lanzhou University, and all the participants had signed an informed consent before the study was initiated.
Investigation Tools
By using the self-designed questionnaire, we have obtained the general demographic information of the respondents, including gender, age, marriage, occupation, education level, specialty, level of worry, and level of expectation.
Neuropsychological Tests
The self-rating anxiety scale (SAS) (7) and self-rating depression scale (SDS) (8) were used to assess anxiety and depression symptoms of medical staff respectively. Both SAS and SDS are 20-item Likert and norm-referenced scales, in which items tap physiological and psychological symptoms and are rated by participants according to how each applied to them within the past week, using a 4-point scale ranging from 1 (none, or a little of the time) to 4 (most, or all of the time) (9). The choice of SAS items is based on diagnostic criteria listed in the major American psychiatry literature, whereas the SDS taps depressive symptoms based on factor analytic studies of depression symptoms (9). The Zung Self-Rating Anxiety/Depression Scale (SAS/SDS) has been widely applied in clinical institutions and scientific research, showing convincing results and a remarkable degree of consensus among clinicians (10). According to the conclusion of other studies (11), we also utilized the standard score of 50 as the critical value to divide depression or anxiety in the present study. The Simplified Coping Style Questionnaire (SCSQ) (12) is a 20-item self-report scale that includes two dimensions. The first entry consists of 1–12 items and reflects the traits of passive coping and active coping (8-item). The second entry consists of 13–20 questions, reflecting the traits of passive coping. This instrument has been commonly used in China and has proven to be highly reliable and valid (13).
Investigation Way
In the current study, we used the Electronic “Questionnaire Star” Questionnaire as the survey tool, and information was collected through friend circle forwarding and WeChat group promotion. “Questionnaire Star” is a professional online survey platform, which can be used for questionnaire surveys, evaluation, voting, and other purposes. Compared with traditional survey methods, “Questionnaire Star” has the obvious advantages of being fast, low cost, easy to learn, and easy to use (14).
Statistical Analysis
The categorical variables were expressed as the frequency (%), while the continuous variables were presented as mean± SD. A single sample Kolmogorov-Smirnov test was used to test whether the data conform to normal distribution. Chi square test was used to compare categorical variables, while independent sample t-test and Mann-whitney U test were respectively used to compare the continuous variables with and without normal distribution. The prevalence of anxiety and depression symptoms was calculated by splitting the total number of cases diagnosed by the total number of participants. The influence factors of anxiety or depression were analyzed by linear regression analysis. Partial correlation analysis was used to analyze the correlation between SCSQ and SDS/SAS. The statistical analysis was performed by using SPSS version 22.0 and a p-value < 0.05 was regarded as significant.
Results
General Demographic Data of Frontline Medical Staff
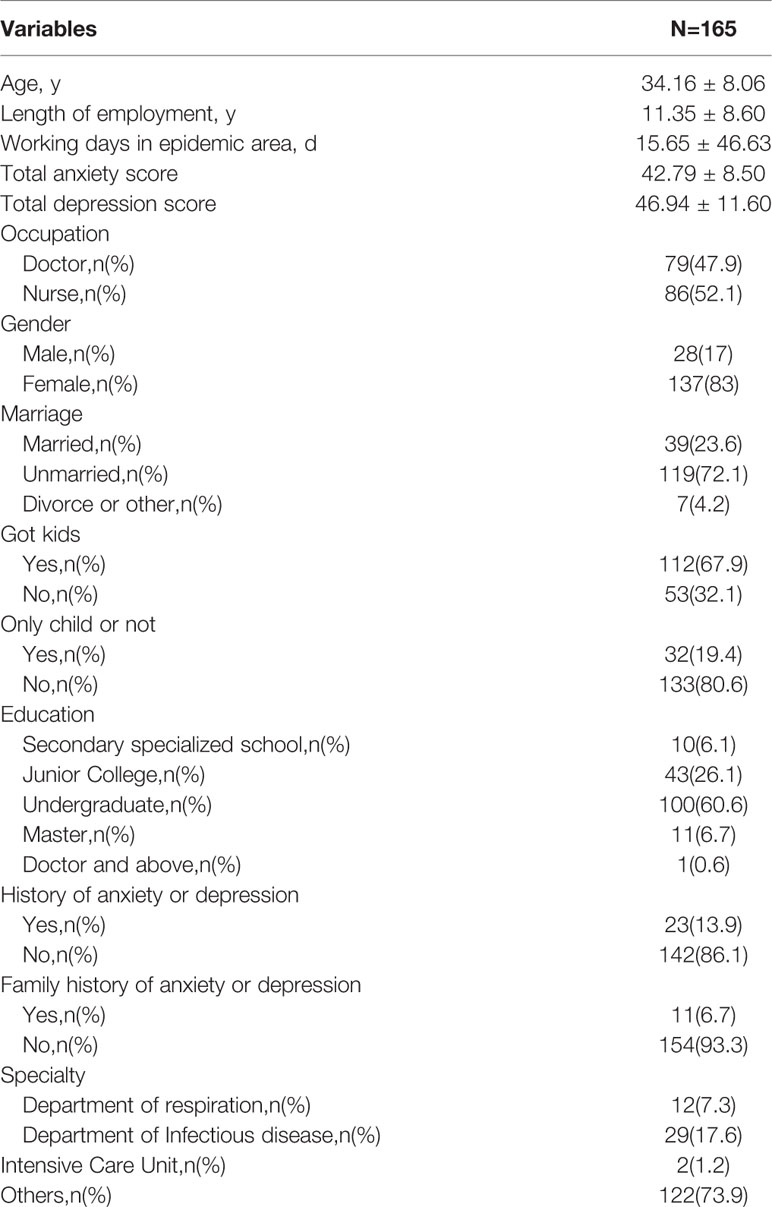
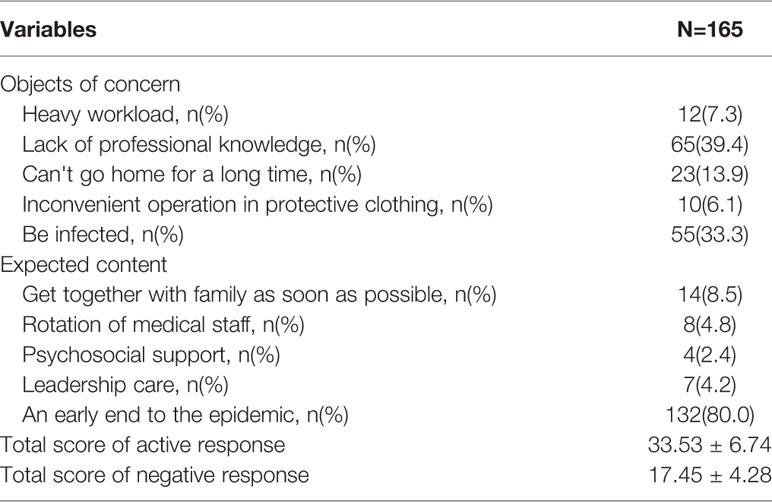
Through the online survey from Questionnaire Stars, we finally received 165 qualified questionnaires, and the recovery rate of the questionnaire was 100%. The average age of the respondents was 34.16 ± 8.06 (years), the average length of employment was 11.35 ± 8.60 (years), the average working day on the fever clinic or isolation ward was 15.65 ± 46.63 (days), the average anxiety score was 42.79 ± 8.50, and the average depression score was 46.94 ± 11.60. Tables 1 and 2 show the results.
Prevalence and Influencing Factors of Anxiety and Depression Symptoms (Doctors)
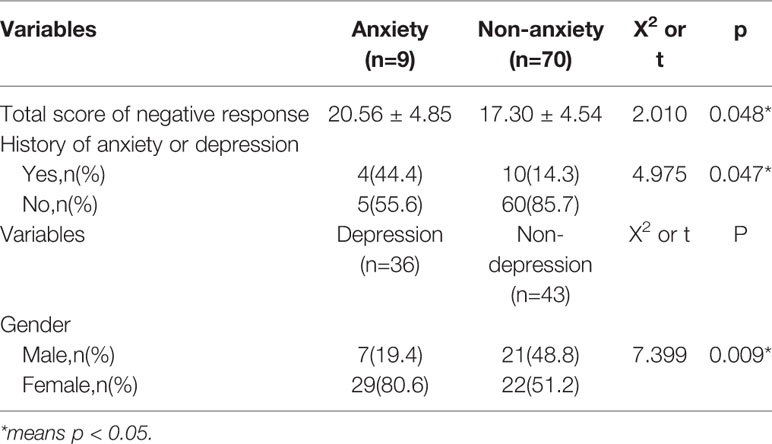
With 50 points as the critical value (both for SAS and SDS), nine people were considered to have anxiety symptoms, with a prevalence of 11.4% (9/79), and 36 people were considered to have depression symptoms, with a prevalence of 45.6% (36/79). There were statistical differences (p < 0.05) in the total score of negative responses and a history of anxiety or depression between the anxiety group and non -anxiety group, while there were statistical differences (p < 0.05) in gender between the depression group and non –depression group. Table 3 presents the results.
Then, by using linear regression analysis, we found that history of depression or anxiety (T=-2.644, p= 0.010, 95%CI: -10.514~-1.481) was a risk factor for anxiety symptoms in doctors, while being male (T=2.970, p=0.004, 95%CI: 2.667~13.521) was a protective factor for depression. Table 5 lists the results.
Prevalence and Influencing Factors of Anxiety and Depression Symptoms (Nurses)
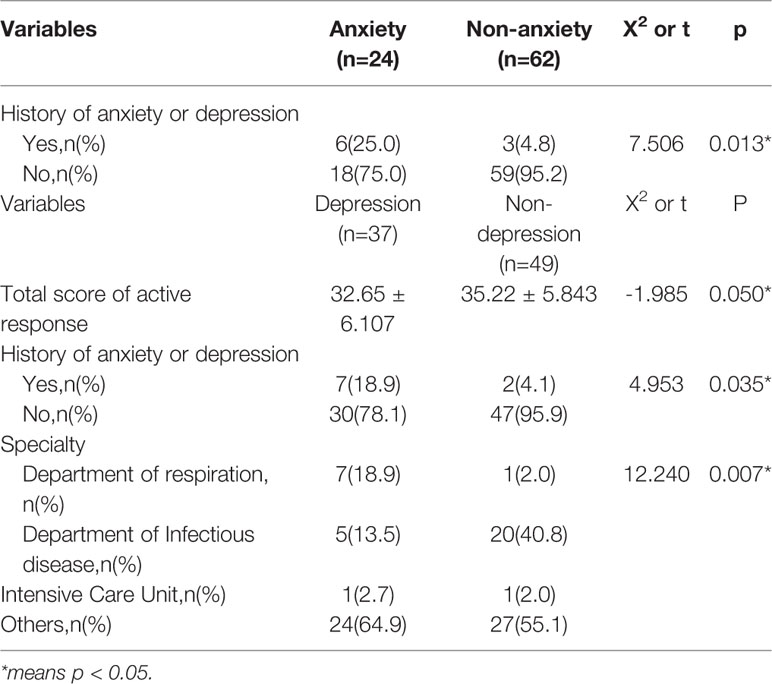
With 50 points as the critical value (both for SAS and SDS), 24 people were considered to have anxiety symptoms, with a prevalence of 27.9% (24/86), and 37 people were considered to have depression symptoms, with a prevalence of 43.0% (37/86). There were statistical differences (p < 0.05) in the history of anxiety or depression between the anxiety group and non -anxiety group, while there were statistical differences (p < 0.05) in the total scores of active response, history of anxiety or depression, and specialty between the depression group and non–depression group. Table 4 lists the results.
Then, by using linear regression analysis, we found that a history of depression or anxiety was a common risk factor for anxiety symptoms (T=-3.635, p=0.000, 95%CI: -16.360~-4.789) and depression symptoms (T=-2.835, p=0.005, 95%CI:-18.238~-3.254) in nurses. Table 6 lists the results.
The Relationship Between Coping Styles and Anxiety and Depression
The results of partial correlation analysis (controlled for gender and history of depression or anxiety) indicated that the total score of positive coping was negatively correlated with the total score of anxiety (r=-0.182, p=0.002) and depression (r=-0.253, p=0.001)
Discussion
In the current study, we investigated the prevalence and influencing factors of anxiety and depression symptoms in the first-line medical staff fighting against novel coronavirus pneumonia in Gansu, and came to some interesting conclusions: 1) the prevalence rate of anxiety and depression symptoms among doctors was 11.4% and 45.6%, respectively; 2) the prevalence rate of anxiety and depression symptoms among nurses was 27.9% and 43.0%, respectively; 3) a history of depression or anxiety (T=-2.644, p= 0.010, 95%CI: -10.514~-1.481) was a risk factor for anxiety symptoms in doctors, while being male (T=2.970, p=0.004, 95%CI: 2.667~13.521) was a protective factor for depression; 4) a history of depression or anxiety was a common risk factor for anxiety symptoms (T=-3.635, p=0.000, 95%CI: -16.360~-4.789) and depression symptoms (T=-2.835, p=0.005, 95%CI:-18.238~-3.254) in nurses; 5) the results of partial correlation (controlled for gender and history of depression or anxiety) indicated that the total score of positive coping was negatively correlated with the total score of anxiety (r=-0.182, p=0.002) and depression (r=-0.253, p=0.001).
Previous studies had suggested that the mental health status of medical staff was worse than in the general population (15, 16). For example, Kerrien M et al. (17) found that 27% of junior doctors were suffering from depression, while 28.7% were suffering from anxiety. Paiva CE et al. (18) found that 12.3%of doctors had depression (HADS-D ≥ 11), and 19.4% had anxiety (HADS-A ≥ 11). A systematic review of 29 studies showed that the prevalence of anxiety and depression among students in medical schools in Europe, the UK, and elsewhere in the English-speaking world outside of North America was 7.7-65.5% and 6.0-66.5%, respectively (19). Similarly, a cross-sectional survey showed that the prevalence of anxiety symptoms in nurses was 43.4% (20). Another cross-sectional survey indicated that the prevalence rate of anxiety among female nurses was 41.1% (21). Maharaj S et al. (22) found that the prevalence rates of depression and anxiety among Australian nurses were 32.4% and 41.2%, respectively. So, our conclusions were not consistent, and this difference might come from the use of different investigation tools. Interestingly, we found that the anxiety level (X2 = 7.019. p=0.011) of nurses was significantly higher than that of doctors, but there was no difference in depression (X2 = 0.108. p=0.756) between the two groups. So we need to pay more attention to nurses in order to relieve their anxiety.
In the present study, we found that being male (T=2.970, p=0.004, 95%CI: 2.667~13.521) was a protective factor for depression in doctors. There is considerable discourse surrounding the disproportionate diagnosis of men with depression as compared to women, often times cited at a rate around 1:2 (23). However, the view that depression rates are universally higher in women is challenged, as biological determinants, sex role changes, and social factors might also contribute to this difference (24). What's more, meta-analyses of diagnoses and symptoms show that the gender difference peaks in adolescence but then will decline and remain stable in adulthood, and cross-national analyses also indicate that larger gender differences are found in nations with greater gender equity for major depression, but not depression symptoms (25). But beyond that, a systematic review of nineteen studies indicates that the male gender is significantly associated with suicide in individuals with depression (26). So, the relationship between gender and depressive symptoms needs to be verified by a large-scale longitudinal study.
We also found that a history of anxiety or depression was a risk factor for anxiety symptoms in doctors, and a common risk factor for anxiety and depression symptoms in nurses. Osasona SO et al. (27) found that previous mental illness was significantly associated with anxiety, depression, or general psychiatric morbidity in a sample of inmates in a Nigerian prison. Ahmed A et al. (28) found that a history of depression and stress was associated with depressive and anxiety symptoms in a sample of 615 women in Saskatchewan from pregnancy to 5 years postpartum. Stafford L et al. (29) found that women with a psychiatric history and high neuroticism are at the greatest risk for future morbidity after adjusting for confounders, such as age, education, and living alone. Therefore, our conclusions are consistent.
By using partial correlation analysis (controlled for gender and history of depression or anxiety), we finally found that a positive coping style was a protective factor for anxiety(r=-0.182, p=0.002) and depression (r=-0.253, p=0.001), suggesting that a positive coping style was helpful in resisting negative emotions. Mahmoud JS et al. (30) found that reducing maladaptive coping behaviors might have the most positive impact on reducing anxiety, depression, and stress in young adult college students. Wang Y et al. (31) found that perceived stress had some positive effects on psychological distress, and coping style might be a mediator in this relationship among Chinese physicians. In addition, Holz NE et al. (32) pointed out that stress exposure would increase rates of depression and anxiety in adults, particularly in females, and had been associated with maladaptive changes in the anterior cingulate cortex (ACC), while positive coping styles could help to increase the ACC volume. So our conclusions were consistent.
We have to admit that our research has certain limitations. First, it was just a cross-sectional study that could not establish a causal link. Second, the sample size used was relatively small and therefore reduced the reliability of the study. Third, we used the self-assessment scale to evaluate the depression and anxiety symptoms of the medical staff, which might have a certain result deviation.
Conclusions
The first-line anti-epidemic medical staff have high anxiety and depression symptoms, and adopting a positive coping style will help to improve their negative emotions.
Data Availability Statement
The datasets analyzed in this article are not publicly available because the datasets are part of an unpublished database and the database is still being used for other manuscripts in preparation. Requests to access the datasets should be directed to 156892477@qq.com.
Ethics Statement
The studies involving human participants were reviewed and approved by the Ethics Committee of the Second Clinical Medical College of Lanzhou University. The patients/participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author Contributions
WL and LS contributed to the study concept and design. JZ acquired the data. LZ, HW, and AF collected the data. SX and BY analyzed the data and drafted the manuscript. All authors read and approved the final manuscript.
Funding
This work was supported by grants from the China Ministry of Science and Technology (2009BAI77B03), National Natural Science Foundation of China (number 81671402), Clinical research center project of Shanghai Mental Health Center (CRC2017ZD02), the National Key R&D program of China (2017YFC1310501500), the Cultivation of Multidisciplinary interdisciplinary Project in Shanghai Jiaotong University (YG2019QNA10), and curriculum reform of Medical College of Shanghai Jiaotong University.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. World Health Organization. WHO Director-Generals Remarks at the Media Briefing on COVID-19 Outbreak on 18 February 2020 (2020). Available online at: https://www.who.int/director-general/speeches/detail/who-director-general-s-remarks-at-the-media-briefing-on-covid-19-outbreak-on-18-february-2020 (accessed February 20, 2020).
2. Xu K, Lai XQ, Liu Z. Suggestions for prevention of 2019 novel coronavirus infection in otolaryngology head and neck surgery medical staff. Zhonghua er bi yan hou tou jing wai ke za zhi = Chin J Otorhinolaryngol Head Neck Surgery (2020) 55(0):E001. doi: 10.3760/cma.j.issn.1673-0860.2020.0001
3. Cattaneo A, Riva MA. Stress-induced mechanisms in mental illness: A role for glucocorticoid signalling. J Steroid Biochem Mol Biol (2016) 160:169–74. doi: 10.1016/j.jsbmb.2015.07.021
4. Liao YT, Hsieh MH, Yang YH, Wang YC, Tsai CS, Chen VC, et al. Association between depression and enterovirus infection: A nationwide population-based cohort study. Medicine. (2017) 96(5):e5983. doi: 10.1097/MD.0000000000005983
5. Askim A, Gustad LT, Paulsen J, Reitan SK, Mehl A, Mohus RM, et al. Anxiety and Depression Symptoms in a General Population and Future Risk of Bloodstream Infection: The HUNT Study. Psychosom Med (2018) 80(7):673–9. doi: 10.1097/PSY.0000000000000619
6. Nayeri Chegeni T, Sharif M, Sarvi S, Moosazadeh M, Montazeri M, Aghayan SA, et al. Is there any association between Toxoplasma gondii infection and depression? A Syst Rev Meta-analysis (2019) 14(6):e0218524. doi: 10.1371/journal.pone.0218524
7. Zung WW. A rating instrument for anxiety disorders. Psychosomatics. (1971) 12(6):371–9. doi: 10.1016/S0033-3182(71)71479-0
8. Zung WW. A Self-Rating Depression Scale. Arch Gen Psychiatry (1965) 12:63–70. doi: 10.1001/archpsyc.1965.01720310065008
9. Dunstan DA, Scott N, Todd AK. Screening for anxiety and depression: reassessing the utility of the Zung scales. BMC Psychiatry (2017) 17(1):329. doi: 10.1186/s12888-017-1489-6
10. Yue T, Li Q, Wang R, Liu Z, Guo M, Bai F, et al. Comparison of Hospital Anxiety and Depression Scale (HADS) and Zung Self-Rating Anxiety/Depression Scale (SAS/SDS) in Evaluating Anxiety and Depression in Patients with Psoriatic Arthritis. Dermatol (Basel Switzerland). (2019) 21:1–9. doi: 10.1159/000498848
11. Chen Y, Zeng Y. [Correlation of depression and anxiety with social support and quality of life in patients with chronic wounds]. Zhong nan da xue xue bao Yi xue ban = J Cent South University. Med Sci (2018) 43(9):1032–6. doi: 10.11817/j.issn.1672-7347.2018.09.016
12. Li X, Guan L, Chang H, Zhang B. Core self-evaluation and burnout among Nurses: the mediating role of coping styles. PloS One (2014) 9(12):e115799. doi: 10.1371/journal.pone.0115799
13. Chen L, Liu J, Yang H, Ma H, Wang H, Huang Y, et al. Work-family conflict and job burn-out among Chinese doctors: the mediating role of coping styles. Gen Psychiatry (2018) 31(1):e000004. doi: 10.1136/gpsych-2018-000004
14. Li H-Y, Zhang Y, Li Y-J, Wang Z. Application and practice of “questionnaire star” in C language flipped classroom teaching. Heilongjiang Sci (2019) 10(9):22–3.
15. Nukui H, Murakami M, Midorikawa S, Suenaga M, Rokkaku Y, Yabe H, et al. Mental Health and Related Factors of Hospital Nurses. Asia-Pacific J Public Health (2017) 29(9)(2_suppl):161s–70s. doi: 10.1177/1010539516682589
16. Zhou C, Shi L, Gao L, Liu W, Chen Z, Tong X, et al. Determinate factors of mental health status in Chinese medical staff: A cross-sectional study. Medicine (2018) 97(10):e0113. doi: 10.1097/MD.0000000000010113
17. Kerrien M, Pougnet R, Garlantezec R, Pougnet L, Le Galudec M, Loddé B, et al. Prevalence of anxiety disorders and depression among junior doctors and their links with their work. Presse Medicale (Paris France : 1983) (2015) 44(4 Pt 1):e84–91. doi: 10.1016/j.lpm.2014.06.042
18. Paiva CE, Martins BP, Paiva BSR. Doctor, are you healthy? A cross-sectional investigation of oncologist burnout, depression, and anxiety and an investigation of their associated factors. BMC Cancer (2018) 2618(1):1044. doi: 10.1186/s12885-018-4964-7
19. Hope V, Henderson M. Medical student depression, anxiety and distress outside North America: a systematic review. Med Educ (2014) 48(10):963–79. doi: 10.1111/medu.12512
20. Gao YQ, Pan BC, Sun W, Wu H, Wang JN, Wang L. Anxiety symptoms among Chinese nurses and the associated factors: a cross sectional study. BMC Psychiatry (2012) 12:141. doi: 10.1186/1471-244X-12-141
21. Zhou J, Yang Y, Qiu X, Yang X, Pan H, Ban B, et al. Serial multiple mediation of organizational commitment and job burnout in the relationship between psychological capital and anxiety in Chinese female nurses: A cross-sectional questionnaire survey. Int J Nurs Stud (2018) 83:75–82. doi: 10.1016/j.ijnurstu.2018.03.016
22. Maharaj S, Lees T. Prevalence and Risk Factors of Depression, Anxiety, and Stress in a Cohort of Australian Nurses. Int J Environ Res Public Health (2018) 16(1):61–71. doi: 10.3390/ijerph16010061
23. Neitzke AB. An Illness of Power: Gender and the Social Causes of Depression. Culture Med Psychiatry (2016) 40(1):59–73. doi: 10.1007/s11013-015-9466-3
24. Parker G, Brotchie H. Gender differences in depression. Int Rev Psychiatry (Abingdon England) (2010) 22(5):429–36. doi: 10.3109/09540261.2010.492391
25. Salk RH, Hyde JS, Abramson LY. Gender differences in depression in representative national samples: Meta-analyses of diagnoses and symptoms. Psychol Bull (2017) 143(8):783–822. doi: 10.1037/bul0000102
26. Hawton K, Casanas ICC, Haw C, Saunders K. Risk factors for suicide in individuals with depression: a systematic review. J Affect Disord (2013) 147(1-3):17–28. doi: 10.1016/j.jad.2013.01.004
27. Osasona SO, Koleoso ON. Prevalence and correlates of depression and anxiety disorder in a sample of inmates in a Nigerian prison. Int J Psychiatry Med (2015) 50(2):203–18. doi: 10.1177/0091217415605038
28. Ahmed A, Bowen A, Feng CX, Muhajarine N. Trajectories of maternal depressive and anxiety symptoms from pregnancy to five years postpartum and their prenatal predictors. BMC Pregnancy Childbirth (2019) 19(1):26. doi: 10.1186/s12884-019-2177-y
29. Stafford L, Judd F, Gibson P, Komiti A, Mann GB, Quinn M. Anxiety and depression symptoms in the 2 years following diagnosis of breast or gynaecologic cancer: prevalence, course and determinants of outcome. Support Care Cancer (2015) 23(8):2215–24. doi: 10.1007/s00520-014-2571-y
30. Mahmoud JS, Staten R, Hall LA, Lennie TA. The relationship among young adult college students' depression, anxiety, stress, demographics, life satisfaction, and coping styles. Issues Ment Health Nursing (2012) 33(3):149–56. doi: 10.3109/01612840.2011.632708
31. Wang Y, Wang P. Perceived stress and psychological distress among chinese physicians: The mediating role of coping style. Medicine. (2019) 98(23):e15950. doi: 10.1097/MD.0000000000015950
Keywords: COVID-19, anxiety, depression, medical staff, Chinese
Citation: Zhu J, Sun L, Zhang L, Wang H, Fan A, Yang B, Li W and Xiao S (2020) Prevalence and Influencing Factors of Anxiety and Depression Symptoms in the First-Line Medical Staff Fighting Against COVID-19 in Gansu. Front. Psychiatry 11:386. doi: 10.3389/fpsyt.2020.00386
Received: 05 March 2020; Accepted: 16 April 2020;
Published: 29 April 2020.
Edited by:
Suraj Bahadur Thapa, University of Oslo, NorwayReviewed by:
Gianfranco Spalletta, Santa Lucia Foundation (IRCCS), ItalyTetsu Tomita, Hirosaki University, Japan
Copyright © 2020 Zhu, Sun, Zhang, Wang, Fan, Yang, Li and Xiao. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Bin Yang, 156892477@qq.com; Wei Li, 822203867@qq.com; Shifu Xiao, xiaoshifu@msn.com
†These authors have contributed equally to this work
 Juhong Zhu1†
Juhong Zhu1† Lin Sun
Lin Sun Bin Yang
Bin Yang Wei Li
Wei Li Shifu Xiao
Shifu Xiao