The effect of health insurance coverage on antenatal care utilizations in Ethiopia: evidence from national survey
- 1School of Public Health, College of Health and Medical Sciences, Haramaya University, Harar, Ethiopia
- 2School of Medicine, College of Health and Medical Sciences, Haramaya University, Harar, Ethiopia
- 3Department of Public Health, Rift Valley University, Harar, Ethiopia
- 4Department of Public Health, Institute of Health Sciences, Wollega University, Nekemte, Ethiopia
Background: About three-fourths of maternal near-miss events and two-fifths of the risk of neonatal mortality can be reduced by having at least one antenatal visit. Several studies have identified potential factors related to maternal health seeking behavior. However, the association between health insurance membership and antenatal care utilization was not well investigated in Ethiopia. Therefore, this study was aimed at assessing the effect of health insurance coverage on antenatal care use in Ethiopia.
Methods: The study utilized data from the 2019 Ethiopia Mini Demographic and Health Survey (EMDHS). The analysis included a weighted sample of 3,919 women who gave birth in the last five years. A logistic regression model was employed to assess the association between antenatal care use and health insurance coverage and other covariates. The results were presented as adjusted odds ratios (AOR) at a 95% confidence interval (CI). Statistical significance was declared at a p-value <0.05 in all analyses.
Results: Antenatal care was used by 43% (95% CI: 41.46 to 44.56%) of Ethiopian women. Those with health insurance coverage had higher odds of antenatal care use than those without health insurance coverage. Women were 33% more likely to use antenatal care (ANC) if they were covered by health insurance. Age, Media access, marital status, education status, wealth index, and economic regions were also factors associated with antenatal care utilizations.
Conclusions: According to our findings, less than half of Ethiopian women had four or more antenatal care visits. Health insurance membership, respondent age, media access, marital status, education status, wealth index, and economic region were factors associated with antenatal care utilization. Improving health insurance, women's economic empowerment, and education coverage are critical determinants of antenatal care utilization.
Background
Antenatal care (ANC) can be defined as “the care provided by skilled health care professionals to pregnant women and adolescent girls in order to ensure the best health conditions for both mother and baby during pregnancy” (1). Globally, only 50% of pregnant women attended the World Health Organization (WHO) recommended minimum of four ANC visits to improve fetal and maternal health (2, 3).
Low and middle-income countries (LMIC) account for the majority (99%) of global maternal deaths. In particular, sub-Saharan Africa and Southern Asia regions bear a significant portion, contributing to over 80% of global maternal mortality (4). However, the prevalence of recommended antenatal care (ANC) utilization in these regions is low, ranging from 53.39% to 78.86% in East Africa and Southern region of Africa respectively (5).
In sub-Saharan African countries, utilizing at least one ANC visit reduces the risk of neonatal mortality by 39% (6), and a systematic review and meta-analysis found a significant effect of ANC on maternal near-miss events in Ethiopia; at least one ANC visit will avoid approximately 75% of maternal near-miss events (7).
According to a Sub-Saharan Africa study conducted from 2006 to 2018, Ethiopia had the lowest prevalence of recommended ANC utilization, at 31.88% (5). However, trends in antenatal care use (4+ ANC visits) in Ethiopia in the past 14 years showed an increment from 12% to 43%. The coverage (four or more ANC visits) has increased more than two-fold (19% to 43%) (8), since community based health insurance (CBHI) started in Ethiopia (9).
Factors affecting ANC utilizations are distance to services (10), media exposure, wealth index and availability of maternal health services (11), maternal education, women's employment, marital status, household income, cost, and pregnant women's history of obstetric complications (12, 13).
Membership to health insurance scheme also increases the odds of antenatal care utilizations (14, 15). The community-based health insurance program is widely accepted in resource limited settings as a strategy for improving healthcare utilization and health seeking behaviors and reducing out-of-pocket catastrophic payments (16) and a promising means to attain universal health coverage (17–19). In the Sustainable Development Goals (SDGs), progress on Universal Health Coverage (UHC) is tracked using two indicators: coverage of essential health services (SDG 3.8.1); and catastrophic health spending (and related indicators) (SDG 3.8.2) (20).
Universal health coverage (UHC) is a situation where every individual and all communities have unparalleled access to quality health services without suffering any form of financial hardship (21). The UHC is effective in reducing barriers to accessing essential primary care services, including antenatal care through removing financial constraints and ensuring availability, UHC enables women to seek early and regular antenatal care, leading to improved maternal and child health outcomes (10).
Several studies have identified potential factors associated with maternal health seeking behavior. However, the association between community-based health insurance coverage and antenatal care utilization was not well investigated in Ethiopia. Therefore, this study was aimed at assessing the effect of community-based health insurance coverage on antenatal care use in Ethiopia.
Methods
Data sources
The study utilized data from the most recent 2019 Ethiopia Mini Demographic and Health Surveys (EMDHS). The DHS is a nationwide survey collected every 5 years. The survey collects information on health and other population characteristics. The DHS employs a two-stage stratified sampling technique to collect nationally representative data from the respondents (22). At first stage sampling process begins with the selection of clusters, usually called enumeration areas (EAs). This is followed by the selection of households for the survey. The survey included a total of 8,865 participants (22). We extracted data for women who had given birth in the last five years. The analysis was conducted on a weighted sample of 3,919 women who had given birth in the last five years. Details about the DHS sampling techniques and sample size are available at http://www.dhsprogram.com/. The EMDHS research protocol complies with the National Health Research Ethics Committee and Institutional Review Board guidelines.
Variables
Outcome variable
The outcome variable was the number of ANC visits. The exact question in the DHS questionnaire was “how many times did you receive antenatal care during this pregnancy?” The answer was either a number or indicated they did not know. Less than four ANC visits were coded as “0” and four or more were coded as “1”. At least four ANC visits were the outcome of interest in this study.
In 2016, the WHO revised its recommendations to a minimum of eight ANC contacts, with the first contact scheduled to take place in the first trimester up to 12 weeks of gestation and subsequent contacts at 20, 26, 30, 34, 36, 38 and 40 weeks (1). However, until the end of 2021 Ethiopia hadn't implemented this new antenatal model. So, we have used the focused ANC care model which is at least 4 visits.
Explanatory variable
The main explanatory variable was community-based health insurance coverage. The question asked was “are you covered by community-based health insurance?” Respondents answered yes or no, and since this data is binary, no further coding was needed.
Covariates
Ten variables linked to various socio-economic and demographic indicators were added as covariates. These were economic regions (agrarians, city dwellers, and pastoralists), place of residence (urban, rural), wealth index (poorest, poorer, middle, richer, richest), family size (categorized as ≤5 members, >5 members), age of the respondent (recorded as continuous and we categorized as 15–24 years, 25–34 years, 35–49 years). Media access (no access, and has access), marital status (single, married, and widowed/separated), and education (no education, primary, and secondary and above) were covariates included in the analysis.
Statistical analysis
Extracted data were weighted so that the sample was representative of respondents in 2019 mini EDHS. Analyses were performed using STATA version 17.0. To assess the association between antenatal care use and CBHI coverage and other covariates, a logistic regression model was employed. First, each variable was entered into a bivariable logistic regression model. Second, variables which were significant at a p-value of less than or equals 0.25 were fitted into a multivariable logistic regression model to identify independent factors associated with antenatal care use in Ethiopia. Statistical significance was declared at a p-value < 0.05 in all analyses. The results from the logistic regression analyses are presented as adjusted odds ratios (OR) with 95% confidence intervals (CIs).
Result
Socio-demographic characteristics of study participants
About half (50.74%) of the participants were in the age group of 25–34 years. Majority (86.6%) of the participants' household were headed by male. Nearly three-fourths of the participants were from rural settings. More than half (51.27%) of the participants had no formal education (Table 1).
Community-based health insurance coverage and antenatal care by socio-demographic characteristics
Only 22.1% of women with female households and 31.5% of women with male household heads were enrolled in the CBHI. Only 26.8% of women from the poorest wealth index were enrolled in the CBHI, compared to 40.3% of those from the median wealth index. About three-fifths (58.8%) of urban residents utilized ANC compared to only 37.3 of rural residents. Majority (74.4%) 0f women with secondary and higher education utilized ANC compared to only 32.4% of women with no education (Table 2).
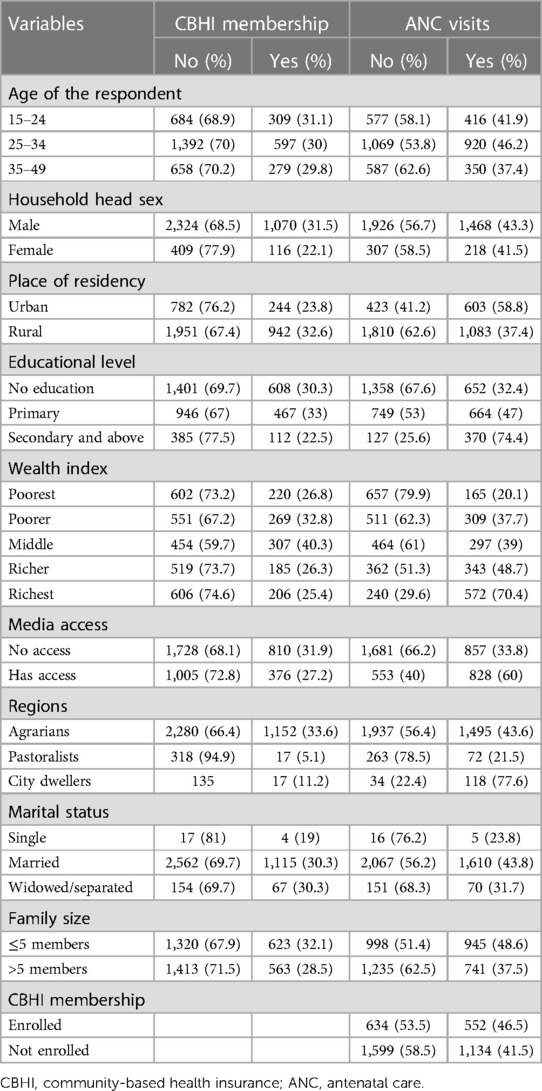
Table 2. Community-based health insurance coverage and antenatal care by socio-demographic characteristics.
The role of health insurance coverage on antenatal care utilizations
The antenatal care was utilized by 43% (95%CI: 41.46 to 44.56%) of Ethiopian women who had child birth in the last five years prior to the survey. Those with health insurance coverage had higher antenatal care than those without health insurance coverage (46.5% vs. 41.5%).
Factors associated with antenatal care
In multivariable logistic regressions insurance membership, respondent age, Media access, marital status, education status, wealth index, and economic regions were factors associated with antenatal care utilizations.
The odds of antenatal care utilizations were higher among health insurance members compared to those nonmembers (AOR = 1.33, 95%CI: 1.14, 1.54). The odds of antenatal care utilizations were higher among women in the age group of 25–34 and 35–49 years compared to women aged 15–24 years (25–34 years; AOR = 1.46, 95%CI: 1.22, 1.75, 35–49 years; AOR = 1.30, 95%CI: 1.03, 1.65). Respondents who had media access had 1.36 times higher odds of antenatal care compared to those who had no media access (AOR = 1.36; 95%CI: 1.15, 1.62). The odds of antenatal care utilizations were 5.22 times higher among married women compared to the single women (AOR = 5.22; 95%: 1.72, 15.86).
The odds of antenatal care utilizations were 1.48 and 3.16 times higher among women attended primary and secondary and above education respectively compared to those who had no formal education (primary, AOR = 1.48; 95%CI: 1.26, 1.75, secondary and above AOR = 3.16; 95%CI: 2.43, 4.12). The odds of antenatal care utilizations were higher among women from higher wealth index compared to those from poorest wealth index (poorer, AOR = 2.06; 95%CI: 1.64, 2.59, middle, AOR = 1.88; 95%CI: 1.49, 2.39, richer, AOR = 2.56; 95%CI: 1.99, 3.29, richest, AOR = 4.94; 95%CI: 3.59, 6.80).
The odds of antenatal care utilizations were higher among women from higher city economic regions residence compared to those from agrarians (AOR = 1.59, 95%CI: 1.03, 2.46). The study found that respondents who were from pastoralist regions had lower odds of utilizing antenatal care compared to those from agrarians (AOR = 0.61; 95%CI: 0.45, 0.83) (Table 3).
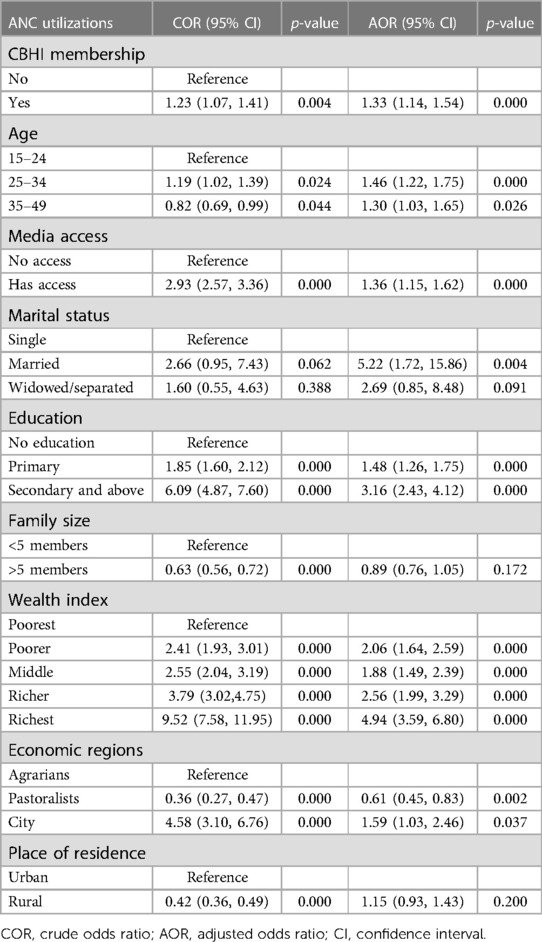
Table 3. Multivariable logistic regressions of factors associated with antenatal care utilizations in Ethiopia, 2019.
Discussion
In this study, we examined the relationship between community-based health insurance coverage and ANC utilization in Ethiopia using 2019 Ethiopia mini-DHS data. One in five of women with female household heads and 31.5% of women with male household heads were enrolled in the CBHI. Only 26.8% of women from the poorest wealth index were enrolled in the CBHI, compared to 40.3% of those from the median wealth index. According to our findings, antenatal care coverage in Ethiopia is less than fifty percent. Women are 33% more likely to use ANC if they have CBHI membership. In addition to CBHI membership, the authorities should think about access to the media, education, and wealth status to improve antenatal services for Ethiopian women.
Ethiopia has been implementing CBHI since 2011 (23). The CBHI in Ethiopia targeted the rural areas and citizens mainly recruited in informal sectors such as agriculture. Its expansion in the recent time has brought a significant improvement in healthcare utilizations and financial risk protection (23).
According to EDHS 2019, 43 percent of pregnant women received prenatal care (ANC 4+) (95% CI: 41.5%–44.3%). Despite of the fact that the prevalence of ANC 4 + coverage has risen over time (12% in 2005, 19% in 2011, and 32% in 2016), more than half of pregnant women did not use it during their pregnancy. Ethiopia is ranked 35th among sub-Saharan African nations in terms of coverage of ANC, according to Ataguba JE and colleagues (24). Multi-sectorial, personal factors and community perceptions are contributing to low coverage of maternal health services in Sub-Saharan Africa. One reason for persistent low coverage of antenatal care could be related to delayed initiation of antenatal care, which hinders the completion of ANC follow-up, as the median survival time was reported was between 5 and 7 months (25, 26). Indication, community attitudes regarding cultural beliefs, the ability of decisions, and interactions with healthcare providers are potential barriers to the utilization of healthcare services during pregnancy (26–28). The uptake of antenatal care (ANC) is critical for universal reproductive coverage. ANC represents women's entrance into health services and the potential to raise safe mother and newborn targets, even though it is not expected to directly impact mortality.
The current study depicted the positive association between health insurance enrollment and ANC 4 + utilizations. Different local studies also reported a significant association (29, 30). This finding is comparable to that of previous studies conducted across Sub Saharan Africa on the association of insurance with ANC use (10, 31). The positive association might be due to insurance providing sufficient protection against catastrophic expenditure and because insurance can be linked to other socioeconomic indicators (32). Although the government provided a complete exemption for the cost of healthcare services for pregnant women, health insurance coverage is essential to eliminate out-of-pocket payments and significantly eliminate the financial barriers that often limit women's ability to attend ANC. In addition, CBHI could have other positive impacts, such as community development and local accountability of health care providers (33–37). Hence, by emphasizing the importance of CBHI and focusing on increasing enrollment, societies can remove financial barriers to healthcare access, leading to improved health-seeking behavior and better health outcomes for their populations.
Being in the highest wealth quintile increased the likelihood of ANC 4 + utilization. The finding is comparable with studies conducted in Bangladesh (38), Mozambique (39) and systematic review across SSA (40). There is strong evidence that women's economic status was a strong predictor of compliance with the nationally recommended first contact with ANC and facility delivery, with the richest women more likely to seek early health care (40–42). This positive impact of economic status could decrease the dropout rate and enable women to attend optimal ANC.
Education emerged as a significant factor in our analyses. Pregnant women with lower formal education were less likely to have ANC attendance as compared to those who had higher education level. Our study also shows that among pregnant women with formal education, those who had secondary or higher education tend to have a higher likelihood of reporting attendance at the ANC compared to their counterparts who did not have formal education. This finding is consistent as previous EDHS data report similar finding (43). Similarly, those who do not have access to the media appear to be excluded from antenatal care programs. Although health planners cannot change education levels, they should be considered in health promotion activities, using methods that are appropriate for this more susceptible demographic. In Ethiopia, health extension workers are a vital resource at the community level, and they would be used to reach women with lower levels of education. Health promotion initiatives should incorporate methods that are appropriate for this group, such as non-written tools for information, education, and communication.
Strength and limitations of the study
The study included data from a countrywide survey, which might be viewed as strength and could improve representativeness. The limitation is that a temporal relationship between the outcome and response variables cannot be established with the cross-sectional study design.
Conclusions
According to our findings, less than half of Ethiopian women had four and more antenatal care visits. We conclude that being covered by health insurance is associated with a higher likelihood of seeking timely ANC attendance. For this reason, we recommend that government and national health insurance authorities in Ethiopia to actively implement health insurance policies as well as roll out health educational programs that will facilitate and ensure high coverage of health insurance. Respondent age, Media access, marital status, education status, wealth index, and economic regions were also factors associated with antenatal care utilizations. Empowering the economic status of women and enhancing education coverage and media access are essential determinant to increase antenatal care utilization.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by National Research Ethics Review Committee (NRERC) of Ethiopia. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
BM, TR, GA, LR, and AB: contributed to the conception of the work, design of the work, acquisition of data, analysis, and interpretation of data. Data curation, drafting of the article, revising it critically for intellectual content, validation, and final approval of the version to be published was done by BM, TR, AD, GA, AB, BN, MG, ET, and LR. All authors contributed to the article and approved the submitted version.
Acknowledgments
The authors would like to acknowledge the measure DHS program for permitting data access to the Ethiopian DHS dataset.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. WHO. World Health Organization recommendations on antenatal care for a positive pregnancy experience. (2016). Available from: https://www.who.int/publications-detailredirect/9789241549912 (Accessed October 2022).
2. Dowswell T, Carroli G, Duley L, Gates S, Gülmezoglu AM, Khan-Neelofur D, et al. Alternative versus standard packages of antenatal care for low-risk pregnancy. Cochrane Database Syst Rev. (2015) 2015(7):Cd000934. doi: 10.1002/14651858.CD000934.pub3
3. Tunçalp Ö, Pena-Rosas JP, Lawrie T, Bucagu M, Oladapo OT, Portela A, et al. WHO Recommendations on antenatal care for a positive pregnancy experience-going beyond survival. BJOG. (2017) 124(6):860–2. doi: 10.1111/1471-0528.14599
4. WHO, UNICEF, UNFPA, World Bank Group, and the United Nations Population Division. Trends in Maternal Mortality 1990 to 2015. (2015). Available from: https://www.unfpa.org/publications/trends-maternal-mortality-1990-2015 (Accessed October 2022)
5. Tessema ZT, Teshale AB, Tesema GA, Tamirat KS. Determinants of completing recommended antenatal care utilization in sub-saharan from 2006 to 2018: evidence from 36 countries using demographic and health surveys. BMC Pregnancy Childbirth. (2021) 21(1):192. doi: 10.1186/s12884-021-03669-w
6. Tekelab T, Chojenta C, Smith R, Loxton D. The impact of antenatal care on neonatal mortality in sub-Saharan Africa: a systematic review and meta-analysis. PLoS One. (2019) 14(9):e0222566-e. doi: 10.1371/journal.pone.0222566
7. Turi E, Fekadu G, Taye B, Kejela G, Desalegn M, Mosisa G, et al. The impact of antenatal care on maternal near-miss events in Ethiopia: a systematic review and meta-analysis. Int J Africa Nurs Sci. (2020) 13:100246. doi: 10.1016/j.ijans.2020.100246
9. United States Agency for International Development. Ethiopia health sector financing reform. Washington DC, USA: USAID (2011).
10. Wang W, Temsah G, Mallick L. The impact of health insurance on maternal health care utilization: evidence from Ghana, Indonesia and Rwanda. Health Policy Plan. (2017) 32(3):366–75. doi: 10.1093/heapol/czw135
11. Fagbamigbe AF, Idemudia ES. Wealth and antenatal care utilization in Nigeria: policy implications. Health Care Women Int. (2017) 38(1):17–37. doi: 10.1080/07399332.2016.1225743
12. Simkhada B, Teijlingen ERV, Porter M, Simkhada P. Factors affecting the utilization of antenatal care in developing countries: systematic review of the literature. J Adv Nurs. (2008) 61(3):244–60. doi: 10.1111/j.1365-2648.2007.04532.x
13. Akowuah JA, Agyei-Baffour P, Awunyo-Vitor D. Determinants of antenatal healthcare utilisation by pregnant women in third trimester in Peri-Urban Ghana. J Trop Med. (2018) 2018:1673517. doi: 10.1155/2018/1673517
14. Aboagye RG, Okyere J, Ahinkorah BO, Seidu A-A, Zegeye B, Amu H, et al. Health insurance coverage and timely antenatal care attendance in sub-Saharan Africa. BMC Health Serv Res. (2022) 22(1):181. doi: 10.1186/s12913-022-07601-6
15. Dixon J, Tenkorang EY, Luginaah IN, Kuuire VZ, Boateng GO. National health insurance scheme enrolment and antenatal care among women in Ghana: is there any relationship? Trop Med Int Health. (2014) 19(1):98–106. doi: 10.1111/tmi.12223
16. Blanchet NJ, Fink G, Osei-Akoto I. The effect of Ghana's national health insurance scheme on health care utilisation. Ghana Med J. (2012) 46(2):76–84.22942455
18. Spaan E, Mathijssen J, Tromp N, McBain F, ten Have A, Baltussen R. The impact of health insurance in Africa and Asia: a systematic review. Bull World Health Organ. (2012) 90(9):685–92. doi: 10.2471/BLT.12.102301
19. Lagarde M, Palmer N. The impact of user fees on access to health services in low- and middle-income countries. Cochrane Database Syst Rev. (2011) 4:Cd009094. doi: 10.1002/14651858.CD009094
21. World Health Organization. Together on the road to Universal Health Coverage: a call to action. (2017). https://apps.who.int/iris/handle/10665/258962 (Accessed October 2022).
22. Central Statistical Agency, ICF. Ethiopia demographic and health survey. Addis Ababa, Ethiopia, and Rockville, Maryland, USA: CSA and ICF (2016).
23. Ethiopian Health Insurance Agency. Evaluation of community-based health insurance pilot schemes in Ethiopia. Final Report 2015 May. (2015).
24. Ataguba JE-O. A reassessment of global antenatal care coverage for improving maternal health using sub-Saharan Africa as a case study. PLoS One. (2018) 13(10):e0204822. doi: 10.1371/journal.pone.0204822
25. Seid A, Ahmed M. Survival time to first antenatal care visit and its predictors among women in Ethiopia. PLoS One. (2021) 16(5):e0251322. doi: 10.1371/journal.pone.0251322
26. Ahinkorah BO, Ameyaw EK, Seidu AA, Odusina EK, Keetile M, Yaya S. Examining barriers to healthcare access and utilization of antenatal care services: evidence from demographic health surveys in sub-Saharan Africa. BMC Health Serv Res. (2021) 21(1):125. doi: 10.1186/s12913-021-06129-5
27. Gage AJ. Barriers to the utilization of maternal health care in rural Mali. Soc Sci Med. (2007) 65(8):1666–82. doi: 10.1016/j.socscimed.2007.06.001
28. Brighton A, D'Arcy R, Kirtley S, Kennedy S. Perceptions of prenatal and obstetric care in sub-Saharan Africa. Int J Gynaecol Obstet. (2013) 120(3):224–7. doi: 10.1016/j.ijgo.2012.09.017
29. Ftwi M, Gebretsadik GG-E, Berhe H, Haftu M, Gebremariam G, Tesfau YB. Coverage of completion of four ANC visits based on recommended time schedule in Northern Ethiopia: a community-based cross-sectional study design. PLoS One. (2020) 15(8):e0236965. doi: 10.1371/journal.pone.0236965
30. Muchie KF. Quality of antenatal care services and completion of four or more antenatal care visits in Ethiopia: a finding based on a demographic and health survey. BMC Pregnancy Childbirth. (2017) 17(1):300. doi: 10.1186/s12884-017-1488-0
31. Dadjo J, Ahinkorah BO, Yaya S. Health insurance coverage and antenatal care services utilization in West Africa. BMC Health Serv Res. (2022) 22(1):311. doi: 10.1186/s12913-022-07698-9
32. Lagarde M, Palmer N. The impact of user fees on health service utilization in low-and middle-income countries: how strong is the evidence? Bull World Health Organ. (2008) 86(11):839–48. doi: 10.2471/BLT.07.049197
33. Gebru T, Lentiro K. The impact of community-based health insurance on health-related quality of life and associated factors in Ethiopia: a comparative cross-sectional study. Health Qual Life Outcomes. (2018) 16(1):110. doi: 10.1186/s12955-018-0946-3
34. Habib SS, Perveen S, Khuwaja HM. The role of micro health insurance in providing financial risk protection in developing countries–a systematic review. BMC Public Health. (2016) 16:281. doi: 10.1186/s12889-016-2937-9
35. Nyandekwe M, Nzayirambaho M, Kakoma JB. Universal health insurance in Rwanda: major challenges and solutions for financial sustainability case study of Rwanda community-based health insurance part I. Pan Afr Med J. (2020) 37:55. doi: 10.11604/pamj.2020.37.55.20376
36. Ranson MK. Reduction of catastrophic health care expenditures by a community-based health insurance scheme in Gujarat, India: current experiences and challenges. Bull World Health Organ. (2002) 80(8):613–21.12219151
37. Sarker AR, Sultana M, Ahmed S, Mahumud RA, Morton A, Khan JAM. Clients’ experience and satisfaction of utilizing healthcare services in a community based health insurance program in Bangladesh. Int J Environ Res Public Health. (2018) 15(8):1637. doi: 10.3390/ijerph15081637
38. Pervin J, Venkateswaran M, Nu UT, Rahman M, O'Donnell BF, Friberg IK, et al. Determinants of utilization of antenatal and delivery care at the community level in rural Bangladesh. PLoS One. (2021) 16(9):e0257782. doi: 10.1371/journal.pone.0257782
39. Yaya S, Idriss-Wheeler D, Shibre G, Amouzou A, Bishwajit G. Prevalence of institutional delivery and its correlates amongst women of reproductive age in Mozambique: a cross-sectional analysis. Reprod Health. (2020) 17(1):1–11. doi: 10.1186/s12978-019-0847-x
40. Okedo-Alex IN, Akamike IC, Ezeanosike OB, Uneke CJ. Determinants of antenatal care utilisation in sub-Saharan Africa: a systematic review. BMJ open. (2019) 9(10):e031890. doi: 10.1136/bmjopen-2019-031890
41. Shibre G, Mekonnen W. Socio-economic inequalities in ANC attendance among mothers who gave birth in the past 12 months in debre brehan town and surrounding rural areas, North East Ethiopia: a community-based survey. Reprod Health. (2019) 16(1):99. doi: 10.1186/s12978-019-0768-8
42. Selebano KM, Ataguba JE. Decomposing socio-economic inequalities in antenatal care utilisation in 12 Southern African development community countries. SSM Popul Health. (2021) 17:101004. doi: 10.1016/j.ssmph.2021.101004
Keywords: health insurance, antenatal care, prenatal care, DHS, women, Ethiopia
Citation: Merga BT, Raru TB, Deressa A, Regassa LD, Gamachu M, Negash B, Birhanu A, Turi E and Ayana GM (2023) The effect of health insurance coverage on antenatal care utilizations in Ethiopia: evidence from national survey. Front. Health Serv. 3:1101164. doi: 10.3389/frhs.2023.1101164
Received: 3 February 2023; Accepted: 13 September 2023;
Published: 6 October 2023.
Edited by:
Goodness C. Aye, Federal University of Agriculture Makurdi, NigeriaReviewed by:
Qingxia Kong, Erasmus University Rotterdam, NetherlandsAndriy Moshyk, Bristol Myers Squibb, United States
© 2023 Merga, Raru, Deressa, Regassa, Gamachu, Negash, Birhanu, Turi and Ayana. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Belay Negash negash.bel@gmail.com
 Bedasa Taye Merga
Bedasa Taye Merga Temam Beshir Raru
Temam Beshir Raru Alemayehu Deressa
Alemayehu Deressa Lemma Demissie Regassa
Lemma Demissie Regassa Mulugeta Gamachu
Mulugeta Gamachu Belay Negash
Belay Negash Abdi Birhanu
Abdi Birhanu Ebisa Turi
Ebisa Turi Galana Mamo Ayana
Galana Mamo Ayana