Prevalence and possible factors of cognitive frailty in the elderly with hypertension and diabetes
- 1Department of Geriatric, The Affiliated Wuxi People's Hospital of Nanjing Medical University, Wuxi, China
- 2Department of Medicine, Wuxi Xin'an Community Health Service Center, Wuxi, China
- 3Department of General Practice, The Affiliated Wuxi People's Hospital of Nanjing Medical University, Wuxi, China
- 4Department of Endocrinology, The Affiliated Wuxi People's Hospital of Nanjing Medical University, Wuxi, China
Background: Cognitive frailty is the coexistence of physical frailty and mild cognitive impairment. Research shows that cognitive frailty is related to an increased risk of hospitalization, mortality, disability, and dementia. Diabetes and hypertension are common risk factors for physical frailty and cognitive impairment. However, the factors influencing cognitive frailty in the elderly with hypertension and diabetes are still unclear. This study aimed to investigate the possible factors influencing cognitive frailty in the elderly with hypertension and diabetes.
Methods: A cross-sectional study was conducted. We evaluated people over 60 years with hypertension and diabetes who underwent physical examination in Wuxi Xin'an Community Health Service Center. Frail scale, Montreal Cognitive Assessment-Basic and clinical dementia rating were used to assess cognitive frailty. We collected demographic characteristics, hypertension and diabetes-related laboratory indicators of the participants. We also used various scales to assess the overall health status of the elderly.
Results: Approximately 20.8% of the participants were determined to have cognitive frailty in elderly adults with hypertension and diabetes. These participants were older, had a lower monthly income, and included a higher proportion of peasants. They also had a higher level of depression (p = 0.037), higher risk of falls (p = 0.000), higher risk of malnutrition (p = 0.002), poorer ability to perform activities of daily living (ADL) (p = 0.000), and less social support (p = 0.030). Multivariate regression analysis was used to further assess the factors for cognitive frailty. After adjusting for possible confounders, age and ADL score emerged as risk factors, whereas high monthly income decreased the risk of cognitive frailty.
Conclusion: Cognitive frailty is correlated with age, income, and ability to perform daily living activities in the elderly with diabetes and hypertension. Closer attention to the elderly who have low income and poor self-care ability may play an important role in the early prevention of cognitive frailty and even dementia.
Introduction
Cognitive frailty, defined as the co-existence of physical frailty and cognitive impairment, has recently attracted increasing attention. The term “cognitive frailty” was coined by experts in 2013 (1). However, its definition has never been well-established. Researchers in different regions of the world have different definitions. Assessment scales are also different. The Fried scale and Frail scale are commonly used to evaluate physical frailty. Montreal Cognitive Assessment (MoCA) scale and Mini-Mental State Examination (MMSE) scale are commonly used in cognitive assessment. Ruan et al. (2) classify cognitive frailty into two types: reversible and potentially reversible. This study considered the latter definition. It is defined by the presence of physical frailty or prefrailty and cognitive impairment, excluding dementia, caused by various reasons (2). The prevalence of cognitive frailty in community settings is 1.2 to 7.7%, which increases to 20% in nursing centers and inpatient departments (3–6).
Cognitive frailty is closely associated with a higher risk of hospitalization, death, and disability (7, 8). It is also a strong predictor of overall dementia and vascular dementia (9). Thus, early intervention for the population with cognitive frailty can help prevent dementia and other aggravations. As we all know, cognitive frailty is strongly correlated with multiple factors. Panza et al. mentioned some possible neurobiological mechanisms underlying cognitive frailty, including vascular diseases, sarcopenia, metabolic disorders, nutritional status, psychological factors and inflammatory status (10). Due to reduced ability of activities and decline of brain function, the prevalence of cognitive frailty increases with age (11). Weight loss and vitamin deficiency may lead to physical frailty. Several studies have shown that the incidence of malnutrition is extremely high among elderly people with cognitive frailty (12–14). In addition, level of education is strongly associated with cognitive decline. The longer the years of education, the slower the cognitive decline (15, 16). Older adults with depression are more likely to develop cognitive frailty (17). Liu et al. indicates that moderate physical activities for 1 year can reduce the progression of cognitive frailty in sedentary older adults (18).
Hypertension and diabetes, the most common chronic diseases worldwide (19, 20), have been considered risk factors for physical frailty (21, 22) and cognitive impairment (23, 24). Thus, more attention should be paid to older adults with hypertension and diabetes. This study aimed to investigate the risk factors of cognitive frailty in the elderly with hypertension and diabetes.
Materials and methods
Participants and data collection
A cross-sectional study was conducted in Wuxi Xin'an Community Health Service Center from April 2018 to May 2018. Participants included older adults with diabetes and hypertension.
Inclusion criteria: 1. aged over 60; 2. previous diagnosis of hypertension and diabetes.
Exclusion criteria: 1. dementia; 2. severe hepatic and renal insufficiency; 3. failure to cooperate in the assessment using various scales.
The demographic and clinical variables included age, gender, occupation, education level, income per month, smoking history, and drinking history. Serum albumin, calcium, 25- hydroxy Vitamin D, triglycerides (TG), low-density lipoprotein cholesterol (LDL), high-density lipoprotein cholesterol (HDL), homocysteine, folic acid, Vitamin B12, fasting plasma glucose, fasting insulin, and HbA1c levels were assessed by the Laboratory Center of Wuxi People's Hospital.
Assessment of cognitive function
Montreal Cognitive Assessment-Basic (MoCA-B) was used to evaluate cognitive function. MoCA-B score <26 and clinical dementia rating (CDR) = 0.5 (excluding dementia) indicated mild cognitive impairment.
Other evaluation scales
The 5-item Frail scale was used to assess physical frailty. Frail score ≥1 indicated physical frailty, with a higher score showing a higher level of frailty. The Mini-Nutrition Assessment-Short Form (MNA-SF) evaluated the nutritional status of the participants. MNA-SF scores <8, 8–11, and >11 indicated malnutrition, risk of nutrition, and no malnutrition, respectively. The Geriatric Depression Scale 15-item (GDS-15) assessed the psychological health of participants, with a higher score indicating severe depression. The 10-item Social Support Rating Scale (SSRS) evaluated support from themselves, others and society. A higher total score indicated better social support. The Morse Fall Scale (MFS) was used to assess participants' risk of falling, with MFS scores <25, 25–45, and >45 indicating low risk, medium risk, and high risk, respectively. The ability to perform activities of daily living (ADL) was assessed at two levels. The basic activities of daily living scale (BADL) assessed skills including eating, dressing, grooming, bathing, going to the toilet, and walking; the instrumental activities of daily living scale (IADL) evaluated skills such as making phone calls, shopping, preparing meals, doing housework, washing clothes, taking public transport, taking drugs, and money management. A score >14 showed functional decline, with a higher score indicating decreased ability to perform daily living activities.
Statistical analysis
All variables were tested for normal distribution. Student t-test, Mann-Whitney U test, and Chi-square test were conducted to compare the variables between groups. Continuous variables with normal distribution were presented as mean with standard deviation. Continuous variables with non-normal distribution were presented as median with quartile, and categorical variables as percentages. The multivariate logistic regression analysis was also performed. SPSS 22.0 software was used for data analysis, and p < 0.05 was considered statistically significant.
Results
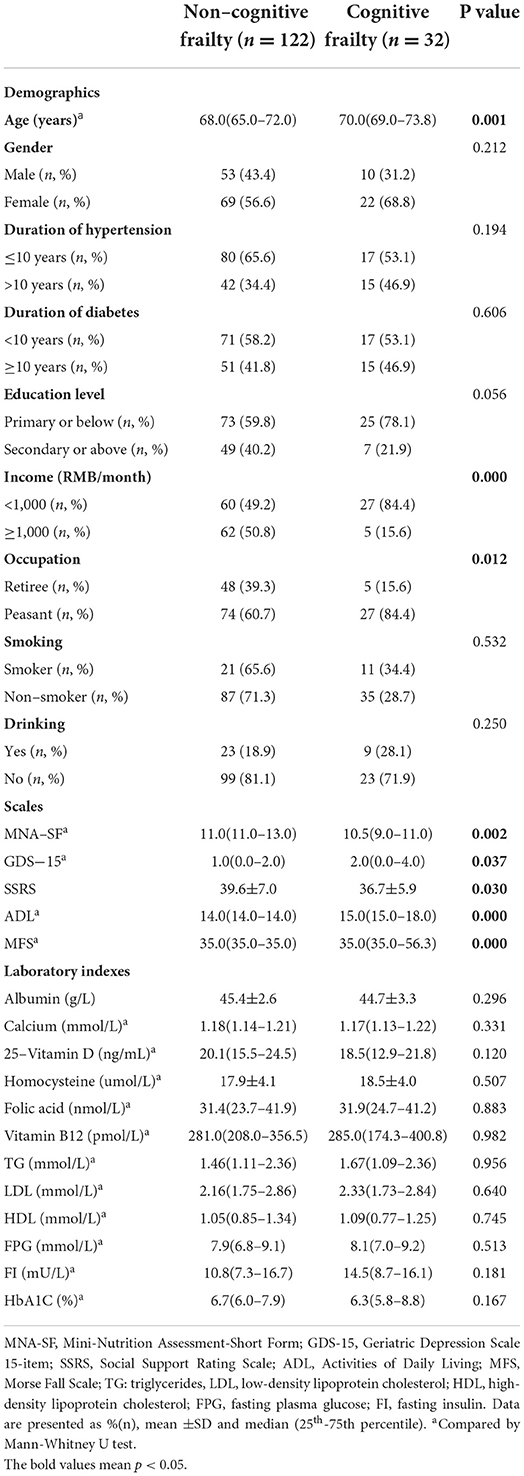
A total of 154 participants were enrolled, including 91 females (59.1%), 98 with a primary level or below education (63.6%), and 122 non-drinkers (79.2%). After the assessment, 32 (20.8%) were determined to have cognitive frailty. These participants were older, had a lower monthly income, and included a higher proportion of peasants. Participants with cognitive frailty also had higher scores of GDS-15 (p = 0.037), higher risk of malnutrition (p = 0.002), higher fall risk (p = 0.000), higher ADL score (p = 0.000), poorer daily living ability (p = 0.000), and less social support (p = 0.030) (Table 1). The participants between the two groups did not differ in laboratory indexes, such as lipid levels, albumin, calcium, 25- hydroxy Vitamin D, homocysteine, folic acid, Vitamin B12, fasting plasma glucose, fasting insulin, and HbA1c level.
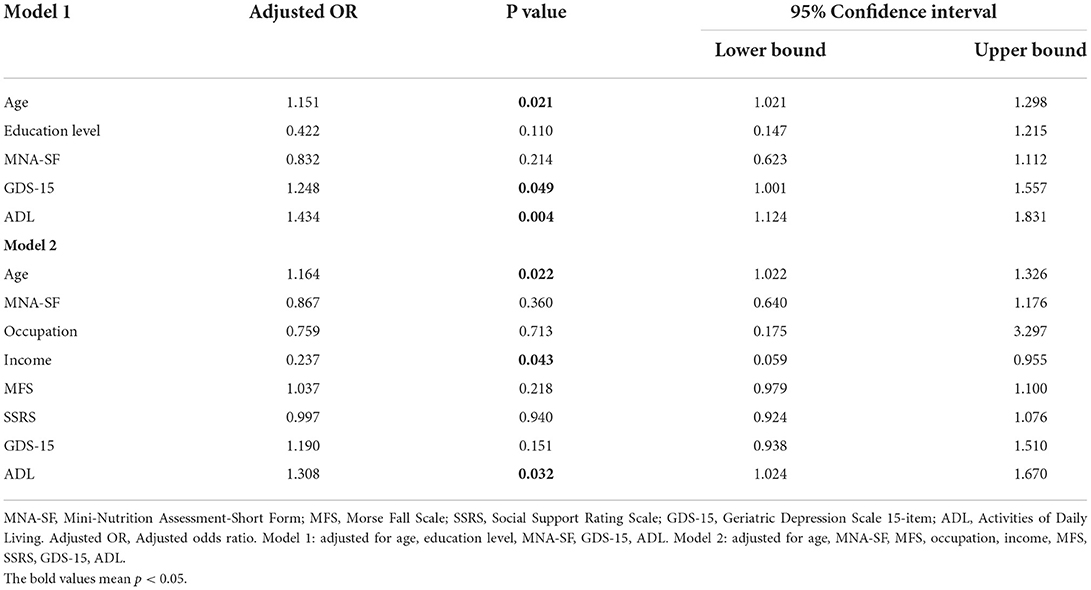
After adjusting for education level, status of nutrition, GDS-15, age and ADL score were risk factors for cognitive frailty. After adjusting for age, social support, ADL score, Morse Fall score, GDS-15 score, MNA-SF score, income, and occupation in Table 2, the risk of cognitive frailty increased significantly with age (OR = 1.164, 95% CI: 1.022–1.326, p < 0.05) and ADL score (OR = 1.308, 95% CI: 1.024–1.670, p < 0.05), and decreased significantly with monthly income (OR = 0.237, 95% CI: 0.059–0.955, p < 0.05).
Discussion
Recently, comprehensive geriatric assessment has been attracting increasing attention in China. In this study, we screened the associated factors of mild cognitive impairment and physical frailty in the elderly by reviewing relevant literature. We evaluated the nutritional status, depression level, social support, demographic and clinical characteristics, lipid levels, blood glucose levels, and other indicators of the recruited population. This was the first study to investigate the influencing factors of cognitive frailty in the elderly with hypertension and diabetes. Cognitive frailty can progress to various forms of dementia (25–27), thus increasing the risk of hospitalization, falls, and death (28–30). About 20.8% of the participants were determined to have cognitive frailty in this study, a number higher than that previously reported (31). This may be explained by the fact that the participants in this study had multiple chronic diseases. Mone et al. (32) suggest that hypertension and diabetes, which are associated with endothelial dysfunction, inflammation, and oxidative stress, can lead to cognitive frailty. Furthermore, adults with cognitive frailty in this study were older, had a lower income, and were mainly peasants with a high risk of malnutrition, less social support, higher ADL score, and a high risk of falling. Moreover, age, income, and ADL score were significantly associated with cognitive frailty, even after adjusting for other possible influencing factors.
Age was found to be the most common risk factor for cognitive frailty, which is consistent with the study of Kim et al. and Mone et al. (33, 34). High-income people may have a stronger awareness of chronic disease management and could intervene in the early stage of the disease. The terms physical frailty, cognitive impairment, and cognitive frailty have partially overlapped in definitions. Several studies have investigated the effects of ADL on people with cognitive frailty, but the assessment methods of ADL in other study are different. IADL has been shown as a risk factor for physical frailty and cognitive impairment. Research also shows that physical disability, indicated by lower performance in BADL (assessed by the Katz index), is a risk factor for cognitive frailty (11, 35–37). Ma et al. (38) showed that cognitive frailty can increase the risk of BADL disability by over ten times during a 3-year follow-up in the elderly compared to robust adults. As Avila-Funes et al. (39) supported, people with cognitive frailty tended to develop ADL dependence. They used internationally recognized scales to assess BADL and IADL dependence. In the present study, the risk of ADL dependence in participants with cognitive frailty was significantly greater than in those without cognitive frailty.
There was no statistical significance in the education level between the two groups in this study, which might be associated with the distribution of education level of our individuals. More participants were primary or lower education level in our study. However, after adjusted for education level, MNA-SF, GDS-15, age and ADL score still significantly increased risk of cognitive frailty. Previous studies suggested that cognitive frailty could be improved with nutritional interventions, muscle exercise, resistance training, and fall avoidance (17, 40). Our study also suggested that improving the ability to perform daily living activities may reduce the prevalence of cognitive frailty in the elderly population. Age is an irreversible factor. With increasing age, more attention should be paid to people with hypertension and diabetes at lower income levels and lower ability of daily living.
There are several limitations of this study. First, the study had a relatively small sample size. Future research should include a bigger sample population. Second, this was a cross-sectional study, and follow-up is required to confirm the findings. Finally, the groups of physical frailty and mild cognitive impairment only should be constructed.
Furthermore, we can screen people at a high risk of cognitive frailty based on ADL assessment quickly. Future research should focus on improving the level of ADL, which may be beneficial in reducing the prevalence of cognitive frailty.
Conclusion
Cognitive frailty is correlated with age, monthly income, and ability to perform daily living activities in the elderly with hypertension and diabetes. For the elderly with low income and poor self-care ability, early intervention for cognitive frailty should be carried out. We will next investigate the effects of these interventions on early dementia.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by Ethics Committee of the Wuxi People's Hospital. The patients/participants provided their written informed consent to participate in this study.
Author contributions
KH, XZ, YZ, and SL designed the research. SL, QX, JY, YY, ZW, BZ, SW, and XC helped with the data collection and analysis. SL and QX wrote the first draft of the manuscript. KH, XZ, and YZ contributed to the critical revision of the manuscript. All authors contributed to the manuscript revision and approved the submitted version.
Funding
This work was funded by the Young Project of the Wuxi Health Committee (Q201914), the Top Talent Support Program for Young and Middle-Aged People of Wuxi Health (BJ2020008), and the Major Project of the Wuxi Health Committee (Z202002).
Acknowledgments
We thank the study participants and the clinical staff for their support and contribution to this study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The reviewer XE declared a shared affiliation with the authors SL, QX, JY, YY, ZW, BZ, YZ, XZ, and KH to the handling editor at the time of review.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. van Kan GA, Ousset PJ, Gillette-Guyonnet S, Abellan Van Kan G, Ousset PJ, Doto ME, et al. Cognitive frailty: Rational and definition from an(IANA/IAGG) international consensus group. J Nutr Health Aging. (2013) 17:726–34. doi: 10.1007/s12603-013-0367-2
2. Ruan QW, Yu ZW, Chen M, Bao ZJ, Li J, He W. Cognitive frailty, a novel target for the prevention of elderly dependency. Ageing Res Rev. (2015) 20:1–10. doi: 10.1016/j.arr.2014.12.004
3. Shimada H, Makizako H, Lee S, Doi T, Lee S, Tsutsumimoto K, et al. Impact of cognitive frailty on daily activities in older persons. J Nutr Health Aging. (2016) 20:729–35. doi: 10.1007/s12603-016-0685-2
4. Rajab NF, Singh DKA, Che Din N, Mahadzir H, Ishak WS, Sahar S, et al. Incidence and predictors of cognitive frailty among older adults: a community-based longitudinal study. Int J Environ Res Public Health. (2020) 17:1547. doi: 10.3390/ijerph17051547
5. Roppolo M, Mulasso A, Rabaglietti E. Cognitive frailty in Italian community dwelling older adults: prevalence rate and its association with disability. J Nutr Health Aging. (2016) 21:631–6. doi: 10.1007/s12603-016-0828-5
6. Sugimoto T, Sakurai T, Ono R, Kimura A, Saji N, Niida S, et al. Epidemiological and clinical significance of cognitive frailty: a mini review. Ageing Res Rev. (2018) 44:1–7. doi: 10.1016/j.arr.2018.03.002
7. Lee WJ, Peng LN, Liang CK, Loh CH, Chen LK. Cognitive frailty predicting all-cause mortality among community-living older adults in Taiwan: a 4-year nationwide population-based cohort study. PLoS ONE. (2018) 13:e0200447. doi: 10.1371/journal.pone.0200447
8. St John PD, Tyas SL, Griffith LE, Menec V. The cumulative effect of frailty and cognition on mortality - results of a prospective cohort study. Int Psychogeriatr. (2016) 29:535–43. doi: 10.1017/S1041610216002088
9. Solfrizzi V, Scafato E, Seripa D, Lozupone M, Imbimbo BP, D'Amato A, et al. Reversible cognitive frailty, dementia, and all-cause mortality. the italian longitudinal study on aging. J Am Med Dir Assoc. (2017) 18:89e1–e8. 10.1016/j.jamda.2016.10.012. doi: 10.1016/j.jamda.2016.10.012
10. Panza F, Lozupone M, Solfrizzi V, Sardone R, Dibello V, Di Lena L, et al. Different cognitive frailty models and health- and cognitive-related outcomes in older age: from epidemiology to prevention. J Alzheimers Dis. (2018) 62:993–1012. doi: 10.3233/JAD-170963
11. Malek Rivan NF, Shahar S, Rajab NF, Singh DKA, Din NC, Hazlina M, et al. Cognitive frailty among Malaysian older adults: baseline findings from the LRGS TUA cohort study. Clin Interv Aging. (2019) 14:1343–52. doi: 10.2147/CIA.S211027
12. Chye L, Wei K, Nyunt MSZ, Gao Q, Wee SL, Ng TP. Strong relationship between malnutrition and cognitive frailty in the Singapore longitudinal ageing studies (SLAS-1 and SLAS-2). J Prev Alzheimers Dis. (2018) 5:1–7. doi: 10.14283/jpad.2017.46
13. Dominguez LJ, Barbagallo M. The relevance of nutrition for the concept of cognitive frailty. Curr Opin Clin Nutr Metab Care. (2017) 20:61–8. doi: 10.1097/MCO.0000000000000337
14. Seesen M, Sirikul W, Ruangsuriya J, Griffiths J, Siviroj P. Cognitive frailty in Thai community-dwelling elderly: prevalence and its association with malnutrition. Nutrients. (2021) 13: 4239. doi: 10.3390/nu13124239
15. Brigola AG, Alexandre TDS, Inouye K, Yassuda MS, Pavarini SCI, Mioshi E. Limited formal education is strongly associated with lower cognitive status, functional disability and frailty status in older adults. Dement Neuropsychol. (2019) 13:216–24. doi: 10.1590/1980-57642018dn13-020011
16. Zahodne LB, Stern Y, Manly JJ. Differing effects of education on cognitive decline in diverse elders with low versus high educational attainment. Neuropsychology. (2015) 29:649–57. doi: 10.1037/neu0000141
17. Kwan RYC, Leung AYM., Yee A, Lau LT, Xu XY, Dai DLK, et al. Cognitive frailty and its association with nutrition and depression in community-dwelling older people. J Nutr Health Aging. (2019) 23:1–6. doi: 10.1007/s12603-019-1258-y
18. King AC, Liu CK, Manini TM. Effect of 24-month physical activity on cognitive frailty and the role of inflammation: the LIFE randomized clinical trial. BMC Med. (2018) 16:185. doi: 10.1186/s12916-018-1174-8
19. Draznin B, Aroda VR, Bakris G, Benson G, Brown FM, Freeman R, et al. Diabetes care in the hospital: standards of medical care in diabetes-2022. Diab Care. (2022)45(Suppl 1):S244–253. doi: 10.2337/dc22-S016
20. Ida S, Kaneko R, Imataka K, Murata K. Relationship between frailty and mortality, hospitalization, and cardiovascular diseases in diabetes: a systematic review and meta-analysis. Cardiovasc Diabetol. (2019) 18:1–13. doi: 10.1186/s12933-019-0885-2
21. Clegg A, Hassan-Smith Z. Frailty and the endocrine system. Lancet Diabetes Endocrinol. (2018) 6:743–52. doi: 10.1016/S2213-8587(18)30110-4
22. Pulgrossi RC, Biella MM, Izbicki R, Torres LM, Biella MM, et al. Hypertension and frailty in older adults. J Clin Hypertens. (2018) 20:186–92. doi: 10.1111/jch.13135
23. Ganmore I, Elkayam I, Ravona-Springer R, Lin HM, Liu X, Plotnik M, et al. Deterioration in motor function over time in older adults with type 2 diabetes is associated with accelerated cognitive decline. Endocr Pract. (2020) 26:1143–52. doi: 10.4158/EP-2020-0289
24. Chan YH, Lim JY, Vellas B. Slow gait, subjective cognitive decline and motoric cognitive RISK syndrome: prevalence and associated factors in community dwelling older adults. J Nutr Health Aging. (2021) 25:48–56. doi: 10.1007/s12603-020-1525-y
25. Muir Hunter SW, Doherty TJ, Duque G. Disentangling cognitive-frailty: results from the gait and brain study. J Gerontol A Biol Sci Med Sci. (2016) 71:1476–82. doi: 10.1093/gerona/glw044
26. Zheng L, Li G, Gao D, Wang S, Meng X, Wang C, et al. Cognitive frailty as a predictor of dementia among older adults: a systematic review and meta-analysis. Arch Gerontol Geriatr. (2020) 87:103997. doi: 10.1016/j.archger.2019.103997
27. Kojima G, Taniguchi Y, Iliffe S, Walters, K. Frailty as a predictor of Alzheimer disease, vascular dementia, and all dementia among community-dwelling older people: a systematic review and meta-analysis. J Am MedDirect Assoc. (2016) 17:881–8. doi: 10.1016/j.jamda.2016.05.013
28. Yu R, Morley JE, Kwok T, Leung J, Cheung O, Woo J. The effects of combinations of cognitive impairment and pre-frailty on adverse outcomes from a prospective community-based cohort study of older Chinese people. Front Med. (2018) 5:1–11. doi: 10.3389/fmed.2018.00050
29. Rivan NFM, Singh DKA, Shahar S, Wen GJ, Rajab NF, Din NC, et al. Cognitive frailty is a robust predictor of falls, injuries, and disability among community-dwelling older adults. BMC Geriatr. (2021) 21:593. doi: 10.1186/s12877-021-02525-y
30. Bu ZH, Huang AL, Xue MT, Li QY, Bai YM, Xu GH, et al. Cognitive frailty as a predictor of adverse outcomes among older adults: a systematic review and meta-analysis. Brain Behav. (2021) 11:e01926. doi: 10.1002/brb3.1926
31. Shimada H, Makizako H, Tsutsumimoto K, Doi T, Lee S, Suzuki T. Cognitive frailty and incidence of dementia in older persons. J Prev Alzheimers Dis. (2018) 5:42–8. doi: 10.14283/jpad.2017.29
32. Mone P, Gambardella J, Lombardi A, Pansini A, De Gennaro S, Leo AL, et al. Correlation of physical and cognitive impairment in diabetic and hypertensive frail older adults. Cardiovasc Diabetol. (2022) 21:1–6. doi: 10.1186/s12933-021-01442-z
33. Kim H, Awata S, Watanabe Y, Kojima N, Osuka Y, Motokawa K, et al. Cognitive frailty in community-dwelling older Japanese people: prevalence and its association with falls. Geriatr Gerontol Int. (2019) 19:647–53. doi: 10.1111/ggi.13685
34. Mone P, Gambardella J, Pansini A, de Donato A, Martinelli G, Boccalone E, et al. Cognitive impairment in frail hypertensive elderly patients: role of hyperglycemia. Cells. (2021) 10:2115. doi: 10.3390/cells10082115
35. Aliberti MJR, Cenzer IS, Smith AK, Lee SJ, Yaffe K, Covinsky KE. Assessing risk for adverse outcomes in older adults: The need to include both physical frailty and cognition. J Am Geriatr Soc. (2019) 67:477–83. doi: 10.1111/jgs.15683
36. Feng L, Zin Nyunt MS, Gao Q, Feng L, Yap KB, Ng TP, et al. Cognitive frailty and adverse health outcomes: findings from the Singapore longitudinal ageing studies (SLAS). J Am Med Dir Assoc. (2017) 18:252–8. doi: 10.1016/j.jamda.2016.09.015
37. Won CW, Lee Y, Kim S, Yoo J, Kim M, Ng TP, et al. Modified criteria for diagnosing “cognitive frailty”. Psychiatry Investig. (2018) 15:839–42. doi: 10.30773/pi.2018.05.22
38. Ma YJ, Li XD, Pan Y, Zhao R, Wang X, Jiang X, et al. Cognitive frailty predicting death and disability in Chinese elderly. Neurol Res. (2021) 43:1–9. doi: 10.1080/01616412.2021.1939235
39. Avila-Funes JA, Amieva H, Barberger-Gateau P, Le Goff M, Raoux N, Ritchie K, et al. Cognitive impairment improves the predictive validity of the phenotype of frailty for adverse health outcomes: the three-city study. J Am Geriatr Soc. (2009) 57:453–61. doi: 10.1111/j.1532-5415.2008.02136.x
Keywords: diabetes, hypertension, cognitive frailty, elderly, activities of daily living
Citation: Lu S, Xu Q, Yu J, Yang Y, Wang Z, Zhang B, Wang S, Chen X, Zhang Y, Zhu X and Hong K (2022) Prevalence and possible factors of cognitive frailty in the elderly with hypertension and diabetes. Front. Cardiovasc. Med. 9:1054208. doi: 10.3389/fcvm.2022.1054208
Received: 26 September 2022; Accepted: 07 November 2022;
Published: 21 November 2022.
Edited by:
Jia Qi, Shanghai Jiao Tong University, ChinaReviewed by:
Xu De En, Nanjing Medical University, ChinaLi Hou, Affiliated Hospital of Jiangsu University, China
Copyright © 2022 Lu, Xu, Yu, Yang, Wang, Zhang, Wang, Chen, Zhang, Zhu and Hong. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Kan Hong, lindashao99@163.com; Xiaowei Zhu, 1766990886@qq.com; Yunyun Zhang, zhangyunyun026133@126.com
†These authors have contributed equally to this work and share first authorship
 Shourong Lu1†
Shourong Lu1†  Kan Hong
Kan Hong