- 1Department of Obstetrics and Gynecology, Shengjing Hospital of China Medical University, Shenyang, China
- 2Department of Social Medicine, School of Public Health, China Medical University, Shenyang, China
- 3Faculty of Medical and Health Sciences, The University of Auckland, Auckland, New Zealand
Background: Prenatal depression is associated with adverse maternal and fetal health consequences, yet it has not raised sufficient concerns in China. Psychological worries and stress may lead to prenatal depression, but resilience could relieve some of the negative effects of worries and stress and mitigate prenatal depression.
Aims: This study aimed to assess the prevalence of prenatal depression and explore its associated factors.
Method: A multisite cross-sectional study was conducted that included 605 pregnant women from three hospitals in two provincial capitals (Shenyang and Zhengzhou) and one municipality (Chongqing). A smartphone questionnaire was employed to assess prenatal depression using the Center for Epidemiologic Studies Depression Scale (CES-D). Multivariate logistic regression analysis was performed to explore factors associated with prenatal depression.
Results: The prevalence of prenatal depression (CES-D≥16) among Chinese pregnant women was 28.4%. Logistic regression analyses revealed that prenatal depression was positively associated with worries about appearance (odds ratio [OR] 1.666, 95% confidence interval [CI] 1.043–2.661) and perceived stress (OR 1.156, 95% CI 1.104–1.211) and negatively associated with monthly income, relationship with mother (OR 0.287, 95% CI 0.103–0.796), and resilience (OR 0.935, 95% CI 0.918–0.953).
Conclusion: These findings revealed that Chinese pregnant women suffered from high levels of prenatal depression (28.4%). Worries about appearance and perceived stress were risk factors for prenatal depression, whereas a pregnant woman’s harmonious relationship with her own mother and resilience could relieve the negative impacts of pregnancy that can lead to prenatal depression. Improving resilience and maintaining harmonious relationships with mothers should be emphasized in order to reduce the detrimental effects of pregnancy and improve the mental well-being of pregnant women.
Introduction
Most pregnant women experience emotional worries and stress during pregnancy: new responsibilities related to their lives and family expectations may lead to depression in both prenatal and postnatal periods (1). Specifically, substantial changes in body function and appearance and worries about fetal health pose great challenges to psychological health, which can result in mental disorders such as depression and anxiety (2, 3).
Prenatal depression is one of the most widespread mental disorders among women during pregnancy, with estimated rates of depression ranging from 7 to 37.1% (4–6). Previous studies indicated that prenatal depression was a strong predictor of postnatal depression, but prenatal depression is more prevalent than postnatal depression (7). In China, there is a scarcity of mental healthcare for women, especially for pregnant women, which can lead not only to adverse health outcomes for the pregnant women themselves but also result in detrimental health outcomes for fetuses and infants, such as abortion, premature birth, low birth weight, and delayed growth and development (8, 9). However, few studies have explored prenatal depression in women in the middle and late stages of pregnancy in China. A previous study found that high resilience can maintain the hypothalamus-pituitary-adrenal axis at an optimal level of activation, making it easier for resilient individuals to avoid psychosomatic disorders such as depression and anxiety (10). According to the social-ecological model, variables predicting the prevalence of prenatal depression can be categorized into individual factors (11) (such as demographic characteristics, pregnancy status, and worries and stress surrounding pregnancy), interpersonal factors (such as relationships with family members and emotional support), and coping and appraisal skills (such as positive psychological abilities, like resilience, that have the potential to enable women to resume normal functioning and engage in activities that help them respond effectively to the process of adaptation). It has been well documented that stress is highly associated with depression (12) among pregnant women. Previous studies have also revealed that worries resulting from pregnancy have emerged as factors that are strongly associated with mental health (13). Worries about fetal sex, appearance changes, and the negative impacts of pregnancy on daily life may have detrimental effects on the prevalence of prenatal depression. Women are susceptible to adverse effects of pregnancy, and, as a result, they experience both physical and psychological changes and negative effects on their daily lives, resulting in an increased risk of depression. Conversely, interpersonal factors, including emotional support and harmonious relationships with family members such as husbands, mothers, and mothers-in-law can positively affect the mental health of pregnant women (14, 15).
Depression can be regulated by positive psychological abilities like resilience. Resilience, as a personality trait and a positive psychological capability, can help individuals adapt to stressful environments or recover after facing difficulties (16). Women with high levels of resilience are flexible and can manage stress rationally to achieve positive psychological outcomes when faced with adversity. A growing number of studies have indicated that resilience acts as a protective factor for mental health and overall positive well-being and functioning in society (17, 18).
Research on prenatal mental disorders has only been conducted in a few regions in mainland China (19–21), including Shanghai and Chongqing. Multisite studies focusing on prenatal depression are relatively rare, especially for women in the second and third trimesters of pregnancy. Thus, this study aimed to evaluate the prevalence of prenatal depression experienced by Chinese pregnant women and explore its associated factors. The underlying hypothesis was that perceived stress and impacts on daily life, such as worries about fetal sex, worries about appearance, and changes to daily routines and relationships, would be positively associated with prenatal depression, but resilience and interpersonal factors, such as emotional support and harmonious relationships with husbands, mothers, and mothers-in-law, would be negatively associated with prenatal depression. The theoretical framework is outlined in Figure 1.
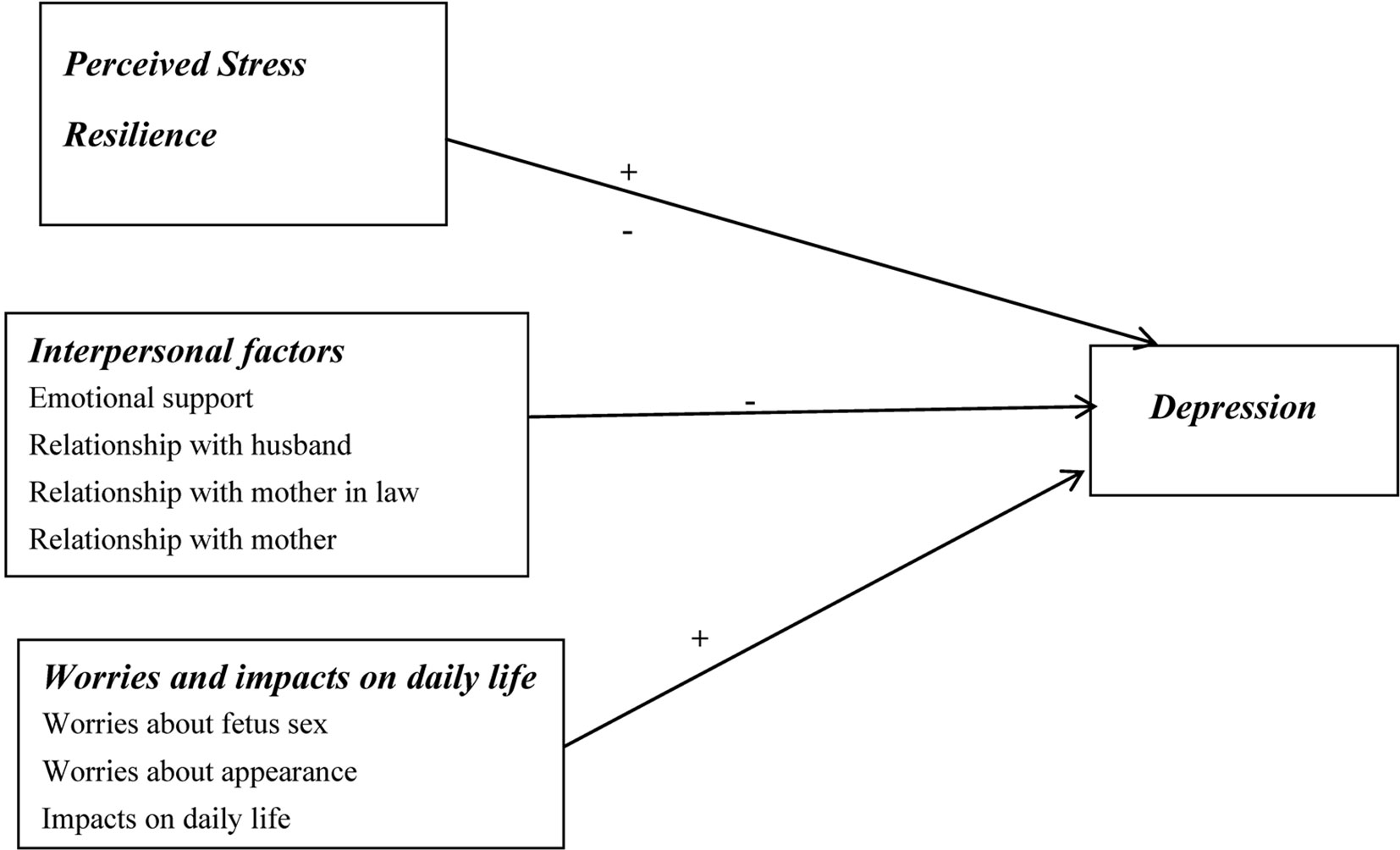
Figure 1 Theoretical framework of prenatal depression in pregnant women. +:Positive correlation; -: Negative correlation.
Materials And Methods
Study Design and Sample
A multisite smartphone questionnaire-based cross-sectional study with systematic sampling was performed between July 2018 and July 2019 in three cities (two provincial capital cities [Shenyang in Liaoning Province and Zhengzhou in Henan Province] and one municipality [Chongqing]). This study was conducted in accordance with and approved by the ethical standards of the Committee on Human Experimentation of China Medical University (CMU2018-033).
A total of 800 Chinese pregnant women in the middle and late stages of pregnancy seeking prenatal care who underwent routine prenatal examinations at the obstetrics clinics in tertiary hospitals (including the Second Affiliated Hospital of China Medical University, Zhengzhou Maternal and Child Health Hospital, and Chongqing Bishan District People’s Hospital) were recruited as participants. About 30% of the total pregnant women who underwent routine prenatal examinations at the obstetrics clinics in each hospital were randomly selected according to the outpatients clinic visit numbers. The inclusion criteria were: i) pregnant women aged 18 years or older seeking prenatal care who underwent routine prenatal examinations at the obstetrics clinics; ii) women who were legally married in mainland China; iii) confirmed gestation of 12 weeks or longer; and iv) women who could understand the content of the mobile phone questionnaires. The exclusion criteria were i) women with serious mental disorders or acute infectious diseases; ii) illicit drug use; iii) abnormal pregnancies such as fetal malformations or stillbirths; and iv) women who desired to have an abortion.
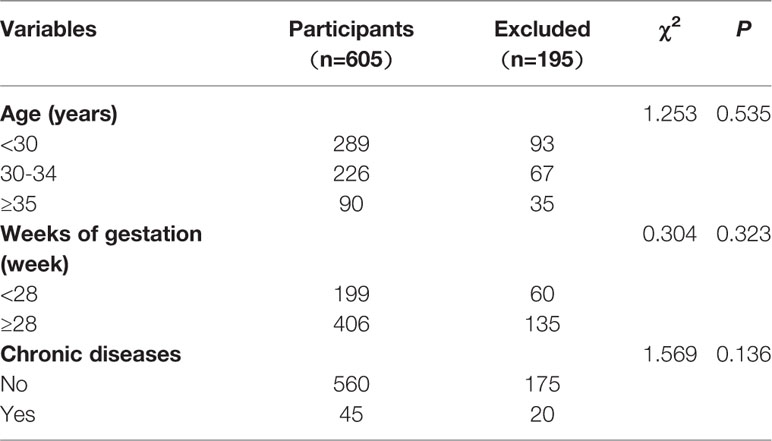
Pregnant women who participated in this study were asked to sign the online consent forms and were then enrolled in the study. The participants completed the online questionnaires using a mobile phone via Chinese WENJUANXING platform, and a trained surveyor of the research team was present to address questions and explain the purpose of this survey. Of the total 800 women identified, 195 declined to participate; the remaining 605 pregnant women took part and responded effectively in the study, resulting in a 75.63% effective consent rate. The characteristics (age, chronic disease status, and weeks of gestation) of the 605 pregnant women included in the analysis were similar to those of the 195 women who were excluded.
Measurements
Demographic Characteristics of Pregnant Women
Demographic characteristics of the pregnant women, including age, educational level (junior college and below, bachelor’s degree and above), monthly income (≤3,000 yuan, 3,001–5,000 yuan, > 5,000 yuan), weeks of gestation, and the presence of chronic diseases, were collected. Chronic disease was assessed through the question: “Are you suffering from any of the following diseases: cancer, cardiovascular disease, diabetes, arthritis, chronic kidney disease, or stomach disease?”, to which a respondent could respond “yes” or “no”.
Interpersonal Factors
Interpersonal factors included emotional support, relationship with husband, relationship with mother, and relationship with mother-in-law. Emotional support was assessed by asking whether or not the respondent could receive emotional support and concern from family members or friends during pregnancy (no/yes). Relationship with husband, relationship with mother, and relationship with mother-in-law were assessed by asking whether these relationships were harmonious (harmonious/not harmonious).
Worries and Impacts on Daily Life
Worries and impacts on daily life included worries about fetal sex, worries about appearance, and changes to daily life. Respondents were asked whether or not they were worried about the sex of the fetus or their physical appearance due to pregnancy (no/yes) and whether or not pregnancy had impacted their daily life (no/yes).
Measurement of Perceived Stress
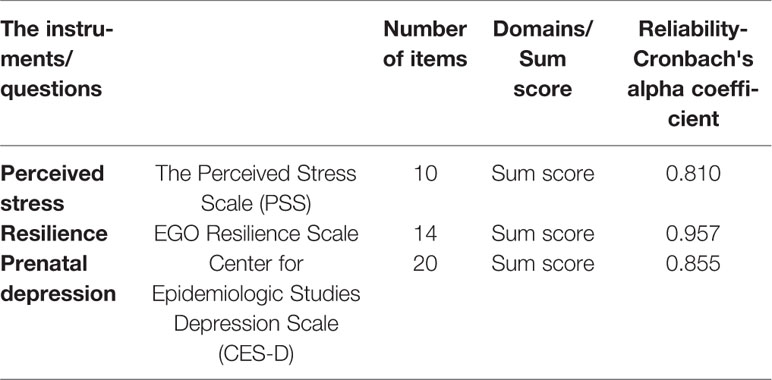
The Perceived Stress Scale (PSS), which was used to measure the perception of stress (22), consists of 10 items involving questions about one’s feelings and thoughts in the past month. Each item is answered on a five-point Likert scale ranging from 0 (never) to 4 (very often). The overall score ranges from 0 to 40, with higher scores indicating higher levels of perceived stress. The Cronbach’s alpha coefficient for this scale in this study was 0.810.
Measurement of Resilience
The 14-item Ego Resilience Scale was applied to assess resilience (23). Each item was rated on a seven-point scale ranging from 1 (strongly disagree) to 7 (strongly agree). Higher scores represent better levels of resilience. This scale has been widely used in previous studies in China with satisfactory reliability (24). The Cronbach’s alpha coefficient for this scale in this study was 0.957.
Measurement of Prenatal Depression
Depression symptoms were measured using the 20-item Center for Epidemiologic Studies Depression Scale (CES-D) (25), a questionnaire that has commonly been used to measure depression in China. Pregnant women reported their feelings and experiences with regard to depression and behaviors to cope with it “during the past few weeks” at any stage during their pregnancy. Each item was scored using a range from 1 (strongly disagree) to 7 (strongly agree). Summed CES-D scores of 16 or higher indicate that individuals are suffering from depression. The Cronbach’s alpha coefficient for this scale in this study was 0.855.
Data Analysis
The distribution of CES-D scores, which was organized into categorical variables, was evaluated using the chi-squared test. The kappa test was used to evaluate the predictive variables, and the results of all kappa values were under 0.50, which implied no agreement, and the variables were not adjusted in the multivariate analysis. Multivariate logistic regression analysis was performed to determine risk factors associated with prenatal depression. The statistical analyses were conducted using SPSS statistical software for Windows version 17.0 (SPSS, Inc., Chicago, IL). A two-tailed P-value of less than 0.05 was considered to be statistically significant.
Results
Descriptions of Demographic Characteristics of Pregnant Women
The demographic characteristics of the participants are shown in Table 1. A total of 605 pregnant women at 12 to 40 weeks of gestation participated in the study. There were no significant differences in the demographic characteristics (age, chronic disease status, and weeks of gestation) between the included 605 pregnant women and the 195 women who were excluded from the study (Table 2). The age of the participants ranged from 19 to 42 years old, with a mean age of 30 years. Most of the women (67.1%; 406) were at 28 or more weeks of gestation. Pregnant women who did not have harmonious relationships with their husbands, mothers, and mothers-in-law comprised 7.4% (45), 5.5% (33), and 19.5% (118) of the population, respectively. As shown in Table 1, scores of 26 and 80 were cut-off values for perceived stress and resilience, respectively. Thus, 52.9% (320) of participants experienced high levels of stress and 49.4% (299) reported high levels of resilience.
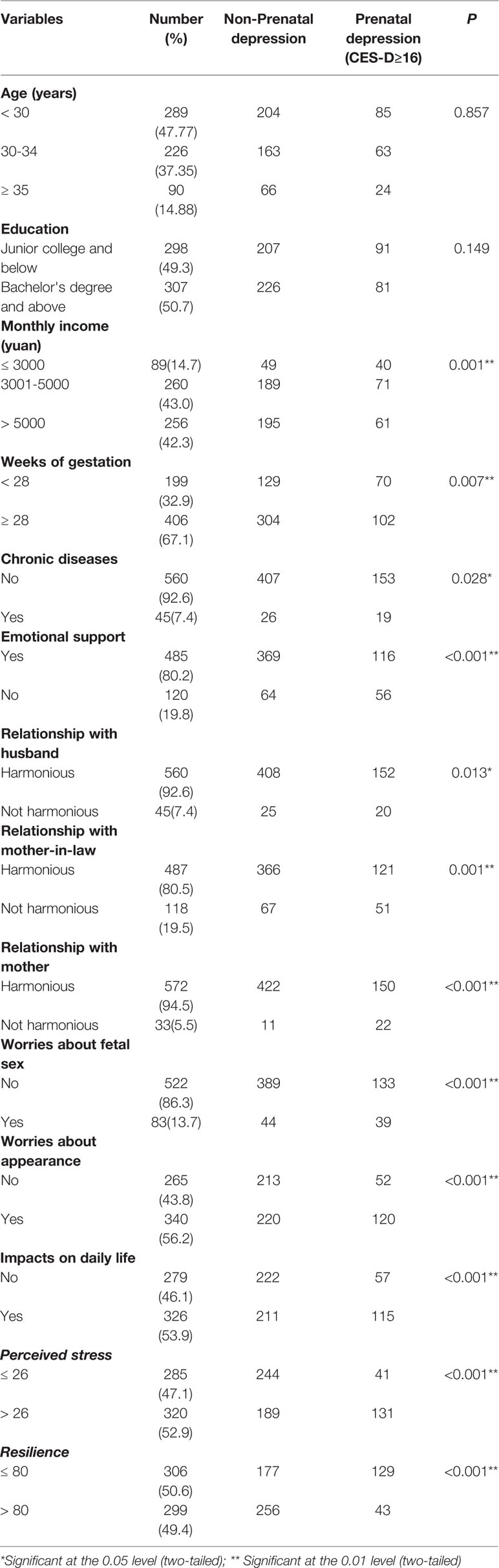
Table 1 The demographic characteristics of the participates and univariate analysis of factors related to prenatal depression of pregnant women (N=605).
Descriptions of Prenatal Depression in Pregnant Women
The prevalence of prenatal depression among Chinese pregnant women was 28.4%. The distribution of prenatal depression is presented in Table 1. Participants with a monthly income of less than 3,000 yuan had a higher prevalence of prenatal depression than women in other income groups (P < 0.01). Women whose gestation was less than 28 weeks had a higher prevalence of depression than women in later stages of pregnancy (P < 0.01), as did participants who suffered from chronic diseases (P < 0.05). Participants who could not receive emotional support from families and friends had a higher prevalence of depression than those who were able to receive support (P < 0.01). Participants who enjoyed harmonious relationships with their husbands, mothers, and mothers-in-law reported lower rates of prenatal depression than those who had poor relationships (P < 0.05). Additionally, participants who worried about their appearance, fetal sex, and pregnancy’s impacts on daily life had a higher prevalence of prenatal depression than those who did worry about such things (P < 0.01). Finally, women who had a higher level of perceived stress and a lower level of resilience had a higher rate of prenatal depression (P < 0.01). The Reliability Analysis of the Scales is provided in Table 3.
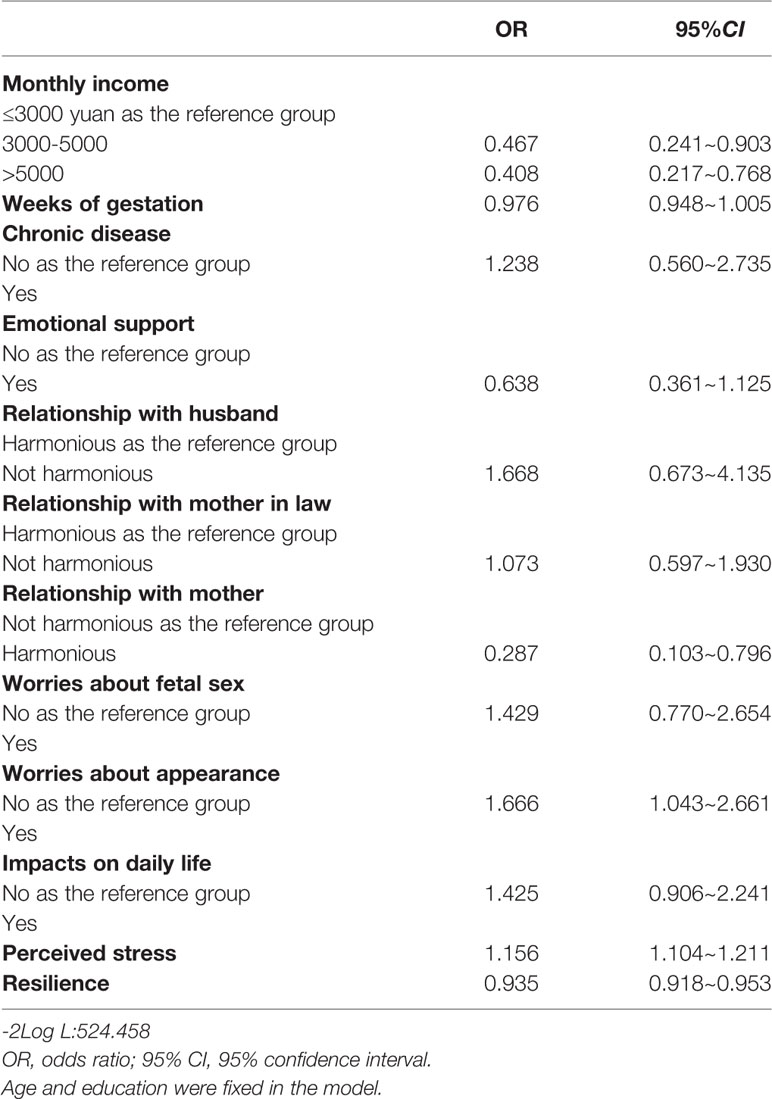
Predictors of Prenatal Depression
The results of multivariate logistic regression analyses of factors associated with prenatal depression are listed in Table 4. After adjusting for age and education, compared with a monthly income of less than 3,000 yuan, monthly incomes of more than 5,000 yuan (odds ratio [OR] 0.408, 95% confidence interval [CI] 0.217–0.768) and 3,000–5,000 yuan (OR 0.467, 95% CI 0.241–0.903) decreased the chance of suffering from prenatal depression. Worrying about appearance (OR 1.666, 95% CI 1.043–2.661) and higher levels of perceived stress (OR 1.156, 95% CI 1.104–1.211) increased the likelihood of prenatal depression. Pregnant women who had harmonious relationships with their own mothers (OR 0.287, 95% CI 0.103–0.796) and higher levels of resilience (OR 0.935, 95% CI 0.918–0.953) were less likely to experience prenatal depression.
Discussion
In this study, the prevalence of prenatal depression in women in the middle and late stages of pregnancy in China was 28.4%, which was higher than the prevalances in high-income countries such as the United States (15%), Australia (7%), Hong Kong (4.4%), and Finland (7.7%), as well as low-income countries such as Pakistan (64.6%), Bangladesh (18%), Nigeria (24.5%), and Ethiopia (24.94%) (26). However, the prevalence we observed was lower than that reported by a study in India (36.7%) (26). In mainland China, depression is often overlooked and untreated. However, the mental health of pregnant women should be emphasized, since it is closely associated with not only the health of women themselves but also the growth and development of the fetus (21, 27). The present findings show that a significant proportion of Chinese women are vulnerable to the negative impacts of pregnancy, which can lead to the development of prenatal depression. The lack of attention to the mental health of pregnant women results in a reduction in the quality of prenatal and postnatal care and a higher prevalence of maternal and fetal complications (21, 27). In Chinese society, married women account for a significantly high proportion of pregnant women with prenatal depression, thus, this study was conducted among married women.
In this study, prenatal depression was not only associated with worries about appearance and perceived stress but was strongly linked to harmonious relationships with mothers. Furthermore, resilience played a positive role in attenuating depression, as observed in previous studies that showed that resilience could mitigate adverse childhood experiences that might lead to prenatal depression (28). Also, in this study, demographic characteristics, such as low income, accounted for some of the risk for prenatal depression, which was in agreement with previous studies (29). Women with lower incomes encounter considerable economic challenges and financial hardships, which increases the likelihood of prenatal depression.
Prenatal depression was best predicted by harmonious relationships with mothers. Among pregnant women, good relationships with their own mothers were negatively associated with prenatal depression, implying that a harmonious relationship between a pregnant woman and her mother could act as a protective factor to reduce the negative influences of pregnancy and mitigate the development of depression. In fact, the better a woman’s relationship with her mother, the lower levels of depression she experienced. Pregnant women can also receive social support from their mothers and take advantage of available resources to combat the detrimental impacts of stress and attenuate symptoms of depression. Our findings are in agreement with previous studies indicating that support from mothers could decrease the risks of mental and physical health problems among pregnant women (30).
Worries about appearance were positively associated with prenatal depression. Women experience physical changes and hormonal fluctuations (31) during pregnancy, which could result in considerable changes in their physical appearance, and, subsequently, their mental health may be severely affected, increasing the appearance of symptoms of depression. Likewise, the extent of perceived stress was a strong predictor of depression and has tremendous detrimental effects on the mental health of pregnant women. Pregnancy is a major transition that imposes numerous stresses on women, adding to the risk of depression during the perinatal period. Previous international studies revealed that most pregnant women reported perceived stress during pregnancy (32). Comprehensive stress management should be considered a priority in order to relieve depression and improve overall well-being for pregnant women.
Notably, in this study, resilience was strongly and negatively associated with prenatal depression, serving to attenuate the deleterious effects of pregnancy on depression, which was in agreement with previous studies that found that resilience was negatively linked to prenatal depression (33). Resilience is a positive psychological characteristic that helps pregnant women appropriately cope with stress and adversity and take advantage of available resources to deal with pregnancy-related stress and recover from challenges. Resilience can be protective against depression: it facilitates an individual’s ability to rationally combat the harmful effects of psychological challenges and enhances her ability to maintain mental well-being. Prenatal depression can be mitigated by the positive psychological trait of resilience, which was confirmed by a previous study (20). Pregnant women with more resilience might recover more quickly from difficulties by accessing positive resources more readily. In my study, we concluded that resilience was acted as not only a stable state-like positive psychological capability, which could be changed and improved, but also as a personality trait. This was in agreement with the recent study of measuring resilience by generalizability theory in breast cancer (34). Thus, counseling and psychotherapy initiatives such as stress management and resilience-enhancement training should be provided for women to reduce the negative effects of pregnancy on the prevalence of prenatal depression.
Early detection of risk factors for prenatal depression among women during pregnancy is important in order to reduce the risk of developing depression. Worries about appearance and perceived stress were the strongest risk factors for prenatal depression. Interpersonal factors, such as harmonious relationships with mothers, and resilience, as a protective factor against depression, played important positive roles in relieving the detrimental effects of pregnancy on prenatal depression. It is of vital importance for pregnant women to improve resilience and build harmonious relationships to help them adjust to additional stress and worries, access positive resources, and avoid prenatal depression. This study will help provide insight into the identification of high-risk pregnant women with emotional distress, give evidence for clinical interventions to improve mental health for pregnant women, and establish holistic and humanized prenatal care policies.
This study has several strengths. First, the large sample size allowed this study to explore the relationships between prenatal depression and interpersonal factors, worries and impacts on daily life, perceived stress, and resilience among Chinese pregnant women. Second, face-to-face interviews and smartphone questionnaires provided a high response rate for this study and guaranteed the accuracy of the information. However, due to the cross-sectional design of this study, conclusions about causality between prenatal depression and related factors could not be derived. Thus, findings from the present study need to be confirmed in future prospective studies. Finally, this research was conducted only in the married pregnant women and urban areas in mainland China, which may not allow for the generalizability of our results to other populations of the pregnant women.
Ethics Statement
The research was conducted in accordance with the Declaration of Helsinki, as revised in 1989, and the protocol was approved by the Ethics Committee of China Medical University (CMU2018-033). All subjects gave their online informed consent for inclusion before participating in the study.
Author Contributions
LZ contributed to the design of the study, acquisition of data, and revision of the manuscript. JZ critically reviewed the manuscript and provided English edits. WZ and CC contributed to the acquisition of data and revision of the manuscript. FY, RM, and YJ contributed to the acquisition and interpretation of data. XY conceived and designed the study. All authors read and approved the final manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as potential conflict of interest.
Acknowledgments
The authors thank the pregnant women who shared their experiences for this study.
References
1. Martínez-Paredesa JF, Jácome-Pérez N. Depression in pregnancy. Rev Colombiana Psiquiatr (2019) 48(1):58–65. doi: 10.1016/j.rcp.2017.07.003
2. Biaggi A, Conroy S, Pawlby S, Pariante CM. Identifying the women at risk of antenatal anxiety and depression: A systematic review. J Affect Disord (2016) 191(18):62–77. doi: 10.1016/j.jad.2015.11.014
3. Priya A, Chaturvedi S, Bhasin SK, Bhatia MS, Radhakrishnan G. Depression, anxiety and stress among pregnant women: A community-based study. Indian J Psychiatry (2018) 60(1):151–2. doi: 10.4103/psychiatry.IndianJPsychiatry_230_17
4. Bennett HA, Einarson A, Taddio A, Koren G, Einarson TR. Precalence of depression during pregnancy:systematic review. Obstetr Gynecol (2004) 103(4):698–709. doi: 10.1097/01.AOG.0000116689.75396.5f
5. Lee AM, Lam SK, Sze Mun Lau SM, Chong CS, Chui HW, Fong DY. Prevalence, course, and risk factors for antenatal anxiety and depression. Obstetr Gynecol (2007) 110(5):1102–12. doi: 10.1097/01.AOG.0000287065.59491.70
6. Bennett HA, Einarson A, Taddio A, Koren G, Einarson TR. Prevalence of depression during pregnancy: A systematic review. Obstetricians Gynecol (2004) 103(4):698–709. doi: 10.1097/01.AOG.0000116689.75396.5f
7. Field T. Prenatal depression effects on early development: A review. Infant Behav& Develop (2011) 34:1–14. doi: 10.1016/j.infbeh.2010.09.008
8. Zhang Y, Muyiduli X, Wang S, Jiang W, Wu J, Li M, et al. Prevalence and relevant factors of anxiety and depression among pregnant women in a cohort study from south-east China. J Reprod Infant Psychol (2018) 36:519–29. doi: 10.1080/02646838.2018.1492098
9. Staneva A, Bogossian F, Pritchard M, Wittkowski A. The effects of maternal depression, anxiety, and perceived stress during pregnancy on preterm birth: a systematic review. Women Birth (2015) 28(3):179–93. doi: 10.1016/j.wombi.2015.02.003
10. Bublitz MH, Stroud LR. Childhood sexual abuse is associated with cortisol awakening response over pregnancy: preliminary findings. Psychoneuroendocrinology (2012) 37(9):1425–30. doi: 10.1016/j.psyneuen.2012.01.009
11. Stokols D. Translating social ecological theory into guidelines for community health promotion. Am J Health Promotion (1996) 10:282–99. doi: 10.1111/hsc.12693
12. Heyningen T, Honikman S, Myer L, Michael NO, Field S, Tomlinson M. Prevalence and predictors of anxiety disorders amongst low-income pregnant women in urban South Africa: A cross-sectional study. Arch Womens Ment Health (2017) 20(6):765–75. doi: 10.1007/s00737-017-0768-z
13. Pampaka D, Papatheodorou SI, AlSeaidan M, Wotayan RA, Wright RJ, Buring JE, et al. Depressive symptoms and comorbid problems in pregnancy - results from a population based study. J Psychosomatic Res (2018) 112:53–8. doi: 10.1016/j.jpsychores.2018.06.011
14. Nylen KJ, O’Hara MW, Engeldinger J. Perceived social support interacts with prenatal depression to predict birth outcomes. J Behav Med (2013) 36(4):427–40. doi: 10.1007/s10865-012-9436-y
15. Cheng ER, Rifas-Shiman SL, Perkins ME, Rich-Edwards JW, Gillman MW, Wright R, et al. The influence of antenatal partner support on pregnancy outcomes. J Women’s Health (2016) 25(7):672–9. doi: 10.1089/jwh.2015.5462
16. Newman R. APA’s resilience initiative. Prof Psychol: Res Pract (2005) 36(3):227–9. doi: 10.1037/0735-7028.36.3.227
17. Sheerin CM, Lind MJ, Brown EA, Gardner CO, Kendler KS, Amstadter AB. The impact of resilience and subsequent stressful life events on MDD and GAD. Depress Anxiety (2018) 35(2):140–7. doi: 10.1002/da.22700
18. Nygren B, Aléx L, Jonsén E, Gustafson Y, Norberg A, Lundman B. Resilience, sense of coherence, purpose in life and self-transcendence in relation to perceived physical and mental health among the oldest old. Aging Ment Health (2005) 9(4):354–62. doi: 10.1080/1360500114415
19. Tang X, Lu Z, Hu D, Zhong X. Influencing factors for prenatal stress, anxiety and depression in early pregnancy among women in Chongqing, China. J Affect Disord (2019) 253:292–302. doi: 10.1016/j.jad.2019.05.003
20. Ma X, Wang Y, Hu H, Tao X, Zhang Y, Shi H. The impact of resilience on prenatal anxiety and depression among pregnant women in Shanghai. J Affect Disord (2019) 250:57–64. doi: 10.1016/j.jad.2019.02.058
21. Li J, Mao J, Du Y, Morris JL, Gong G, Xiong X. Health-related quality of life among pregnant women with and without depression in Hubei, China. Mater Child Health (2012) 16:1355–63. doi: 10.1007/s10995-011-0900-z
22. Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav (1983) 12(24):385–96. doi: 10.2307/2136404
23. Isaksson M, Ghaderi A, Wolf-Arehult M, Ramklint M. Psychometric properties of the Swedish version of the Ego Resilience scale (ER) and a new shortened version of the Ego Undercontrol Scale (EUC). Curr Psychol (2018) 21:1–9. doi: 10.1007/s12144-018-0069-3
24. Shi M, Wang X, Bian Y, Wang L. The mediating role of resilience in the relationship between stress and life satisfaction among Chinese medical students: a cross-sectional study. BMC Med Education (2015) 15(16):1–7. doi: 10.1186/s12909-015-0297-2
25. Radloff LS. The CES-D scale: a self-report depression scale for research in the general population. Appl psychol Measurement (1977) 1(33):385–401. doi: 10.1177/014662167700100306
26. Sheeba B, Nath A, Metgud CS, Krishna M, Venkatesh S, Vindhya J, et al. Prenatal depression and its associated risk factors among pregnant women in Bangalore: a hospital based prevalence study. Front Public Health (2019) 7(108):1–9. doi: 10.3389/fpubh.2019.00108
27. Field T, Diego M, Dieter J, Hernandez-Reif M, Schanberg S, Kuhn C, et al. Prenatal depression effects on the fetus and the newborn. Infant Behav& Develop (2004) 27:216–29. doi: 10.1016/j.infbeh.2003.09.010
28. Johnson KM, Paley FM, Modest AM, Hacker MR, Shaughnessy S, Ricciotti HA, et al. An assessment of depression, psychosocial factors, and resilience among women seeking prenatal care at an urban community health center. Int Fed Gynecol Obstetr (2017) 10:1–6. doi: 10.1002/ijgo.12358
29. Chen L, Ding L, Qi M, Jiang C, Mao X, Cai W. Incidence of and social-demographic and obstetric factors associated with postpartum depression: Differences among ethnic Han and Kazak women of Northwestern China. Peer J (2018) 6:e4335. doi: 10.7717/peerj.4335
30. Vesile S, Melanie A, Oguz B, Robert S. Social support and antenatal depression in extended and nuclear family environments in Turkey: a cross-sectional survey. BMC Psychiatry (2011) 11(48):260–8. doi: 10.1186/1471-244X-11-48
31. Kumar P, Magon N. Hormones in pregnancy. Niger Med J (2012) 53:(4):179–83. doi: 10.4103/0300-1652.107549
32. Nima AA, Rosenberg P, Archer T, Garcia D. Anxiety, affect, self-esteem, and stress: mediation and moderation effects on depression. PloS One (2013) 8(9):e73265. doi: 10.1371/journal.pone.0073265
33. Howel KH, Miller-Graff LE, Schaefer LM, Scrafford KE. Relational resilience as a potential mediator between adverse childhood experiences and prenatal depression.r. J Health Psychol (2017) 25:1–13. doi: 10.1177/1359105317723450
Keywords: prenatal depression, perceived stress, resilience, worries about appearance, harmonious relationship
Citation: Zhang L, Yang X, Zhao J, Zhang W, Cui C, Yang F, Ma R and Jia Y (2020) Prevalence of Prenatal Depression Among Pregnant Women and the Importance of Resilience: A Multi-Site Questionnaire-Based Survey in Mainland China. Front. Psychiatry 11:374. doi: 10.3389/fpsyt.2020.00374
Received: 23 December 2019; Accepted: 15 April 2020;
Published: 06 May 2020.
Edited by:
Alexandre Andrade Loch, University of São Paulo, BrazilReviewed by:
Zeng Jie Ye, Guangzhou University of Chinese Medicine, ChinaMichaela Pascoe, Victoria University, Australia
Copyright © 2020 Zhang, Yang, Zhao, Zhang, Cui, Yang, Ma and Jia. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xiaoshi Yang, xsyang@cmu.edu.cn
 Lijuan Zhang1
Lijuan Zhang1 Xiaoshi Yang
Xiaoshi Yang