- 1Global Health Research Center, Guangdong Provincial People's Hospital, Guangdong Academy of Medical Sciences, Guangzhou, China
- 2Department of Information, Sun Yat-sen University Cancer Center, Sun Yat-sen University, Guangzhou, China
- 3Department of Medical Statistics, School of Public Health, Sun Yat-sen University, Guangzhou, China
Background: Healthcare workers (HCWs) have been exposed to increased risks of insomnia and fatigue during the COVID-19 pandemic. In this study, we identify important risk factors associated with insomnia symptoms and fatigue among HCWs, and evaluate the effect of organizational support on insomnia and fatigue symptoms.
Methods: This is an online cross-sectional survey of HCWs in China administered during the COVID-19 epidemic (from February 27, 2020 to March 12, 2020). We employed the AIS-8 scale for insomnia screening, and a self-reported ten-point scale to evaluate subjects' degrees of fatigue. We also designed a four-point scale to assess the degree of social support provided on an organizational level. Additionally, we conducted logistic regression analysis to identify risk factors.
Results: This study included a total of 3,557 participants, 41% of which consisted of non-frontline HCWs and 59% of which was frontline HCWs. Of the non-frontline HCWs, 49% reported insomnia symptoms, and 53.8% reported a moderate to high degree of fatigue. Meanwhile, among the frontline HCWs, the percentages for insomnia and moderate to high fatigue were 63.4% and 72.2%, respectively. Additionally, frontline HCWs and HCWs employed at Centers for Disease Control and Prevention (CDCs) had elevated risks of insomnia and fatigue. However, with increased organizational support, insomnia symptoms decreased among frontline HCWs. Also, organizational support mitigated the positive correlation between daily working hours and degree of fatigue among HCWs.
Conclusion: Frontline HCWs and staff in Chinese CDCs have been at a high risk of insomnia symptoms and fatigue during the fight against COVID-19. This study provides evidence for the positive effects of organizational support in relation to insomnia and fatigue among HCWs. This sheds light on government responses to the COVID-19 epidemic for other countries.
Introduction
The 2019 coronavirus (COVID-19) pandemic has been characterized by high transmissibility. As of April 3, 2020, it has caused 9.76 million infections and 50,414 deaths worldwide (1). To contain the epidemic within its borders, the Chinese government has declared the highest level of public health emergency alert, and has taken rapid and comprehensive action to limit its spread. This has included enacting strict quarantine measures, improving case identification, patient diagnosis, treatment, and psychological interventions, and improving the training of healthcare workers (HCWs), as well as strengthening logistical support and establishing units and hospitals for quarantined patients (2–5). Nationwide, these policies have resulted in millions of clinical staff, public health workers and other HCWs working consecutive days on the front lines during this period (6).
Front line HCWs have faced tremendous challenges during the COVID-19 epidemic. This has included an ever-increasing suspected and confirmed COVID-19 caseload, excessive workloads, isolation from friends and families, feelings of inadequate support, and discrimination (7). In such an unprecedented stressful situation, insomnia, feelings of fatigue, and even burn-out have been common. Insomnia has been the earliest and most prominent symptom reported by patients coping with stress (8), and fatigue has been the most common and persistent symptom caused by insomnia (9). These symptoms can result in daytime exhaustion, medical and psychiatric disorders, and lowered immune response among HCWs. Consequently, this elevates their risk of infection, and even death (10–12). Although only a few studies have reported data concerning insomnia and degree of fatigue among HCWs during the COVID-19 epidemic, these studies have identified several putative factors associated with both of these ailments.
For example, it has been documented that high levels of social support attenuate insomnia and fatigue symptoms associated with stress (13–15). In particular, previous studies have reported that organizational support improves job satisfaction for HCWs with high burnout levels (16). To help front line HCWs combat the challenges of this stressful situation, the Chinese government has launched a series of measures designed to support HCWs and their families. These measures have included providing protective equipment and training, improving subsidies, offering incentives, guaranteeing adequate daily necessities for HCWs and their families, shifting work schedules and providing psychological interventions (2). However, to date, no studies have examined the effect of organizational support on insomnia and fatigue among HCWs during the COVID-19 epidemic.
In addition, work-related factors and mental factors were also reported to be associated with insomnia and fatigue. For example, previous study shows that doctors whose inter-shift interval <10 h were more likely to be sleepless and fatigued (17). In Leblanc's study, psychological factors (include depression and anxiety) were found to the most important risk factors of new onset insomnia (18). Williamson et al. reported a negative association between fatigue and mental health measures (19). But the factors associated with insomnia and fatigue of HCWs in during the COVID-19 epidemic have not been well-understood.
In this study, we identify the factors associated with insomnia and fatigue among HCWs, and evaluate organizational support's effect on insomnia and fatigue in HCWs. To this end, we conducted an online cross-sectional survey during the COVID-19 epidemic. This report may be helpful for other countries dealing with the psychological problems and fatigue that HCWs face in the fight against COVID-19.
Methods
Study Design and Participants
We conducted an online cross-sectional survey targeting HCWs in China during the early stages of the COVID-19 epidemic (February 27, 2020 to March 12, 2020).
Participants were eligible if they: (1) were engaged in work related to healthcare, including, but not limited to, clinical doctors, nurses, medical laboratory staff, public health practitioners, health management personnel and healthcare research staff; and (2) were able to provide written informed consent. Those who were unable to complete the survey were excluded from participation.
The questionnaire was designed and piloted among HCWs before the online survey was deployed. A brief questionnaire which can be finished within 10 min was finalized to improve the acceptance of the survey. We employed a popular electronic survey tool (Wenjuanxing, Changsha Ranxing Information Technology Co. Ltd, China) to generate a link to the online questionnaire. Participants were recruited through peer referral. The questionnaire link was disseminated via WeChat, a popular social media platform in which users register with a unique phone number. We performed online written informed consent before the survey to ask whether participants would like to participate. It included the aims, contents, risks and benefits of participating in this study. If they answered “yes,” the survey would begin. Otherwise, the survey was terminated. Once a participant submitted the questionnaire, he or she would not be able to access it again.
Ethical Approval
This study has been approved by the ethical committee at Sun Yat-sen University [(2020) No. 011].
Measures
Insomnia and Fatigue (Dependent Variables)
We used the Athens Insomnia Scale-8 (AIS-8) to assess risk of insomnia. This instrument was developed in 1985 based on the International Classification of Diseases-10 criteria, and it has been used in many evaluations of insomnia severity (20–22). The scale contains eight items which were coded on a scale from 0 to 3 (0 = none, 1 = mild, 2 = significant, 3 = severe). A cut-off point of six was used to identify participants who had insomnia. Previous studies have demonstrated this scale's reliability and validity (23). Accordingly, the instrument in this study demonstrated good internal consistency (Cronbach's α = 0·89).
Participants were asked to evaluate their degree of fatigue during the previous week. We used a brief continuous numerical scale ranging from 0 to 10 for evaluation (0 = no fatigue, 10 = burn out).
Independent Variables
Participants' demographic information was collected, including sex, age, educational attainment, marital status, occupation(s), job title(s) and employer. Participants were also asked to describe their role in the COVID-19 response effort (1 = front line healthcare worker, 2 = non-front line healthcare worker). Front line HCWs were defined as those directly engaged in work related to the detection, testing, diagnosis and treatment of COVID-19 patients.
Data were also collected regarding work-related factors, including daily working hours, shift length and hours of sleep per day.
Participants were asked the extent to which they perceived support from organizations (this included government offices, state-owned enterprises, and private companies) and individuals (including friends, colleagues and their families). We designed a four-point scale to measure perceived degree of social support. Each grade was coded on a scale from 0 to 3 (0 = not at all, 1 = low, 2 = moderate, 3 = high). Participants could answer “not applicable” where appropriate.
We used the Patient Health Questionnaire-9 (PHQ-9) to assess the presence of major depressive disorder. In total, this instrument includes nine items coded on a scale from 0 to 3 (0 = not at all, 1 = several days, 2 = more than half of the days, 3 = nearly every day). Total scores ranged from 0 to 27, and a higher score suggested the presence of more severe depressive disorder. A cutoff point of five has been previously validated as an appropriate threshold for depression screening (24). Anxiety was measured using the Generalized Anxiety Disorder scale-7 (GAD-7). This instrument is a seven-item scale coded from 0 (none) to 3 (nearly every day). It is based on DSM-IV criteria. Participants were identified as having anxiety if they scored higher than four points.
Statistical Analysis
The primary outcomes of this study were insomnia (AIS-8 score > 6) and moderate to high degree of fatigue (fatigue scale score ≥ 5). Descriptive data are presented according to the distribution of the variables. Logistic modeling was used to compare participants' contributions to COVID-19 response efforts to their risk of insomnia and fatigue. In step 1, the correlation between participants' roles and the outcomes was tested, controlling for demographic variables (Model 1). In step 2, work-related factors were added, and their potential correlations with the outcomes were considered (Model 2). In step 3, other psychological factors were incorporated into the model, since there were strong correlations between the psychological factors (Model 3). In step 4 (Model 4), social support variables were added to assess how they influenced outcomes. With regard to fatigue, insomnia was also added as an associated factor, since previous studies have documented its correlation with fatigue (9). Finally, interactions between organizational support and participants' roles, work-related factors and mental health statuses were introduced to explore the modifying effects of social support. Modifying factors with a two-tailed p-values < 0.05 were considered significant, and are presented. Odds ratios (OR) and 95% confidence intervals (CIs) are reported for all models. All analysis was conducted with SAS 9.4 (SAS Institute Inc., Cary, NC).
Results
Characteristics
For this study, a total of 3,619 individuals were recruited to participate in the online survey. After excluding those who were not healthcare workers (62/3,619, 1.7%), a total of 3,557 participants were eligible for subsequent analysis.
Of all eligible participants, 59% (2,099/3,557) worked on the front lines of containment efforts related to the COVID-19 epidemic in China. Participants were predominantly female (2,460/3,557, 69.2%), had bachelor's degrees (1,973/3,557, 55.5%), and were married (2,520/3,557, 70.8%). The majority of the participants were either clinical doctors (1,342/3,557, 37.7%) or nurses (1,333/3,557, 37.5%). Public health practitioners accounted for 8% (285/3,557) of the participants. Consistent with this finding, 85% (3,026/3,557) of participants were working in hospitals, while 230 (6.5%) were working in centers for disease control and prevention (CDCs). Most of the participants reported working over 8 h per day (73.3%). Also, most participants had received a moderate to high degree of social support from organizations and individuals; median scores were 3.0 (2.0, 3.0) and 2.7 (2.0, 3.0), respectively (Table 1).
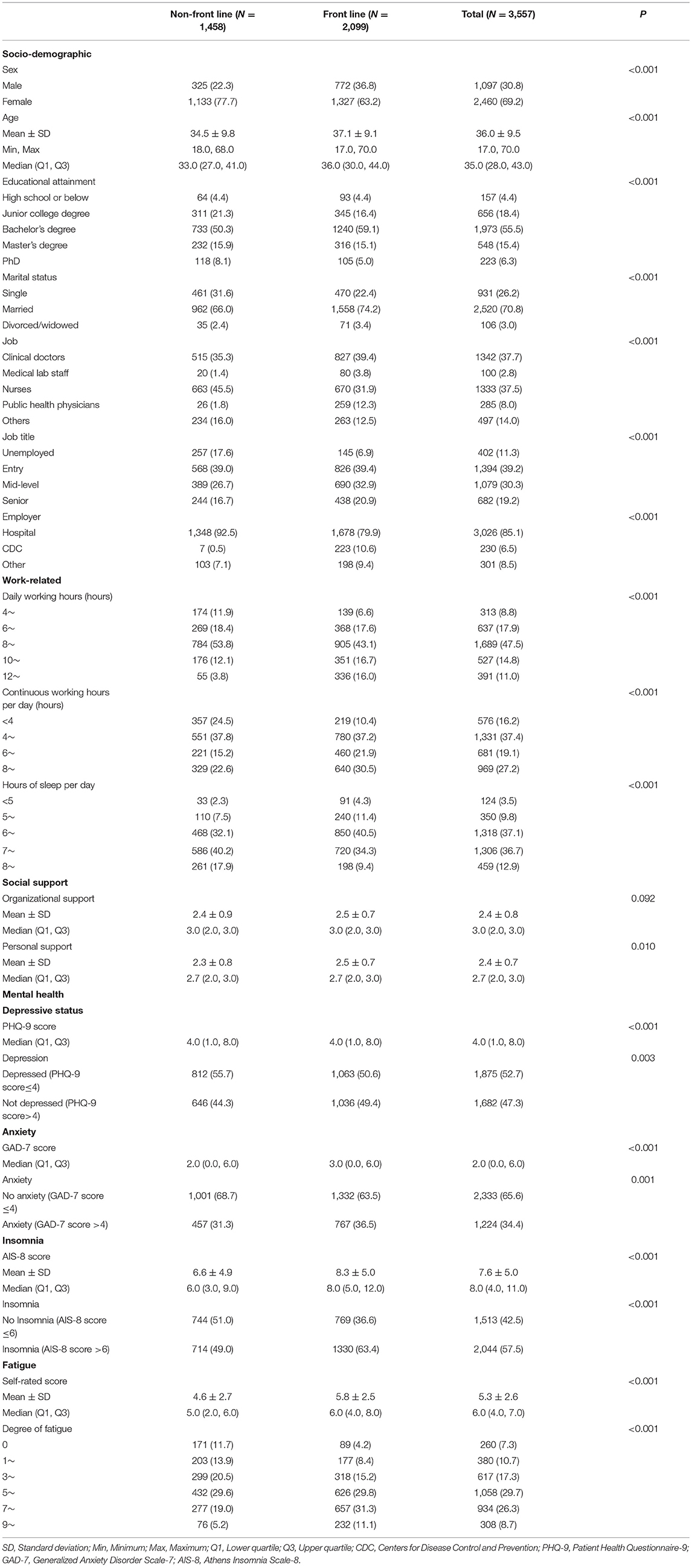
Table 1. Participants' socio-demographic factors, work-related factors, social support, mental health, insomnia and fatigue (N %).
Insomnia and Fatigue
The majority (2,044/3,557, 58%) of the participants suffered from insomnia, based on the AIS-8 scale. Front line HCWs were more likely than non-front line HCWs to have insomnia symptoms (1,330/2,099, 63% and 714/1,458, 49%, respectively). Similarly, 72% (1,515/2,099) of front line HCWs reported a moderate to high (score ≥ 5) degree of fatigue. This suggests that this group is more likely to report severe fatigue than non-front line HCWs (785/1,458, 53.8%). Eight point Seven percentage percent of respondents reported feeling burned out or nearly burned out (score ≥ 9: 308/3,557) (Table 1).
Factors Associated With Insomnia
As presented in Table 2, front line HCWs (OR = 1.62, 95% CI = 1.40–1.87) had higher odds of reporting insomnia symptoms than non-front line HCWs. HCWs who were married (OR = 1.60, 95% CI = 1.31–1.97) or divorced/widowed (OR = 1.84, 95% CI = 1.16–2.91) were found to be at higher risk of insomnia than unmarried HCWs. HCWs who worked in CDC facilities (OR = 2.11, 95% CI = 1.42–3.13) were found to be at higher risk of insomnia than those employed in hospital settings. Younger HCWs (OR = 0.99, 95% CI = 0.97–1.00) also had lower risks of insomnia, as did those who had obtained PhDs (OR = 0.48, 95% CI = 0.30–0.76) relative to those who had only completed middle-or high-school (Table 2, Model 1).
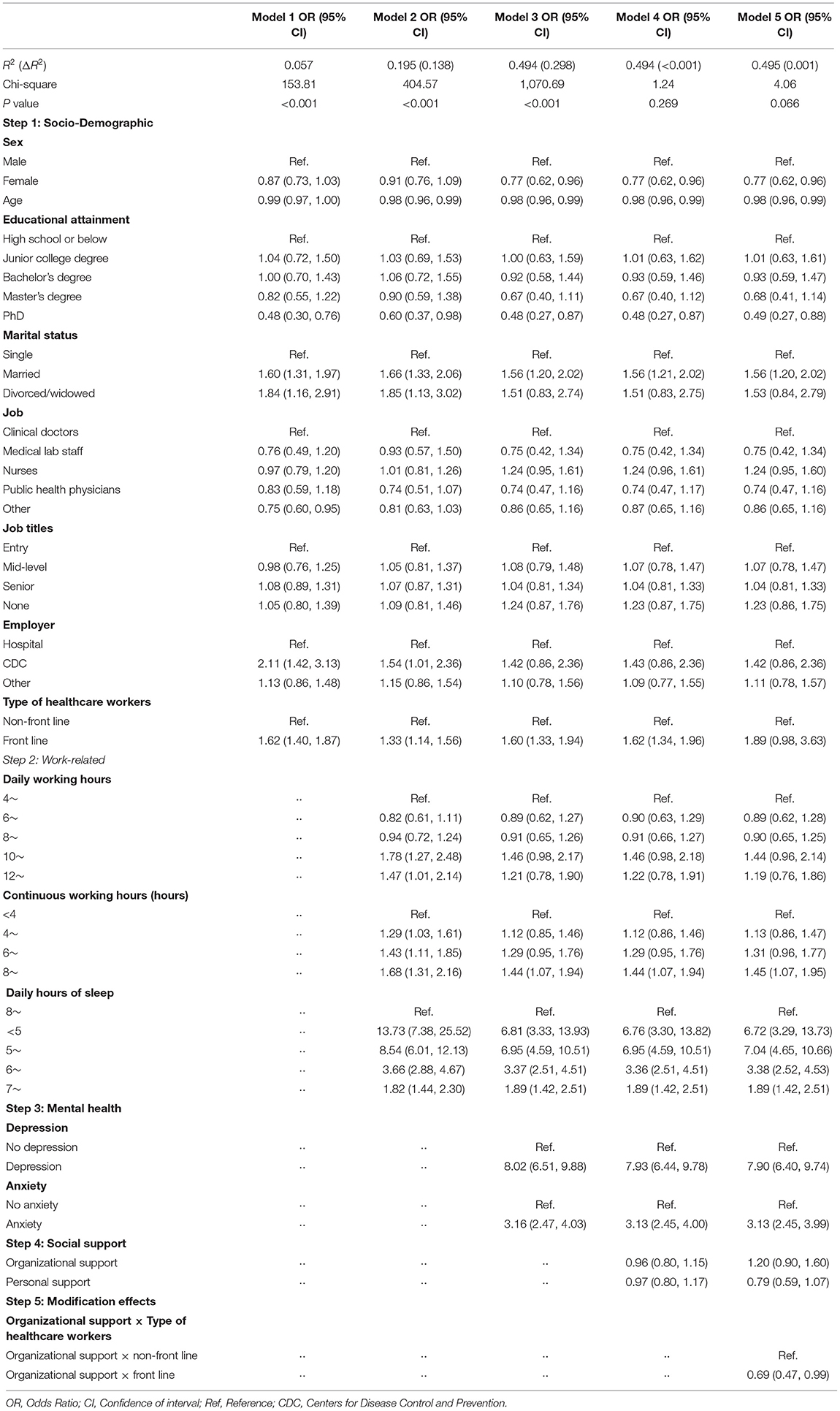
Table 2. Logistic regression of factors correlated with insomnia among healthcare workers during the COVID-19 epidemic.
Work-related factors contributed an additional 13.8% of the observed variance in insomnia symptoms. HCWs who worked 10–12 h per day (OR = 1.78, 95% CI = 1.27–2.48) and those who worked 12 h or more per day (OR = 1.47, 95% CI = 1.01–2.14) were at higher risk of insomnia than those who worked 4–6 h per day. Those who worked longer shifts were also more likely to be at risk of insomnia (4~ h vs. <4 h: OR = 1.29, 95% CI = 1.03–1.61; 6~ h vs. <4 h: OR = 1.43, 95% CI = 1.11–1.85; 8~ h vs. <4 h: OR = 1.68, 95% CI = 1.31–2.16). Additionally, lack of sleep was correlated with insomnia. HCWs who slept <5 h were 13.73 times more likely to report insomnia symptoms than those who slept over 8 h (OR = 13.73, 95% CI = 7.38–25.52) (Table 2, Model 2).
Psychological factors explained 29.8% of the variance in reported insomnia symptoms. HCWs who had depressive symptoms (OR = 8.02, 95% CI = 6.51–9.88) and those who had anxiety symptoms (OR = 3.16, 95% CI = 2.47–4.03) had higher risks of insomnia (Table 2, Model 3).
Social support only accounted for ~0.1% of the variance in reported insomnia symptoms (Table 2, Model 4). However, organizational support modified the correlation between a HCW's role and their risk of insomnia (OR = 0.69, 95% CI = 0.47–0.99) (Table 2, Model 5). With increasing organizational support, the risk of insomnia among front line HCWs declined, and the difference in insomnia risk between front line and non-front line HCWs decreased even more. Meanwhile, there was no significant influence of organizational support among non-front line HCWs (Figure 1A).
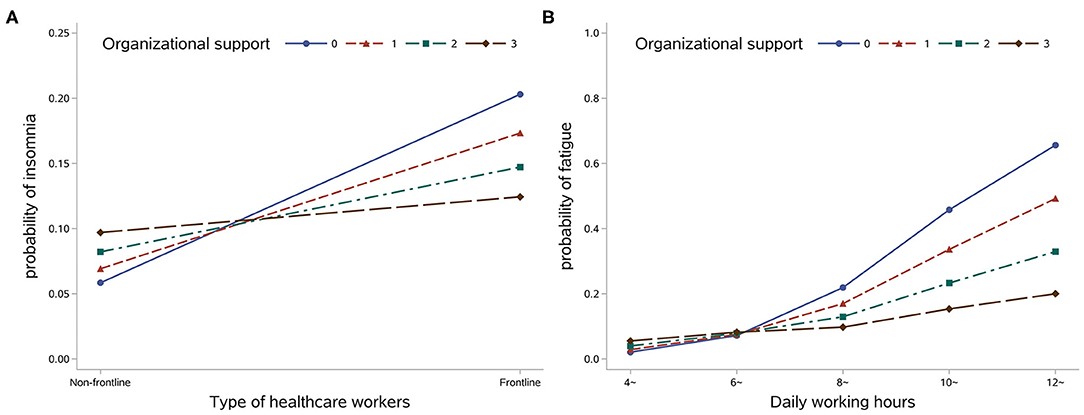
Figure 1. Predicted probability of insomnia among different types of healthcare worker by organizational support level (A) and predicted probability of moderate to high degree of fatigue among different types of healthcare worker by organizational support level (B).
Factors Associated With Fatigue
The HCWs roles were also associated with fatigue in all models. Front line HCWs (OR = 1.83, 95% CI = 1.58–2.13) were at higher risk of reporting fatigue than non-front line HCWs. Additionally, HCWs who worked in CDCs were more likely to feel fatigued than those who worked in hospitals (OR = 3.59, 95% CI = 2.16–5.97) (Table 3, Model 1).
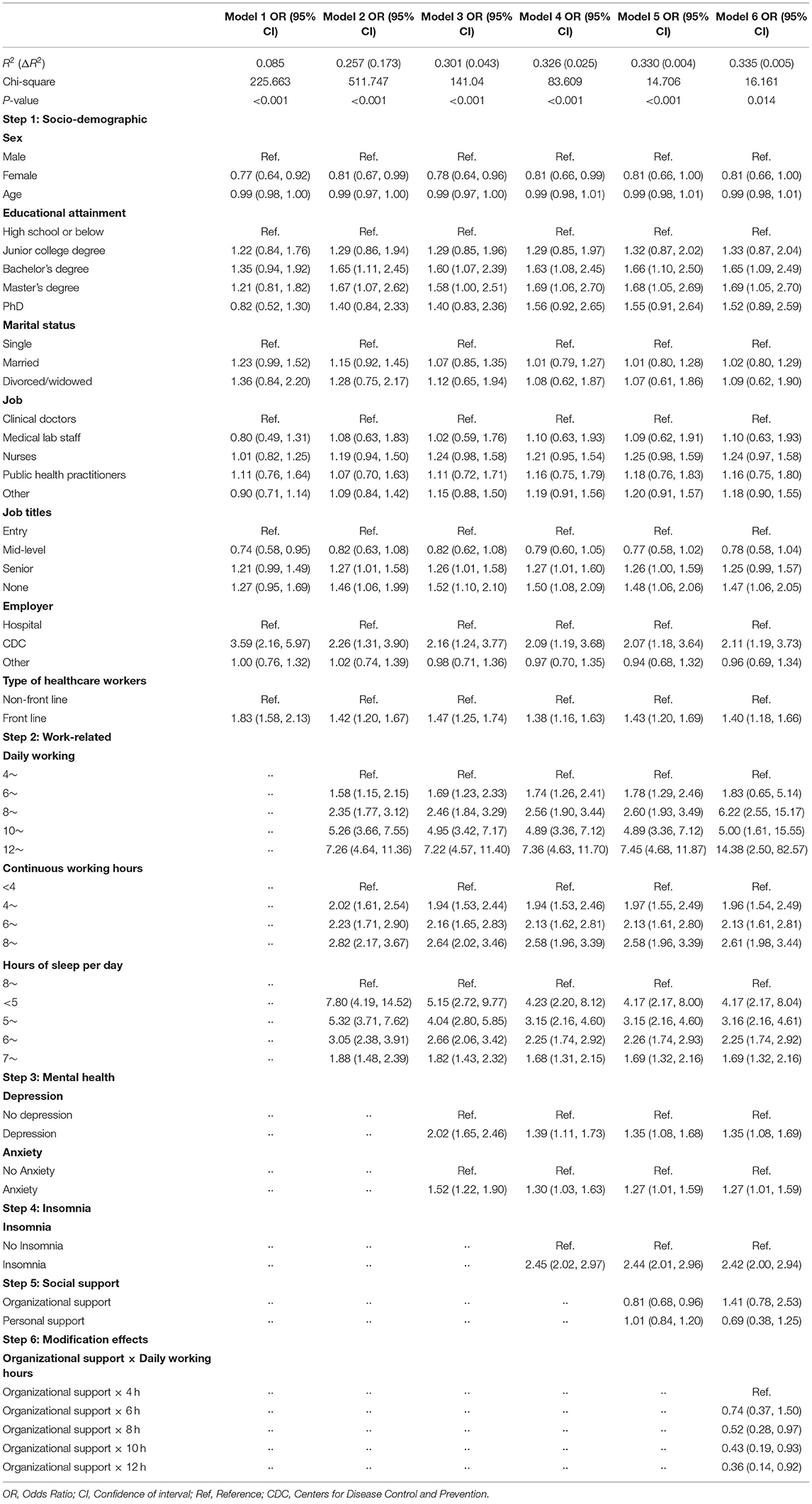
Table 3. Logistic regression of factors correlated with fatigue among healthcare workers during the COVID-19 epidemic.
Work-related factors made the greatest contribution (17.3%) to reported degree of fatigue. Compared with those who worked 4–6 h per day, HCWs who worked more than 12 h per day had the highest odds of reporting fatigue (OR = 7.26, 95% CI = 4.64–11.36). Similarly, compared to those who worked <4 h per day, HCWs who worked 4 continuous hours or more per day were more likely to report a higher degree of fatigue. Compared with those who slept 8 h or more per day, HCWs who slept <8 h per day had higher odds of reporting fatigue (<5 vs. 8~ h: OR = 7.80, 95% CI = 4.19–14.52; 5~ vs. 8~ h: OR = 5.32, 95% CI = 3.71–7.62; 6~ vs. 8~ h: OR = 3.05, 95% CI = 2.38–3.91; 7~ vs. 8~ h: OR = 1.88, 95% CI = 1.48–2.39) (Table 3, Model 2).
Psychological factors accounted for 4.3% of the variance in reported feelings of fatigue. Depressive symptoms (OR = 2.02, 95% CI = 1.65–2.46) and anxiety (OR = 1.52, 95% CI = 1.22–1.90) were considered risk factors for fatigue (Table 3, Model 3). Additionally, insomnia was associated with feelings of fatigue (OR = 2.45, 95% CI = 2.02–2.97), but only explained 2.5% of the total variance (Table 3, Model 4).
Similar to the results regarding insomnia, social support explained an additional 0.4% of the variance in reported feelings of fatigue (Table 3, Model 5). It also modified the correlation between daily working hours and feelings of fatigue (Table 3, Model 6). Organizational support mitigated the positive association between daily work hours and degree of fatigue (Figure 1B).
Discussion
This study reported that 49 and 63.4% of non-front line and front line HCWs, respectively, experienced insomnia. Moreover, health practitioners employed in CDCs had higher risk of insomnia, and reported a higher degree of fatigue, than clinical doctors. Our results suggest that organizational support modifies the association between HCWs' role and insomnia. It also mitigates the positive correlation between working hours and reported feelings of fatigue.
The percentage of participants reporting symptoms of insomnia in our study exceeded those reported in other studies (34.0~38.4%) (7, 25). This may partly be explained by the different scales [e.g., Insomnia Severity Index (ISI)] for assessing insomnia severity. Several studies have suggested a higher sensitivity when diagnosing insomnia with the AIS-8 than with the ISI. Moreover, AIS-8 has shown superior diagnostic performance in detecting health outcomes associated with insomnia (26, 27). This study reports that during the COVID-19 epidemic, 53.8 and 72.2% of non-front line and front line HCWs, respectively, reported feeling moderate to high degrees of fatigue, and about 10% of participants reported being near exhaustion. These percentages were similar to those obtained in a previous study of self-reported fatigue among HCWs during the SARS outbreak (70.3%) (26). These high percentages for insomnia and feelings of fatigue should be noted as early alerts for additional psychological problems.
Health practitioners working in CDCs, who were critical to curbing the COVID-19 epidemic in China, were at an even higher risk of developing insomnia symptoms than were clinical doctors working in hospitals. During the crisis, HCWs in CDCs were tasked with administrative responsibilities and needed to undertake efforts to contain the disease. They were engaged in work related to disease surveillance, case finding, reporting, close contact tracing, investigation, laboratory testing, disinfecting high-risk public places, health education, training and policy-making (27). Heavy workload and exposure to extreme stress put them at high risk for insomnia and fatigue.
In this study, we found that psychological problems (depression and anxiety) accounted for the largest proportion (29.9%) of variance in reported insomnia symptoms, but only contributed slightly to variance in reported feelings of fatigue (4.4%). Current evidence suggests that the relationship between insomnia and depression can be bidirectional (28). Previous study reported that about 20% of patient with insomnia presented depressive symptoms (29, 30). Insomnia symptoms may have predictive value for subsequent development of depression (31). Other studies reported continued insomnia may become chronic despite successful resolution of depressive symptoms (32). Among those who firstly get insomnia and depression, 29% of patients' insomnia symptoms developed after depressive symptoms (33). Most researchers agreed that mutual effect exist between insomnia and depression (34, 35). Previous studies have reported that fatigue is the most common symptom of insomnia (9, 36). However, we found that insomnia only explained a small proportion (2.4%) of the variance in feelings of fatigue, with these feelings predominantly explained by work-related variables (17.5%). We highlight the need to identify insomnia symptoms in HCWs, and take measures to provide early intervention for psychological problems, considering that a large proportion of the variance in insomnia symptoms can be explained by depression and anxiety. Although the Chinese government has launched a series of measures related to psychological intervention, there remains a need for further studies to evaluate their effects.
A strong association was also shown between work-related factors and both insomnia and fatigue. We found that as daily working hours increased, the risk of insomnia spiked. Similar results have also been reported in other studies conducted during the COVID-19 epidemic. This evidence reveals a close relationship between work overload and insomnia; overload's effect on sleep disturbance can be considerable, especially in working populations (37). Daily working hours was also found to be positively correlated with fatigue, which is consistent with a previous study (38). Moreover, in addition to daily working hours, longer continuous working hours also contributed to insomnia symptoms and feelings of fatigue. During the early stages of the COVID-19 epidemic, HCWs often worked longer each day. Under these circumstances, breaks were crucial to alleviating fatigue (39). In line with previous research, insomnia symptoms and feelings of fatigue were found to be inversely correlated with sleep duration (40). Of note, the odds of insomnia and fatigue spiked when sleeping hours decreased, especially for HCWs who reported sleeping <5 h per day.
At the outset of the COVID-19 epidemic, scarcities of both HCWs and resources made it difficult to divide work shifts between HCWs and to ensure adequate rest. During this stressful situation, organizational support attenuated the positive correlation between working hours and fatigue. This implies that political commitment from the government and broad community participation promote anti-epidemic work (41). The Chinese government has taken several key measures to combat the COVID-19 epidemic, along with implementing additional supporting measures (42). Adequate training, as well as logistical support for HCWs, has been shown to reduce their fears of infection (2, 43). Psychological interventions may also mitigate mental health problems (44). Services provided to HCWs' families could reduce their worries about their families. With a growing number of HCWs participating in the fight against COVID-19, HCWs have gained peer support and had their workloads reduced. All of these measures could mitigate the fatigue symptoms caused by both workload and psychological problems. Organizational support could also attenuate insomnia symptoms. Of note, front line HCWs who faced more stressors were more likely to have insomnia symptoms, and they also received more organizational support. The results of this study suggest that organizational support mitigates insomnia symptoms among front line HCWs.
This study has several limitations. Firstly, participants were not selected as a representative sample of HCWs in China. Secondly, HCWs who were under extreme stress or an extreme workload were less likely to participate in the survey, potentially leading to an underestimation of insomnia and fatigue. Thirdly, questionnaires were shortened to increase the completion rate, meaning that several potential associated factors were not included in this study.
Conclusion
Front line HCWs in the fight against COVID-19 have reported both insomnia symptoms and feelings of fatigue. Organizational support is negatively correlated with the risk of insomnia symptoms, and mitigates the positive correlation between working hours and degree of fatigue in front line HCWs.
Data Availability Statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.
Ethics Statement
The studies involving human participants were reviewed and approved by the ethical committee of Sun Yat-sen University [(2020) No. 011]. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
LL, WC, and XZ designed the study. LL, WC, JY, SL, YY, and FZ collected the data, and SL conducted data analysis. XZ drafted the paper. LL, XZ, SL, JL, YY, and FZ contributed to paper revisions. All authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
We would like to thank Yin Liu, Qian Lu, Muyang Chu, Shangqing Tang, Shuxian Wu, Chaofan Xu, and Dexin Zhou at the School of Public Health, Sun Yat-sen University, for their contribution to data collection, and Rong Peng for her valuable suggestions on this study.
References
1. WHO. WHO Coronavirus Disease (COVID-19) Dashboard: World Health Organization. (2020). Available online at: https://covid19.who.int/ (accessed April 23, 2020)
2. Kang L, Li Y, Hu S, Chen M, Yang C, Yang BX, et al. The mental health of medical workers in Wuhan, China dealing with the 2019 novel coronavirus. Lancet Psychiatry. (2020) 7:e14. doi: 10.1016/S2215-0366(20)30047-X
3. Xiang YT, Yang Y, Li W, Zhang L, Zhang Q, Cheung T, et al. Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. Lancet Psychiatry. (2020) 7:228–9. doi: 10.1016/S2215-0366(20)30046-8
4. Chen W, Wang Q, Li YQ, Yu HL, Xia YY, Zhang ML, et al. Early containment strategies and core measures for prevention and control of novel coronavirus pneumonia in China. Zhonghua Yu Fang Yi Xue Za Zhi. (2020) 54:239–44. doi: 10.3760/cma.j.issn.0253-9624.2020.03.003
5. Li W, Yang Y, Liu ZH, Zhao YJ, Zhang Q, Zhang L, et al. Progression of mental health services during the COVID-19 outbreak in China. Int J Biol Sci. (2020) 16:1732–8. doi: 10.7150/ijbs.45120
6. National Health Commission of the People's Republic of China. Healthcare Workers Fight Against Disease: National Health Commission of the People's Republic of China. (2020). Available online at: http://www.gov.cn/xinwen/2020-06/07/content_5517742.htm (accessed March 15, 2020).
7. Lai J, Ma S, Wang Y, Cai Z, Hu J, Wei N, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw Open. (2020) 3:e203976. doi: 10.1001/jamanetworkopen.2020.3976
8. Su TP, Lien TC, Yang CY, Su YL, Wang JH, Tsai SL, et al. Prevalence of psychiatric morbidity and psychological adaptation of the nurses in a structured SARS caring unit during outbreak: a prospective and periodic assessment study in Taiwan. J Psychiatr Res. (2007) 41:119–30. doi: 10.1016/j.jpsychires.2005.12.006
9. Kim SJ, Kim S, Jeon S, Leary EB, Barwick F, Mignot E. Factors associated with fatigue in patients with insomnia. J Psychiatr Res. (2019) 117:24–30. doi: 10.1016/j.jpsychires.2019.06.021
10. Marcks BA, Weisberg RB. Co-occurrence of insomnia and anxiety disorders: a review of the literature. Am J Lifestyle Med. (2009) 3:300–9. doi: 10.1177/1559827609334681
11. Bos SC, Macedo AF. Literature review on insomnia (2010–2016). Biol Rhythm Res. (2018) 50:94–163. doi: 10.1080/09291016.2017.1413766
12. Lovato N, Lack L. Insomnia and mortality: a meta-analysis. Sleep Med Rev. (2019) 43:71–83. doi: 10.1016/j.smrv.2018.10.004
13. Kamen C, Garland SN, Heckler CE, Peoples AR, Kleckner IR, Cole CL, et al. Social support, insomnia, and adherence to cognitive behavioral therapy for insomnia after cancer treatment. Behav Sleep Med. (2019) 17:70–80. doi: 10.1080/15402002.2016.1276019
14. Kim S, Suh S. Social support as a mediator between insomnia and depression in female undergraduate students. Behav Sleep Med. (2019) 17:379–87. doi: 10.1080/15402002.2017.1363043
15. Nakata A, Haratani T, Takahashi M, Kawakami N, Arito H, Kobayashi F, et al. Job stress, social support, and prevalence of insomnia in a population of Japanese daytime workers. Soc Sci Med. (2004) 59:1719–30. doi: 10.1016/j.socscimed.2004.02.002
16. Alcover CM, Chambel MJ, Fernández JJ, Rodríguez F. Perceived organizational support-burnout-satisfaction relationship in workers with disabilities: the moderation of family support. Scand J Psychol. (2018) 59:451–61. doi: 10.1111/sjop.12448
17. Tucker P, Brown M, Dahlgren A, Davies G, Ebden P, Folkard S, et al. The impact of junior doctors' worktime arrangements on their fatigue and well-being. Scand J Work Environ Health. (2010) 36:458–65. doi: 10.5271/sjweh.2985
18. Leblanc M, Mérette C, Savard J, Ivers H, Baillargeon L, Morin CM. Incidence and risk factors of insomnia in a population-based sample. Sleep. (2009) 32:1027–37. doi: 10.1093/sleep/32.8.1027
19. Williamson RJ, Purcell S, Sterne A, Wessely S, Hotopf M, Farmer A, et al. The relationship of fatigue to mental and physical health in a community sample. Soc Psychiatry Psychiatr Epidemiol. (2005) 40:126–32. doi: 10.1007/s00127-005-0858-5
20. Soldatos CR, Dikeos DG, Paparrigopoulos TJ. Athens insomnia scale: validation of an instrument based on ICD-10 criteria. J Psychosom Res. (2000) 48:555–60. doi: 10.1016/S0022-3999(00)00095-7
21. Kokras N, Kouzoupis AV, Paparrigopoulos T, Ferentinos P, Karamanakos P, Kontoyannis DA, et al. Predicting insomnia in medical wards: the effect of anxiety, depression and admission diagnosis. Gen Hosp Psychiatry. (2011) 33:78–81. doi: 10.1016/j.genhosppsych.2010.12.003
22. Bhaskar S, Hemavathy D, Prasad S. Prevalence of chronic insomnia in adult patients and its correlation with medical comorbidities. J Family Med Prim Care. (2016) 5:780–4. doi: 10.4103/2249-4863.201153
23. Soldatos CR, Dikeos DG, Paparrigopoulos TJ. The diagnostic validity of the athens insomnia scale. J Psychosom Res. (2003) 55:263–7. doi: 10.1016/S0022-3999(02)00604-9
24. Levis B, Benedetti A, Thombs BD, Collaboration DESD. Accuracy of patient health questionnaire-9 (PHQ-9) for screening to detect major depression: individual participant data meta-analysis. BMJ. (2019) 365:l1476–l. doi: 10.1136/bmj.l1476
25. Zhang WR, Wang K, Yin L, Zhao WF, Xue Q, Peng M, et al. Mental health and psychosocial problems of medical health workers during the COVID-19 epidemic in China. Psychother Psychosom. (2020) 89:242–50. doi: 10.1159/000507639
26. McAlonan GM, Lee AM, Cheung V, Cheung C, Tsang KW, Sham PC, et al. Immediate and sustained psychological impact of an emerging infectious disease outbreak on health care workers. Can J Psychiatry. (2007) 52:241–347. doi: 10.1177/070674370705200406
27. Deng SQ, Peng HJ. Characteristics of and public health responses to the coronavirus disease 2019 outbreak in China. J Clin Med. (2020) 9:575. doi: 10.3390/jcm9020575
28. Gao X, Meng LX, Ma KL, Liang J, Wang H, Gao Q, et al. The bidirectional causal relationships of insomnia with five major psychiatric disorders: a Mendelian randomization study. Eur Psychiatry. (2019) 60:79–85. doi: 10.1016/j.eurpsy.2019.05.004
29. Quera-Salva MA, Orluc A, Goldenberg F, Guilleminault C. Insomnia and use of hypnotics: study of a french population. Sleep. (1991) 14:386–91. doi: 10.1093/sleep/14.5.386
30. Weissman MM, Greenwald S, Niño-Murcia G, Dement WC. The morbidity of insomnia uncomplicated by psychiatric disorders. Gen Hosp Psychiatry. (1997) 19:245–50. doi: 10.1016/S0163-8343(97)00056-X
31. Riemann D. Primary insomnia: a risk factor to develop depression? J Affect Disord. (2003) 76:255–9. doi: 10.1016/S0165-0327(02)00072-1
32. Van Londen L, Molenaar RP, Goekoop JG, Zwinderman AH, Rooijmans HG. Three- to 5-year prospective follow-up of outcome in major depression. Psychol Med. (1998) 28:731–5. doi: 10.1017/S0033291797006466
33. Ohayon MM, Roth T. Place of chronic insomnia in the course of depressive and anxiety disorders. J Psychiatr Res. (2003) 37:9–15. doi: 10.1016/S0022-3956(02)00052-3
34. Manber R, Chambers AS. Insomnia and depression: a multifaceted interplay. Curr Psychiatry Rep. (2009) 11:437–42. doi: 10.1007/s11920-009-0066-1
35. Riemann D, Krone LB, Wulff K, Nissen C. Sleep, insomnia, and depression. Neuropsychopharmacology. (2020) 45:74–89. doi: 10.1038/s41386-019-0411-y
36. Theorell-Haglöw J, Lindberg E, Janson C. What are the important risk factors for daytime sleepiness and fatigue in women? Sleep. (2006) 29:751–7. doi: 10.1093/sleep/29.6.751
37. Yang B, Wang Y, Cui F, Huang T, Sheng P, Shi T, et al. Association between insomnia and job stress: a meta-analysis. Sleep Breath. (2018) 22:1221–31. doi: 10.1007/s11325-018-1682-y
38. Zhan YX, Zhao SY, Yuan J, Liu H, Liu YF, Gui LL, et al. Prevalence and influencing factors on fatigue of first-line nurses combating with COVID-19 in China: a descriptive cross-sectional study. Curr Med Sci. (2020) 40:625–35. doi: 10.1007/s11596-020-2226-9
39. Sagherian K, Steege LM, Cobb SJ, Cho H. Insomnia, fatigue and psychosocial well-being during COVID-19 pandemic: a cross-sectional survey of hospital nursing staff in the United States. J Clin Nurs. (2020) doi: 10.1111/jocn.15566. [Epub ahead of print].
40. Chaudhary NS, Grandner MA, Jackson NJ, Chakravorty S. Caffeine consumption, insomnia, and sleep duration: results from a nationally representative sample. Nutrition. (2016) 32:1193–9. doi: 10.1016/j.nut.2016.04.005
41. The Lancet. COVID-19 and China: lessons and the way forward. Lancet. (2020) 396:213. doi: 10.1016/S0140-6736(20)31637-8
42. National Health Commission of the People's Republic of China. Novel COVID-19-Infected Pneumonia is Subject to the Administration of Statutory Contagious Diseases: National Health Commission of the People's Republic of China. (2020). Available online at: http://www.nhc.gov.cn/jkj/s7915/202001/e4e2d5e6f01147e0a8df3f6701d49f33.shtml (accessed April 25, 2020).
43. Wang H, Wang S, Yu K. COVID-19 infection epidemic: the medical management strategies in heilongjiang province, China. Critical Care. (2020) 24:107. doi: 10.1186/s13054-020-2832-8
Keywords: COVID-19, healthcare workers, insomnia, fatigue, organizational support
Citation: Zou X, Liu S, Li J, Chen W, Ye J, Yang Y, Zhou F and Ling L (2021) Factors Associated With Healthcare Workers' Insomnia Symptoms and Fatigue in the Fight Against COVID-19, and the Role of Organizational Support. Front. Psychiatry 12:652717. doi: 10.3389/fpsyt.2021.652717
Received: 13 January 2021; Accepted: 01 March 2021;
Published: 26 March 2021.
Edited by:
Tina L. Rochelle, City University of Hong Kong, Hong KongReviewed by:
Zezhi Li, Shanghai JiaoTong University, ChinaRuoxi Wang, Huazhong University of Science and Technology, China
Copyright © 2021 Zou, Liu, Li, Chen, Ye, Yang, Zhou and Ling. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Li Ling, lingli@mail.sysu.edu.cn
†These authors have contributed equally to this work
 Xia Zou
Xia Zou Shaokun Liu2†
Shaokun Liu2† Li Ling
Li Ling