- School of Public Health, Wolaita Sodo University, Sodo, Ethiopia
Background: Intestinal Parasitic Infections (IPIs) are among the most prevalent diseases in the world, particularly in developing countries with low socio-economic and poor living conditions. From the estimated one third global population infected by intestinal parasitic infections; the majority lives in tropical and sub-tropical parts of the world. These diseases are highly prevalent in Ethiopia. However, its magnitude in the context of Wolaita Sodo University, where a large number of students reside in a campus is not studied. Therefore, the objective of this study was to assess the prevalence and factors associated with intestinal parasitic infections among food handlers in students' caterings of Wolaita Sodo University, Southern Ethiopia.
Methods: Institutional based cross sectional study was conducted among food handlers working in Wolaita Sodo University students' caterings' from January 10 to February 10, 2016. The study was undertaken among 233 food handlers by using simple random sampling technique. Data were collected using structured and pretested questionnaire; observation of food handlers while working and microbiological laboratory investigations. Bivariate and multivariate analyses were used to assess the association between covariate and the outcome variables. Adjusted Odds Ratio (AOR) with 95% confidence interval (CI) was considered to ascertain the significance of the association.
Results: The mean age of the study participants was 27.2 (±6.4 SD). The overall prevalence of intestinal parasitic infections was 23.6%, with 95% CI of 18.2% to 29.1% of which 12.4% was due to amoeba cyst. Untrimmed fingernail with AOR (95% CI) 2.06 (1.06, 4.00) and regular hand washing habit without soap before food handling with AOR (95% CI) 2.68 (1.25, 5.73) were found to be significantly associated with intestinal parasitic infections.
Conclusions: The prevalence of intestinal parasitic infections was high among Wolaita Sodo University food handlers. Untrimmed fingernail and hand washing habit without soap before food handling were found to increase odds of intestinal parasitic infections. The university may need to consider interventions recommended accordingly.
Background
Intestinal Parasitic Infections (IPIs) are among the most prevalent diseases in the world, particularly in developing countries with low socio-economic and poor living conditions. (1–4). From the estimated one third global population infected by intestinal parasitic infections; the majority lives in tropical and sub-tropical parts of the world (5, 6). These infections are endemic in some countries of Africa, Southeast Asia, South America and Eastern Europe (2, 4, 7).
The epidemiology of intestinal parasitic infections in the world varies from parasites to parasites. Entamoeba histolytica, Ascaris lumbricoides (Roundworm), Ancylostoma duodenale (hookworm), and Trichuris trichiura (Whipworm) are the most common. According to the World Health Organization (WHO) estimates, globally there are 800–1,000 million A. lumbricoides, 700–900 million Hookworm, 500 million T. trichiura, 200 million Giardia intestinalis, and 500 million E. histolytica/dispar cases (8–10). Despite the efforts made to control IPIs, the diseases are continuing to be the leading causes of mortality and morbidity in the world (2, 4, 11, 12).
Ethiopia is one of the countries in Africa with high prevalence of intestinal parasitic infections. Based on the studies conducted in Ethiopia; one third of the population is estimated to be infected with Ascaris lumbricoides, one quarter is infected with Trichuris trichiura and one in eight lives with hookworm (4, 11, 13–17). Thus, Ethiopia has the second highest ascariasis, the third highest hookworm, and the fourth highest trichiuriasis infections in Sub-Saharan Africa (4, 11, 13–17).
The health status and hygienic practices of the food handlers are the major determinants of food contamination in developing countries where there is a poor regulatory system for food hygiene. Because of urbanization and expansion of large institutions; eating and drinking from food caterings are becoming common practices in developing countries like Ethiopia (4–6, 11). Often, food handlers in developing countries, including Ethiopia are employed without proper screening for hygiene related infectious diseases (4, 11, 18). The rapid growth of public universities in Ethiopia in the past two decades, urging to ensure hygienic food handling and preparation practices to safeguard the health of students getting food and drink services in a mass. Meals served in caterings' of higher learning institutions can cause food borne disease outbreaks. A few local studies conducted among food handler's revealed high prevalence of IPIs and unsatisfactory practices of food hygiene measurements (19). However, most studies were old and no similar studies had been conducted in the study area. Therefore, this study aimed at assessing prevalence and factors associated with IPIs among food handlers in the context of Wolaita Sodo University (WSU).
Methods
Study Setting and Period
Institutional based cross sectional study was conducted at WSU, Wolaita Sodo, Southern Ethiopia from January 10 to February 10, 2016. WSU enrolled a total of 11,235 regular students in the 2016 academic year in its two campuses located at Sodo town. The university supplies, food and drink services for its students residing in two campuses located in Wolaita Sodo town. There are 558 food handlers working in the students' caterings, of which 144 were males and 414 were females. WSU has only two campuses (Gandaba and Ottona) only.
Source Population
The source population was all food handlers who were working in the students' Caterings of WSU located in Wolaita Sodo town.
Study Population
The study population was randomly selected food handlers working in the students' caterings of WSU. Food handlers engaged in food preparation, serving and cleaning regardless of their employment status were included in the study. Whereas, those who were on annual leave during the data collection time and those who were taking anti-parasitic drugs in the past two to three weeks prior to the data collection were excluded from the study.
Sample Size and Sampling Technique
The sample size was calculated based on a study in Mekelle university showed that IPIs has been reported in 49.4% of food handlers. Assuming, 95% Confidence Interval (CI), 5% margin of error and 10% non-response rate using single population proportion formula, finite population correction factor for a population <10,000 was used to calculate final sample size (19). Hence, a total of 251 samples were determined. Study participants were selected using simple random sampling technique after entering alphabetic ordered lists of food handlers into Statistical Software for Social Sciences (SPSS) version 20. The samples were distributed between two campuses proportional to their size.
Data Collection Instruments and Procedures
A structured and pretested questionnaire was used to collect data related to socio-demographic, economic, personal and environmental characteristics. Variables such as age, sex, monthly income, personal hygiene, regular medical checkup, waste management and accessibility to safe water supply were included in the questionnaire. The questionnaire was prepared in English and translated into local language. Data were collected by two Environmental Health Officers who speak the local language. Trained staffs collected the data. Training for data collectors and supervisor was given for 3 days. Supervision was made by Environmental Health Officer who has experience of research work and familiar with the study area. Pretest before the actual data collection was carried out on food handlers working at Wolaita Sodo Agricultural Vocation Training College with a size equivalent to 5% of the study subjects.
The stool collection and microscopic investigation were conducted by three Medical laboratory technologists. Triplicate smears from the collected sample of every study subjects were prepared. To ensure consistency of measurements every smear examination was carried out and confirmed by two laboratory technologists. Stool specimens were collected from food handlers with labeled wide-mouthed clean plastic cups using clean wooden applicator stick at WSU Teaching and Referral Hospital Medical Laboratory (20, 21). From each study subjects about 2 gm of stool was collected. The stool samples were processed in WSU Teaching and Referral Hospital Medical Laboratory using WHO standard and calibrated instruments with a direct microscopic technique to detect cysts, trophozoites, eggs, and larva of intestinal parasites (20). Stool examinations were performed using the formol-ether concentration technique. Both the 10× and 40× objectives were used to detect eggs and larvae of helminthes and cysts and trophozoites of protozoan parasites. Iodine solution was used to detect and identify cysts of protozoan parasites (20, 21). The results of the stool examination and observation of the working environment were recorded using checklists.
Data Analysis
Data were checked for completeness and consistency. Coded data were entered using EpiData version 3.1 software and exported to SPSS version 20 for Windows (SPSS, Chicago, IL, USA) for cleaning and analysis. Descriptive summaries were calculated to determine the prevalence of intestinal parasitic infections. Positive result of IPIs coded = 1 and negative results coded = 0 in a logistic regression analysis. Based on the existing evidence, the least contributing factor to the dependent variable was used as reference category. Variables with P-value <0.25 in bivariate analysis were included in the multivariate analysis. Adjusted Odds Ratio (AOR) with 95% CI was considered to ascertain the significance of the association at p-value < 0.05.
Results
Socio-Demographic Characteristics
A total of 233 food handlers were participated with a response rate of 92.8%. Most of the food handlers are female dominant in WSU, hence the male to female ratio of the respondents was 0.25. The mean age of the study participants was 27.2 (±6.4 SD). About 68 (29.2%) participants were educated at the level of college and above. The mean monthly income of respondents was 825 (± 346 SD) Ethiopian Birr (ETB) ranged from 500 to 3,000 ETB (Note: 1USD = 29.00 ETB in May, 2019) (Table 1).
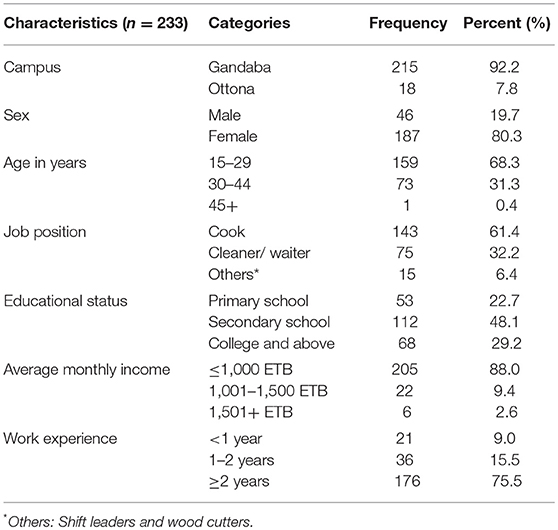
Table 1. Socio-demographic characteristics of the food handlers worked in the students' caterings of WSU, Wolaita Sodo, South Ethiopia from January 10 to February 10, 2016.
Personal Hygiene Practices of Food Handlers
From the total food handlers 113 (48.5%) observed using an outer protective coat or gown during observational assessment of food handlers at work. During observation of finger nail status, 103 (44.2%) food handlers found to have their fingernails untrimmed. About 158 (67.8%) food handlers washed their hands after toilet with soap, while the rest washed only with water. The magnitude of hand washing with soap habit before food handling was 189 (81.1%) (Table 2).
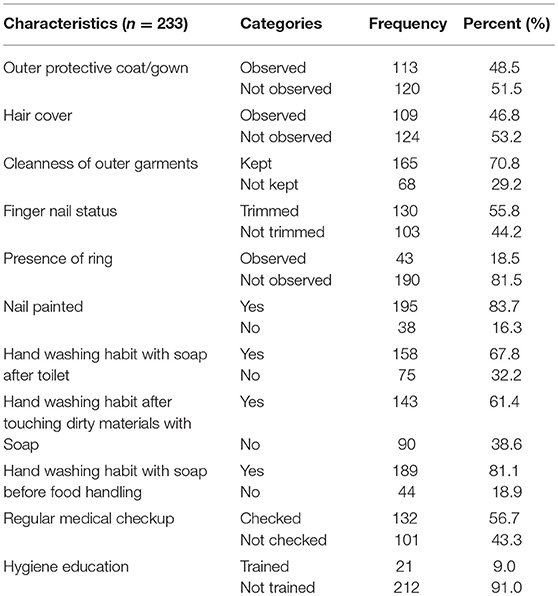
Table 2. Personal hygiene practices of food handlers worked in the students' caterings of WSU, Wolaita Sodo, South Ethiopia from January 10 to February 10, 2016.
Knowledge of Food Handlers
Out of the total participants interviewed for knowledge assessment, 225 (96.6%) knew about person to person transmission of IPIs. On the other hand 232(99.6%) knew washing hands before handling food reduce the transmission of IPIs (Table 3).
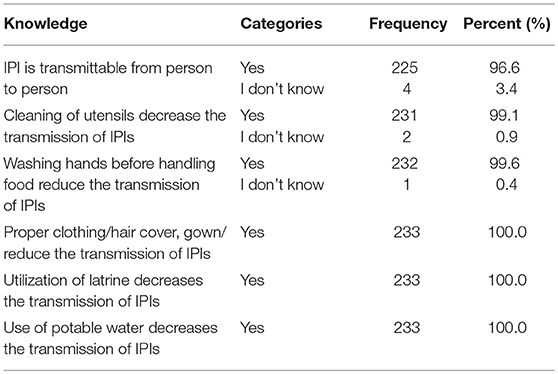
Table 3. Knowledge of food handlers worked in the students' caterings of WSU, Wolaita Sodo, South Ethiopia from January 10 to February 10, 2016.
Prevalence of Intestinal Parasitic Infections
The overall prevalence of IPIs among the food handlers in the students' catering center of WSU was 23.6% (95% CI: 18.2–29.1%). Among all participants, 55(23.6%) were positive for at least one intestinal parasite. Amoeba cyst was the predominant parasite 29(12.4%) followed by Amoeba trophozoites 10 (4.3%) (Table 4).
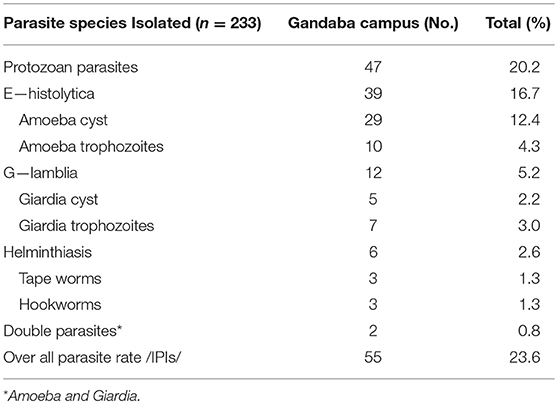
Table 4. Prevalence of IPIs identified from food handlers worked in the students' caterings of WSU, Wolaita Sodo, South Ethiopia from January 10 to February 10, 2016.
Factors Associated With Intestinal Parasitic Infections
Socio-demographic and hygiene related factors such as work experience and finger nail status were entered into binary logistic regression and then variables showing p value < 0.25 were re-entered into multivariate logistic regression to control for confounding. From the binary logistic regression analysis, hand washing habit with soap before food handling with Crude Odds Ratio (COR) (95% CI) of 2.84 (1.41–5.72) was positively associated with intestinal parasitic infections. However, in the binary logistic regression variables such as work experience, finger nail status, educational status, hand washing habit with soap after touching dirty materials, nail painted and cleanness of outer garments were not associated with intestinal parasitic infections (Table 5).
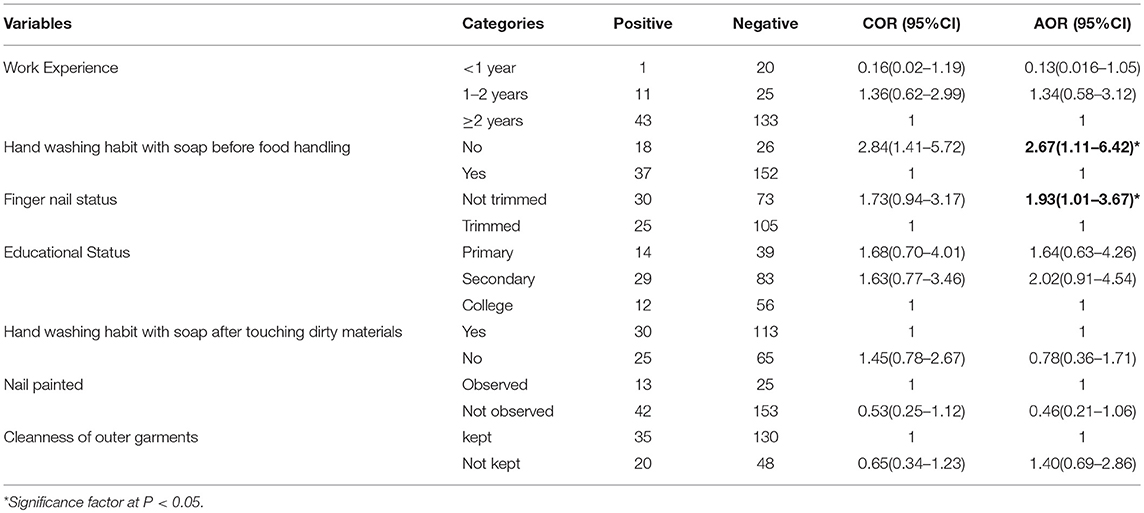
Table 5. Factors associated with IPIs among food handlers worked in students' caterings of WSU, Wolaita Sodo, South Ethiopia from January 10 to February 10, 2016.
On multivariate analysis hand washing habit with soap before food handling and finger nail status showed a significant association with intestinal parasitic infections. There is a 93 % increased odds of developing intestinal parasitic infections among food handlers who had untrimmed finger nail with AOR (95% CI) of 1.93 (1.01, 3.67). Food handlers who had no habit of washing their hands with soap before food handling were 2.67 times more likely to be infected with intestinal parasitic infections than their counterparts with AOR (95% CI) of 2.67 (1.11, 6.42) (Table 5).
Discussion
The spread of intestinal parasitic infections (IPIs) through food handlers is a common and persistent problem worldwide (4, 11, 13–17). Intestinal parasitic infections are among the major health problems in developing countries like Ethiopia (22). The spread of intestinal parasitic infections through food handlers can cause epidemics in the public and students in the university. Therefore, this study was undertaken to assess the prevalence and associated factors of intestinal parasitic infections among food handlers in students' caterings of Wolaita Sodo University. The prevalence of intestinal parasitic infections in this study was found to be 23.6%.
The prevalence of IPIs observed in this study is comparable with the findings from Eldoret Municipality, Kenya (23.7%) (23) and Gonder in Ethiopia (29.1%) (24). However, it is higher than the findings reported from Western Iran (9%) (25), North India (7%), Sari (26), Northern Iran (15.5%) (27). The observed discrepancy might be due to differences in climatic conditions, geographic locations and socio-economic features of the populations. The finding reported in this study is lower than the findings obtained from other studies conducted in Ethiopia; Addis Ababa (45.3%) (20), Hawassa (63%) (28), Mekelle (49.4%) (19), Jimma (58.4%) (22), Yebu (44.1%) (6), Bahir Dar (41.1%) (29), and Arba Minich (36%) (16). The difference might be due to socio-demographic features and geographic locations of the populations.
The rate of double infections was 0.8%. This is relatively similar to the findings from Arba Minich University students' caterings in Southern Ethiopia (0.6%) (16) and Gondar University students' caterings(1.6%) in North-western Ethiopia (24). While it is lower than the finding from Mekelle university students' caterings(5.2%) in Northern Ethiopia (19). Availability and accessibility of medical checkups at Wolaita Sodo University and socio-demographic features might be some of the reasons for the difference.
In this study, the predominant parasitic infection was Amoeba cyst with a prevalence of 12.4%. This is consistent with the finding from Bahir Dar, North-western Ethiopia, 10.2% (29, 30). The prevalence of hookworm was 1.3%, which is in consistent with the findings from Jimma, South-western Ethiopia (2.9%) (31), and Addis Ababa University (2.1%) (20).
Untrimmed fingernail and hand washing habit without soap before food handling were found associated with IPIs. This is similar with the findings from Arbaminch University; where, untrimmed finger nail, hand washing practice after toilet and hand washing before food handling were identified as predictors for IPIs (16). This evidence also supported with the study conducted from Mekele University; where, hand washing habit with soap before food handling and utilization of soap were found determinants for IPIs (19). Both of the study, participants were from university cafeteria food handlers. In either of evidences, untrimmed fingernail can serve as a vehicle for the transmission of intestinal parasitic infections and washing hands with soap before handling food could remove parasites. The study from Addis Ababa University has found no association between untrimmed finger nail and hand washing habit with soap before food handling; and intestinal parasitic infections (20). Examination of food handlers' fingernail contents for ova or parasites is one way of identifying possible contamination of food; however, the current study did not include the assessment of parasite in the fingernail contents. The data of this study are limited to Wolaita Sodo University; therefore, we recommend further study that include other universities in the country. Since the study, design is cross-sectional; it cannot establish temporal relationship between variables; therefore, we recommend intervention study in the same population.
Conclusions
The present study demonstrated a high prevalence of IPIs among food handlers working in Wolaita Sodo University. The study revealed that fingernail determines the prevalence of IPIs, similarly handwashing with soap before food handling was additional determinants of IPI in food handlers. It identified fingernail status and hand washing habit with soap before food handling as determinants of IPIs among food handlers in Wolaita Sodo University. Therefore, enforcement of standard hygienic and sanitary practices by the university was recommended to improve personal hygiene of the food handlers and sanitary facilities of the caterings.
Ethics Statement
The study was conducted after obtaining ethical clearance from WSU College of Health Sciences and Medicine institutional ethical review committee. Letter of cooperation obtained from the university was submitted to the students' caterings administration. Informed oral consent was obtained from the participants of the study. Participants found positive for intestinal parasitic infections were treated at WSU Teaching and Referral Hospital. Information obtained from the study participants was kept confidential. Information's were kept locked in office. Any personal information never pass to the third party.
Author Contributions
WK, WM, and AA designed the study, responsible for supervision, and wrote the manuscript. WM collected data and analysis.
Funding
The research was partially funded by the Wolaita Sodo University.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
The authors hereby sincerely acknowledge Wolaita Sodo University for partially funding this research. We are glad to forward our special thanks to the laboratory department of WSU Teaching and Referral Hospital for their cooperation and provision of necessary materials for this study. Our special thanks go to data collectors and supervisors of this study. We would like to thank food handlers for their participation in this study.
Abbreviations
AOR, Adjusted Odds Ratio; CI, Confidence Interval; COR, Crude Odds Ratio; ETB, Ethiopian Birr; IPIs, Intestinal Parasitic Infections; SPSS, Statistical Package for Social Sciences; WHO, World Health Organization; WSU, Wolaita Sodo University.
References
1. Adamu H, Endeshaw T, Teka T, Kifle A, Petros B. Prevalence of intestinal parasites in paediatric diarrhoeal and non-diarrhoeal patients in Addis Ababa hospitals, with special emphasis on opportunistic parasitic infections and with insight into the demographic and socio-economic factors. Eth J Health Div. (2006) 20:39–47. doi: 10.4314/ejhd.v20i1.10010
2. Carneiro F, Cifuentes E, Tellez-Rojo M. Environmental health indicators and development of preventive actions against Ascaris lumbricoides infections in rural communities, Caparao and Alto Caparao, Minas Gerais, Brazil. Epidemiology. (2000) 11:S63. doi: 10.1097/00001648-200007000-00056
3. Saki J. Prevalence of Intestinal Parasitic Infections among food handlers in Khuzestan, Southwest of Iran: A 10–year retrospective study. Afr J Microbiol Res. (2012) 6:6. doi: 10.5897/AJMR11.1533
5. Chan MS. The global burden of intestinal nematode infections-Fifty years on. Parasitol Today. (1997) 13:438–43. doi: 10.1016/S0169-4758(97)01144-7
6. Tamirat T, Mebrie G. Prevalence and predictors of intestinal parasites among food handlers in Yebu Town, Southwest Ethiopia. PLoS ONE. (2014) 9:0110621. doi: 10.1371/journal.pone.0110621
7. Kendrovski V. Climate change and communicable diseases. A Manual for Health Workers of the former Yugoslav Republic of Macedonia. Denmark: WHO Regional Office for Europe, (2011), p. 41.
8. Abate A, Kibret B, Bekalu E, Abera S, Teklu T, Yalew A, et al. Cross-sectional study on the prevalence of intestinal parasites and associated risk factors in teda health centre, Northwest Ethiopia. ISRN Parasitol. (2013) 2013:757451. doi: 10.5402/2013/757451
9. Prevention and Control of Intestinal Parasitic Infections. WHO Technical Report Series 741, Geneva: WHO, (1987).
10. Pullan RL, Smith JL, Jasrasaria R, Brooker SJ. Global numbers of infection and disease burden of soil transmitted helminth infections in 2010. Parasit Vectors. (2014) 7:37. doi: 10.1186/1756-3305-7-37
11. Deribe K, Meribo K, Gebre T, Hailu A, Ali A, Aseffa A, et al. The burden of neglected tropical diseases in Ethiopia, and opportunities for integrated control and elimination. Parasit Vectors. (2012) 5:240 doi: 10.1186/1756-3305-5-240
12. Duc PP, Nguyen-Viet H, Hattendorf J, Zinsstag J, Cam PD, Odermatt P. Risk factors for Entamoeba histolytica infection in an agricultural community in Hanam province, Vietnam. Parasit Vectors. (2011) 4:102–11. doi: 10.1186/1756-3305-4-102
13. Stephenson LS, Latham MC, Adams EJ, Kinoti SN, Pertet A. Physical fitness, growth and appetite of Kenyan school boys with hookworm, Trichuris trichiura and Ascaris lumbricoides infections are improved four months after a single dose of albendazole. J Nutr. (1993) 123:1036–46. doi: 10.1093/jn/123.4.656
14. de Silva NR, Guyatt HL, Bundy DA. Morbidity and mortality due to ascaris-induced intestinal obstruction. Transac R Soc Trop Med Hygien. (1997) 91:31–6. doi: 10.1016/S0035-9203(97)90384-9
15. Nokes C, Bundy DA. Compliance and absenteeism in school children: implications for helminth control. Transac R Soc Trop Med Hygiene. (1993) 87:148–52. doi: 10.1016/0035-9203(93)90464-2
16. Mama M, Alemu G. Prevalence and factors associated with intestinal parasitic infections among food handlers of Southern Ethiopia: cross sectional study. BMC Public Health. (2016) 16:105. doi: 10.1186/s12889-016-2790-x
17. Hadidjaja P, Bonang E, Suyardi MA, Abidin SAN, Ismid IS, Margono SS. The effect of intervention methods on nutritional status and cognitive function of primary school children infected with Ascaris lumbricoides. Am J Trop Med Hygiene. (1998) 59:791–5. doi: 10.4269/ajtmh.1998.59.791
18. Mudey AB. Health Status and Personal Hygiene among Food Handlers Working at Food Establishment around a Rural Teaching Hospital in Wardha District of Maharashtra, India. Global J Health Sci. (2010) 2:38. doi: 10.5539/gjhs.v2n2p198
19. Nigusse D, Kumie A. Food hygiene practices and prevalence of intestinal parasites among food handlers working in Mekelle university student's cafeteria, Mekelle. Global Adv Res J Soc Sci. (2012) 1:65–71.
20. Aklilu A. Prevalence of Intestinal Parasites, Salmonella and Shigella Among Apparently Health Food Handlers of Addis Ababa University student's Cafeteria. Addis Ababa: BMC Research Notes. (2015).
21. Missaye A. Prevalence of intestinal parasites and associated risk factors among HIV/AIDS patients with pre-ART and on-ART attending dessie hospital ART clinic, Northeast Ethiopia. AIDS Res Ther. (2013) 10:2–8. doi: 10.1186/1742-6405-10-7
22. Assefa T. Assessment of bacterial hand contamination and associated factors among food handlers working in the student cafeterias of jimma university main campus, Jimma, South West Ethiopia. J Community Med Health Educ. (2015) 5:2–7. doi: 10.4172/2161-0711.1000345
23. Biwott GK, Wanjala PM, Ngeiywa MM. Prevalence of gastrointestinal parasitic infections among food handlers in eldoret municipality, Kenya. J Biol Agric Healthcare. (2014) 4:160–8.
24. Andargie G. Prevalence of bacteria and intestinal parasites among food-handlers in gondar town, Northwest Ethiopia. J Health Popul Nutr. (2008) 26:4. doi: 10.3329/jhpn.v26i4.1887
25. Kheirandish F, Ezatpour B. Prevalence of intestinal parasites among food handlers in Western Iran. Rev Inst Med Trop Sao Paulo. (2014) 56:6. doi: 10.1590/S0036-46652014000200004
26. Mehdi S. Prevalence of Intestinal Parasites among Food Handlers of Sari, Northern Iran. Rev Inst Med Trop Sao Paulo. (2015) 57:7. doi: 10.1590/S0036-46652015000200007
27. Khurana S. Intestinal bacterial and parasitic infections among food handlers in a tertiary care hospital of North India. Trop Gastroenterol. (2008) 29:207–9.
28. T/mariam S. Assessment of sanitary and hygeinic status of catering establishment of Awasa Town. Ethiop J Health Dev. (2000) 14:8. doi: 10.4314/ejhd.v14i1.9934
29. Abera B, Biadegelgen F, Bezabih B. Prevalence of Salmonella typhi and intestinal parasites among food handlers in Bahir Dar Town, Northwest Ethiopia. Ethiop J Health Dev. (2010) 24:1–5. doi: 10.4314/ejhd.v24i1.62944
30. Gebre W. Prevalence of intestinal parasites among pregnant women attending antenatal care at gandhi memorial hospital, Addis Ababa, Ethiopia. Harar Bull Health Sci. (2012) 5:74–95.
Keywords: intestinal parasitic infections, food handlers, associated factors, Wolaita Sodo University, Southern Ethiopia
Citation: Kumma WP, Meskele W and Admasie A (2019) Prevalence of Intestinal Parasitic Infections and Associated Factors Among Food Handlers in Wolaita Sodo University Students Caterings, Wolaita Sodo, Southern Ethiopia: A Cross-Sectional Study. Front. Public Health 7:140. doi: 10.3389/fpubh.2019.00140
Received: 03 February 2018; Accepted: 16 May 2019;
Published: 04 June 2019.
Edited by:
Yang Liu, Emory University, United StatesReviewed by:
M. Jahangir Alam, University of Houston, United StatesRosalind Brigham Penney, San Juan Basin Public Health, United States
Copyright © 2019 Kumma, Meskele and Admasie. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Wondimagegn P. Kumma, wondimagegnk@yahoo.com
 Wondimagegn P. Kumma
Wondimagegn P. Kumma Wubshet Meskele
Wubshet Meskele Amha Admasie
Amha Admasie