- 1Department of Infectious Diseases, Vietnam Military Medical University, Hanoi, Vietnam
- 2Division of Military Science, Military Hospital 103, Hanoi, Vietnam
- 3International Center for Health Information Technology, Taipei Medical University, Taipei, Taiwan
- 4Department of Healthcare Information and Management, Ming Chuan University, Taoyuan City, Taiwan
- 5Faculty of Public Health, Hai Phong University of Medicine and Pharmacy, Hai Phong, Vietnam
- 6President Office, Hai Phong University of Medicine and Pharmacy, Hai Phong, Vietnam
- 7Director Office, Thai Nguyen National Hospital, Thai Nguyen City, Vietnam
- 8President Office, Thai Nguyen University of Medicine and Pharmacy, Thai Nguyen City, Vietnam
- 9International Master/Ph.D. Program in Medicine, Taipei Medical University, Taipei, Taiwan
- 10Department of Anesthesiology, Thu Duc District Hospital, Ho Chi Minh City, Vietnam
- 11Director Office, Thu Duc District Health Center, Ho Chi Minh City, Vietnam
- 12Health Management Training Institute, Hue University of Medicine and Pharmacy, Hue, Vietnam
- 13Department of Health Economics, Corvinus University of Budapest, Budapest, Hungary
- 14Director Office, Military Hospital 103, Hanoi, Vietnam
- 15Department of Pulmonary and Cardiovascular Diseases, Hai Phong University of Medicine and Pharmacy Hospital, Hai Phong, Vietnam
- 16Director Office, Hai Phong University of Medicine and Pharmacy Hospital, Hai Phong, Vietnam
- 17Director Office, Hospital District 2, Ho Chi Minh City, Vietnam
- 18Nursing Office, Tan Phu District Hospital, Ho Chi Minh City, Vietnam
- 19Department of Internal Medicine, Thai Nguyen University of Medicine and Pharmacy, Thai Nguyen City, Vietnam
- 20Department of Health Education, Faculty of Social Sciences, Behavior and Health Education, Hanoi University of Public Health, Hanoi, Vietnam
- 21Graduate Institute of Data Science, Taipei Medical University, Taipei, Taiwan
- 22School of Nutrition and Health Sciences, Taipei Medical University, Taipei, Taiwan
Purpose: We examined factors associated with health literacy among elders with and without suspected COVID-19 symptoms (S-COVID-19-S).
Methods: A cross-sectional study was conducted at outpatient departments of nine hospitals and health centers 14 February−2 March 2020. Self-administered questionnaires were used to assess patient characteristics, health literacy, clinical information, health-related behaviors, and depression. A sample of 928 participants aged 60–85 years were analyzed.
Results: The proportion of people with S-COVID-19-S and depression were 48.3 and 13.4%, respectively. The determinants of health literacy in groups with and without S-COVID-19-S were age, gender, education, ability to pay for medication, and social status. In people with S-COVID-19-S, one-score increment of health literacy was associated with 8% higher healthy eating likelihood (odds ratio, OR, 1.08; 95% confidence interval, 95%CI, 1.04, 1.13; p < 0.001), 4% higher physical activity likelihood (OR, 1.04; 95%CI, 1.01, 1.08, p = 0.023), and 9% lower depression likelihood (OR, 0.90; 95%CI, 0.87, 0.94; p < 0.001). These associations were not found in people without S-COVID-19-S.
Conclusions: The older people with higher health literacy were less likely to have depression and had healthier behaviors in the group with S-COVD-19-S. Potential health literacy interventions are suggested to promote healthy behaviors and improve mental health outcomes to lessen the pandemic's damage in this age group.
Introduction
The COVID-19 pandemic has upended public health systems around the globe (1, 2), and spurring millions of health, research and administrative professionals to seek ways to mitigate transmission and mortality (3, 4). Older people are at high risk of more severe health conditions from COVID-19 disease (5, 6). By the time the virus killed 350,000 people, the over-60 death rate was estimated at 75%. The pandemic also has caused panic and mental illness, especially for the elderly (7, 8). Quarantine and lockdown contain infection but they negatively impact mental health (9–11). Different approaches are needed to mitigate the pandemic's psychological effects (12, 13).
Health literacy (HL) is known as a crucial means to appraise health-related information for preventing non-communicable and infectious diseases. It helps people achieve better quality care and improves disease management, lifestyle, and health outcomes (14, 15). Health literacy is considered a crucial element in public health strategies to protect people from disease (16, 17). This has never been more important than during the COVID-19 epidemic (18, 19). Vietnam has a high risk of coronavirus infection, having a long border with China, and Vietnamese people have lower health literacy scores when ranked among other Asian countries (20). Finding factors associated with health literacy can assist in planning interventions to reduce health inequalities during the epidemic.
This study explores determinants of health literacy and its associations with health-related behaviors and depression among older people with and without suspected COVID-19 symptoms (S-COVID-19-S).
Materials and Methods
Study Design
We conducted a cross-sectional study on outpatient department (OPD) visitors 14 February−2 March 2020. The study was reviewed and approved by the nine participating hospitals and health centers as well as the Institutional Ethical Review Committee of Hanoi School of Public Health in Vietnam (IRB No. 029/2020/YTCC-HD3).
Study Participants and Settings
Patients recruited in the study were ages 60–85 years, able to communicate in Vietnamese, and visited an OPD during the study period. Participants were excluded if they were in any emergency condition or if they were diagnosed with psychotic disorders, dementia or blindness. The process of recruiting participants is detailed in a previous study (15).
We included 928 patients aged 60–85 years in the analysis, including 152 from Thai Nguyen National Hospital in Thai Nguyen Province, 56 from Military Hospital 103 in Hanoi; 162 from Hai Phong University of Medicine, and Pharmacy Hospital, 281 from Kien Thuy District Health Center, in Hai Phong city; 141 from Trieu Phong District Health Center in Quang Tri province; 40 from Thu Duc Hospital, 27 from Tan Phu District Hospital, 23 from Hospital District 2, and 46 from Thu Duc District Health Center, in Ho Chi Minh city.
Data Collection Procedure
The interviewers (e.g., nurses, staff, and medical students) at each hospital or health center had received 4 h of training for the data collection; the sessions were led by two senior researchers with a detailed protocol. Technical guidance for prevention and control of COVID-19 disease was also provided during the training, including mask use, hand washing and physical distancing (4).
Interviewers invited OPD visitors to participate in the survey after signing consent form. The interviews were conducted at the OPDs using printed questionnaires that took about 20 min to complete. Personal information (e.g., name, identification) was anonymized before the analysis.
Measurements
Demographic Characteristics and Clinical Indicators
Socio-demographic indicators assessed included age (date of birth), gender (female, male), marital status (never, ever married), education (illiterate or elementary school, junior high school, high school, college/university, or above), occupation (employed, business owner, others), social status (low, middle, or high level), and ability to pay for medication (very difficult to very easy).
Participants visiting the OPD were asked why they sought healthcare services, and were screened for suspected COVID-19 symptoms (S-COVID-19-S). Patients were classified in the S-COVID-19-S group if they carried any of the common symptoms (e.g., fever, cough, dyspnea, fatigue, myalgia, anorexia, or sore throat) or uncommon symptoms (e.g., confusion, headache, rhinorrhea, hemoptysis, chest pain, conjunctivitis, bronchial breath sounds, diarrhea, cyanosis, and nausea/vomiting) (21). In addition, height (cm), weight (kg), body mass index (BMI, kg/m2), and comorbid conditions (Charlson comorbidity index diseases) were assessed.
Health-Related Behaviors
Health-related behaviors included current smoking status (no vs. yes), drinking status (no vs. yes), and eating behaviors during the COVID-19 outbreak (unchanged or less healthy, or healthier). The seven-item International Physical Activity Questionnaire short version (IPAQ-SF) asked patients' activities (vigorous, moderate, walking, and sitting) over the past 7 days before the OPD visiting date (22, 23). The overall physical activity score as MET-min/week was calculated for each subject and used in the analysis (24).
Health Literacy
We used a short-form questionnaire (HLS-SF12) to measure health literacy (15, 25, 26). People were asked about the perceived difficulty of 12 items on a 4-point Likert scale (1 = very difficult to 4 = very easy). We calculated the general health literacy (HL) index score using the formula (1):
where the HL index is ranged from 0 to 50; M is the mean of 12 items of HLS-SF12. The higher HL index indicates a greater HL level (25, 27).
Depression
We assessed depression using patient health questionnaire with 9 items (PHQ-9) that had been validated and used in Vietnam (28–30). Patients rated each item using the 4-point Likert scale from 0 = not at all to 3 = almost every day for the past 14 days. The depression scores range from 0 to 27, with those scoring ≥10 classified as having depression (31).
Statistical Analysis
The distributions of studied variables were explored using descriptive analysis. The Student's t-test and Chi-square tests were used appropriately for continuous and categorical variables. The determinants of health literacy were examined using simple and multiple linear regression analysis. Next, the simple and multiple binary logistic regression analyses were used to examine the associations of health literacy (as a predictor/independent variable) with binary outcome variables such as BMI (normal weight vs. overweight/obese), smoking status (non-smoking vs. smoking), drinking (non-drinking vs. drinking), eating behavior (eat less healthily or unchanged vs. eating healthier diet), depression (not depressed vs. depressed). The simple and multiple multinomial logistic regression analyses were used to examine the association between health literacy and physical activity (tertile-1 vs. tertile-2, tertile-3). Variables showing significant associations with outcome variables in simple regression models were selected for multiple regression models. In order to avoid multicollinearity, the Spearman's correlation coefficient test was used to check associations between independent variables. If independent variables correlated with one another at rho ≥ 0.3, one representative independent variable was selected to the multiple regression model. The significance level was set at a p-value < 0.05. Data were analyzed using SPSS for windows, version 20.0 (IBM Corp, Armonk, NY, USA).
Results
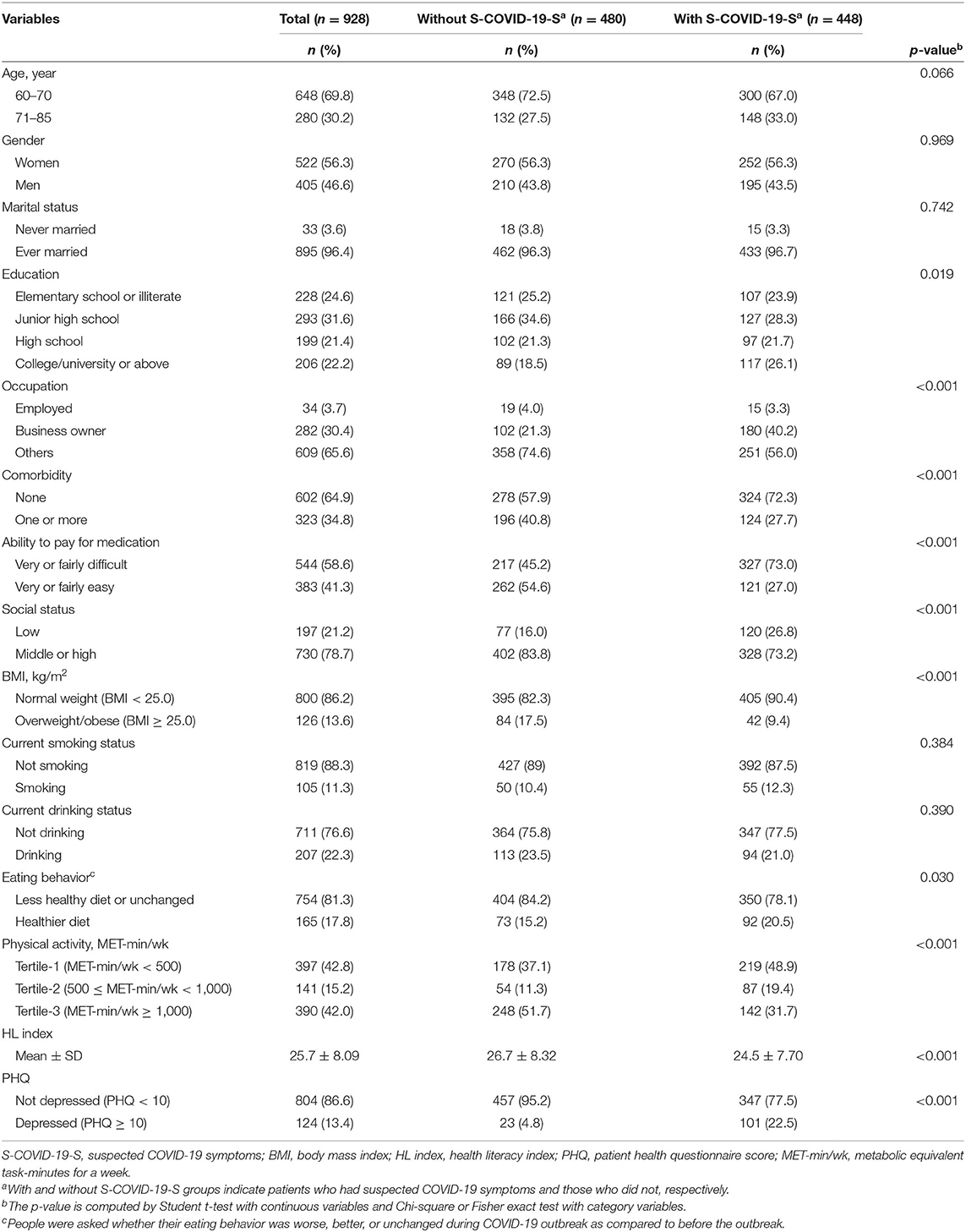
Demographic Characteristics of Participants
Out of sample, percentages of older people with S-COVID-19-S, and depression were 48.3% (448/928), and 13.4% (124/928), respectively. The mean age and health literacy scores were 68.2 ± 6.51, and 25.7 ± 8.09, respectively. The proportion of people with S-COVID-19-S varied with different categories of educational attainment, occupation, comorbidity, ability to pay for medication, social status, BMI, drinking, physical activity, and depression. People with S-COVID-19-S also had lower HL score than those without (Table 1).
Determinants of Health Literacy
Table 2 illustrates the determinants of health literacy for both groups with and without S-COVID-19-S. We checked correlations among the independent variables and found education and social status moderately correlated for people without S-COVID-19-S (rho = 0.36; Supplementary Table 1). Social status was selected into the multiple linear regression model. There was no moderate or high correlation among confounders for people with S-COVID-19-S (Supplementary Table 2). Therefore, all independent variables in the simple regression model were retained in the multiple linear regression model. The results of multiple linear regression analysis show that in comparison to the 60–70 years group, people 71–85 had lower health literacy (regression coefficient, B, −4.36; 95% confidence interval, 95% CI, −5.95, −2.77; p = 0.001, for participants with S-COVID-19-S; and B, −3.74; 95% CI, −5.05, −2.43; p < 0.001, for those without S-COVID-19-S). Men had higher health literacy scores than women (B, 1.77; 95% CI, 0.42, 3.13; p = 0.01 for the S-COVID-19-S group; and B, 1.94; 95% CI, 0.42, 3.46; p = 0.013, for the without S-COVID-19-S group). People with higher educational attainment had higher health literacy scores (B, 3.28 ~ 4.59, p < 0.001, for the group with S-COVID-19-S). People with a better ability to pay for medication had higher health literacy scores than their counterparts (B, 5.69; 95% CI, 4.33, 7.06; p < 0.001, for the group with S-COVID-19-S; and B, 1.53; 95% CI, 0.16, 2.90; p = 0.028). Finally, people with higher social status had higher health literacy scores (B, 3.33, 95%CI, 1.327, 5.33, p = 0.001, for the group without S-COVID-19-S; and B, 1.65 (0.22, 3.08), p = 0.024, for the group with S-COVID-19-S; Table 2).
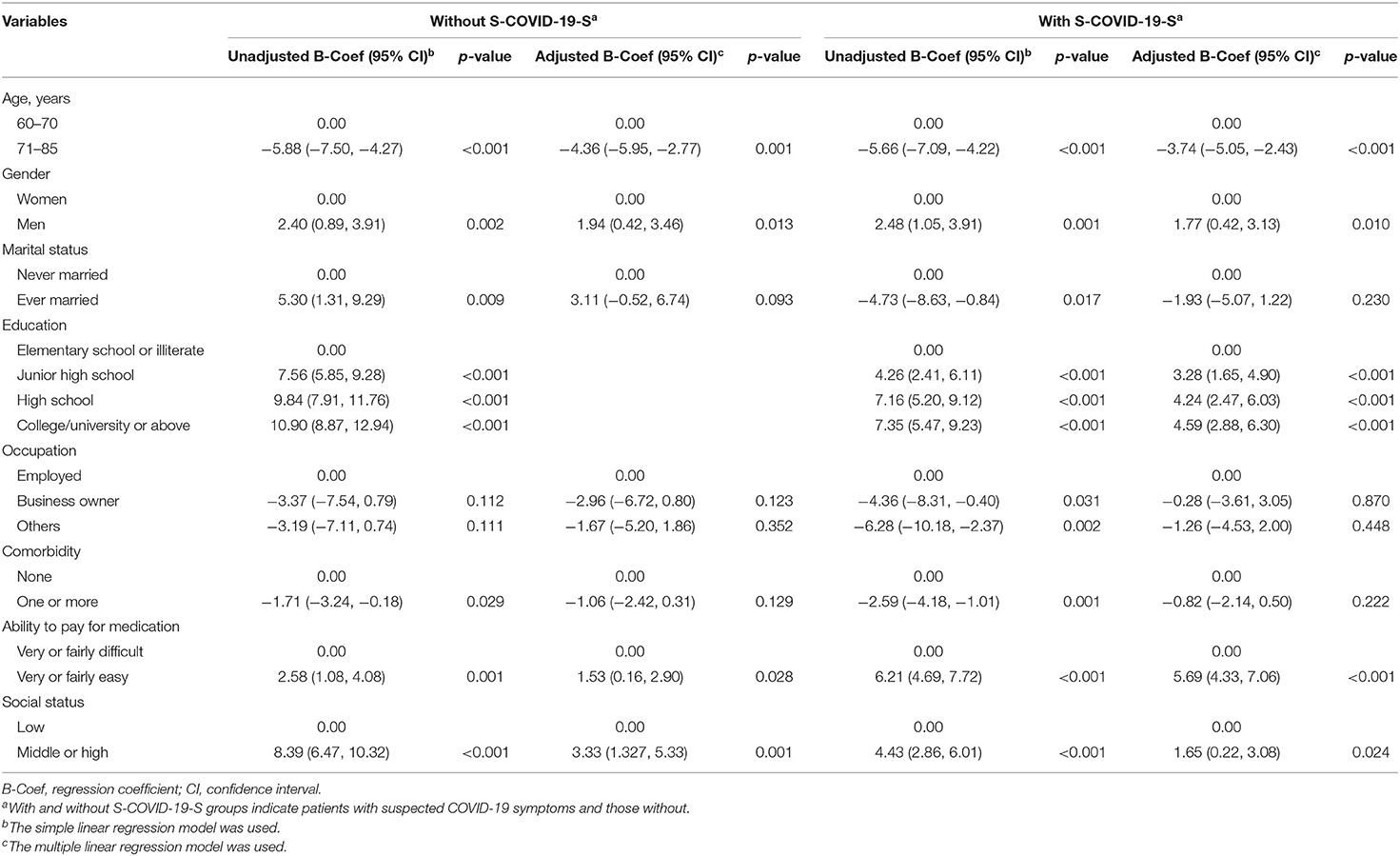
Table 2. Factors associated with health literacy among participants with and without suspected COVID-19 symptoms.
Health Literacy and Its Consequences
Table 3 presents associations of health literacy (HL) and related outcomes (e.g., BMI, smoking status, drinking status, eating behavior, physical activity, and depression). To adjust for potential confounders of the association between HL and consequences, we conducted the analyses to explore the potential determinants of each outcome. The results are shown in Supplementary Tables 3–8. The results of multiple logistic regression analysis show that people with higher health literacy scores ate healthier diets in the group with S-COVID-19-S (odds ratio, OR, 1.08; 95% confidence interval, 95% CI, 1.04, 1.13; p < 0.001). Similar results were found with those who reported more physical activity in the S-COVID-19-S group (OR, 1.04; 95% CI, 1.01, 1.08; p = 0.023 for tertile-3). People with higher HL scores had a lower likelihood of depression (OR, 0.91; 95% CI, 0.87, 0.94; p < 0.001; Table 3).
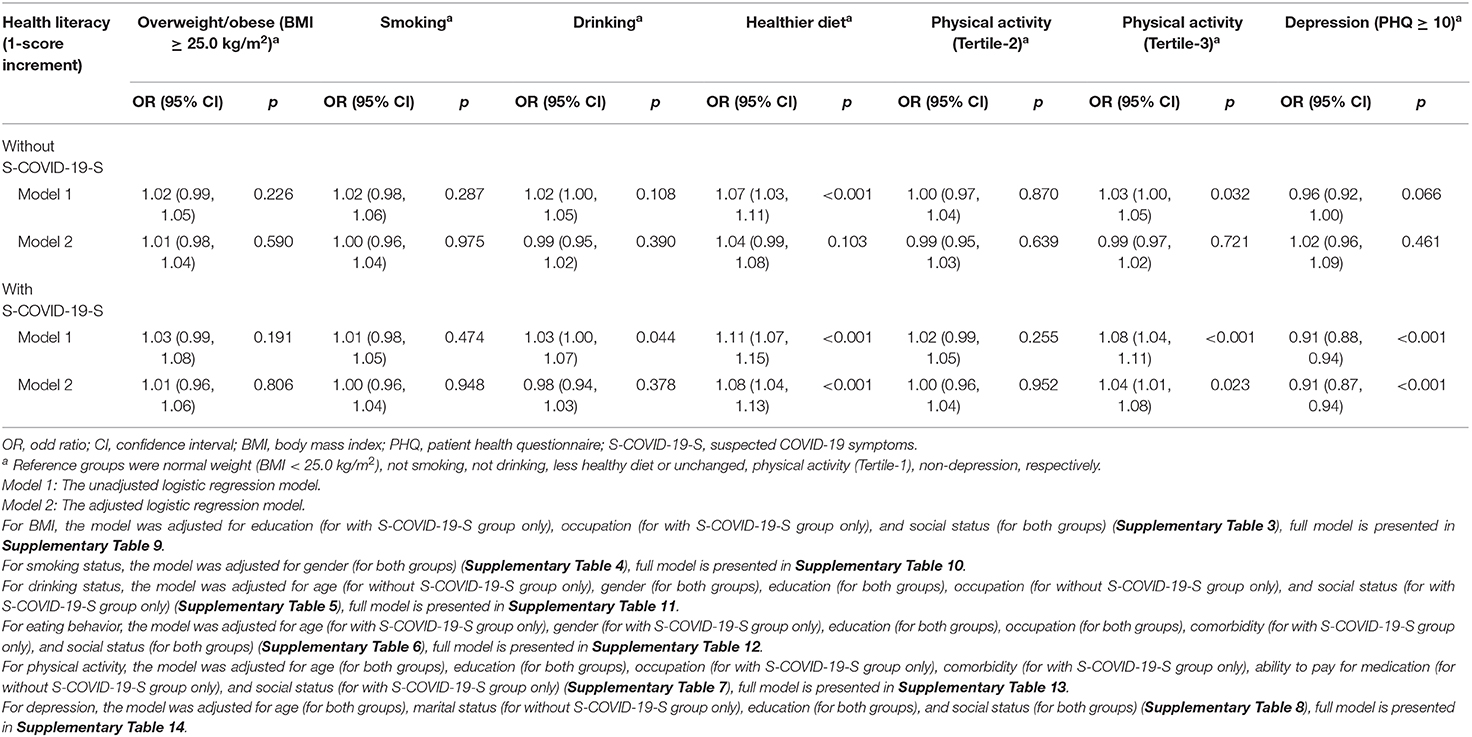
Table 3. Health literacy as a predictor associates with body mass index, health-related behaviors, and depression among participants with and without suspected COVID-19 symptoms.
Discussion
Our study shows men had higher health literacy scores compared to women for both with and without S-COVID-19-S groups. Previous studies showed men facing higher risks of worse health outcomes and death from COVID-19 disease, especially among older adults (32–35). Similarly, older people (ages 71–85 years) had lower health literacy compared to the younger group (ages 60–70 years) in both with and without S-COVID-19-S groups. The findings were consistent with other studies finding health literacy levels lower among elders in various nations and periods (36, 37). Likewise, higher levels of education and social status were associated with higher health literacy scores in older people, which is in line with previous studies (38, 39). Therefore, improving health literacy might be a strategic approach to prevent COVID-19 and minimize its consequences, especially in men and the older people. In addition, active engagement of the elderly is encouraged to contain the pandemic (40, 41). Governments must provide detailed, timely and accurate information regarding the epidemic, particularly about prevention efforts and self-protective behaviors that minimize new infections (42–44). Vietnam's Ministry of Health has led all health institutions and related sectors to collaborate with the public against the COVID-19 epidemic (45). The government has encouraged people to enhance behaviors such as washing hands, wearing masks, and following updated health-related information to prevent the disease and improve health literacy (46).
The COVID-19 pandemic has devastated economies and labor markets, especially reducing jobs and workers' earnings (47). Vietnam's GDP is $2,740, lower than many industrializing nations, so its people particularly fear the pandemics' impacts on household income, such as not able to cover daily living costs or health care expenses (48). Our study shows elders with better ability to pay medication had higher health literacy scores in both with and without S-COVID-19-S groups. This evidence calls for a quick response from governments in terms of stimulus packages to cover food, water, essential goods, basic health services, and medical costs during the crisis (46).
In the current study, we found health literacy significantly associated with healthier diet and physical activity only in older people with S-COVID-19-S. This can be explained by those participants facing higher projected risks of coronavirus infection and severe outcomes. They arguably have the most to gain from practicing healthy lifestyles (e.g., healthy dietary intake and more physical activity) to protect and improve their health-related quality of life (46, 49).
One important finding was that higher health literacy scores were associated with lower likelihood of depression in older people with S-COVID-19-S. This finding is similar to previous studies (50, 51). In our previous study, higher health literacy scores also were associated with lower fear of COVID-19 and lower likelihood of depression (15). We observed that nearly 13% of elders had depressive symptoms with 22.5 and 4.8% of participants with and without S-COVID-19-S, respectively. This might indicate that the uncertain progression of the COVID-19 epidemic affects mental health possibly leading to hypochondriasis, worry about being infected, and fear of the uncontrollable epidemic's consequences (52).
The study has several limitations. First, causality cannot be generated on the basis of a cross-sectional design. The findings could be considered for further studies regarding the pandemic, especially in elderly participants. Second, the study was conducted during the sensitive time period of the global COVID-19 pandemic, when all participants and interviewers might have been at risk of infection. Researchers and leaders of hospitals and health centers made great efforts to protect the safety of study participants, and fortunately there were no new cases during the data collection period. In addition, have selected 9 hospitals and health centers in three parts of Vietnam, yet the sample may not fully-represent the general Vietnamese population. Finally, while we cannot follow-up with the participants to assess long-term associations, future longitudinal studies with larger samples are suggested to confirm these findings.
Conclusions
In groups with and without S-COVID-19-S, the factors of age, gender, education, ability to pay for medication, and social status were significantly associated with health literacy. Elders with higher health literacy had greater likelihood of healthier behavior (e.g., healthy eating, physical exercise) and lower likelihood of depression, especially in the S-COVID-19-S group. Because improved health literacy protects elders, our findings should be helpful for policy-makers worldwide.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available on reasonable request to the corresponding author.
Ethics Statement
The study was reviewed and approved the Institutional Ethical Review Committee of Hanoi University of Public Health, Vietnam (IRB No. 029/2020/YTCC-HD3).
Author Contributions
BD, P-AN, and TD analyzed the data and drafted the manuscript. BD, P-AN, KP, HN, MN, CT, TN, TT, LP, KT, TTD, THD, KN, TP, M-HH, and TD contributed to conceptualization, investigation, methodology, validation, and writing review and editing. BD, P-AN, KP, HN, MN, CT, TN, TT, LP, KT, TTD, THD, KN, TP, and TD conducted data curation.
Funding
This research was funded by Military Hospital 103, and Taipei Medical University (108-6202-008-112; 108-3805-022-400).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
The authors would like to thank the doctors, nurses, and medical students who helped with data collection.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2020.581746/full#supplementary-material
References
1. Koh J, Shah SU, Chua PEY, Gui H, Pang J. Epidemiological and clinical characteristics of cases during the early phase of covid-19 pandemic: a systematic review and meta-analysis. Front Med. (2020) 7:295. doi: 10.3389/fmed.2020.00295
2. Keni R, Alexander A, Nayak PG, Mudgal J, Nandakumar K. COVID-19: emergence, spread, possible treatments, and global burden. Front Public Health. (2020) 8:216. doi: 10.3389/fpubh.2020.00216
3. World Health Organization. COVID-19 Strategy Update. (2020). Available online at: https://www.who.int/docs/default-source/coronaviruse/covid-strategy-update-14april2020.pdf?sfvrsn=29da3ba0_19 (accessed May 28, 2020).
4. World Health Organization. Coronavirus Disease (COVID-19) Technical Guidance: Infection Prevention and Control/Wash. (2020). Available online at: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technical-guidance/infection-prevention-and-control (accessed May 20, 2020).
5. Alhazzani W, Møller MH, Arabi YM, Loeb M, Gong MN, Fan E, et al. Surviving sepsis campaign: guidelines on the management of critically ill adults with Coronavirus disease 2019 (COVID-19). Intensive Care Med. (2020) 46:854–87. doi: 10.1097/CCM.0000000000004363
6. CDC COVID-19 Response Team. Severe outcomes among patients with Coronavirus disease 2019 (COVID-19) - United States, February 12-March 16, 2020. MMWR Morb Mortal Wkly Rep. (2020) 69:343–6. doi: 10.15585/mmwr.mm6912e2
7. Armitage R, Nellums LB. COVID-19 and the consequences of isolating the elderly. Lancet Public Health. (2020) 5:e256. doi: 10.1016/S2468-2667(20)30061-X
8. CDC COVID-19 Response Team. Preliminary estimates of the prevalence of selected underlying health conditions among patients with Coronavirus disease 2019 - United States, February 12-March 28, 2020. MMWR Morb Mortal Wkly Rep. (2020) 69:382–6. doi: 10.15585/mmwr.mm6913e2
9. Hiremath P, Suhas Kowshik CS, Manjunath M, Shettar M. COVID 19: impact of lock-down on mental health and tips to overcome. Asian J Psychiatr. (2020) 51:102088. doi: 10.1016/j.ajp.2020.102088
10. Gunawan J, Juthamanee S, Aungsuroch Y. Current mental health issues in the era of Covid-19. Asian J Psychiatr. (2020) 51:102103. doi: 10.1016/j.ajp.2020.102103
11. Rajkumar RP. COVID-19 and mental health: a review of the existing literature. Asian J Psychiatr. (2020) 52:102066. doi: 10.1016/j.ajp.2020.102066
12. Roy D, Tripathy S, Kar SK, Sharma N, Verma SK, Kaushal V. Study of knowledge, attitude, anxiety & perceived mental healthcare need in Indian population during COVID-19 pandemic. Asian J Psychiatr. (2020) 51:102083. doi: 10.1016/j.ajp.2020.102083
13. Yao H, Chen JH, Xu YF. Rethinking online mental health services in China during the COVID-19 epidemic. Asian J Psychiatr. (2020) 50:102015. doi: 10.1016/j.ajp.2020.102015
14. Castro-Sánchez E, Chang PWS, Vila-Candel R, Escobedo AA, Holmes AH. Health literacy and Infectious Diseases: why does it matter? Int J Infect Dis. (2016) 43:103–10. doi: 10.1016/j.ijid.2015.12.019
15. Nguyen HC, Nguyen MH, Do BN, Tran CQ, Nguyen TTP, Pham KM, et al. People with suspected COVID-19 symptoms were more likely depressed and had lower health-related quality of life: the potential benefit of health literacy. J Clin Med. (2020) 9:965. doi: 10.3390/jcm9040965
16. Berkman ND, Sheridan SL, Donahue KE, Halpern DJ, Crotty K. Low health literacy and health outcomes: an updated systematic review. Ann Intern Med. (2011) 155:97–107. doi: 10.7326/0003-4819-155-2-201107190-00005
17. Sørensen K, Van den Broucke S, Fullam J, Doyle G, Pelikan J, Slonska Z, et al. Health literacy and public health: a systematic review and integration of definitions and models. BMC Public Health. (2012) 12:80. doi: 10.1186/1471-2458-12-80
18. Sentell T, Vamos S, Okan O. Interdisciplinary perspectives on health literacy research around the world: more important than ever in a time of COVID-19. Int J Environ Res Public Health. (2020) 17:3010. doi: 10.3390/ijerph17093010
19. Paakkari L, Okan O. COVID-19: health literacy is an underestimated problem. Lancet Public Health. (2020) 5:e249–50. doi: 10.1016/S2468-2667(20)30086-4
20. Carmona RH. Health literacy: a national priority. J Gen Intern Med. (2006) 21:803. doi: 10.1111/j.1525-1497.2006.00569.x
21. BMJ Best Practice. Coronavirus Disease 2019 (COVID-19), History and Exam. (2020). Available online at: https://bestpractice.bmj.com/topics/en-gb/3000168/history-exam (accessed May 15, 2020).
22. Craig CL, Marshall AL, Sjöström M, Bauman AE, Booth ML, Ainsworth BE, et al. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc. (2003) 35:1381–95. doi: 10.1249/01.MSS.0000078924.61453.FB
23. Lachat CK, Verstraeten R, Hagströmer M, Khan NC, Van NDA, Dung NQ, et al. Validity of two physical activity questionnaires (IPAQ and PAQA) for Vietnamese adolescents in rural and urban areas. Int J Behav Nutr Phys Act. (2008) 5:37. doi: 10.1186/1479-5868-5-37
24. Lee PH, Macfarlane DJ, Lam TH, Stewart SM. Validity of the international physical activity questionnaire short form (IPAQ-SF): a systematic review. Int J Behav Nutr Phys Act. (2011) 8:115. doi: 10.1186/1479-5868-8-115
25. Duong TV, Aringazina A, Kayupova G, Pham TV, Pham KM, Truong TQ, et al. Development and validation of a new short-form health literacy instrument (HLS-SF12) for the general public in six Asian countries. Health Lit Res Pract. (2019) 3:e91–102. doi: 10.3928/24748307-20190225-01
26. Duong TV, Nguyen TTP, Pham KM, Nguyen KT, Giap MH, Tran TDX, et al. Validation of the short-form health literacy questionnaire (HLS-SF12) and its determinants among people living in rural areas in Vietnam. Int J Environ Res Public Health. (2019) 16:3346. doi: 10.3390/ijerph16183346
27. Sørensen K, Van den Broucke S, Pelikan JM, Fullam J, Doyle G, Slonska Z, et al. Measuring health literacy in populations: illuminating the design and development process of the European Health Literacy Survey Questionnaire (HLS-EU-Q). BMC Public Health. (2013) 13:948. doi: 10.1186/1471-2458-13-948
28. Löwe B, Kroenke K, Herzog W, Gräfe K. Measuring depression outcome with a brief self-report instrument: sensitivity to change of the Patient Health Questionnaire (PHQ-9). J Affect Disord. (2004) 81:61–6. doi: 10.1016/S0165-0327(03)00198-8
29. Pham T, Bui L, Nguyen A, Nguyen B, Tran P, Vu P, et al. The prevalence of depression and associated risk factors among medical students: an untold story in Vietnam. PLoS ONE. (2019) 14:e0221432. doi: 10.1371/journal.pone.0221432
30. Nguyen TQ, Bandeen-Roche K, Bass JK, German D, Nguyen NTT, Knowlton AR. A tool for sexual minority mental health research: the Patient Health Questionnaire (PHQ-9) as a depressive symptom severity measure for sexual minority women in Viet Nam. J Gay Lesbian Ment Health. (2016) 20:173–91. doi: 10.1080/19359705.2015.1080204
31. Kocalevent R-D, Hinz A, Brähler E. Standardization of the depression screener patient health questionnaire (PHQ-9) in the general population. Gen Hosp Psychiatry. (2013) 35:551–5. doi: 10.1016/j.genhosppsych.2013.04.006
32. Tang N, Bai H, Chen X, Gong J, Li D, Sun Z. Anticoagulant treatment is associated with decreased mortality in severe coronavirus disease 2019 patients with coagulopathy. J Thromb Haemost. (2020) 18:1094–9. doi: 10.1111/jth.14817
33. Shi S, Qin M, Shen B, Cai Y, Liu T, Yang F, et al. Association of cardiac injury with mortality in hospitalized patients with COVID-19 in Wuhan, China. JAMA Cardiol. (2020) 5:802–10. doi: 10.1001/jamacardio.2020.0950
34. Baud D, Qi X, Nielsen-Saines K, Musso D, Pomar L, Favre G. Real estimates of mortality following COVID-19 infection. Lancet Infect Dis. (2020) 20:773. doi: 10.1016/S1473-3099(20)30195-X
35. Jin JM, Bai P, He W, Wu F, Liu XF, Han DM, et al. Gender differences in patients With COVID-19: focus on severity and mortality. Front Public Health. (2020) 8:152. doi: 10.3389/fpubh.2020.00152
36. Baker DW, Wolf MS, Feinglass J, Thompson JA, Gazmararian JA, Huang J. Health literacy and mortality among elderly persons. Arch Intern Med. (2007) 167:1503–9. doi: 10.1001/archinte.167.14.1503
37. Van Hoa H, Giang HT, Vu PT, Van Tuyen D, Khue PM. Factors associated with health literacy among the elderly people in Vietnam. Biomed Res Int. (2020) 2020:3490635. doi: 10.1155/2020/3490635
38. Wolf MS, Gazmararian JA, Baker DW. Health literacy and functional health status among older adults. Arch Intern Med. (2005) 165:1946–52. doi: 10.1001/archinte.165.17.1946
39. Bains SS, Egede LE. Associations between health literacy, diabetes knowledge, self-care behaviors, and glycemic control in a low income population with type 2 diabetes. Diabetes Technol Ther. (2011) 13:335–41. doi: 10.1089/dia.2010.0160
40. Kayupova G, Turdaliyeva B, Tulerayev K, Duong TV, Chang PW, Zagulova D. Health literacy among visitors of district polyclinics in Almaty, Kazakhstan. Iran J Public Health. (2017) 46:1062–70.
41. Pham VT, Chen Y-M, Duong TV, Nguyen TPT, Chie WC. Adaptation and validation of active aging index among older Vietnamese adults. J Aging Health. (2019). doi: 10.1177/0898264319841524. [Epub ahead of print].
42. del Rio C, Malani PN. 2019 novel Coronavirus—important information for clinicians. JAMA. (2020) 323:1039–40. doi: 10.1001/jama.2020.1490
43. Gostin LO, Hodge JG. US emergency legal responses to novel Coronavirus: balancing public health and civil liberties. JAMA. (2020) 323:1131–2. doi: 10.1001/jama.2020.2025
44. Wang CJ, Ng CY, Brook RH. Response to COVID-19 in Taiwan: big data analytics, new technology, and proactive testing. JAMA. (2020) 323:1341–2. doi: 10.1001/jama.2020.3151
45. The Government of the Socialist Republic of Vietnam. Government in Action. (2020). Available online at: http://news.chinhphu.vn/Home/Government-in-action.vgp (accessed March 15, 2020).
46. Smith N, Fraser M. Straining the system: novel coronavirus (COVID-19) and preparedness for concomitant disasters. Am J Public Health. (2020) 110:648–9. doi: 10.2105/AJPH.2020.305618
47. McKee M, Stuckler D. If the world fails to protect the economy, COVID-19 will damage health not just now but also in the future. Nat Med. (2020) 26:640–2. doi: 10.1038/s41591-020-0863-y
48. Hai HT, Quang ND, Thang NT, Nam NH. Circular economy in Vietnam. In: Ghosh S, editor. Circular Economy: Global Perspective. Singapore: Springer (2020). p. 423–52. doi: 10.1007/978-981-15-1052-6_22
49. Opie RS, Itsiopoulos C, Parletta N, Sanchez-Villegas A, Akbaraly TN, Ruusunen A, et al. Dietary recommendations for the prevention of depression. Nutr Neurosci. (2017) 20:161–71. doi: 10.1179/1476830515Y.0000000043
50. Wang C, Pan R, Wan X, Tan Y, Xu L, Ho CS, et al. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int J Environ Res Public Health. (2020) 17:1729. doi: 10.3390/ijerph17051729
51. Lai J, Ma S, Wang Y, Cai Z, Hu J, Wei N, et al. Factors associated with mental health outcomes among health care workers exposed to Coronavirus disease 2019. JAMA Netw Open. (2020) 3:e203976. doi: 10.1001/jamanetworkopen.2020.3976
Keywords: COVID-19, older people, health literacy, health-related behaviors, depression, Vietnam
Citation: Do BN, Nguyen P-A, Pham KM, Nguyen HC, Nguyen MH, Tran CQ, Nguyen TTP, Tran TV, Pham LV, Tran KV, Duong TT, Duong TH, Nguyen KT, Pham TTM, Hsu M-H and Duong TV (2020) Determinants of Health Literacy and Its Associations With Health-Related Behaviors, Depression Among the Older People With and Without Suspected COVID-19 Symptoms: A Multi-Institutional Study. Front. Public Health 8:581746. doi: 10.3389/fpubh.2020.581746
Received: 09 July 2020; Accepted: 05 October 2020;
Published: 16 November 2020.
Edited by:
Marcia G. Ory, Texas A&M University, United StatesReviewed by:
Marissa Dickins, Bolton Clarke Research Institute, AustraliaKenneth Chui, Tufts University, United States
Copyright © 2020 Do, Nguyen, Pham, Nguyen, Nguyen, Tran, Nguyen, Tran, Pham, Tran, Duong, Duong, Nguyen, Pham, Hsu and Duong. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Tuyen Van Duong, duongtuyenvna@gmail.com
†These authors have contributed equally to this work
 Binh N. Do
Binh N. Do Phung-Anh Nguyen
Phung-Anh Nguyen Khue M. Pham
Khue M. Pham Hoang C. Nguyen7,8
Hoang C. Nguyen7,8 Minh H. Nguyen
Minh H. Nguyen Thao T. P. Nguyen
Thao T. P. Nguyen Linh V. Pham
Linh V. Pham Kien T. Nguyen
Kien T. Nguyen Thu T. M. Pham
Thu T. M. Pham Tuyen Van Duong
Tuyen Van Duong