- 1Department of Pulmonary and Critical Care Medicine, Shanghai Fifth People's Hospital, Fudan University, Shanghai, China
- 2Department of Respiratory and Critical Care Medicine, Shanghai Pulmonary Hospital, Tongji University School of Medicine, Shanghai, China
- 3Department of Respiratory and Critical Care Medicine, Shanghai Fifth People's Hospital, Fudan University, Shanghai, China
- 4Department of Respiratory Disease, Jing'an District Centre Hospital of Shanghai (Huashan Hospital Fudan University Jing'an Branch), Shanghai, China
- 5Department of Respiratory and Critical Medicine, Yangpu Hospital, Tongji Universtiy, Shanghai, China
- 6Section of Pulmonary, Critical Care and Sleep Medicine, Yale University School of Medicine, New Haven, CT, United States
- 7Department of Pulmonary and Critical Care Medicine, Tongren Hospital, Shanghai Jiao Tong University School of Medicine, Shanghai, China
- 8Department of Respiratory and Critical Care Medicine, Shanghai Eighth People's Hospital, Shanghai, China
- 9Department of Pulmonary and Critical Care Medicine, Tongji Hospital, Tongji University School of Medicine, Shanghai, China
- 10Department of Respiratory and Critical Medicine, Jiading Center Hospital, Shanghai University of Medicine & Health Sciences, Shanghai, China
- 11Department of Respiratory and Critical Medicine, Songjiang Hospital Affiliated to Shanghai Jiao Tong University School of Medicine, Shanghai, China
- 12Department of Pulmonary and Critical Care Medicine, Shanghai Sixth People's Hospital, Shanghai Jiao Tong University, Shanghai, China
- 13Department of Respiratory Medicine, Shanghai Putuo District People' Hospital, Shanghai, China
- 14Department of Respiratory Medicine, Zhongshan Hospital Subordinating Qingpu Hospital, Shanghai, China
- 15Department of Respiratory Medicine, Shanghai Pudong New Area People's Hospital, Shanghai, China
- 16Department of Respiratory Medicine, Fengxian Central Hospital, Shanghai, China
- 17Department of Respiratory Disease, Baoshan District Hospital of Integrated Traditional Chinese and Western Medicine, Shanghai, China
- 18Department of Respiratory and Critical Medicine, Shanghai Tenth People's Hospital, Shanghai, China
- 19Gumei Community Health Service Center, Shanghai, China
- 20Yinhang Community Health Service Center, Shanghai, China
- 21Zhoujiaqiao Community Health Service Center, Shanghai, China
- 22Jiuting Community Health Service Center, Shanghai, China
- 23Nanqiao Community Health Service Center, Shanghai, China
- 24Changfeng Community Health Service Center, Shanghai, China
- 25Zhuanqiao Community Health Service Center, Shanghai, China
- 26Jiading Town Community Health Service Center, Shanghai, China
- 27Jiangchuan Community Health Service Center, Shanghai, China
- 28Department of Pulmonary and Critical Care Medicine, Ruijin Hospital, Institutes of Respiratory Diseases, Shanghai Jiao Tong University School of Medicine, Shanghai, China
Background: The COVID-19 pandemic is a significant health threat. Health care worker (HCWs) are at a significant risk of infection which may cause high levels of psychological distress. The aim of this study was to investigate the psychological impact of the COVID-19 on HCWs and factors which were associated with these stresses during the first outbreak in Shanghai.
Methods: Between February 9 and 21, 2020, a total of 3,114 frontline HCWs from 26 hospitals in Shanghai completed an online survey. The questionnaire included questions on their sociodemographic characteristics, 15 stress-related questions, and General Health Questionnaire-12 (GHQ-12). Exploratory factor analysis was applied to the 15 stress-related questions which produced four distinct factors for evaluation. Multiple linear regression models were performed to explore the association of personal characteristics with each score of the four factors. Binary logistic analysis was used to explain the association of personal characteristics and these four factors with the GHQ-12.
Results: There were 2,691 valid surveys received. The prevalence of emotional distress (defined as GHQ-12 ≥ 12) was noted in 47.7% (95%CI:45.7–49.6%) HCWs. Females (OR = 1.43, 95%CI:1.09–1.86) were more likely to have a psychological distress than males. However, HCWs who work in secondary hospitals (OR = 0.71, 95% CI:0.58–0.87) or had a no contact history (OR = 0.45, 95%CI: 0.35–0.58) were less likely to suffer psychological distress. HCWs who were nurses, married, and had a known contact history were highly likely to have anxiety. HCWs working at tertiary hospitals felt an elevated anxiety regarding the infection, a lack of knowledge, and less protected compared to those who worked at secondary hospitals.
Conclusions: Our study shows that the frontline HCWs had a significant psychosocial distress during the COVID-19 outbreak in Shanghai. HCWs felt a lack of knowledge and had feelings of being not protected. It is necessary for hospitals and governments to provide additional trainings and psychological counseling to support the first-line HCWs.
Introduction
The novel coronavirus disease 2019 (COVID-19) emerged as a major healthcare challenge which has spread across the world. The etiological agent for COVID-19 was identified as an enveloped RNA betacoronavirus (1) that is named severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), which has a phylogenetic similarity to SARS-CoV (2). Despite 1 year having passed since its emergence, COVID-19 continues to cause extensive disease and death without any effective treatment. Healthcare professionals have been at major risks of epidemic especially at the first outbreak of COVID-19. It has infected at least 1,716 healthcare workers including six fatalities by February 14, 2020 (3), which was at the beginning of the epidemic in China.
World Health Organization (WHO) declared the COVID-19 as a public health emergency of international concerns (4). The pandemic had created considerable anxiety and panic worldwide including in China (5, 6). Health Care Workers (HCWs) encountered an increasing workload and a perception of being at an increased risk of infection, as in any infectious disease outbreaks. These conditions could possibly affect their psychological well-being. It is expected that the current epidemic has placed significant stresses on people including HCWs, especially during the first outbreak when there was limited knowedge regarding its transmission, disease course, and pathogenesis (7). A lot of studies conducted in China and other countries had reported that HCWs suffers depression, anxiety, and stress because of COVID-19 (8–11). Previous studies has shown that many of the HCWs presented high levels of psychological distress during these outbreaks such as the severe acute respiratory syndrome (SARS) (12), H1N1 (13), and H7N9 (14) outbreaks.
Several studies have demonstrated the psychological impact of the epidemic on health care workers in different aspects, such as medical staff working in different risk workplace (15), different medical care population in front of this pandemic (16, 17), and posttraumatic stress disorder symptoms (PTSD) (18, 19). However, only a few studies have looked into the psychological stress during the first outbreak outside Wuhan, when a very limited knowledge of the disease existed. The lack of knowledge regarding COVID-19 and absence of any effective medicine or vaccine at that time made HCWs highly vulnerable to stress. Due to the high risk of exposure, the medical staff is at a high risk of SARS-CoV-2 virus infection.
Shanghai is the largest city in China with a population of ~24 million. The first case of COVID-19 was identified on January 20, 2020 in Shanghai. A total of 342 cases was confirmed until March 8, 2020, which were scattered throughout the city (20). At the meantime, Wuhan was in the center of the pandemic. More than 40,000 medical staff from other provinces including Shanghai has been deployed to the Hubei province to assist with the medical needs in Wuhan since January 25, 2020 (15). At the beginning of the outbreak, the lack of knowledge and rising cases of death induced high levels of stress to the public. We sought to investigate the psychological impact of the initial COVID-19 outbreak in these frontline HCWs, who are working in the departments of respiratory, emergency, or infectious diseases. There were 975 physicians and 1,584 nurses who completed the survey from 26 hospitals. Twelve item version of General Health Questionnaire (GHQ-12) survey was used as described previously (21). The GHQ-12 is a well-established method to quantify stress and has been used in a wide range of conditions (22, 23). Our questionnaire was designed to assess four major factors based on the relevant factors during the early stage of pandemic. These factors included anxiety related to the infection, awareness of the COVID-19, feeling of being protected from infection, and attitude toward work in the face of the current outbreak, as described before (24, 25). Although studies had reported that COVID-19 had caused psychological problems around the world, this is the first study to define the stress in HCWs at the early stage of the pandemic in Shanghai, when limited knowledge about COVID-19 existed.
Our data showed that there was a significant psychological distress among the HCWs in Shanghai hospitals. The psychological distress was higher among the HCWs who were working in tertiary hospitals, females, and unsure of their contact history with COVID-19 infected subjects.
Methods
Subjects and Procedure
HCWs from 26 hospitals in 14 out of the 16 districts in Shanghai were invited to participate in this survey. The two excluded districts are the Huangpu and Chongming districts. Huangpu has a fewer hospitals than others due to the small area, while Chongming is an island far away from the center of Shanghai. The data for this study were collected between February 9 and February 21, 2020, which was approximately around the peak of the COVID-19 outbreak in Shanghai. The questionnaire was completed through an online survey platform (“SurveyStar,” Changsha Ranxing Science and Technology, Shanghai, China). A total of 3,114 frontline HCWs, from seven tertiary, 10 secondary, and nine primary hospitals (referred as community health centers in China) were invited to participate. Three types of hospitals are organized according to a three-tier system in China (26). Two thousand six hundred ninety-one (2,691) of the potential participants returned the survey (86.4% return rate). Among these responses, 132 were excluded because they failed to answer the quality check question correctly which explicitly asked them to pick the last option. A total of 2,559 surveys were analyzed.
Content of the Questionnaire
This questionnaire consisted of three sections: sociodemographic characteristics, GHQ-12, and stress-related questions associated with COVID-19. The sociodemographic characteristics included gender, age, occupation, technical title, marital status, level of hospital, and contact history with suspected or confirmed cases.
GHQ-12 was used to assess the HCWs' psychological distress. GHQ-12 is a well-standardized measure of recent emotional distress, which is the most widely used tool in quantitative social science and epidemiology for the analysis of mental health trends (21, 27, 28). Studies have shown the usefulness of GHQ-12 to assess the psychological impact of SARS among HCWs (21). A 4-point Likert scoring method (0, never; 1, occasionally; 2, often; 3, almost always) was used in this study. A threshold score of >12 was used to identify the presence of emotional distress (27).
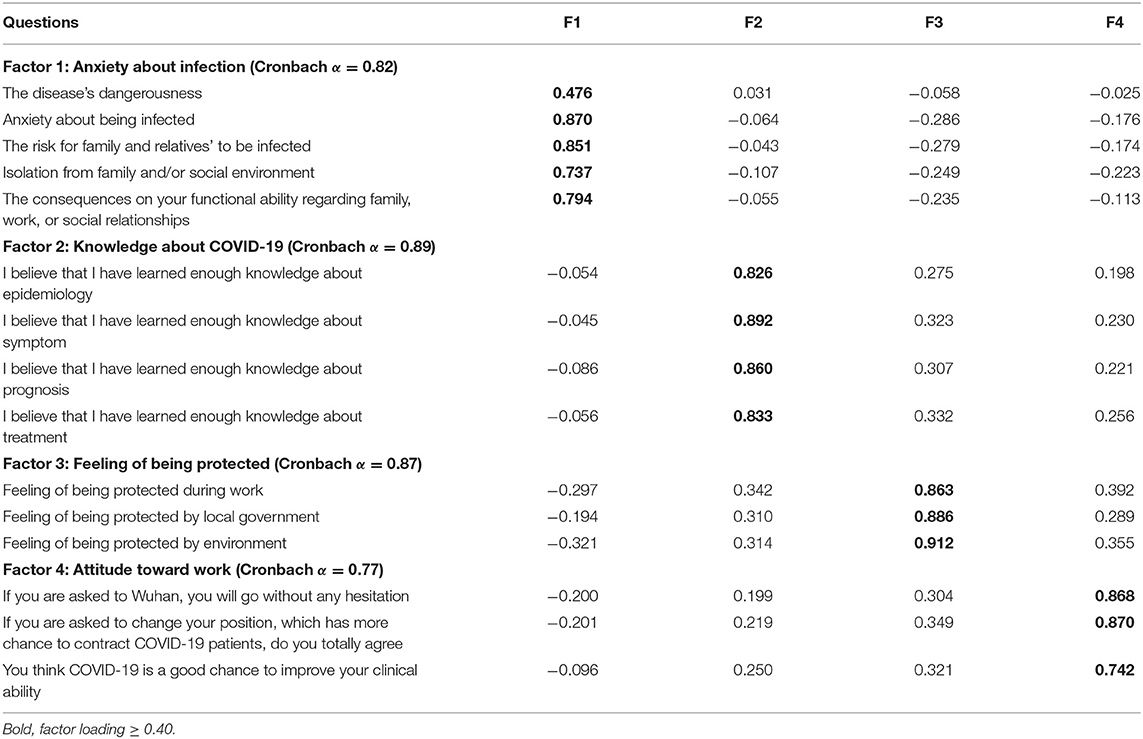
To assess the HCWs' concerns and worries about the pandemic, knowledge about COVID-19, their attitude toward work during the pandemic, and whether these factors were associated with personal characteristics, we designed 15 items of stress-related questions (Table 2). These questions were based on the previous studies of similar novel infection mediated outbreaks including the SARS (29), H1N1 pandemic (24), and avian influenza (30). We used a factor analysis to classify these 15 items to four distinct aspects of psychological stress. (a) “Anxiety about infection” included five items about the disease's dangerousness, perception of personal risk, perception of being a risk to family or friends, isolation from family, and functional ability toward social relationship. (b)“Knowledge about COVID-19” included questions about the epidemiology, symptoms, prognosis, and treatment. (c)“Feeling of being protected” included questions about the perception of feeling safe during work and at home. (d)“Attitude toward work” is designed to determine the willingness of HCWs to move to a position involving a high risk of contacting infection including moving to the epicenter of the disease. Each item was scored from 1 to 5, representing not at all, barely, a little, high, and very high, respectively. The survey was approved by the Ethical Review Board (2020-046) and the participation was voluntary.
Statistical Analysis
Summary statistics for all variables and the prevalence of psychological distress were calculated. The data are expressed as mean ± standard deviation (SD) or as a number (percent). We applied a confirmatory factor analysis to the 15 stress-related questions. Principal component analysis with varimax rotation was used for factor analysis. For each factor, the total score of the stress-related questions was calculated. Multiple linear regression models were performed to explore the association of personal characteristics with each score of the four factors. Binary logistic analyses were used to explain the association of personal characteristics and these four factors with GHQ-12.
Statistical analysis were carried out using the SPSS (version 21) and graphs were prepared using the GraphPad Prism 8.
Results
Demographic Information
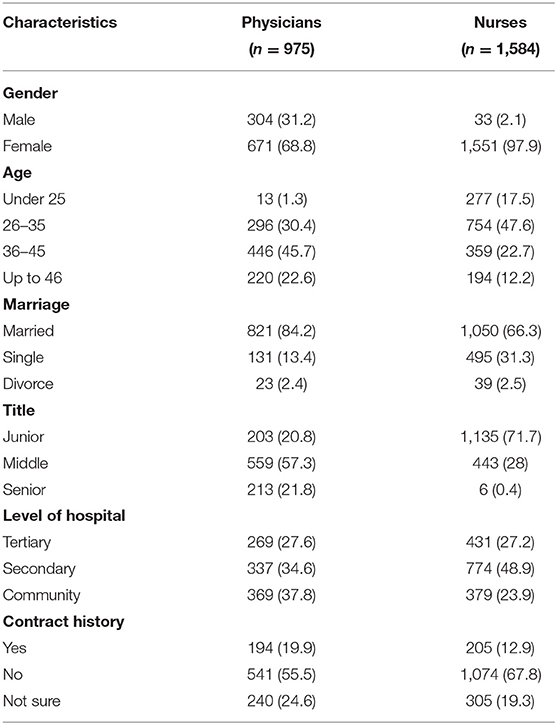
The basic demographic information was given in Table 1. A total of 2,559 answers from 26 hospitals in 14 out of the 16 districts of Shanghai were analyzed. The participants included 975 physicians (38.1%) and 1,584 nurses (61.9%). Majority of the responders were female, with a proportion of 68.8% in physicians and 97.9% in nurses, which reflects the overall population of the HCWs in Shanghai hospitals. Most of the nurses were 26–35 years old (47.6%) while most of the physicians were 36–45 years old (45.7%). Most of the HCWs were married. HCWs with junior and middle levels of technical title consisted the majority of the participants in this survey. 34.6 and 37.8% of participants in physicians were from secondary hospitals and community healthcare center, respectively. 48.9% of the nurses were from a secondary hospital. Most of them, 55.5% of the physicians and 67.8% of the nurses, did not had a suspected or confirmed contact with COVID-19 patients.
Factors Associated With the Presence of Psychological Distress
The Cronbach alpha coefficient of the GHQ-12 in this study was 0.81, a level considered good for internal consistency. The prevalence of high scores (GHQ-12 ≥ 12) was in 47.7% (95%CI 45.7–49.6%) of the respondents, which indicated an elevated psychological distress among HCWs. As shown in Figure 1, multivariate analyses found that females were more likely to have a higher emotional distress than males (OR = 1.43, 95%CI: 1.09–1.86). However, HCWs working at secondary hospitals (OR = 0.71, 95%CI: 0.58–0.87) or among those who had a no known contact history (OR = 0.45, 95%CI: 0.35–0.58) were less likely to have a psychological distress compared with those who are working at tertiary or primary hospitals or had a known or suspected contact history. In contrast, age, marital status, occupation, and technical title were not associated with psychological distress.
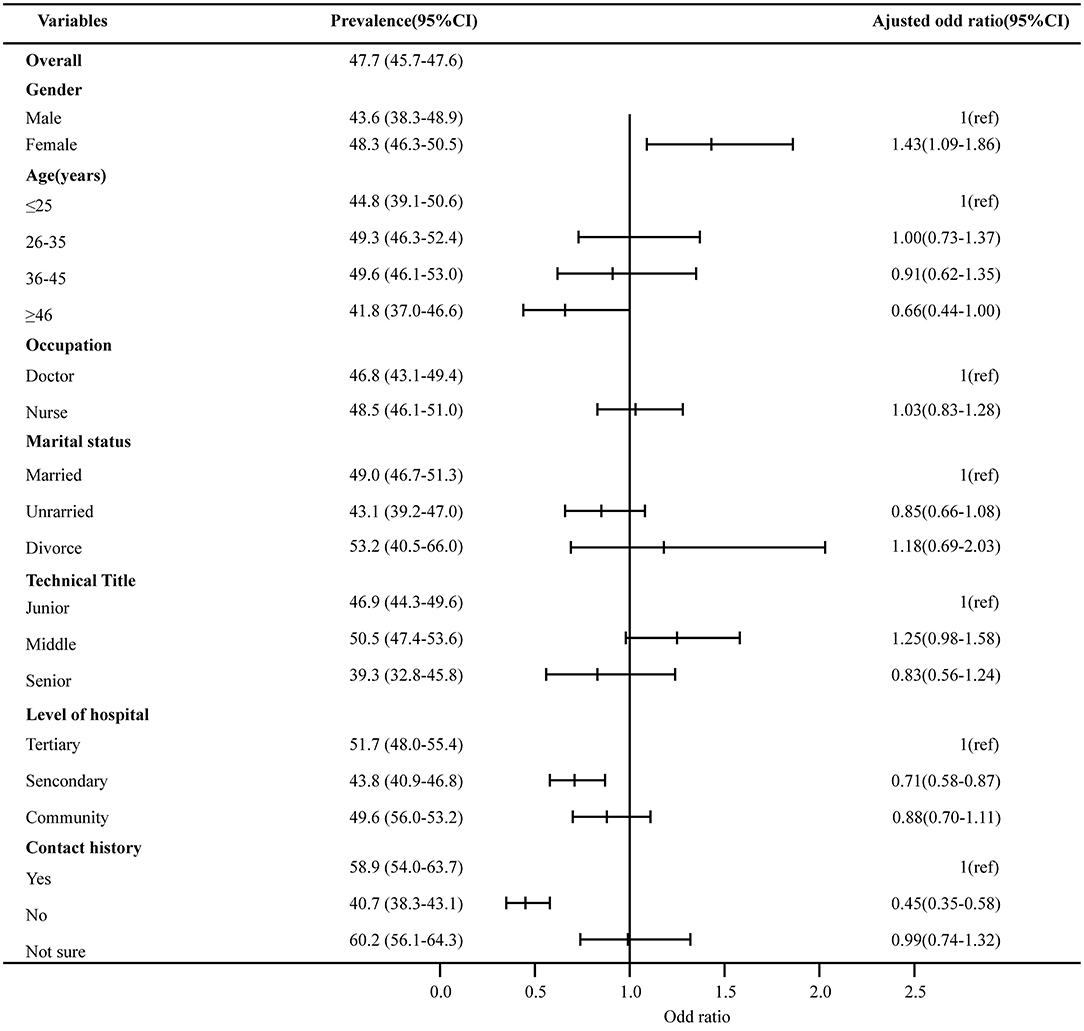
Figure 1. Factors associated with the presence of psychological distress. The prevalence of psychological distress with 95% CI of independent variables is presented on the left column. Multivariate analyses were used to calculate the adjusted odds ratio of psychological distress, adjusted ORs, and their 95% CI were shown in the figures, and the numbers are given in the right column.
The Association of Personal Characteristics With Each Score of the Four Factors
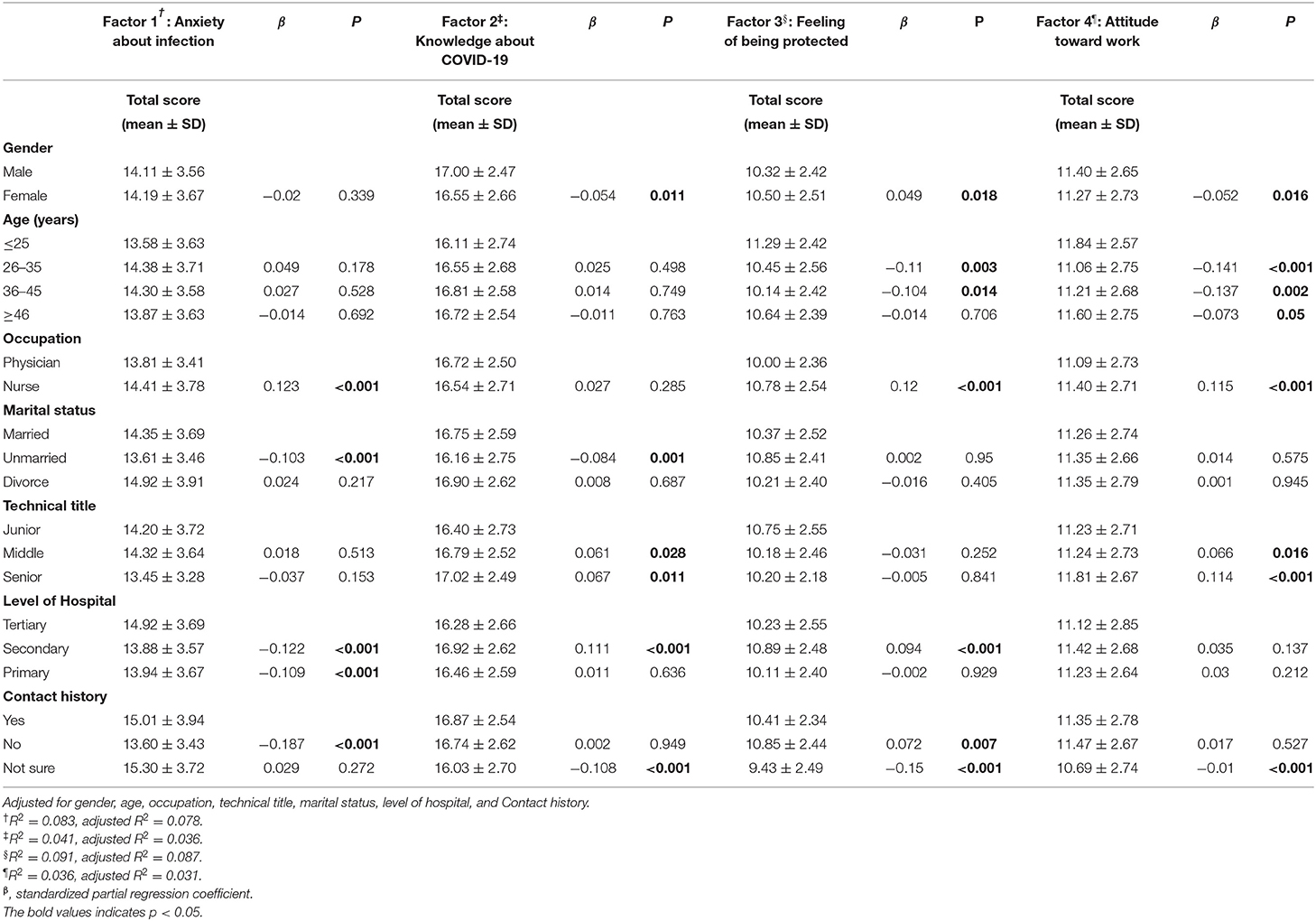
Four factors were classification from the 15 questionnaire items having factor loadings ≥ 0.40 (Table 2). Exploratory factor analysis on the 15 items of perceived threat yielded four factors (explaining 68.8% of the total variance; KMO = 0.83). The Cronbach alpha coefficient of the 15 stress-related questions was 0.80, again indicating a good internal consistency and reliability. Estimated associations between the sociodemographic characteristics with the total score in each of the four factors is indicated in Table 3. The detailed scores for the four factors were showed in Supplementary Table 1. The comparison between nurse and physician in the four factors was also analyzed (Please see Supplementary Table 2).
Worries About the COVID-19 Pandemic
For factor 1, “Anxiety about infection,” nurses were more likely to have anxiety than physicians [partial regression coefficient (B) = 0.926, SE = 0.178, β = 0.123, P < 0.001]. Married or divorce workers were associated with more anxiety than unmarried workers (B = −0.874, SE = 0.214, β = −0.103, P < 0.001). HCWs at tertiary hospitals felt more anxiety than those at secondary or primary hospitals (secondary hospitals: B = −0.901, SE = 0.171, β = −0.122, P < 0.001; primary hospitals: B = −0.875, SE = 0.191, β = −0.109, P < 0.001). In regard to contact history, people who had a no known contact history felt less anxiety compared to those who had a known contact with a COVID-19 patient or were not sure about their contact history (B = −1.413, SE = 0.202, β = −0.187, P < 0.001).
Perceived Knowledge of the COVID-19 Pandemic
For factor 2, “Knowledge about COVID-19,” females felt that they were less aware about the COVID-19 than their male counterparts (B = −0.424, SE = 0.168, β = −0.054, P = 0.011). Unmarried HCWs reported less knowledge compared to the married and divorced HCWs (B = −0.518, SE = 0.158, β = −0.084, P = 0.001). HCWs at tertiary hospitals were more likely to feel that they had less knowledge compared to HCWs at secondary hospitals (B = 0.59, SE = 0.126, β = 0.111, P < 0.001). In regard to the contact history, HCWs who were not sure of their contact history felt that they lack knowledge more (B = −0.698, SE = 0.174, β = −0.108, P < 0.001). There was no association between the age, occupation, and technical title and perception of knowledge about COVID-19.
Concerns on Environmental Safety During the COVID-19 Pandemic
For factor 3, “Feeling of being protected,” males felt less protected than the female HCWs (B = 0.364, SE = 0.154, β = 0.049, P = 0.018). Similarly, physicians also thought that they lacked protection than the nurses (B = 0.617, SE = 0.127, β = 0.12, P < 0.001). HCWs who were 25–35 y and 36–45 y felt less protected (25–35y: B = −0.558, SE = 0.185, β = −0.11, P = 0.003; 36–45y: B = −0.56, SE = 0.227, β = −0.104, P = 0.014). Workers at secondary hospitals thought they were well-protected compared with workers at tertiary hospitals and community service centers (B = −0.475, SE = 0.117, β = 0.094, P < 0.001). In regard to the contact history, workers who did not have a contact history felt well-protected than others (B = 0.371, SE = 0.137, β = 0.072, P = 0.007). On the other hand, HCWs who were not sure of their contact history felt less protected (B = −0.917, SE = 0.16, β = −0.15, P < 0.001).
Impact on Work Attitude During the COVID-19 Pandemic
For factor 4, “Attitude toward work,” males and nurses had a more positive attitude toward work than females (B = −0.416, SE = 0.173, β = −0.052, P = 0.016) and physicians (B = 0.646, SE = 0.142, β = 0.115, P < 0.001), respectively. HCWs of age under 25 y were the most willing group of all ages when they were asked to move to a position involving a high risk of contacting infection. HCWs with a technical title of senior showed a positive attitude toward work than HCWs with junior or middle titles (B = 1.111, SE = 0.258, β = 0.114, P < 0.001). HCWs who were not sure of their contact history had a negative attitude toward work (B = −0.665, SE = 0.18, β = −0.01, P < 0.001).
The Association of GHQ-12 With Scores of Each of the Four Factors
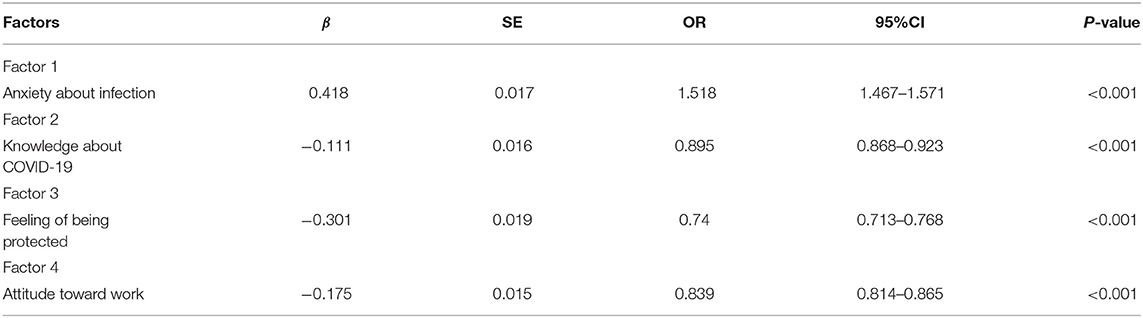
Logistic regression was performed to identify the association between emotional distress and the four factors as shown in Table 4. All four factors were positively correlated with a higher distress. The feeling of anxiety about infection was positively correlated with a high GHQ-12 score [OR = 1.518 (1.467, 1.571)]. Both the feeling of a lack of knowledge and being less protected led to a higher anxiety and psychological distress [OR = 0.895 (0.868, 0.923) and OR = 0.74 (0.713, 0.768), respectively]. HCWs with a positive attitude toward work had less psychological distress [OR = 0.839 (0.814, 0.865)]. Furthermore, the correlation among these factors are indicated in Supplementary Figure 1.
Discussion
The ongoing pandemic of COVID-19 is one of the worst respiratory viral infections in the twenty-first century. It has surpassed the SARS (8,098 patients with 774 deaths) outbreak of 2002–2003 (31) and MERS outbreak (2,506 infections with 862 deaths) of 2012 (32). Due to the highly contagious nature of the infection, HCWs are at a heightened risk of getting the coronavirus infection (33). At the first few weeks of this pandemic, a sharp increase in the number of confirmed cases, along with the lack of a clear knowledge about the possible modes of transmission and availability of effective therapeutics, has created widespread panic in the general population, including among the HCWs. At the same time, HCWs from all over the country were asked to volunteer to go to Wuhan to serve at the epicenter of the disease. The volunteers included HCWs from Shanghai, especially those working in the departments of Respiratory, Emergency, and Infectious diseases. Although many studies have reported the psychological effects during COVID-19, a few studies have focused on the psychologic problems experienced by HCWs in Shanghai and during the early stage of the pandemic.
Some studies have reported that COVID-19 caused psychological impacts in other countries as the pandemic has spread all over the world. The study from Italy has shown that the greatest prevalence of psychological distress was reported in the <34 years age group and in north Italy. The psychological impact influenced important daily life activities, such as sexuality and nutrition among the general population (34). Leivy Patricia et al. reported that during the phase 2 of the COVID-19 outbreak in Mexico, psychological distress and post-traumatic stress symptoms were present in over a quarter of the population (35). A French study reported that a hospital staff displayed the psychological consequences of pandemic stress, resulting in the use of anxiolytics and sleeping pills (36). Another survey on nurses in the USA showed that nurses who lack access to adequate personal protective equipment were more likely to report symptoms of depression, anxiety, and post-traumatic stress disorder (37).
Our study shows that 47.7% of the HCWs experienced psychological distress based on the GHQ-12 score. We only chose the GHQ-12 which has been used in various studies for many years because of the intensive schedule of the medical staff. Fu et al. used the GHQ-12 to study the psychological impact of the COVID-19 cases on the medical staff of Beijing Xiaotangshan Hospital on March 20 to 29, 2020. The results show that the medical staff working at Xiaotangshan Hospital underwent relatively low levels (17%) of emotional distress (38). A meta-analysis of other studies showed that the prevalence of anxiety in healthcare workers was 26% (18–34%), ranged between 7% (5–9%) in Singapore and 57% (52–63%) in Italy (9). Other studies which looked into PTSD reported that 40.2% of the health care professionals indicated positive screens for significant posttraumatic stress disorder symptoms (18). To investigate further in-depth of the mental state of HCWs, a French study reported that 32% had symptoms of anxiety, 16% of depression, and 16% of post-traumatic stress disorder (36). Compared to these studies on the psychological impact of COVID-19 among health care workers, our study showed a higher prevalence of psychological distress in HCWs. This difference may be explained by the following reasons: Firstly, our study was conducted between February 9 to 21, 2020, which was the beginning of the outbreak, while other studies were carried out at the later stages. Secondly, other studies, including in China for the dedicated COVID-19 hospitals such as the Beijing Xiaotangshan Hospital, reported a lower psychological stress (38). This may be due to the renovation of the Beijing Xiaotangshan Hospital as the designated hospital for the screening and treating of COVID-19 cases, which had sufficient medical and psychological preparations. Compared with other studies on the psychological impact of COVID-19 among health care workers using other measurements, our study used the GHQ-12. This was simpler than other studies who used more than one scale, such as the IES (Impact of Event Scale), Seven-Item Generalized Anxiety Disorder Scale (GAD-7), and DASS (Depression, Anxiety, and Stress Scale). Different measurement tools may bring different results. Lack of knowledge and insufficient psychological coping strategies to the disease at the first outbreak may be essential components to make an impact on the psychological well-being.
However, other studies also revealed a prevalence of psychological problems, which was even higher than our study. Marques used the GHQ-12 to study the impact of COVID-19 on the psychological health of university students in Spain. The result shows that 52.1% of the respondents were classified as high scores (39). Another study demonstrated a high prevalence of mental health symptoms among health care workers treating patients with COVID-19 in China, which revealed that 50.4, 44.6, 34.0, and 71.5% of all the participants reported symptoms of depression, anxiety, insomnia, and distress, respectively (8). Reports of the psychological impact of SARS on hospital staff indicated that high levels of distress were common (40). During the SARS epidemics, 68% of the HCWs reported a high level of stress and about 57% were found to have experienced psychological distress in Hong Kong (25).
In this study, HCWs who were female, working at tertiary hospitals, with confirmed or unsure contact history had a significantly elevated psychological distress. However, the level of stress was not significantly affected by age, occupation, technical total, and marital status. Females more easily perceive a higher lack of knowledge about COVID-19 than males in our study, a possible contributing factor to distress in females. A significant association was noted between the prevalence of psychological distress and contact history with suspected or confirmed patients. HCWs who had a no known contact history had a lower psychological distress compared to those who had a known contact with a COVID-19 patient or were unsure of their contact history. On similar lines, Ko et al. (41) also reported that a direct or indirect exposure to SARS would bring a greater psychological impact on the public. Tang et al. (14) also showed that the PTSD level among physicians and nurses after their exposure to H7N9 patients was high. Nurses were more likely to have a higher distress about being infected compared to the physicians. Similar results were reported in other studies about the COVID-19 (8, 42) and SARS outbreak (31, 43). Nurses often need to spend more time with infectious patients and are in closer contact with patients. Nurses constitute the largest workforce in the hospitals and are directly and intensively involved in patient care, experiencing a greater risk.
Higher number of patients including the number of beds in tertiary hospitals may increase the chances of contact with suspected or confirmed patients. On the other hand, many HCWs were asked to volunteer to Wuhan after the out coming traffic from Wuhan was blocked on January 23, 2020. Most of these HCWs going to Wuhan came from tertiary hospitals. This may be one of the contributing factors for a higher psychological distress in tertiary hospitals. Factor analysis results show that HCWs at tertiary hospitals and people unsure of their contact history had a higher anxiety about the infection, felt that they lacked the knowledge, and felt less protected than those at secondary hospitals and people with no contact history, indicating that all the three factors might contribute to psychological distress. HCWs working in primary hospitals were more likely to have a higher emotional distress than those at secondary hospitals. At the early stage of the pandemic, many of the suspected patients from other cities and community residents were recommended to isolate themselves at home or hotels for 14 days. The medical staffs at primary hospitals were responsible for monitoring their health changes. This may have led to the higher distress in these HCWs.
The results revealed that HCWs who had a higher anxiety regarding the infection were more likely to have a psychological distress. The feeling of lack of knowledge and not being protected led to higher levels of anxiety. These factors emphasize the need to minimize the stress at work. Decreasing psychological distress could give HCWs a positive attitude toward work when they are needed at the frontline during emerging pandemics such as COVID-19.
Our study was conducted during the peak of the initial phase of the COVID-19 outbreak in Shanghai, when information was changing rapidly and knowledge about the disease was limited. As the disease evolves and institutional policies are implemented, the HCWs' perceptions and experience may change. Future follow-up investigations, using both qualitative and quantitative approaches, will be necessary to understand the psychosocial effects of COVID-19 on HCWs over time after significant knowledge and preventive vaccines are administered. Because the adjusted R2 in Table 3 is low, future studies should look for other variables that can better explain the psychological impact of a pandemic. Overall, we recommend an appropriate training and support to the HCWs to ensure their psychological well-being, as effective clinical service depends on their overall and psychological well-being.
Limitations
This study has some limitations. The multicenter design of the study did not allow us to transpose its conclusions to all types of hospital staff. Most of the respondents were female which may limit the generalizability of the findings. Another limitation is that only one measurement tool was used to evaluate the HCWs' psychological problems, which might be insufficient to evaluate all psychological problems. Thirdly, we did not evaluate the psychological distress of the participants after the pandemic. A follow-up study on the same participants should be conducted to observe the persistence of the perceived psychological distress.
Conclusion
This study examined the emotional distress experienced by HCWs responding to COVID-19 in Shanghai, China during the first outbreak of the disease outside Wuhan. HCWs felt a lack of knowledge about COVID-19 and had feelings of being unprotected. It is necessary for hospitals and governments to implement not only more prevention strategies, but also psychological supports for the frontline HCWs.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
Ethics Statement
The studies involving human participants were reviewed and approved by Shanghai Ethical Review Board (2020-046) and the participation was voluntary. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
Author Contributions
JF for interpretation of the data, preparation, funding acquisition, and writing-original draft. JX for conceptualization and design. SX for software, writing-review, and editing. LS and CSD for writing-review and editing. HC, CZ, JinZ, DC, LY, CTu, FL, TR, FZ, CD, WG, HL, YQ, CS, CTa, YB, FX, KG, JieZ, ZY, LZ, JZhai, and XH for resources supply. JQ for conceptualization, writing-review, and editing. ZJ for conceptualization, interpretation of the data, resources, funding acquisition, writing-review, and editing. All authors contributed to the article and approved the submitted version.
Funding
This study was supported by the Specialized Department Foundation of the Minhang District (No: 2020MWTZB02) and High-level professional physician training program of the Minhang District (No: 2020MZYS12).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpubh.2021.646780/full#supplementary-material
Supplementary Figure 1. Correlation among the four factors: Spearman correlation analysis was performed to assess the correlation among the four factors. In total, six figures were shown to express correlations between each other. Spearman r-value and p-value are shown beside each figure.
Supplementary Table 1. The score of the four factors with personal characteristics.
Supplementary Table 2. Factors and prevalence of psychological problem in different occupation.
Abbreviations
HCWs, Health care worker; GHQ-12, General Health Questionnaire-12; COVID-19, The novel coronavirus disease 2019; WHO, World Health Organization; SARS, severe acute respiratory syndrome; MERS, Middle East Respiratory Syndrome Coronavirus; Cis, Confidence intervals; β, Standardized partial regression coefficients; PTSD, Post-traumatic stress disorder; IES, Impact of Event Scale; GAD-7, Seven-Item Generalized Anxiety Disorder Scale; DASS, Depression, Anxiety and Stress Scale.
References
1. Lu R, Zhao X, Li J, Niu P, Yang B, Wu H, et al. Genomic characterisation and epidemiology of 2019 novel coronavirus: implications for virus origins and receptor binding. Lancet. (2020) 395:565–74. doi: 10.1016/S0140-6736(20)30251-8
2. Zhu N, Zhang D, Wang W, Li X, Yang B, Song J, et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. (2020) 382:727–33. doi: 10.1056/NEJMoa2001017
3. Zhang Y. The epidemiological characteristics of an outbreak of 2019 novel coronavirus diseases (COVID-19) in China. Zhonghua Liuxingbingxue Za Zhi. (2020) 41:145–51. doi: 10.3760/cma.j.issn.0254-6450.2020.02.003
4. WHO. Director-General's Statement on IHR Emergency Committee on Novel Coronavirus (2019-nCoV). World Health Organization. (2020). Available online at: https://www.who.int/director-general/speeches/detail/who-director-general-s-statement-on-ihr-emergency-committee-on-novel-coronavirus-(2019-ncov) (accessed January 30, 2020).
5. Zhang W, Wang K, Yin L, Zhao W, Xue Q, Peng M, et al. Mental health and psychosocial problems of medical health workers during the COVID-19 epidemic in China. Psychotherapy Psychosomatics. (2020) 89:242–50. doi: 10.1159/000507639
6. Liang Y, Wu K, Zhou Y, Huang X, Zhou Y, Liu Z. Mental health in frontline medical workers during the 2019 novel coronavirus disease epidemic in China: a comparison with the general population. Int J Environ Res Public Health. (2020) 17:186550. doi: 10.3390/ijerph17186550
7. Du J, Dong L, Wang T, Yuan C, Fu R, Zhang L, et al. Psychological symptoms among frontline healthcare workers during COVID-19 outbreak in Wuhan. General Hospital Psychiatry. (2020) 67:144–5. doi: 10.1016/j.genhosppsych.2020.03.011
8. Lai J, Ma S, Wang Y, Cai Z, Hu J, Wei N, et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Network Open. (2020) 3:e203976. doi: 10.1001/jamanetworkopen.2020.3976
9. Luo M, Guo L, Yu M, Jiang W, Wang H. The psychological and mental impact of coronavirus disease 2019 (COVID-19) on medical staff and general public—a systematic review and meta-analysis. Psychiatry Res. (2020) 291:113190. doi: 10.1016/j.psychres.2020.113190
10. d'Ettorre G, Ceccarelli G, Santinelli L, Vassalini P, Innocenti G, Alessandri F, et al. Post-traumatic stress symptoms in healthcare workers dealing with the COVID-19 pandemic: a systematic review. Int J Environ Res Public Health. (2021) 18:20601. doi: 10.3390/ijerph18020601
11. Cag Y, Erdem H, Gormez A, Ankarali H, Hargreaves S, Ferreira-Coimbra J, et al. Anxiety among front-line health-care workers supporting patients with COVID-19: a global survey. General Hospital Psychiatry. (2021) 68:90–6. doi: 10.1016/j.genhosppsych.2020.12.010
12. Lin CY, Peng YC, Wu YH, Chang J, Chan CH, Yang DY. The psychological effect of severe acute respiratory syndrome on emergency department staff. Emerg Med J. (2007) 24:12–7. doi: 10.1136/emj.2006.035089
13. Liao Q, Cowling BJ, Lam WW, Ng DM, Fielding R. Anxiety, worry and cognitive risk estimate in relation to protective behaviors during the 2009 influenza A/H1N1 pandemic in Hong Kong: 10 cross-sectional surveys. BMC Infect Dis. (2014) 14:169. doi: 10.1186/1471-2334-14-169
14. Tang L, Pan L, Yuan L, Zha L. Prevalence and related factors of post-traumatic stress disorder among medical staff members exposed to H7N9 patients. Int J Nurs Sci. (2017) 4:63–7. doi: 10.1016/j.ijnss.2016.12.002
15. Wang L, Zhang M, Liu G, Nan S, Li T, Xu L, et al. Psychological impact of coronavirus disease (2019) (COVID-19) epidemic on medical staff in different posts in China: a multicenter study. J Psychiatric Res. (2020) 129:198–205. doi: 10.1016/j.jpsychires.2020.07.008
16. Ni J, Wang F, Liu Y, Wu M, Jiang Y, Zhou Y, et al. Psychological impact of the COVID-19 pandemic on Chinese health care workers: cross-sectional survey study. JMIR Mental Health. (2021) 8:e23125. doi: 10.2196/23125
17. Que J, Shi L, Deng J, Liu J, Zhang L, Wu S, et al. Psychological impact of the COVID-19 pandemic on healthcare workers: a cross-sectional study in China. General Psychiatry. (2020) 33:e100259. doi: 10.1136/gpsych-2020-100259
18. Si M, Su X, Jiang Y, Wang W, Gu X, Ma L, et al. Psychological impact of COVID-19 on medical care workers in China. Infect Dis Poverty. (2020) 9:113. doi: 10.1186/s40249-020-00724-0
19. Geng S, Zhou Y, Zhang W, Lou A, Cai Y, Xie J, et al. The influence of risk perception for COVID-19 pandemic on posttraumatic stress disorder in healthcare workers: a survey from four designated hospitals. Clin Psychol Psychotherapy. (2021). doi: 10.1002/cpp.2564. [Epub ahead of print].
20. SMHC. Shanghai Municipal Health Commission: Report for confirmed COVID 19 cases in Shanghai at March 8th 2020. (2020). Available online at: http://wsjkw.sh.gov.cn/xwfb/20200309/8cd055e9ae5840a781764423a505397c.html (accessed March 09, 2020).
21. Nickell LA, Crighton EJ, Tracy CS, Al-Enazy H, Bolaji Y, Hanjrah S, et al. Psychosocial effects of SARS on hospital staff: survey of a large tertiary care institution. CMAJ. (2004) 170:793–8. doi: 10.1503/cmaj.1031077
22. Mäkikangas A, Feldt T, Kinnunen U, Tolvanen A, Kinnunen M, Pulkkinen L. The factor structure and factorial invariance of the 12-item General Health Questionnaire (GHQ-12) across time: evidence from two community-based samples. Psychol Assessment. (2006) 18:444–51. doi: 10.1037/1040-3590.18.4.444
23. Hystad S, Johnsen B. The dimensionality of the 12-item general health questionnaire (GHQ-12): comparisons of factor structures and invariance across samples and time. Front Psychol. (2020) 11:1300. doi: 10.3389/fpsyg.2020.01300
24. Matsuishi K, Kawazoe A, Imai H, Ito A, Mouri K, Kitamura N, et al. Psychological impact of the pandemic (H1N1) 2009 on general hospital workers in Kobe. Psychiatry Clin Neurosci. (2012) 66:353–60. doi: 10.1111/j.1440-1819.2012.02336.x
25. Tam CW, Pang EP, Lam LC, Chiu HF. Severe acute respiratory syndrome (SARS) in Hong Kong in 2003: stress and psychological impact among frontline healthcare workers. Psychol Med. (2004) 34:1197–204. doi: 10.1017/S0033291704002247
26. Li X, Huang J, Zhang H. An analysis of hospital preparedness capacity for public health emergency in four regions of China: Beijing, Shandong, Guangxi, and Hainan. BMC Public Health. (2008) 8:319. doi: 10.1186/1471-2458-8-319
27. Goldberg DP, Gater R, Sartorius N, Ustun TB, Piccinelli M, Gureje O, et al. The validity of two versions of the GHQ in the WHO study of mental illness in general health care. Psychol Med. (1997) 27:191–7. doi: 10.1017/S0033291796004242
28. Griffith GJ, Jones K. Understanding the population structure of the GHQ-12: methodological considerations in dimensionally complex measurement outcomes. Soc Sci Med. (2019) 243:112638. doi: 10.1016/j.socscimed.2019.112638
29. Maunder R. The experience of the 2003 SARS outbreak as a traumatic stress among frontline healthcare workers in Toronto: lessons learned. Philos Trans R Soc Lond B Biol Sci. (2004) 359:1117–25. doi: 10.1098/rstb.2004.1483
30. Wong TY, Koh GC, Cheong SK, Sundram M, Koh K, Chia SE, et al. A cross-sectional study of primary-care physicians in Singapore on their concerns and preparedness for an avian influenza outbreak. Ann Acad Med. (2008) 37:458–64.
31. Drosten C, Gunther S, Preiser W, van der Werf S, Brodt HR, Becker S, et al. Identification of a novel coronavirus in patients with severe acute respiratory syndrome. N Engl J Med. (2003) 348:1967–76. doi: 10.1056/NEJMoa030747
32. Killerby ME, Biggs HM, Midgley CM, Gerber SI, Watson JT. Middle east respiratory syndrome coronavirus transmission. Emerg Infect Dis. (2020) 26:191–8. doi: 10.3201/eid2602.190697
33. Chang, Lin M, Wei L, Xie L, Zhu G, Dela Cruz CS, et al. Epidemiologic and clinical characteristics of novel coronavirus infections involving 13 patients outside Wuhan, China. JAMA. (2020) 323:1092–3. doi: 10.1001/jama.2020.1623
34. Ferrucci R, Averna A, Marino D, Reitano M, Ruggiero F, Mameli F, et al. Psychological impact during the first outbreak of COVID-19 in Italy. Front Psychiatry. (2020) 11:559266. doi: 10.3389/fpsyt.2020.559266
35. Gonzalez Ramirez LP, Martinez Arriaga RJ, Hernandez-Gonzalez MA, De la Roca-Chiapas JM. Psychological distress and signs of post-traumatic stress in response to the COVID-19 health emergency in a Mexican sample. Psychol Res Behav Manag. (2020) 13:589–97. doi: 10.2147/PRBM.S259563
36. Flateau C, Noël C, Bonnafoux A, Fuentes E, de Pontfarcy A, Diamantis S. Psychological impact of the SARS-CoV-2 outbreak on the staff of a French Hospital. Infect Dis. (2021) 51:187–93. doi: 10.1016/j.idnow.2021.01.007
37. Arnetz J, Goetz C, Sudan S, Arble E, Janisse J, Arnetz B. Personal protective equipment and mental health symptoms among nurses during the COVID-19 pandemic. J Occup Environ Med. (2020) 62:892–7. doi: 10.1097/JOM.0000000000001999
38. Fu Y, Wang M, Zhao B, Liu B, Sun J, Feng Y, et al. Psychological impact of COVID-19 cases on medical staff of Beijing Xiaotangshan Hospital. Psychol Res Behav Manag. (2021) 14:41–7. doi: 10.2147/PRBM.S287842
39. Marques G, Drissi N, Díez I, de Abajo B, Ouhbi S. Impact of COVID-19 on the psychological health of university students in Spain and their attitudes toward Mobile mental health solutions. Int J Med Informat. (2021) 147:104369. doi: 10.1016/j.ijmedinf.2020.104369
40. Maunder RG, Lancee WJ, Rourke S, Hunter JJ, Goldbloom D, Balderson K, et al. Factors associated with the psychological impact of severe acute respiratory syndrome on nurses and other hospital workers in Toronto. Psychosom Med. (2004) 66:938–42. doi: 10.1097/01.psy.0000145673.84698.18
41. Ko CH, Yen CF, Yen JY, Yang MJ. Psychosocial impact among the public of the severe acute respiratory syndrome epidemic in Taiwan. Psychiatry Clin Neurosci. (2006) 60:397–403. doi: 10.1111/j.1440-1819.2006.01522.x
42. Qiu J, Shen B, Zhao M, Wang Z, Xie B, Xu Y. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: implications and policy recommendations. General Psychiatry. (2020) 33:e100213. doi: 10.1136/gpsych-2020-100213
Keywords: COVID-19 pandemic, hospital care workers, psychological distress, first outbreak, GHQ-12
Citation: Feng J, Xu J, Xu S, Cao H, Zheng C, Sharma L, Dela Cruz CS, Zhang J, Chu D, Yu L, Tu C, Li F, Ren T, Zhang F, Du C, Gu W, Liu H, Qian Y, Shen C, Tang C, Bi Y, Xiao F, Gu K, Zhang J, Ye Z, Zhao L, Zhai J, Hu X, Qu J and Jie Z (2021) Psychological Impact During the First Outbreak of COVID-19 on Frontline Health Care Workers in Shanghai. Front. Public Health 9:646780. doi: 10.3389/fpubh.2021.646780
Received: 07 January 2021; Accepted: 18 March 2021;
Published: 17 May 2021.
Edited by:
Caterina Ledda, University of Catania, ItalyReviewed by:
Monia Vagni, University of Urbino Carlo Bo, ItalyTiziana Maiorano, University of Urbino Carlo Bo, Italy
Copyright © 2021 Feng, Xu, Xu, Cao, Zheng, Sharma, Dela Cruz, Zhang, Chu, Yu, Tu, Li, Ren, Zhang, Du, Gu, Liu, Qian, Shen, Tang, Bi, Xiao, Gu, Zhang, Ye, Zhao, Zhai, Hu, Qu and Jie. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zhijun Jie, jiezjlxh@163.com; Jieming Qu, jmqu0906@163.com
†These authors have contributed equally to this work and share first authorship
 Jingjing Feng
Jingjing Feng Jinfu Xu
Jinfu Xu Susu Xu3†
Susu Xu3† Lokesh Sharma
Lokesh Sharma Charles S. Dela Cruz
Charles S. Dela Cruz Changxing Shen
Changxing Shen Jieming Qu
Jieming Qu Zhijun Jie
Zhijun Jie