Are the Levels of Lipid Parameters Associated with Biometeorological Conditions?
Abstract
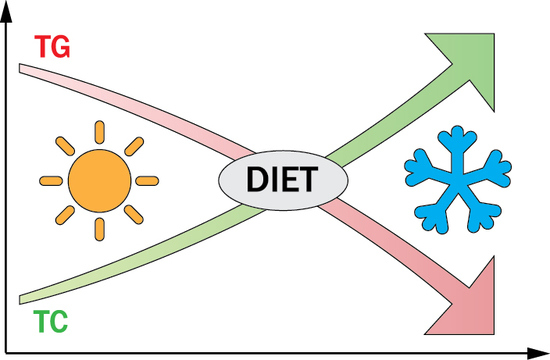
:1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Meteorological Data
2.3. Special Situations
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
6. Limitations
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Farzadfar, F.; Finucane, M.M.; Danaei, G.; Pelizzari, P.M.; Cowan, M.J.; Paciorek, C.J.; Singh, G.M.; Lin, J.K.; Stevens, G.A.; Riley, L.M. National, regional, and global trends in serum total cholesterol since 1980: Systematic analysis of health examination surveys and epidemiological studies with 321 country-years and 3·0 million participants. Lancet 2011, 377, 578–586. [Google Scholar] [CrossRef]
- McEvoy, C.T.; Temple, N.; Woodside, J.V. Vegetarian diets, low-meat diets and health: A review. Pub. Health Nutr. 2012, 15, 2287–2294. [Google Scholar] [CrossRef] [PubMed]
- Catapano, A.L.; Graham, I.; De Backer, G.; Wiklund, O.; Chapman, M.J.; Drexel, H.; Hoes, A.W.; Jennings, C.S.; Landmesser, U.; Pedersen, T.R. 2016 ESC/EAS guidelines for the management of dyslipidaemias. Eur. Heart J. 2016, 37, 2999–3058. [Google Scholar] [CrossRef] [PubMed]
- Marti-Soler, H.; Gubelmann, C.; Aeschbacher, S.; Alves, L.; Bobak, M.; Bongard, V.; Clays, E.; De Gaetano, G.; Di Castelnuovo, A.; Elosua, R. Seasonality of cardiovascular risk factors: An analysis including over 230,000 participants in 15 countries. Heart 2014, 100, 1517–1523. [Google Scholar] [CrossRef]
- Vedel-Krogh, S.; Kobylecki, C.J.; Nordestgaard, B.G.; Langsted, A. The Christmas holidays are immediately followed by a period of hypercholesterolemia. Atherosclerosis 2019, 281, 121–127. [Google Scholar] [CrossRef]
- Nadif, R.; Goldberg, S.; Gourmelen, J.; Ozguler, A.; Goldberg, M.; Zins, M.; Henny, J. Seasonal variations of lipid profiles in a French cohort. Atherosclerosis 2019, 286, 181–183. [Google Scholar] [CrossRef]
- Ockene, I.S.; Chiriboga, D.E.; Stanek, E.J., III; Harmatz, M.G.; Nicolosi, R.; Saperia, G.; Well, A.D.; Freedson, P.; Merriam, P.A.; Reed, G. Seasonal variation in serum cholesterol levels: Treatment implications and possible mechanisms. Arch. Intern. Med. 2004, 164, 863–870. [Google Scholar] [CrossRef]
- Janecki, J.M. Cholesterol level in human serum: Seasonal variations and differences in 14 distant regions. Ann. Clin. Lab. Sci. 2013, 43, 407–413. [Google Scholar]
- Zhou, X.; Lin, H.; Zhang, S.; Ren, J.; Wang, Z.; Zhang, Y.; Wang, M.; Zhang, Q. Effects of climatic factors on plasma lipid levels: A 5-year longitudinal study in a large Chinese population. J. Clin. Lipidol. 2016, 10, 1119–1128. [Google Scholar] [CrossRef]
- Shahar, D.R.; Froom, P.; Harari, G.; Yerushalmi, N.; Lubin, F.; Kristal-Boneh, E. Changes in dietary intake account for seasonal changes in cardiovascular disease risk factors. Eur. J. Clin. Nutr. 1999, 53, 395. [Google Scholar] [CrossRef]
- Stelmach-Mardas, M.; Kleiser, C.; Uzhova, I.; Peñalvo, J.; La Torre, G.; Palys, W.; Lojko, D.; Nimptsch, K.; Suwalska, A.; Linseisen, J. Seasonality of food groups and total energy intake: A systematic review and meta-analysis. Eur. J. Clin. Nutr. 2016, 70, 700. [Google Scholar] [CrossRef]
- Ersoy, N.; Tasci, I.; Ozgurtas, T.; Salih, B.; Doruk, H.; Rakicioglu, N. Effect of seasonal changes on nutritional status and biochemical parameters in Turkish older adults. Nutr. Res. Pract. 2018, 12, 315–323. [Google Scholar] [CrossRef] [PubMed]
- Nordestgaard, B.G. A test in context: Lipid profile, fasting versus nonfasting. J. Am. Coll. Cardiol. 2017, 70, 1637–1646. [Google Scholar] [CrossRef] [PubMed]
- Pivarnik, J.M.; Reeves, M.J.; Rafferty, A.P. Seasonal variation in adult leisure-time physical activity. Med. Sci. Sports Exerc. 2003, 35, 1004–1008. [Google Scholar] [CrossRef] [PubMed]
- Uitenbroek, D.G. Seasonal variation in leisure time physical activity. Med. Sci. Sports Exerc. 1993, 25, 755755–755760. [Google Scholar] [CrossRef]
- Adlouni, A.; Ghalim, N.; Benslimane, A.; Lecerf, J.M.; Saile, R. Fasting during Ramadan induces a marked increase in high-density lipoprotein cholesterol and decrease in low-density lipoprotein cholesterol. Ann. Nutr. Metab. 1997, 41, 242–249. [Google Scholar] [CrossRef] [PubMed]
- Schoeller, D.A. The effect of holiday weight gain on body weight. Physiol. Behav. 2014, 134, 66–69. [Google Scholar] [CrossRef]
- Diaz-Zavala, R.G.; Castro-Cantu, M.F.; Valencia, M.E.; Alvarez-Hernandez, G.; Haby, M.M.; Esparza-Romero, J. Effect of the Holiday Season on Weight Gain: A Narrative Review. J. Obes. 2017, 2017, 2085136. [Google Scholar] [CrossRef]
- Hull, H.R.; Radley, D.; Dinger, M.K.; Fields, D.A. The effect of the Thanksgiving holiday on weight gain. Nutr. J. 2006, 5, 29. [Google Scholar] [CrossRef]
- Napierała, M.; Majkowska, L. Ile kalorii zjadamy w Święta Bożego Narodzenia. Diabet. Prakt 2011, 12, B40. [Google Scholar]
- Blazejczyk, K.; Epstein, Y.; Jendritzky, G.; Staiger, H.; Tinz, B. Comparison of UTCI to selected thermal indices. Int. J. Biometeorol. 2012, 56, 515–535. [Google Scholar] [CrossRef] [PubMed]
- Bröde, P.; Fiala, D.; Błażejczyk, K.; Holmér, I.; Jendritzky, G.; Kampmann, B.; Tinz, B.; Havenith, G. Deriving the operational procedure for the Universal Thermal Climate Index (UTCI). Int. J. Biometeorol. 2012, 56, 481–494. [Google Scholar] [CrossRef] [PubMed]
- Fiala, D.; Havenith, G.; Bröde, P.; Kampmann, B.; Jendritzky, G. UTCI-Fiala multi-node model of human heat transfer and temperature regulation. Int. J. Biometeorol. 2012, 56, 429–441. [Google Scholar] [CrossRef] [PubMed]
- Fiala, D.; Lomas, K.J.; Stohrer, M. Computer prediction of human thermoregulatory and temperature responses to a wide range of environmental conditions. Int. J. Biometeorol. 2001, 45, 143–159. [Google Scholar] [CrossRef] [PubMed]
- Błażejczyk, K.; Broede, P.; Fiala, D.; Havenith, G.; Holmér, I.; Jendritzky, G.; Kampmann, B. UTCI–Nowy wskaźnik oceny obciążeń cieplnych człowieka. Prz. Geogr. 2010, 82, 49–71. [Google Scholar]
- Peel, M.C.; Finlayson, B.L.; McMahon, T.A. Updated world map of the Köppen-Geiger climate classification. Hydrol. Earth Syst. Sci. Discuss. 2007, 4, 439–473. [Google Scholar] [CrossRef]
- Haines, P.S.; Hama, M.Y.; Guilkey, D.K.; Popkin, B.M. Weekend eating in the United States is linked with greater energy, fat, and alcohol intake. Obes. Res. 2003, 11, 945–949. [Google Scholar] [CrossRef]
- Kheiri, B.; Abdalla, A.; Osman, M.; Ahmed, S.; Hassan, M.; Bachuwa, G. Vitamin D deficiency and risk of cardiovascular diseases: A narrative review. Clin. Hypertens. 2018, 24, 9. [Google Scholar] [CrossRef]
- Romaszko, J.; Skutecki, R.; Bocheński, M.; Cymes, I.; Dragańska, E.; Jastrzębski, P.; Morocka-Tralle, I.; Jalali, R.; Jeznach-Steinhagen, A.; Glińska-Lewczuk, K. Applicability of the universal thermal climate index for predicting the outbreaks of respiratory tract infections: A mathematical modeling approach. Int. J. Biometeorol. 2019, 63, 1231–1241. [Google Scholar] [CrossRef]
- Sheth, T.; Nair, C.; Muller, J.; Yusuf, S. Increased winter mortality from acute myocardial infarction and stroke: The effect of age. J.Am. Coll. Cardiol. 1999, 33, 1916–1919. [Google Scholar] [CrossRef]
- Skutecki, R.; Jalali, R.; Dragańska, E.; Cymes, I.; Romaszko, J.; Glińska-Lewczuk, K. UTCI as a bio-meteorological tool in the assessment of cold-induced stress as a risk factor for hypertension. Sci. Total Environ. 2019, 688, 970–975. [Google Scholar] [CrossRef] [PubMed]
- Warren-Gash, C.; Smeeth, L.; Hayward, A.C. Influenza as a trigger for acute myocardial infarction or death from cardiovascular disease: A systematic review. Lancet Infect. Dis. 2009, 9, 601–610. [Google Scholar] [CrossRef]
- Pędziwiatr, K. The Catholic Church in Poland on Muslims and Islam. Patterns Prejud. 2018, 52, 461–478. [Google Scholar] [CrossRef]
- De Castro, J.M. Seasonal rhythms of human nutrient intake and meal pattern. Physiol. Behav. 1991, 50, 243–248. [Google Scholar] [CrossRef]
- Shahar, D.; Yerushalmi, N.; Lubin, F.; Froom, P.; Shahar, A.; Kristal-Boneh, E. Seasonal variations in dietary intake affect the consistency of dietary assessment. Eur. J. Epidemiol. 2001, 17, 129–133. [Google Scholar] [CrossRef]
- Heeren, J.; Scheja, L. Brown adipose tissue and lipid metabolism. Curr. Opin. Lipidol. 2018, 29, 180–185. [Google Scholar] [CrossRef]
- Schlein, C.; Heeren, J. Implications of thermogenic adipose tissues for metabolic health. Best Pract. Res. Clin. Endocrinol. Metab. 2016, 30, 487–496. [Google Scholar] [CrossRef]
- Van Ooijen, A.M.; van Marken Lichtenbelt, W.D.; van Steenhoven, A.A.; Westerterp, K.R. Seasonal changes in metabolic and temperature responses to cold air in humans. Physiol. Behav. 2004, 82, 545–553. [Google Scholar] [CrossRef]
- Van der Lans, A.A.; Hoeks, J.; Brans, B.; Vijgen, G.H.; Visser, M.G.; Vosselman, M.J.; Hansen, J.; Jorgensen, J.A.; Wu, J.; Mottaghy, F.M.; et al. Cold acclimation recruits human brown fat and increases nonshivering thermogenesis. J. Clin. Investig. 2013, 123, 3395–3403. [Google Scholar] [CrossRef]
- Bluher, M.; Hentschel, B.; Rassoul, F.; Richter, V. Influence of dietary intake and physical activity on annual rhythm of human blood cholesterol concentrations. Chronobiol. Int. 2001, 18, 541–557. [Google Scholar] [CrossRef]
- Łagowska, K.; Woźniewicz, M.; Jeszka, J. Comparison of eating habits among students according to sex and level of physical activity. Rocz. Panstw. Zakl. Hig. 2011, 62, 335–342. [Google Scholar] [PubMed]
- Castellani, J.W.; Young, A.J. Human physiological responses to cold exposure: Acute responses and acclimatization to prolonged exposure. Auton Neurosci. 2016, 196, 63–74. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Klop, B.; do Rego, A.T.; Cabezas, M.C. Alcohol and plasma triglycerides. Curr. Opin. Lipidol. 2013, 24, 321–326. [Google Scholar] [CrossRef] [PubMed]
- Gupta, R.; Sharma, M.; Goyal, N.K.; Bansal, P.; Lodha, S.; Sharma, K.K. Gender differences in 7 years trends in cholesterol lipoproteins and lipids in India: Insights from a hospital database. Indian J. Endocrinol. Metab. 2016, 20, 211–218. [Google Scholar] [CrossRef] [PubMed]
- NCD Risk Factor Collaboration. National trends in total cholesterol obscure heterogeneous changes in HDL and non-HDL cholesterol and total-to-HDL cholesterol ratio: A pooled analysis of 458 population-based studies in Asian and Western countries. Int. J. Epidemiol. 2019. [Google Scholar] [CrossRef]
- Friedewald, W.T.; Levy, R.I.; Fredrickson, D.S. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin. Chem. 1972, 18, 499–502. [Google Scholar]

| Year | Total (SD; n) | Females (SD; n) | Males (SD; n) |
|---|---|---|---|
| 2016 | 56.84ab (16.32; 26,177) | 58.27ab (16.33; 15,352) | 54.80ab (16.01; 10,825) |
| 2017 | 54.83a (16.32; 39,645) | 55.79a (16.53; 23,027) | 53.50ac (15.92; 16,618) |
| 2018 | 54.65b (16.37; 40,503) | 55.71b (16.56; 24,382) | 53.05bc (15.97; 16,121) |
| Year | TC (mg%) (SD; n) | HDL (mg%) (SD; n) | TG (mg%) (SD; n) |
|---|---|---|---|
| Total | |||
| 2016 | 208.64ab (45.37; 10,986) | 60.77a (18.11; 7256) | 131.09a (91.00; 7935) |
| 2017 | 203.52ac (44.71; 16,262) | 60.75b (17.79; 11,176) | 131.55b (93.62; 12,207) |
| 2018 | 199.16bc (44.82; 16,303) | 61.60ab (18.02; 11,614) | 134.77ab (103.71; 12,586) |
| Males | |||
| 2016 | 205.37de (44.22; 4682) | 52.85 (15.09; 2924) | 147.69c (111.47; 3219) |
| 2017 | 200.18df (45.16; 6858) | 52.91 (14.99; 4665) | 149.79 (121.82; 5095) |
| 2018 | 194.74ef (45.37; 6429) | 53.24 (15.00; 4634) | 154.60c (139.24; 5058) |
| Females | |||
| 2016 | 211.06gh (45.14; 6304) | 66.12c (18.03; 4332) | 119.76 (71.67; 4716) |
| 2017 | 205.96gi (44.22; 9404) | 66.36d (17.52; 6511) | 118.49d (63.29; 7112) |
| 2018 | 202.04hi (44.23; 9874) | 67.16cd (17.70; 6980) | 121.45d (67.20; 7528) |
| Cold Stress (SD; n) | Thermoneutral Conditions (SD; n) | Heat Stress (SD; n) | |
|---|---|---|---|
| Total | |||
| TC | 204.32ab (45.43; 21,803) | 202.47ac (44.58; 17,020) | 200.49bc (45.01; 4728) |
| HDL | 60.89 (27.85; 15,340) | 61.14 (18.18; 11,468) | 61.82 (17.69; 3238) |
| TG | 131.92a (90.14; 16,730) | 132.36b (100.02; 12,468) | 137.42ab (115.88; 3530) |
| Females | |||
| TC | 206.73ab (45.29; 12,593) | 205.20ac (43.89; 10,058) | 203.02bc (43.80; 2931) |
| HDL | 66.55 (17.76; 8896) | 66.49 (17.81; 6930) | 67.36 (17.17; 1997) |
| TG | 119.73 (67.72; 9707) | 120.26 (67.72; 7474) | 119.87 (66.21; 2175) |
| Males | |||
| TC | 201.01ab (45.42; 9210) | 198.53a (45.27; 6962) | 196.37b (46.64; 1797) |
| HDL | 53.08 (14.75; 6444) | 52.97 (15.51; 4538) | 52.91 (14.60; 1241) |
| TG | 148.77a (111.93; 7023) | 150.46b (133.75; 4994) | 165.59ab (163.30; 1355) |
| Before Holidays | After Holidays | Change (%) | p | |
|---|---|---|---|---|
| Males (SD; n) | ||||
| TC | 198.55 (43.74; 461) | 207.6 (46.49; 473) | 4.56 | <0.0023 |
| HDL | 50.49 (14.02; 323) | 54.15 (14.27; 388) | 7.25 | <0.0007 |
| TG | 156.82 (176.56; 353) | 158.58 (105.25; 418) | 1.12 | <0.8644 |
| Females (SD; n) | ||||
| TC | 203.18 (47.19; 504) | 205.18 (41.58; 625) | 0.98 | <0.1803 |
| HDL | 67.75 (18.29; 358) | 66.6 (17.13; 482) | −1.70 | <0.3519 |
| TG | 111.11 (73.55; 390) | 126.07 (110.80; 523) | 13.46 | <0.0210 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Skutecki, R.; Cymes, I.; Dragańska, E.; Glińska-Lewczuk, K.; Buciński, A.; Drozdowski, M.; Romaszko, J. Are the Levels of Lipid Parameters Associated with Biometeorological Conditions? Int. J. Environ. Res. Public Health 2019, 16, 4636. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph16234636
Skutecki R, Cymes I, Dragańska E, Glińska-Lewczuk K, Buciński A, Drozdowski M, Romaszko J. Are the Levels of Lipid Parameters Associated with Biometeorological Conditions? International Journal of Environmental Research and Public Health. 2019; 16(23):4636. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph16234636
Chicago/Turabian StyleSkutecki, Rafał, Iwona Cymes, Ewa Dragańska, Katarzyna Glińska-Lewczuk, Adam Buciński, Marek Drozdowski, and Jerzy Romaszko. 2019. "Are the Levels of Lipid Parameters Associated with Biometeorological Conditions?" International Journal of Environmental Research and Public Health 16, no. 23: 4636. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph16234636