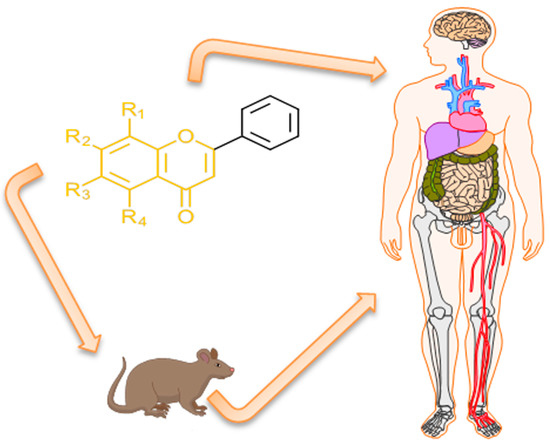
Pharmacokinetics of B-Ring Unsubstituted Flavones
Abstract
:1. Flavones as a Subgroup of Flavonoids
2. B-Ring Unsubstituted Flavones
3. Search Strategy
4. Deglycosilation
5. Absorption
6. Albumin Binding
7. Recycling
8. Distribution
9. Metabolism and Stability to Metabolic Attack
9.1. Glucuronidation
9.2. Sulfation
9.3. Demethylation
9.4. Methylation and Other Biotransformations
10. Excretion
11. Bioavailability
12. Inter-Species Differences
13. Intra-Species Differences (PK Variability)
14. Linearity and PK Parameters
15. Knowledge Gaps and Directions of Future Research
16. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Markham, K.R.; Porter, L.J. Flavonoids in the green algae (chlorophyta). Phytochemistry 1969, 8, 1777–1781. [Google Scholar] [CrossRef]
- Ben Saad, H.; Gargouri, M.; Kallel, F.; Chaabene, R.; Boudawara, T.; Jamoussi, K.; Magné, C.; Mounir Zeghal, K.; Hakim, A.; Ben Amara, I. Flavonoid compounds from the red marine alga Alsidium corallinum protect against potassium bromate-induced nephrotoxicity in adult mice: Alsidium corallinum protect against KBrO3-induced nephrotoxicity. Environ. Toxicol. 2017, 32, 1475–1486. [Google Scholar] [CrossRef] [PubMed]
- Saito, K.; Yonekura-Sakakibara, K.; Nakabayashi, R.; Higashi, Y.; Yamazaki, M.; Tohge, T.; Fernie, A.R. The flavonoid biosynthetic pathway in Arabidopsis: Structural and genetic diversity. Plant Physiol. Biochem. 2013, 72, 21–34. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Martens, S.; Mithöfer, A. Flavones and flavone synthases. Phytochemistry 2005, 66, 2399–2407. [Google Scholar] [CrossRef] [PubMed]
- Tohge, T.; de Souza, L.P.; Fernie, A.R. Current understanding of the pathways of flavonoid biosynthesis in model and crop plants. J. Exp. Bot. 2017, 68, 4013–4028. [Google Scholar] [CrossRef] [PubMed]
- Wang, T.; Li, Q.; Bi, K. Bioactive flavonoids in medicinal plants: Structure, activity and biological fate. Asian J. Pharm. Sci. 2018, 13, 12–23. [Google Scholar] [CrossRef]
- Harrison, P.G.; Bailey, B.K.; Steck, W. Biosynthesis of Furanochromones. Can. J. Biochem. 1971, 49, 964–970. [Google Scholar] [CrossRef]
- Hostetler, G.L.; Ralston, R.A.; Schwartz, S.J. Flavones: Food Sources, Bioavailability, Metabolism, and Bioactivity. Adv. Nutr. Int. Rev. J. 2017, 8, 423–435. [Google Scholar] [CrossRef] [Green Version]
- Berim, A.; Gang, D.R. Methoxylated flavones: Occurrence, importance, biosynthesis. Phytochem. Rev. 2016, 15, 363–390. [Google Scholar] [CrossRef]
- Lin, C.H.; Chang, C.Y.; Lee, K.R.; Lin, H.J.; Chen, T.H.; Wan, L. Flavones inhibit breast cancer proliferation through the Akt/FOXO3a signaling pathway. BMC Cancer 2015, 15, 958. [Google Scholar] [CrossRef]
- Arai, Y.; Watanabe, S.; Kimira, M.; Shimoi, K.; Mochizuki, R.; Kinae, N. Dietary Intakes of Flavonols, Flavones and Isoflavones by Japanese Women and the Inverse Correlation between Quercetin Intake and Plasma LDL Cholesterol Concentration. J. Nutr. 2000, 130, 2243–2250. [Google Scholar] [CrossRef] [Green Version]
- Herath, W.; Mikell, J.R.; Hale, A.L.; Ferreira, D.; Khan, I.A. Microbial metabolism. Part 6. Metabolites of 3-and 7-hydroxyflavones. Chem. Pharm. Bull. 2006, 54, 320–324. [Google Scholar] [CrossRef]
- Valant-Vetschera, K.M.; Wollenweber, E. Flavones and Flavonols. In Flavonoids Chemistry, Biochemistry and Applications; CRC Press/Taylor & Francis: Boca Raton, FL, USA, 2006; pp. 618–748. ISBN 978-0-8493-2021-7. [Google Scholar]
- Mani, R.; Natesan, V. Chrysin: Sources, beneficial pharmacological activities, and molecular mechanism of action. Phytochemistry 2018, 145, 187–196. [Google Scholar] [CrossRef]
- Wen, Q.; Li, H.L.; Mai, S.Y.; Tan, Y.F.; Chen, F. Tissue Distribution of Active Principles from Alpiniae Oxyphyllae Fructus Extract: An Experimental Study in Rats. Curr. Pharm. Anal. 2019, 15, 286–293. [Google Scholar] [CrossRef]
- Zhang, B.; Dong, Y.; Yu, N.; Sun, Y.; Xing, Y.; Yang, F.; Yu, X.; Sun, W.; Sun, J.; Li, X.; et al. Intestinal metabolism of baicalein after oral administration in mice: Pharmacokinetics and mechanisms. J. Funct. Foods 2019, 54, 53–63. [Google Scholar] [CrossRef]
- Tai, M.C.; Tsang, S.Y.; Chang, L.Y.F.; Xue, H. Therapeutic potential of wogonin: A naturally occurring flavonoid. CNS Drug Rev. 2005, 11, 141–150. [Google Scholar] [CrossRef]
- Wei, H.L.; Zhou, S.X.; Jiang, Y.; Song, Y.L.; Li, J.; Tu, P.F. Chemical constituents from leaves of Evodia lepta. China J. Chin. Mater. Med. 2013, 38, 1193–1197. [Google Scholar]
- Cao, X.D.; Ding, Z.S.; Jiang, F.S.; Ding, X.H.; Chen, J.Z.; Chen, S.H.; Lv, G.Y. Antitumor constituents from the leaves of Carya cathayensis. Nat. Prod. Res. 2012, 26, 2089–2094. [Google Scholar]
- Lu, L.; Guo, Q.; Zhao, L. Overview of Oroxylin A: A Promising Flavonoid Compound. Phytother. Res. PTR 2016, 30, 1765–1774. [Google Scholar] [CrossRef]
- Xing, H.; Kong, D.; Ning, C.; Kong, Y.; Ren, C.; Cheng, Y.; Cai, H.; Wang, J.; Zhao, D.; Li, N.; et al. An Investigation on Glucuronidation Metabolite Identification, Isozyme Contribution, and Species Differences of GL-V9 In Vitro and In Vivo. Molecules 2019, 24, 1576. [Google Scholar] [CrossRef]
- Ha, L.; Qian, Y.; Zhang, S.; Ju, X.; Sun, S.; Guo, H.; Wang, Q.; Li, K.; Fan, Q.; Zheng, Y.; et al. Synthesis and Biological Evaluation of Scutellaria Flavone Cyclaneaminol Mannich Base Derivatives as Novel CDK1 Inhibitors. Anticancer Agents Med. Chem. 2016, 16, 914–924. [Google Scholar] [CrossRef]
- Han, X.H.; Zhong, J.; Guo, J.Y.; Shi, R.; Wang, X.H.; Wang, C.H.; Wang, K.; Du, G.L.; Shen, Y.H.; Ma, Y.M. Relationships between pharmacokinetics and efficacy of Xie-xin decoction in rats with experimental ulcerative colitis. J. Ethnopharmacol. 2013, 148, 182–189. [Google Scholar] [CrossRef]
- Németh, K.; Plumb, G.W.; Berrin, J.G.; Juge, N.; Jacob, R.; Naim, H.Y.; Williamson, G.; Swallow, D.M.; Kroon, P.A. Deglycosylation by small intestinal epithelial cell beta-glucosidases is a critical step in the absorption and metabolism of dietary flavonoid glycosides in humans. Eur. J. Nutr. 2003, 42, 29–42. [Google Scholar] [CrossRef]
- Wang, J.; Pang, Q.; Cen, W.; Zhu, P.; Xu, Y. Simultaneous determination of ten active constituents of Yankening Capsule in rat plasma by ultra high performance liquid chromatography with tandem mass spectrometry. J. Chromatogr. B Anal. Technol. Biomed. Life Sci. 2015, 978–979, 43–53. [Google Scholar] [CrossRef]
- Li, C.; Homma, M.; Oka, K. Characteristics of delayed excretion of flavonoids in human urine after administration of Shosaiko-to, a herbal medicine. Biol. Pharm. Bull. 1998, 21, 1251–1257. [Google Scholar] [CrossRef]
- Akao, T.; Kawabata, K.; Yanagisawa, E.; Ishihara, K.; Mizuhara, Y.; Wakui, Y.; Sakashita, Y.; Kobashi, K. Baicalin, the predominant flavone glucuronide of scutellariae radix, is absorbed from the rat gastrointestinal tract as the aglycone and restored to its original form. J. Pharm. Pharmacol. 2000, 52, 1563–1568. [Google Scholar] [CrossRef]
- Sakurama, H.; Kishino, S.; Uchibori, Y.; Yonejima, Y.; Ashida, H.; Kita, K.; Takahashi, S.; Ogawa, J. β-Glucuronidase from Lactobacillus brevis useful for baicalin hydrolysis belongs to glycoside hydrolase family 30. Appl. Microbiol. Biotechnol. 2014, 98, 4021–4032. [Google Scholar] [CrossRef]
- Zhang, R.; Cui, Y.; Wang, Y.; Tian, X.; Zheng, L.; Cong, H.; Wu, B.; Huo, X.; Wang, C.; Zhang, B.; et al. Catechol-O-Methyltransferase and UDP-Glucuronosyltransferases in the Metabolism of Baicalein in Different Species. Eur. J. Drug Metab. Pharmacokinet. 2017, 42, 981–992. [Google Scholar] [CrossRef]
- Xing, J.; Chen, X.; Sun, Y.; Luan, Y.; Zhong, D. Interaction of baicalin and baicalein with antibiotics in the gastrointestinal tract. J. Pharm. Pharmacol. 2005, 57, 743–750. [Google Scholar] [CrossRef]
- Akao, T.; Sakashita, Y.; Hanada, M.; Goto, H.; Shimada, Y.; Terasawa, K. Enteric excretion of baicalein, a flavone of Scutellariae Radix, via glucuronidation in rat: Involvement of multidrug resistance-associated protein 2. Pharm. Res. 2004, 21, 2120–2126. [Google Scholar] [CrossRef]
- Cai, Y.; Li, S.; Li, T.; Zhou, R.; Wai, A.T.S.; Yan, R. Oral pharmacokinetics of baicalin, wogonoside, oroxylin A 7-O-β-d-glucuronide and their aglycones from an aqueous extract of Scutellariae Radix in the rat. J. Chromatogr. B Anal. Technol. Biomed. Life Sci. 2016, 1026, 124–133. [Google Scholar] [CrossRef]
- Kalapos-Kovács, B.; Magda, B.; Jani, M.; Fekete, Z.; Szabó, P.T.; Antal, I.; Krajcsi, P.; Klebovich, I. Multiple ABC Transporters Efflux Baicalin. Phytother. Res. PTR 2015, 29, 1987–1990. [Google Scholar] [CrossRef]
- Noh, K.; Kang, Y.; Nepal, M.R.; Jeong, K.S.; Oh, D.G.; Kang, M.J.; Lee, S.; Kang, W.; Jeong, H.G.; Jeong, T.C. Role of Intestinal Microbiota in Baicalin-Induced Drug Interaction and Its Pharmacokinetics. Molecules 2016, 21, 337. [Google Scholar] [CrossRef]
- Wang, Q.; Shi, R.; Dai, Y.; Li, Y.; Wang, T.; Ma, Y.; Cheng, N. Mechanism in the existent difference in form of wogonin/wogonoside between plasma and intestine/liver in rats. RSC Adv. 2018, 8, 3364–3373. [Google Scholar] [CrossRef] [Green Version]
- Zuo, F.; Zhou, Z.M.; Yan, M.Z.; Liu, M.L.; Xiong, Y.L.; Zhang, Q.; Song, H.Y.; Ye, W.H. Metabolism of constituents in Huangqin-Tang, a prescription in traditional Chinese medicine, by human intestinal flora. Biol. Pharm. Bull. 2002, 25, 558–563. [Google Scholar] [CrossRef]
- Xing, S.; Wang, M.; Peng, Y.; Chen, D.; Li, X. Simulated gastrointestinal tract metabolism and pharmacological activities of water extract of Scutellaria baicalensis roots. J. Ethnopharmacol. 2014, 152, 183–189. [Google Scholar] [CrossRef]
- Dai, J.; Yang, J.; Li, C. Transport and metabolism of flavonoids from Chinese herbal remedy Xiaochaihu-tang across human intestinal Caco-2 cell monolayers. Acta Pharmacol. Sin. 2008, 29, 1086–1093. [Google Scholar] [CrossRef]
- Du, L.Y.; Guo, J.M.; Qian, D.W.; Shang, E.X.; Jiang, S.; Liu, P.; Su, S.L.; Zhang, F.; Duan, J.A.; Xu, J.; et al. Simultaneous determination of seven active ingredients in rat plasma by UPLC-MS/MS and application in pharmacokinetic studies after oral administration of scutellaria-coptis herb couple. Med. Chem. Res. 2015, 24, 1289–1297. [Google Scholar] [CrossRef]
- Sun, R.; Zeng, M.; Du, T.; Li, L.; Yang, G.; Hu, M.; Gao, S. Simultaneous determinations of 17 marker compounds in Xiao–Chai–Hu–Tang by LC–MS/MS: Application to its pharmacokinetic studies in mice. J. Chromatogr. B 2015, 1003, 12–21. [Google Scholar] [CrossRef]
- Tao, J.H.; Xu, J.; Jiang, S.; Ling, Y.; Wang, D.G. Simultaneous determination of the bioactive components in rat plasma by UPLC-MS/MS and application in pharmacokinetic studies after oral administration of radix Scutellariae extract. Biomed. Chromatogr. BMC 2017, 31. [Google Scholar] [CrossRef]
- Du, K.; Wu, C.; Ding, C.; Zhao, S.; Qin, H.; Zhang, J. Simultaneous LC–MS Analysis and of Wogonin and Oroxylin A in Rat Plasma, and Pharmacokinetic Studies After Administration of the Active Fraction from Xiao-Xu-Ming Decoction. Chromatographia 2009, 69, 1259–1266. [Google Scholar] [CrossRef]
- Rastogi, H.; Jana, S. Evaluation of physicochemical properties and intestinal permeability of six dietary polyphenols in human intestinal colon adenocarcinoma Caco-2 cells. Eur. J. Drug Metab. Pharmacokinet. 2016, 41, 33–43. [Google Scholar] [CrossRef]
- Zhu, M.L.; Liang, X.L.; Zhao, L.J.; Liao, Z.G.; Zhao, G.W.; Cao, Y.C.; Zhang, J.; Luo, Y. Elucidation of the transport mechanism of baicalin and the influence of a Radix Angelicae Dahuricae extract on the absorption of baicalin in a Caco-2 cell monolayer model. J. Ethnopharmacol. 2013, 150, 553–559. [Google Scholar] [CrossRef]
- Zhang, L.; Lin, G.; Kovács, B.; Jani, M.; Krajcsi, P.; Zuo, Z. Mechanistic study on the intestinal absorption and disposition of baicalein. Eur. J. Pharm. Sci. 2007, 31, 221–231. [Google Scholar] [CrossRef]
- Li, C.; Zhang, L.; Zhou, L.; Wo, S.K.; Lin, G.; Zuo, Z. Comparison of intestinal absorption and disposition of structurally similar bioactive flavones in Radix Scutellariae. AAPS J. 2012, 14, 23–34. [Google Scholar] [CrossRef]
- Akao, T.; Sato, K.; Hanada, M. Hepatic contribution to a marked increase in the plasma concentration of baicalin after oral administration of its aglycone, baicalein, in multidrug resistance-associated protein 2-deficient rat. Biol. Pharm. Bull. 2009, 32, 2079–2082. [Google Scholar] [CrossRef]
- Akao, T.; Hanada, M.; Sakashita, Y.; Sato, K.; Morita, M.; Imanaka, T. Efflux of baicalin, a flavone glucuronide of Scutellariae Radix, on Caco-2 cells through multidrug resistance-associated protein 2. J. Pharm. Pharmacol. 2007, 59, 87–93. [Google Scholar] [CrossRef]
- Taiming, L.; Xuehua, J. Investigation of the absorption mechanisms of baicalin and baicalein in rats. J. Pharm. Sci. 2006, 95, 1326–1333. [Google Scholar] [CrossRef]
- Lu, T.; Song, J.; Huang, F.; Deng, Y.; Xie, L.; Wang, G.; Liu, X. Comparative pharmacokinetics of baicalin after oral administration of pure baicalin, Radix scutellariae extract and Huang-Lian-Jie-Du-Tang to rats. J. Ethnopharmacol. 2007, 110, 412–418. [Google Scholar] [CrossRef]
- Xing, H.; Ren, C.; Kong, Y.; Ning, C.; Kong, D.; Zhang, Y.; Zhao, D.; Li, N.; Wang, Z.; Chen, X.; et al. Mechanistic study of absorption and first-pass metabolism of GL-V9, a derivative of wogonin. Biopharm. Drug Dispos. 2019, 40, 151–161. [Google Scholar] [CrossRef]
- Sekiya, K.; Kadota, S.; Katayama, K.; Koizumi, T.; Namba, T. Study on baths with crude drug. III. The effect of ligustici chuanxiong rhizoma extract on the percutaneous absorption of some natural compounds. Biol. Pharm. Bull. 1997, 20, 983–987. [Google Scholar] [CrossRef]
- Zhang, Y.; Zhang, K.; Guo, T.; Li, Y.; Zhu, C.; Feng, N. Transdermal baicalin delivery using diethylene glycol monoethyl ether-mediated cubic phase gel. Int. J. Pharm. 2015, 479, 219–226. [Google Scholar] [CrossRef]
- Wang, G.; Li, R.; Zhang, X. Pharmacokinetics of Two Ingredients of the Compound Chinese Herbal Medicine Transdermal Preparation in Cows. Agric. Sci. China 2009, 8, 1138–1142. [Google Scholar] [CrossRef]
- Li, C.; Liu, S.; Luo, G.; Wang, G.; Zhang, B.; Nie, Q. Comparison of plasma pharmacokinetics of Tanreqing solution between intratracheal aerosolization and intravenous injection in rats. Biomed. Chromatogr. BMC 2018, 32. [Google Scholar] [CrossRef]
- Zhang, J.; Lv, H.; Jiang, K.; Gao, Y. Enhanced bioavailability after oral and pulmonary administration of baicalein nanocrystal. Int. J. Pharm. 2011, 420, 180–188. [Google Scholar] [CrossRef] [PubMed]
- Wei, Y.; Liang, J.; Zheng, X.; Pi, C.; Liu, H.; Yang, H.; Zou, Y.; Ye, Y.; Zhao, L. Lung-targeting drug delivery system of baicalin-loaded nanoliposomes: Development, biodistribution in rabbits, and pharmacodynamics in nude mice bearing orthotopic human lung cancer. Int. J. Nanomed. 2016, 12, 251–261. [Google Scholar] [CrossRef]
- Wei, Y.; Pi, C.; Yang, G.; Xiong, X.; Lan, Y.; Yang, H.; Zhou, Y.; Ye, Y.; Zou, Y.; Zheng, W.; et al. LC-UV Determination of Baicalin in Rabbit Plasma and Tissues for Application in Pharmacokinetics and Tissue Distribution Studies of Baicalin after Intravenous Administration of Liposomal and Injectable Formulations. Molecules 2016, 21, 444. [Google Scholar] [CrossRef]
- Ye, J.X.; Wei, W.; Quan, L.H.; Liu, C.Y.; Chang, Q.; Liao, Y.H. An LC–MS/MS method for the simultaneous determination of chlorogenic acid, forsythiaside A and baicalin in rat plasma and its application to pharmacokinetic study of Shuang-huang-lian in rats. J. Pharm. Biomed. Anal. 2010, 52, 625–630. [Google Scholar] [CrossRef]
- Xing, H.; Ren, C.; Kong, Y.; Ni, Q.; Wang, Z.; Zhao, D.; Li, N.; Chen, X.; Lu, Y. Determination of GL-V9, a derivative of wogonin, in rat plasma by UPLC-MS/MS and its application to a pharmacokinetic study after oral and pulmonary administration. Biomed. Chromatogr. 2019, 33, e4556. [Google Scholar] [CrossRef]
- Zhang, L.; Zhang, J.; Wang, L.; Xia, H. Ocular pharmacokinetics and availability of topically applied baicalein in rabbits. Curr. Eye Res. 2009, 34, 257–263. [Google Scholar] [CrossRef]
- Ashraf, O.; Nasr, M.; Nebsen, M.; Said, A.M.A.; Sammour, O. In vitro stabilization and in vivo improvement of ocular pharmacokinetics of the multi-therapeutic agent baicalin: Delineating the most suitable vesicular systems. Int. J. Pharm. 2018, 539, 83–94. [Google Scholar] [CrossRef]
- Liu, Z.; Zhang, X.; Wu, H.; Li, J.; Shu, L.; Liu, R.; Li, L.; Li, N. Preparation and evaluation of solid lipid nanoparticles of baicalin for ocular drug delivery system in vitro and in vivo. Drug Dev. Ind. Pharm. 2011, 37, 475–481. [Google Scholar] [CrossRef]
- Liu, Z.; Zhang, X.; Li, J.; Liu, R.; Shu, L.; Jin, J. Effects of Labrasol on the corneal drug delivery of baicalin. Drug Deliv. 2009, 16, 399–404. [Google Scholar] [CrossRef]
- Xiao, J.; Cao, H.; Wang, Y.; Yamamoto, K.; Wei, X. Structure-affinity relationship of flavones on binding to serum albumins: Effect of hydroxyl groups on ring A. Mol. Nutr. Food Res. 2010, 54, S253–S260. [Google Scholar] [CrossRef]
- Jiang, B.; Zhao, A.; Miao, J.; Chang, P.; Chen, H.; Pan, W.; Lin, C. Molecular docking and reaction kinetic studies of chrysin binding to serum albumin. Nat. Prod. Commun. 2014, 9, 195–200. [Google Scholar] [CrossRef]
- Wang, J.; Wang, Q.; Wu, D.; Yan, J.; Wu, Y.; Li, H. Comparative studies on the interactions of baicalein and Al(III)-baicalein complex with human serum albumin. Luminescence 2016, 31, 54–62. [Google Scholar] [CrossRef]
- Tian, J.; Liu, J.; Hu, Z.; Chen, X. Interaction of wogonin with bovine serum albumin. Bioorg. Med. Chem. 2005, 13, 4124–4129. [Google Scholar] [CrossRef]
- Tian, J.; Liu, J.; Xie, J.; Yao, X.; Hu, Z.; Chen, X. Binding of wogonin to human serum albumin: A common binding site of wogonin in subdomain IIA. J. Photochem. Photobiol. B 2004, 74, 39–45. [Google Scholar] [CrossRef]
- Ma, J.; Liu, Y.; Chen, L.; Xie, Y.; Wang, L.Y.; Xie, M.X. Spectroscopic investigation on the interaction of 3,7-dihydroxyflavone with different isomers of human serum albumin. Food Chem. 2012, 132, 663–670. [Google Scholar] [CrossRef]
- Mohos, V.; Fliszár-Nyúl, E.; Schilli, G.; Hetényi, C.; Lemli, B.; Kunsági-Máté, S.; Bognár, B.; Poór, M. Interaction of Chrysin and Its Main Conjugated Metabolites Chrysin-7-Sulfate and Chrysin-7-Glucuronide with Serum Albumin. Int. J. Mol. Sci. 2018, 19, 4073. [Google Scholar] [CrossRef]
- Liu, H.; Bao, W.; Ding, H.; Jang, J.; Zou, G. Binding modes of flavones to human serum albumin: Insights from experimental and computational studies. J. Phys. Chem. B 2010, 114, 12938–12947. [Google Scholar] [CrossRef]
- Tang, Y.; Zhu, H.; Zhang, Y.; Huang, C. Determination of human plasma protein binding of baicalin by ultrafiltration and high-performance liquid chromatography. Biomed. Chromatogr. BMC 2006, 20, 1116–1119. [Google Scholar] [CrossRef]
- Talbi, A.; Zhao, D.; Liu, Q.; Li, J.; Fan, A.; Yang, W.; Han, X.; Chen, X. Pharmacokinetics, tissue distribution, excretion and plasma protein binding studies of wogonin in rats. Molecules 2014, 19, 5538–5549. [Google Scholar] [CrossRef]
- Xiao, J.; Cao, H.; Wang, Y.; Zhao, J.; Wei, X. Glycosylation of dietary flavonoids decreases the affinities for plasma protein. J. Agric. Food Chem. 2009, 57, 6642–6648. [Google Scholar] [CrossRef]
- Xia, B.; Zhou, Q.; Zheng, Z.; Ye, L.; Hu, M.; Liu, Z. A novel local recycling mechanism that enhances enteric bioavailability of flavonoids and prolongs their residence time in the gut. Mol. Pharm. 2012, 9, 3246–3258. [Google Scholar] [CrossRef]
- Dai, P.; Zhu, L.; Luo, F.; Lu, L.; Li, Q.; Wang, L.; Wang, Y.; Wang, X.; Hu, M.; Liu, Z. Triple Recycling Processes Impact Systemic and Local Bioavailability of Orally Administered Flavonoids. AAPS J. 2015, 17, 723–736. [Google Scholar] [CrossRef] [Green Version]
- Liu, Y.; Liu, Y.; Dai, Y.; Xun, L.; Hu, M. Enteric disposition and recycling of flavonoids and ginkgo flavonoids. J. Altern. Complement. Med. 2003, 9, 631–640. [Google Scholar] [CrossRef]
- Wang, L.; Sun, R.; Zhang, Q.; Luo, Q.; Zeng, S.; Li, X.; Gong, X.; Li, Y.; Lu, L.; Hu, M.; et al. An update on polyphenol disposition via coupled metabolic pathways. Expert Opin. Drug Metab. Toxicol. 2019, 15, 151–165. [Google Scholar] [CrossRef]
- Liu, S.; Zheng, H.; Sun, R.; Jiang, H.; Chen, J.; Yu, J.; Zhang, Q.; Chen, Q.; Zhu, L.; Hu, M.; et al. Disposition of Flavonoids for Personal Intake. Curr. Pharmacol. Rep. 2017, 3, 196–212. [Google Scholar] [CrossRef]
- Xing, J.; Chen, X.; Zhong, D. Absorption and enterohepatic circulation of baicalin in rats. Life Sci. 2005, 78, 140–146. [Google Scholar] [CrossRef]
- Zeng, M.; Sun, R.; Basu, S.; Ma, Y.; Ge, S.; Yin, T.; Gao, S.; Zhang, J.; Hu, M. Disposition of flavonoids via recycling: Direct biliary excretion of enterically or extrahepatically derived flavonoid glucuronides. Mol. Nutr. Food Res. 2016, 60, 1006–1019. [Google Scholar] [CrossRef]
- Li, M.; Shi, A.; Pang, H.; Xue, W.; Li, Y.; Cao, G.; Yan, B.; Dong, F.; Li, K.; Xiao, W.; et al. Safety, tolerability, and pharmacokinetics of a single ascending dose of baicalein chewable tablets in healthy subjects. J. Ethnopharmacol. 2014, 156, 210–215. [Google Scholar] [CrossRef]
- Morisaki, T.; Hou, X.L.; Takahashi, K.; Takahashi, K. Baicalin pharmacokinetic profile of absorption process using novel in-vitro model: Cytochrome P450 3A4-induced Caco-2 cell monolayers combined with rat intestinal rinse fluids. J. Pharm. Pharmacol. 2013, 65, 1526–1535. [Google Scholar] [CrossRef]
- Wang, Y.; Zhang, Y.; Xiao, J.; Xu, R.; Wang, Q.; Wang, X. Simultaneous determination of baicalin, baicalein, wogonoside, wogonin, scutellarin, berberine, coptisine, ginsenoside Rb1 and ginsenoside Re of Banxia xiexin decoction in rat plasma by LC-MS/MS and its application to a pharmacokinetic study. Biomed. Chromatogr. BMC 2018, 32. [Google Scholar] [CrossRef]
- Zan, B.; Shi, R.; Wang, T.; Wu, J.; Ma, Y.; Cheng, N. Simultaneous quantification of multiple active components from Xiexin decoction in rat plasma by LC-ESI-MS/MS: Application in pharmacokinetics. Biomed. Chromatogr. BMC 2011, 25, 816–826. [Google Scholar] [CrossRef]
- Tong, L.; Wan, M.; Zhang, L.; Zhu, Y.; Sun, H.; Bi, K. Simultaneous determination of baicalin, wogonoside, baicalein, wogonin, oroxylin A and chrysin of Radix scutellariae extract in rat plasma by liquid chromatography tandem mass spectrometry. J. Pharm. Biomed. Anal. 2012, 70, 6–12. [Google Scholar] [CrossRef]
- Zhang, J.; Zhang, S.; Teng, S.; Zhai, L. An LC-MS/MS method for simultaneous determination of four flavonoids from Semen Oroxyli in rat plasma and its application to a pharmacokinetic study. J. Chromatogr. B Anal. Technol. Biomed. Life Sci. 2016, 1020, 96–102. [Google Scholar] [CrossRef]
- Wen, Q.; Li, H.L.; Tan, Y.F.; Zhang, X.G.; Qin, Z.M.; Li, W.; Li, Y.H.; Zhang, J.Q.; Chen, F. LC-MS/MS-based method for simultaneous quantification of known chemicals and metabolites of Alpiniae oxyphyllae Fructus extract in rat plasma and its application in a pharmacokinetic study. Anal. Methods 2016, 8, 2069–2081. [Google Scholar] [CrossRef]
- Wang, Z.; An, R.; Du, G.; Liang, K.; Li, G. Validation of an LC–MS/MS method for simultaneous detection of diverse components of Qinxing Qingre Zhike Granule in rat plasma and its application to pharmacokinetic study after oral administration to rats. Biomed. Chromatogr. 2019, 33, e4524. [Google Scholar] [CrossRef]
- Wang, J.; Zheng, D.; Wang, Y.; Zhang, C.; Sun, X. Pharmacokinetics study of Erhuang decoction extracts in rats by HPLC-MS/MS. J. Chromatogr. B Anal. Technol. Biomed. Life Sci. 2017, 1059, 35–42. [Google Scholar] [CrossRef]
- Bo, Y.; Wang, L.; Wu, X.; Zhao, L.; Yang, J.; Xiong, Z.; Wu, C. Development and validation of a UHPLC-MS/MS method for the simultaneous determination of five bioactive flavonoids in rat plasma and comparative pharmacokinetic study after oral administration of Xiaochaihu Tang and three compatibilities. J. Sep. Sci. 2017, 40, 1896–1905. [Google Scholar] [CrossRef]
- Fu, Z.; Di, Y.; Gao, L.; Wu, J.; Shi, M.; Zheng, F. The drug metabolism and pharmacokinetics investigation about baicalin effect and baicalein on mice U14 cervical cancer. J. Spectrosc. 2015, 2015, 632062. [Google Scholar] [CrossRef]
- Li, T.; Feng, Z.; Yao, M.; Liao, Q.; Zhao, Z.; Zhang, L. Comparative pharmacokinetic and tissue distribution study of baicalin, baicalein, wogonoside, wogonin and oroxylin-A after oral administration of Component compatibility of SHT and total flavonoids fractions of Radix scutellariae to rats. Anal. Methods 2014, 6, 5799–5807. [Google Scholar] [CrossRef]
- Zhu, H.; Qian, Z.; Li, H.; Guo, L.; Pan, L.; Zhang, Q.; Tang, Y. Integrated pharmacokinetics of major bioactive components in MCAO rats after oral administration of Huang-Lian-Jie-Du-Tang. J. Ethnopharmacol. 2012, 141, 158–169. [Google Scholar] [CrossRef]
- Chung, H.J.; Lim, S.Y.; Kim, I.S.; Bu, Y.M.; Kim, H.C.; Kim, D.H.; Yoo, H.H. Simultaneous Determination of Baicalein, Baicalin, Wogonin, and Wogonoside in Rat Plasma by LC-MS/MS for Studying the Pharmacokinetics of the Standardized Extract of Scutellariae Radix. Bull. Korean Chem. Soc. 2012, 33, 177–182. [Google Scholar] [CrossRef] [Green Version]
- Yan, J.; Liu, Z.; Wang, T.; Shi, R.; Ma, Y. Pharmacokinetics of flavonoids from xiexin decoction in rats. Yao Xue Xue Bao 2007, 42, 722–729. [Google Scholar]
- Kim, Y.H.; Jeong, D.W.; Paek, I.B.; Ji, H.Y.; Kim, Y.C.; Sohn, D.H.; Lee, H.S. Liquid chromatography with tandem mass spectrometry for the simultaneous determination of baicalein, baicalin, oroxylin A and wogonin in rat plasma. J. Chromatogr. B Anal. Technol. Biomed. Life Sci. 2006, 844, 261–267. [Google Scholar] [CrossRef]
- Zhang, Y.; Yuan, J.; Zhang, Y.; Chen, Y.; Cao, J.; An, R.; Wang, X. LC-MS/MS analysis of Gegen Qinlian Decoction and its pharmacokinetics after oral administration to rats: LC-MS/MS analysis of Gegen Qinlian Decoction and its pharmacokinetics. Biomed. Chromatogr. 2015, 29, 485–495. [Google Scholar] [CrossRef]
- Zhao, L.; Qian, X.; Li, W.; Lv, L.; Zhang, H.; Chai, Y.; Zhang, G. An LC-MS/MS method for the simultaneous determination and pharmacokinetic studies of bergenin, chlorogenic acid and four flavonoids in rat plasma after oral administration of a QingGanSanJie decotion extract. Biomed. Chromatogr. BMC 2014, 28, 1670–1678. [Google Scholar] [CrossRef]
- Zeng, L.; Wang, M.; Yuan, Y.; Guo, B.; Zhou, J.; Tan, Z.; Ye, M.; Ding, L.; Chen, B. Simultaneous multi-component quantitation of Chinese herbal injection Yin-zhi-huang in rat plasma by using a single-tube extraction procedure for mass spectrometry-based pharmacokinetic measurement. J. Chromatogr. B 2014, 967, 245–254. [Google Scholar] [CrossRef]
- Xu, B.; Li, P.; Zhang, G. Comparative pharmacokinetics of puerarin, daidzin, baicalin, glycyrrhizic acid, liquiritin, berberine, palmatine and jateorhizine by liquid chromatography-mass spectrometry after oral administration of Gegenqinlian decoction and active components alignment (ACA) to rats. J. Chromatogr. B 2015, 988, 33–44. [Google Scholar]
- Huang, P.; Gao, J.; Shi, Z.; Zou, J.; Lu, Y.; Yuan, Y.; Yao, M. A novel UPLC-MS/MS method for simultaneous quantification of rhein, emodin, berberine and baicalin in rat plasma and its application in a pharmacokinetic study. Bioanalysis 2012, 4, 1205–1213. [Google Scholar] [CrossRef]
- Wang, Y.; Yao, Y.; An, R.; You, L.; Wang, X. Simultaneous determination of puerarin, daidzein, baicalin, wogonoside and liquiritin of GegenQinlian decoction in rat plasma by ultra-performance liquid chromatography-mass spectrometry. J. Chromatogr. B 2009, 877, 1820–1826. [Google Scholar] [CrossRef]
- Deng, Y.X.; Lu, T.; Xie, L.; Liu, X.D. High-performance liquid chromatographic method for the determination and pharmacokinetic study of wogonoside in rat serum after oral administration of traditional Chinese medicinal preparation Huang-Lian-Jie-Du decoction. Biomed. Chromatogr. 2006, 20, 1098–1102. [Google Scholar] [CrossRef]
- Huang, T.; Xiong, Y.; Chen, N.; Wang, D.; Lai, Y.; Deng, C. Highly selective enrichment of baicalin in rat plasma by boronic acid-functionalized core-shell magnetic microspheres: Validation and application to a pharmacokinetic study. Talanta 2016, 147, 501–509. [Google Scholar] [CrossRef]
- Lu, C.M.; Lin, L.C.; Tsai, T.H. Determination and Pharmacokinetic Study of Gentiopicroside, Geniposide, Baicalin, and Swertiamarin in Chinese Herbal Formulae after Oral Administration in Rats by LC-MS/MS. Molecules 2014, 19, 21560–21578. [Google Scholar] [CrossRef] [Green Version]
- Gao, R.; Zheng, Q.; Gong, T.; Fu, Y.; Deng, L.; Zhang, Z.R. Gradient high-performance liquid chromatography for the simultaneous determination of chlorogenic acid and baicalin in plasma and its application in the study of pharmacokinetics in rats. J. Pharm. Biomed. Anal. 2007, 43, 335–340. [Google Scholar] [CrossRef]
- Feng, J.; Xu, W.; Tao, X.; Wei, H.; Cai, F.; Jiang, B.; Chen, W. Simultaneous determination of baicalin, baicalein, wogonin, berberine, palmatine and jatrorrhizine in rat plasma by liquid chromatography-tandem mass spectrometry and application in pharmacokinetic studies after oral administration of traditional Chinese medicinal preparations containing scutellaria-coptis herb couple. J. Pharm. Biomed. Anal. 2010, 53, 591–598. [Google Scholar]
- Li, Z.; Qiu, F.; Yin, X.; Zou, H.; Gong, M.; Zhai, Y.; Ni, J. Simultaneous LC-MS/MS quantification and pharmacokinetics of baicalin, chlorogenic acid and forsythin after intravenous administration of Shuang-huang-lian powder to dogs. Anal. Methods 2013, 5, 2784. [Google Scholar] [CrossRef]
- Zhu, N.; Li, J.C.; Zhu, J.X.; Wang, X.; Zhang, J. Characterization and Bioavailability of Wogonin by Different Administration Routes in Beagles. Med. Sci. Monit. Int. Med. J. Exp. Clin. Res. 2016, 22, 3737–3745. [Google Scholar] [CrossRef] [Green Version]
- Zhu, Y.; Tong, L.; Zhou, S.; Sun, H.; Bi, K.; Zhang, B. Simultaneous determination of active flavonoids and alkaloids of Tang-Min-Ling-Pill in rat plasma by liquid chromatography tandem mass spectrometry. J. Chromatogr. B Anal. Technol. Biomed. Life Sci. 2012, 904, 51–58. [Google Scholar] [CrossRef]
- Song, J.Z.; Li, L.J.; Ji, L.; Shun, L.; Rui, Y. The pharmacokinetics of Tiangou antihypertensive capsule in rat in vivo. Biomed. Rep. 2017, 6, 113–119. [Google Scholar] [CrossRef]
- Chen, H.; Li, Z.; Li, Y.; Wu, X.; Wang, S.; Chen, K.; Zheng, X.; Du, Q.; Tang, D. Simultaneous determination of baicalin, oroxylin A-7-O-glucuronide and wogonoside in rat plasma by UPLC-DAD and its application in pharmacokinetics of pure baicalin, Radix Scutellariae and Yinhuang granule. Biomed. Chromatogr. BMC 2015, 29, 1819–1825. [Google Scholar] [CrossRef]
- Peng, L.; Gao, X.; Song, Y.; Zhao, L.; Guo, M.; Su, J.; Zhang, L.; Liu, H. A rapid and sensitive UPLC-MS/MS method for quantification of two caffeoylquinic acids and four main active components in rat plasma after an intravenous administration of Qingkailing injection and its application to a pharmacokinetic study: Quantification of six components from Qingkailing injection in plasma. Biomed. Chromatogr. 2014, 28, 601–609. [Google Scholar]
- Lu, Q.Y.; Zhang, L.; Moro, A.; Chen, M.C.; Harris, D.M.; Eibl, G.; Go, V.L.W. Detection of baicalin metabolites baicalein and oroxylin-a in mouse pancreas and pancreatic xenografts. Pancreas 2012, 41, 571–576. [Google Scholar] [CrossRef]
- Hou, Y.C.; Lin, S.P.; Tsai, S.Y.; Ko, M.H.; Chang, Y.C.; Chao, P.D.L. Flavonoid pharmacokinetics and tissue distribution after repeated dosing of the roots of Scutellaria baicalensis in rats. Planta Med. 2011, 77, 455–460. [Google Scholar] [CrossRef]
- Zhu, H.; Qian, Z.; He, F.; Liu, M.; Pan, L.; Zhang, Q.; Tang, Y. Novel pharmacokinetic studies of the Chinese formula Huang-Lian-Jie-Du-Tang in MCAO rats. Phytomed. Int. J. Phytother. Phytopharm. 2013, 20, 767–774. [Google Scholar] [CrossRef]
- Zeng, H.; Yang, R.; Guo, C.; Wang, Q.; Qu, L.; Li, J. Pharmacokinetic study of six flavones in rat plasma and tissues after oral administration of ‘JiangYaBiFeng’ using SPE-HPLC–DAD. J. Pharm. Biomed. Anal. 2011, 56, 815–819. [Google Scholar] [CrossRef]
- Bei, D.; An, G. Pharmacokinetics and tissue distribution of 5,7-dimethoxyflavone in mice following single dose oral administration. J. Pharm. Biomed. Anal. 2016, 119, 65–70. [Google Scholar] [CrossRef]
- Tsuji, P.A.; Winn, R.N.; Walle, T. Accumulation and metabolism of the anticancer flavonoid 5,7-dimethoxyflavone compared to its unmethylated analog chrysin in the Atlantic killifish. Chem. Biol. Interact. 2006, 164, 85–92. [Google Scholar] [CrossRef]
- Fong, S.Y.K.; Li, C.; Ho, Y.C.; Li, R.; Wang, Q.; Wong, Y.C.; Xue, H.; Zuo, Z. Brain Uptake of Bioactive Flavones in Scutellariae Radix and Its Relationship to Anxiolytic Effect in Mice. Mol. Pharm. 2017, 14, 2908–2916. [Google Scholar] [CrossRef]
- Huang, H.; Zhang, Y.; Yang, R.; Tang, X. Determination of baicalin in rat cerebrospinal fluid and blood using microdialysis coupled with ultra-performance liquid chromatography-tandem mass spectrometry. J. Chromatogr. B 2008, 874, 77–83. [Google Scholar] [CrossRef] [PubMed]
- Liu, S.; Li, X.Z.; Xu, L.M.; Lei, P.; Liang, Y.Z. UPLC-MS-MS Analysis of Baicalin in the Cerebrospinal Fluid of Rabbits: Application to a Pharmacokinetic Study. Chromatographia 2008, 68, 463–466. [Google Scholar] [CrossRef]
- Tsai, T.H.; Liu, S.C.; Tsai, P.L.; Ho, L.K.; Shum, A.Y.C.; Chen, C.F. The effects of the cyclosporin A, a P-glycoprotein inhibitor, on the pharmacokinetics of baicalein in the rat: A microdialysis study. Br. J. Pharmacol. 2002, 137, 1314–1320. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Xing, D.; Wang, W.; Wang, R.; Du, L. Kinetic difference of baicalin in rat blood and cerebral nuclei after intravenous administration of Scutellariae Radix extract. J. Ethnopharmacol. 2006, 103, 120–125. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Ouyang, L.; Mai, X.; Wang, H.; Liu, S.; Zeng, H.; Chen, T.; Li, J. Use of UHPLC-QTOF-MS/MS with combination of in silico approach for distributions and metabolites profile of flavonoids after oral administration of Niuhuang Shangqing tablets in rats. J. Chromatogr. B Anal. Technol. Biomed. Life Sci. 2019, 1114–1115, 55–70. [Google Scholar] [CrossRef]
- Wang, C.; Jia, Z.; Wang, Z.; Hu, T.; Qin, H.; Du, G.; Wu, C.; Zhang, J. Pharmacokinetics of 21 active components in focal cerebral ischemic rats after oral administration of the active fraction of Xiao-Xu-Ming decoction. J. Pharm. Biomed. Anal. 2016, 122, 110–117. [Google Scholar] [CrossRef] [PubMed]
- Fong, S.Y.K.; Wong, Y.C.; Zuo, Z. Development of a SPE-LC/MS/MS method for simultaneous quantification of baicalein, wogonin, oroxylin A and their glucuronides baicalin, wogonoside and oroxyloside in rats and its application to brain uptake and plasma pharmacokinetic studies. J. Pharm. Biomed. Anal. 2014, 97, 9–23. [Google Scholar] [CrossRef]
- Tsai, M.J.; Wu, P.C.; Huang, Y.B.; Chang, J.S.; Lin, C.L.; Tsai, Y.H.; Fang, J.Y. Baicalein loaded in tocol nanostructured lipid carriers (tocol NLCs) for enhanced stability and brain targeting. Int. J. Pharm. 2012, 423, 461–470. [Google Scholar] [CrossRef]
- Liu, Y.; Ma, Y.; Xu, J.; Chen, Y.; Xie, J.; Yue, P.; Zheng, Q.; Yang, M. Apolipoproteins adsorption and brain-targeting evaluation of baicalin nanocrystals modified by combination of Tween80 and TPGS. Colloids Surf. B Biointerfaces 2017, 160, 619–627. [Google Scholar] [CrossRef]
- Liu, Z.; Zhao, H.; Shu, L.; Zhang, Y.; Okeke, C.; Zhang, L.; Li, J.; Li, N. Preparation and evaluation of Baicalin-loaded cationic solid lipid nanoparticles conjugated with OX26 for improved delivery across the BBB. Drug Dev. Ind. Pharm. 2015, 41, 353–361. [Google Scholar] [CrossRef] [PubMed]
- Jiang, X.H.; Ma, J.H.; Li, N.; Je, Y.J.; Yang, M. Pharmacokinetics of baicalin-phospholipid complex in rat plasma and brai tissues after intranasal and intravenous administration. Pharmazie 2011, 66, 374–377. [Google Scholar]
- Zhiyan, J.; Zhengzhong, B.; Liange, J.; Shujie, Z.; Kai, D.; Hao, C.; Yongbin, Y.; Ping, L. Ocular pharmacokinetic study on baicalin in lens of rabbits following intragastric administration. Graefes Arch. Clin. Exp. Ophthalmol. 2010, 248, 59–63. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Q.; Cong, D.; An, D.; Fan, A.; Liu, Q.; Yi, Y.; Song, Z.; Chen, X.; Lu, Y.; Zhao, D.; et al. Determination of oroxylin A and oroxylin A 7-O-d-glucuronide in HepG2 cell lysate and subcellular fractions with SPE-UPLC-MS/MS: Cellular pharmacokinetic study to indicate anti-cancer mechanisms. J. Pharm. Biomed. Anal. 2018, 154, 364–372. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Q.; Zheng, Z.; Xia, B.; Tang, L.; Lv, C.; Liu, W.; Liu, Z.; Hu, M. Use of isoform-specific UGT metabolism to determine and describe rates and profiles of glucuronidation of wogonin and oroxylin A by human liver and intestinal microsomes. Pharm. Res. 2010, 27, 1568–1583. [Google Scholar] [CrossRef] [PubMed]
- Wen, X.; Walle, T. Methylated flavonoids have greatly improved intestinal absorption and metabolic stability. Drug Metab. Dispos. Biol. Fate Chem. 2006, 34, 1786–1792. [Google Scholar] [CrossRef] [PubMed]
- Simons, A.L.; Renouf, M.; Hendrich, S.; Murphy, P.A. Human gut microbial degradation of flavonoids: Structure-function relationships. J. Agric. Food Chem. 2005, 53, 4258–4263. [Google Scholar] [CrossRef]
- Griffiths, L.A.; Smith, G.E. Metabolism of apigenin and related compounds in the rat. Metabolite formation in vivo and by the intestinal microflora in vitro. Biochem. J. 1972, 128, 901–911. [Google Scholar] [CrossRef]
- Lin, Y.T.; Hsiu, S.L.; Hou, Y.C.; Chen, H.Y.; Chao, P.D.L. Degradation of flavonoid aglycones by rabbit, rat and human fecal flora. Biol. Pharm. Bull. 2003, 26, 747–751. [Google Scholar] [CrossRef]
- Zhang, L.; Lin, G.; Chang, Q.; Zuo, Z. Role of intestinal first-pass metabolism of baicalein in its absorption process. Pharm. Res. 2005, 22, 1050–1058. [Google Scholar] [CrossRef] [PubMed]
- Zhou, W.; Di, L.; Shan, J.; Bi, X.; Chen, L.; Wang, L.; Cai, B. In vitro metabolism in Sprague–Dawley rat liver microsomes of forsythoside A in different compositions of Shuang-Huang-Lian. Fitoterapia 2011, 82, 1222–1230. [Google Scholar] [CrossRef] [PubMed]
- Srinivas, N.R. Baicalin, an emerging multi-therapeutic agent: Pharmacodynamics, pharmacokinetics, and considerations from drug development perspectives. Xenobiotica 2010, 40, 357–367. [Google Scholar] [CrossRef] [PubMed]
- Fan, L.; Wang, J.C.; Jiang, F.; Tan, Z.R.; Chen, Y.; Li, Q.; Zhang, W.; Wang, G.; Lei, H.P.; Hu, D.L.; et al. Induction of cytochrome P450 2B6 activity by the herbal medicine baicalin as measured by bupropion hydroxylation. Eur. J. Clin. Pharmacol. 2009, 65, 403–409. [Google Scholar] [CrossRef] [PubMed]
- Tang, L.; Ye, L.; Singh, R.; Wu, B.; Lv, C.; Zhao, J.; Liu, Z.; Hu, M. Use of Glucuronidation Fingerprinting to Describe and Predict Mono-and Dihydroxyflavone Metabolism by Recombinant UGT Isoforms and Human Intestinal and Liver Microsomes. Mol. Pharm. 2010, 7, 664–679. [Google Scholar] [CrossRef] [PubMed]
- Zhang, W.; Saif, M.W.; Dutschman, G.E.; Li, X.; Lam, W.; Bussom, S.; Jiang, Z.; Ye, M.; Chu, E.; Cheng, Y.C. Identification of chemicals and their metabolites from PHY906, a Chinese medicine formulation, in the plasma of a patient treated with irinotecan and PHY906 using liquid chromatography/tandem mass spectrometry (LC/MS/MS). J. Chromatogr. A 2010, 1217, 5785–5793. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhang, H.; Duan, S.; Wang, L.; Liu, J.; Qi, W.; Yuan, D. Identification of the absorbed components and their metabolites of Tianma-Gouteng granule in rat plasma and bile using ultra-high-performance liquid chromatography combined with quadrupole time-of-flight mass spectrometry. Biomed. Chromatogr. 2019, 33, e4480. [Google Scholar] [CrossRef] [PubMed]
- Chen, F.; Li, H.L.; Tan, Y.F.; Li, Y.H.; Lai, W.Y.; Guan, W.W.; Zhang, J.Q.; Zhao, Y.S.; Qin, Z.M. Identification of known chemicals and their metabolites from Alpinia oxyphylla fruit extract in rat plasma using liquid chromatography/tandem mass spectrometry (LC–MS/MS) with selected reaction monitoring. J. Pharm. Biomed. Anal. 2014, 97, 166–177. [Google Scholar] [CrossRef] [PubMed]
- Quan, E.; Wang, H.; Dong, D.; Zhang, X.; Wu, B. Characterization of chrysin glucuronidation in UGT1A1-overexpressing HeLa cells: Elucidating the transporters responsible for efflux of glucuronide. Drug Metab. Dispos. Biol. Fate Chem. 2015, 43, 433–443. [Google Scholar] [CrossRef]
- Ma, G.; Wu, B.; Gao, S.; Yang, Z.; Ma, Y.; Hu, M. Mutual Regioselective Inhibition of Human UGT1A1-Mediated Glucuronidation of Four Flavonoids. Mol. Pharm. 2013, 10, 2891–2903. [Google Scholar] [CrossRef] [Green Version]
- Wang, S.W.J.; Kulkarni, K.H.; Tang, L.; Wang, J.R.; Yin, T.; Daidoji, T.; Yokota, H.; Hu, M. Disposition of Flavonoids via Enteric Recycling: UDP-Glucuronosyltransferase (UGT) 1As Deficiency in Gunn Rats Is Compensated by Increases in UGT2Bs Activities. J. Pharmacol. Exp. Ther. 2009, 329, 1023–1031. [Google Scholar] [CrossRef] [Green Version]
- Zhang, L.; Li, C.; Lin, G.; Krajcsi, P.; Zuo, Z. Hepatic metabolism and disposition of baicalein via the coupling of conjugation enzymes and transporters-in vitro and in vivo evidences. AAPS J. 2011, 13, 378–389. [Google Scholar] [CrossRef]
- Galijatovic, A.; Otake, Y.; Walle, U.K.; Walle, T. Extensive metabolism of the flavonoid chrysin by human Caco-2 and Hep G2 cells. Xenobiotica Fate Foreign Compd. Biol. Syst. 1999, 29, 1241–1256. [Google Scholar] [CrossRef]
- Walle, T.; Otake, Y.; Brubaker, J.A.; Walle, U.K.; Halushka, P.V. Disposition and metabolism of the flavonoid chrysin in normal volunteers. Br. J. Clin. Pharmacol. 2001, 51, 143–146. [Google Scholar] [CrossRef]
- Walle, U.K.; Walle, T. Induction of human UDP-glucuronosyltransferase UGT1A1 by flavonoids-structural requirements. Drug Metab. Dispos. Biol. Fate Chem. 2002, 30, 564–569. [Google Scholar] [CrossRef]
- Wu, B.; Xu, B.; Hu, M. Regioselective Glucuronidation of Flavonols by Six Human UGT1A Isoforms. Pharm. Res. 2011, 28, 1905–1918. [Google Scholar] [CrossRef] [Green Version]
- Singh, R.; Wu, B.; Tang, L.; Hu, M. Uridine Diphosphate Glucuronosyltransferase Isoform-Dependent Regiospecificity of Glucuronidation of Flavonoids. J. Agric. Food Chem. 2011, 59, 7452–7464. [Google Scholar] [CrossRef] [Green Version]
- Xie, S.; Chen, Y.; Chen, S.; Zeng, S. Structure-metabolism relationships for the glucuronidation of flavonoids by UGT1A3 and UGT1A9. J. Pharm. Pharmacol. 2011, 63, 297–304. [Google Scholar] [CrossRef]
- Robotham, S.A.; Brodbelt, J.S. Identification of flavone glucuronide isomers by metal complexation and tandem mass spectrometry: Regioselectivity of uridine 5′-diphosphate-glucuronosyltransferase isozymes in the biotransformation of flavones. J. Agric. Food Chem. 2013, 61, 1457–1463. [Google Scholar] [CrossRef]
- Wong, Y.C.; Zhang, L.; Lin, G.; Zuo, Z. Intestinal first-pass glucuronidation activities of selected dihydroxyflavones. Int. J. Pharm. 2009, 366, 14–20. [Google Scholar] [CrossRef]
- Chen, Y.; Xie, S.; Chen, S.; Zeng, S. Glucuronidation of flavonoids by recombinant UGT1A3 and UGT1A9. Biochem. Pharmacol. 2008, 76, 416–425. [Google Scholar] [CrossRef]
- Guo, H.M.; Sun, Y.M.; Zhang, S.X.; Ju, X.L.; Xie, A.Y.; Li, J.; Zou, L.; Sun, X.D.; Li, H.L.; Zheng, Y. Metabolism and pharmacokinetics of 8-hydroxypiperidinylmethyl-baicalein (BA-j) as a novel selective CDK1 inhibitor in monkey. Fitoterapia 2015, 107, 36–43. [Google Scholar] [CrossRef]
- Fong, S.Y.K.; Zuo, Z. Species difference in the inhibitory potentials of non-steroidal anti-inflammatory drugs on the hepatic sulfation and glucuronidation of bioactive flavonoids: Differential observations among common inhibition parameters. Xenobiotica Fate Foreign Compd. Biol. Syst. 2014, 44, 417–431. [Google Scholar] [CrossRef]
- Shia, C.S.; Tsai, S.Y.; Kuo, S.C.; Hou, Y.C.; Chao, P.D.L. Metabolism and Pharmacokinetics of 3,3′,4′,7-Tetrahydroxyflavone (Fisetin), 5-Hydroxyflavone, and 7-Hydroxyflavone and Antihemolysis Effects of Fisetin and Its Serum Metabolites. J. Agric. Food Chem. 2009, 57, 83–89. [Google Scholar] [CrossRef]
- Ng, S.P.; Wong, K.Y.; Zhang, L.; Zuo, Z.; Lin, G. Evaluation of the first-pass glucuronidation of selected flavones in gut by Caco-2 monolayer model. J. Pharm. Pharm. Sci. 2004, 8, 1–9. [Google Scholar]
- Akao, T.; Sato, K.; He, J.X.; Ma, C.M.; Hattori, M. Baicalein 6-O-β-D-glucopyranuronoside is a main metabolite in the plasma after oral administration of baicalin, a flavone glucuronide of scutellariae radix, to rats. Biol. Pharm. Bull. 2013, 36, 748–753. [Google Scholar] [CrossRef]
- Zhang, Z.Q.; Liua, W.; Zhuang, L.; Wang, J.; Zhang, S. Comparative pharmacokinetics of baicalin, wogonoside, baicalein and wogonin in plasma after oral administration of pure baicalin, radix scutellariae and scutellariae-paeoniae couple extracts in normal and ulcerative colitis rats. Iran. J. Pharm. Res. IJPR 2013, 12, 399–409. [Google Scholar]
- Guo, X.Y.; Yang, L.; Chen, Y.; Wang, Q.F.; Sun, Q.S.; Che, Y.X.; Che, Q.M. Identification of the metabolites of baicalein in human plasma. J. Asian Nat. Prod. Res. 2011, 13, 861–868. [Google Scholar] [CrossRef]
- Abe, K.; Inoue, O.; Yumioka, E. Biliary excretion of metabolites of baicalin and baicalein in rats. Chem. Pharm. Bull. 1990, 38, 209–211. [Google Scholar] [CrossRef]
- Zhang, J.; Cai, W.; Zhou, Y.; Liu, Y.; Wu, X.; Li, Y.; Lu, J.; Qiao, Y. Profiling and identification of the metabolites of baicalin and study on their tissue distribution in rats by ultra-high-performance liquid chromatography with linear ion trap-Orbitrap mass spectrometer. J. Chromatogr. B Anal. Technol. Biomed. Life Sci. 2015, 985, 91–102. [Google Scholar] [CrossRef]
- Li, C.; Zhang, L.; Lin, G.; Zuo, Z. Identification and quantification of baicalein, wogonin, oroxylin A and their major glucuronide conjugated metabolites in rat plasma after oral administration of Radix scutellariae product. J. Pharm. Biomed. Anal. 2011, 54, 750–758. [Google Scholar] [CrossRef]
- Liu, W.; Xu, X.; Feng, F.; Wu, C. Simultaneous Quantification of Oroxylin A and Its Metabolite Oroxylin A-7-O-Glucuronide: Application to a Pharmacokinetic Study in Rat. Chromatographia 2011, 74, 75–81. [Google Scholar] [CrossRef]
- Srinivas, N.R. Is There Saturation in the Conversion of Baicalein to Baicalin After Oral Chewable Tablets: Retrospective Evaluation of the Human Pharmacokinetic Data? Clin. Drug Investig. 2016, 36, 1075–1076. [Google Scholar] [CrossRef]
- Li, W.; Sun, H.; Zhang, X.; Wang, H.; Wu, B. Efflux transport of chrysin and apigenin sulfates in HEK293 cells overexpressing SULT1A3: The role of multidrug resistance-associated protein 4 (MRP4/ABCC4). Biochem. Pharmacol. 2015, 98, 203–214. [Google Scholar] [CrossRef]
- Pasqualini, J.R. Estrogen Sulfotransferases in Breast and Endometrial Cancers. Ann. N. Y. Acad. Sci. 2009, 1155, 88–98. [Google Scholar] [CrossRef]
- Zhang, L.; Lin, G.; Zuo, Z. Involvement of UDP-glucuronosyltransferases in the extensive liver and intestinal first-pass metabolism of flavonoid baicalein. Pharm. Res. 2007, 24, 81–89. [Google Scholar] [CrossRef]
- Lai, M.Y.; Hsiu, S.L.; Chen, C.C.; Hou, Y.C.; Chao, P.D.L. Urinary pharmacokinetics of baicalein, wogonin and their glycosides after oral administration of Scutellariae Radix in humans. Biol. Pharm. Bull. 2003, 26, 79–83. [Google Scholar] [CrossRef]
- Vietri, M.; Pietrabissa, A.; Spisni, R.; Mosca, F.; Pacifici, G.M. 7-OH-flavone is sulfated in the human liver and duodenum, whereas 5-OH-flavone and 3-OH-flavone are potent inhibitors of SULT1A1 activity and 7-OH-flavone sulfation rate. Xenobiotica 2002, 32, 563–571. [Google Scholar] [CrossRef]
- Ung, D.; Nagar, S. Variable sulfation of dietary polyphenols by recombinant human sulfotransferase (SULT) 1A1 genetic variants and SULT1E1. Drug Metab. Dispos. Biol. Fate Chem. 2007, 35, 740–746. [Google Scholar] [CrossRef]
- Wen, X.; Walle, T. Methylation protects dietary flavonoids from rapid hepatic metabolism. Xenobiotica Fate Foreign Compd. Biol. Syst. 2006, 36, 387–397. [Google Scholar] [CrossRef]
- Walle, U.K.; Walle, T. Bioavailable flavonoids: Cytochrome P450-mediated metabolism of methoxyflavones. Drug Metab. Dispos. Biol. Fate Chem. 2007, 35, 1985–1989. [Google Scholar] [CrossRef]
- Kim, M.; Kim, N.; Han, J. Metabolism of Kaempferia parviflora Polymethoxyflavones by Human Intestinal Bacterium Bautia sp. MRG-PMF1. J. Agric. Food Chem. 2014, 62, 12377–12383. [Google Scholar] [CrossRef] [PubMed]
- Burapan, S.; Kim, M.; Han, J. Demethylation of Polymethoxyflavones by Human Gut Bacterium, Blautia sp. MRG-PMF1. J. Agric. Food Chem. 2017, 65, 1620–1629. [Google Scholar] [CrossRef] [PubMed]
- Rajilić-Stojanović, M.; de Vos, W.M. The first 1000 cultured species of the human gastrointestinal microbiota. FEMS Microbiol. Rev. 2014, 38, 996–1047. [Google Scholar] [CrossRef] [PubMed]
- Fischer, M.; Fadda, H.M. The Effect of Sex and Age on Small Intestinal Transit Times in Humans. J. Pharm. Sci. 2016, 105, 682–686. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yu, J.; Guo, X.; Zhang, Q.; Peng, Y.; Zheng, J. Metabolite profile analysis and pharmacokinetic study of emodin, baicalin and geniposide in rats. Xenobiotica 2018, 48, 927–937. [Google Scholar] [CrossRef] [PubMed]
- Yang, H.; Li, J.; Zheng, Y.; Zhou, L.; Tong, S.; Zhao, B.; Cai, W. Drug activity screening based on microsomes-hydrogel system in predicting metabolism induced antitumor effect of oroxylin A. Sci. Rep. 2016, 6, 21604. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Currò, D. The role of gut microbiota in the modulation of drug action: A focus on some clinically significant issues. Expert Rev. Clin. Pharmacol. 2018, 11, 171–183. [Google Scholar] [CrossRef] [PubMed]
- Kim, D.H.; Jung, E.A.; Sohng, I.S.; Han, J.A.; Kim, T.H.; Han, M.J. Intestinal bacterial metabolism of flavonoids and its relation to some biological activities. Arch. Pharm. Res. 1998, 21, 17–23. [Google Scholar] [CrossRef]
- Liu, W.; Zhang, S.; Fu, X.; Li, H.J.; Xiao, W.; Zhang, Z.Q. A comparative study of excretion of the components after oral administration of pure baicalin radix scutellariae and scutellariae-paeoniae couple extracts to normal and ulcerative colitis rats. Biomed. Res. INDIA 2015, 26, 13–22. [Google Scholar]
- Pang, H.; Xue, W.; Shi, A.; Li, M.; Li, Y.; Cao, G.; Yan, B.; Dong, F.; Xiao, W.; He, G.; et al. Multiple-Ascending-Dose Pharmacokinetics and Safety Evaluation of Baicalein Chewable Tablets in Healthy Chinese Volunteers. Clin. Drug Investig. 2016, 36, 713–724. [Google Scholar] [CrossRef]
- Wang, T.; Long, F.; Jiang, G.; Cai, H.; Jiang, Q.; Cheng, K.; Hu, Z.; Wang, Y. Pharmacokinetic properties of wogonin and its herb-drug interactions with docetaxel in rats with mammary tumors. Biomed. Chromatogr. BMC 2018, e4264. [Google Scholar] [CrossRef]
- Peng, J.; Qi, Q.; You, Q.; Hu, R.; Liu, W.; Feng, F.; Wang, G.; Guo, Q. Subchronic toxicity and plasma pharmacokinetic studies on wogonin, a natural flavonoid, in Beagle dogs. J. Ethnopharmacol. 2009, 124, 257–262. [Google Scholar] [CrossRef]
- Shen, H.; Liu, Y.; Zhang, H.; Ding, P.; Zhang, L.; Zhang, L.; Ju, J. Enhancing the oral bioavailability of baicalein via Solutol® HS15 and Poloxamer 188 mixed micelles system. J. Pharm. Pharmacol. 2018, 71, 765–773. [Google Scholar] [CrossRef]
- Fan, J.; Dai, Y.; Shen, H.; Ju, J.; Zhao, Z. Application of Soluplus to Improve the Flowability and Dissolution of Baicalein Phospholipid Complex. Molecules 2017, 22, 776. [Google Scholar] [CrossRef]
- Guo, X.Y.; Yang, L.; Chen, Y.; Che, Q.M. Comparison of pharmacokinetics of baicalein and baicalin in rats. Chin. Pharm. J. 2008, 43, 524–526. [Google Scholar]
- Zhang, H.; Yang, X.; Zhao, L.; Jiao, Y.; Liu, J.; Zhai, G. In vitro and in vivo study of Baicalin-loaded mixed micelles for oral delivery. Drug Deliv. 2015, 23, 1933–1939. [Google Scholar]
- Li, W.; Pi, J.; Zhang, Y.; Ma, X.; Zhang, B.; Wang, S.; Qi, D.; Li, N.; Guo, P.; Liu, Z. A strategy to improve the oral availability of baicalein: The baicalein-theophylline cocrystal. Fitoterapia 2018, 129, 85–93. [Google Scholar] [CrossRef]
- Huang, Y.; Zhang, B.; Gao, Y.; Zhang, J.; Shi, L. Baicalein-nicotinamide cocrystal with enhanced solubility, dissolution, and oral bioavailability. J. Pharm. Sci. 2014, 103, 2330–2337. [Google Scholar] [CrossRef]
- Zhu, B.; Zhang, Q.; Wang, J.R.; Mei, X. Cocrystals of Baicalein with Higher Solubility and Enhanced Bioavailability. Cryst. Growth Des. 2017, 17, 1893–1901. [Google Scholar] [CrossRef]
- Li, B.; He, M.; Li, W.; Luo, Z.; Guo, Y.; Li, Y.; Zang, C.; Wang, B.; Li, F.; Li, S.; et al. Dissolution and pharmacokinetics of baicalin-polyvinylpyrrolidone coprecipitate. J. Pharm. Pharmacol. 2013, 65, 1670–1678. [Google Scholar] [CrossRef]
- Pi, J.; Wang, S.; Li, W.; Kebebe, D.; Zhang, Y.; Zhang, B.; Qi, D.; Guo, P.; Li, N.; Liu, Z. A nano-cocrystal strategy to improve the dissolution rate and oral bioavailability of baicalein. Asian J. Pharm. Sci. 2019, 14, 154–164. [Google Scholar] [CrossRef]
- Jin, S.-Y.; Han, J.; Jin, Shi-Xiao; Lv, Q.-Y.; Bai, J.-X.; Chen, H.-G.; Li, R.-S.; Wu, W.; Yuan, H.-L. Characterization and evaluation in vivo of baicalin-nanocrystals prepared by an ultrasonic-homogenization-fluid bed drying method. Chin. J. Nat. Med. 2014, 12, 71–80. [Google Scholar] [CrossRef]
- Yue, P.F.; Li, Y.; Wang, Y.; Zhu, W.-F.; Wang, C.-H.; Yuan, H.L.; Yang, M. Process optimization and evaluation of novel baicalin solid nanocrystals. Int. J. Nanomed. 2013, 8, 2961–2973. [Google Scholar] [CrossRef] [Green Version]
- Meng, L.; Xia, X.; Yang, Y.; Ye, J.; Dong, W.; Ma, P.; Jin, Y.; Liu, Y. Co-encapsulation of paclitaxel and baicalein in nanoemulsions to overcome multidrug resistance via oxidative stress augmentation and P-glycoprotein inhibition. Int. J. Pharm. 2016, 513, 8–16. [Google Scholar] [CrossRef]
- Yin, J.; Xiang, C.; Wang, P.; Yin, Y.; Hou, Y. Biocompatible nanoemulsions based on hemp oil and less surfactants for oral delivery of baicalein with enhanced bioavailability. Int. J. Nanomed. 2017, 12, 2923–2931. [Google Scholar] [CrossRef]
- Zhao, L.; Wei, Y.; Huang, Y.; He, B.; Zhou, Y.; Fu, J. Nanoemulsion improves the oral bioavailability of baicalin in rats: In vitro and in vivo evaluation. Int. J. Nanomed. 2013, 8, 3769–3779. [Google Scholar] [CrossRef]
- Wu, L.; Bi, Y.; Wu, H. Formulation optimization and the absorption mechanisms of nanoemulsion in improving baicalin oral exposure. Drug Dev. Ind. Pharm. 2018, 44, 266–275. [Google Scholar] [CrossRef]
- Gao, Y.; Jiang, K.; Li, L.; Xi, Y.F. Bioavailability enhancement of baicalein by nanosuspension. J. China Pharm. Univ. 2011, 42, 314–318. [Google Scholar]
- Liang, J.; Wu, W.; Liu, Q.; Chen, S. Long-circulating nanoliposomes (LCNs) sustained delivery of baicalein (BAI) with desired oral bioavailability in vivo. Drug Deliv. 2013, 20, 319–323. [Google Scholar] [CrossRef]
- Zhao, L.; Wei, Y.; Guo, J.; Zheng, X.; Wu, J.; Zhou, Y.; Yu, Y.; Zhang, L.; Ye, Y. Preparation, pharmacokinetics and biodistribution of baicalin-loaded liposomes. Int. J. Nanomed. 2014, 9, 3623–3630. [Google Scholar] [CrossRef] [Green Version]
- Shi, F.; Wei, Z.; Zhao, Y.; Xu, X. Nanostructured lipid carriers loaded with baicalin: An efficient carrier for enhanced antidiabetic effects. Pharmacogn. Mag. 2016, 12, 198. [Google Scholar]
- Luan, J.; Zheng, F.; Yang, X.; Yu, A.; Zhai, G. Nanostructured lipid carriers for oral delivery of baicalin: In vitro and in vivo evaluation. Colloids Surf. Physicochem. Eng. Asp. 2015, 466, 154–159. [Google Scholar] [CrossRef]
- Wang, W.; Xi, M.; Duan, X.; Wang, Y.; Kong, F. Delivery of baicalein and paclitaxel using self-assembled nanoparticles: Synergistic antitumor effect in vitro and in vivo. Int. J. Nanomed. 2015, 10, 3737–3750. [Google Scholar]
- Hao, J.; Wang, F.; Wang, X.; Zhang, D.; Bi, Y.; Gao, Y.; Zhao, X.; Zhang, Q. Development and optimization of baicalin-loaded solid lipid nanoparticles prepared by coacervation method using central composite design. Eur. J. Pharm. Sci. 2012, 47, 497–505. [Google Scholar] [CrossRef]
- Yu, H.; Chang, J.S.; Kim, S.Y.; Kim, Y.G.; Choi, H.K. Enhancement of solubility and dissolution rate of baicalein, wogonin and oroxylin A extracted from Radix scutellariae. Int. J. Pharm. 2017, 528, 602–610. [Google Scholar] [CrossRef]
- He, X.; Pei, L.; Tong, H.H.Y.; Zheng, Y. Comparison of spray freeze drying and the solvent evaporation method for preparing solid dispersions of baicalein with Pluronic F68 to improve dissolution and oral bioavailability. AAPS PharmSciTech 2011, 12, 104–113. [Google Scholar] [CrossRef]
- Zhou, Y.; Dong, W.; Ye, J.; Hao, H.; Zhou, J.; Wang, R.; Liu, Y. A novel matrix dispersion based on phospholipid complex for improving oral bioavailability of baicalein: Preparation, in vitro and in vivo evaluations. Drug Deliv. 2017, 24, 720–728. [Google Scholar] [CrossRef]
- Cui, L.; Sune, E.; Song, J.; Wang, J.; Jia, X.B.; Zhang, Z.H. Characterization and Bioavailability Study of Baicalin-mesoporous Carbon Nanopowder Solid Dispersion. Pharmacogn. Mag. 2016, 12, 326–332. [Google Scholar]
- Liu, J.; Qiu, L.; Gao, J.; Jin, Y. Preparation, characterization and in vivo evaluation of formulation of baicalein with hydroxypropyl-beta-cyclodextrin. Int. J. Pharm. 2006, 312, 137–143. [Google Scholar] [CrossRef]
- Liu, W.; Tian, R.; Hu, W.; Jia, Y.; Jiang, H.; Zhang, J.; Zhang, L. Preparation and evaluation of self-microemulsifying drug delivery system of baicalein. Fitoterapia 2012, 83, 1532–1539. [Google Scholar] [CrossRef]
- Lai, M.Y.; Hsiu, S.L.; Tsai, S.Y.; Hou, Y.C.; Chao, P.D.L. Comparison of metabolic pharmacokinetics of baicalin and baicalein in rats. J. Pharm. Pharmacol. 2003, 55, 205–209. [Google Scholar] [CrossRef]
- Wakui, Y.; Yanagisawa, E.; Ishibashi, E.; Matsuzaki, Y.; Takeda, S.; Sasaki, H.; Aburada, M.; Oyama, T. Determination of baicalin and baicalein in rat plasma by high-performance liquid chromatography with electrochemical detection. J. Chromatogr. 1992, 575, 131–136. [Google Scholar] [CrossRef]
- Wakui, Y.; Takeda, S.; Yanagisawa, E.; Isoni, T.; Kaneko, M.; Ishihara, K.; Miyamoto, C.; Hirayama, M.; Imai, K.; Ishibashi, E.; et al. Pharmacokinetic study of the herbal preparation TJ-9 (Shosaiko-to). Eur. J. Pharmacol. 1990, 183, 1867. [Google Scholar] [CrossRef]
- Li, Z.; Wen, R.; Du, Y.; Zhao, S.; Zhao, P.; Jiang, H.; Rong, R.; Lv, Q. Simultaneous quantification of fifteen compounds in rat plasma by LC-MS/MS and its application to a pharmacokinetic study of Chaihu-Guizhi decoction. J. Chromatogr. B Anal. Technol. Biomed. Life Sci. 2019, 1105, 15–25. [Google Scholar] [CrossRef]
- Shia, C.S.; Hou, Y.C.; Juang, S.H.; Tsai, S.Y.; Hsieh, P.H.; Ho, L.C.; Chao, P.D.L. Metabolism and Pharmacokinetics of San-Huang-Xie-Xin-Tang, a Polyphenol-Rich Chinese Medicine Formula, in Rats and Ex-Vivo Antioxidant Activity. Evid. Based Complement. Altern. Med. 2011, 2011, 1–9. [Google Scholar] [CrossRef]
- Kotani, A.; Kojima, S.; Hakamata, H.; Kusu, F. HPLC with electrochemical detection to examine the pharmacokinetics of baicalin and baicalein in rat plasma after oral administration of a Kampo medicine. Anal. Biochem. 2006, 350, 99–104. [Google Scholar] [CrossRef]
- Tian, S.; He, G.; Song, J.; Wang, S.; Xin, W.; Zhang, D.; Du, G. Pharmacokinetic study of baicalein after oral administration in monkeys. Fitoterapia 2012, 83, 532–540. [Google Scholar] [CrossRef]
- Chen, X.; Wang, H.; Du, Y.; Zhong, D. Quantitation of the flavonoid wogonin and its major metabolite wogonin-7 beta-D-glucuronide in rat plasma by liquid chromatography-tandem mass spectrometry. J. Chromatogr. B Anal. Technol. Biomed. Life Sci. 2002, 775, 169–178. [Google Scholar] [CrossRef]
- Chadha, R.; Bhalla, Y.; Nandan, A.; Chadha, K.; Karan, M. Chrysin cocrystals: Characterization and evaluation. J. Pharm. Biomed. Anal. 2017, 134, 361–371. [Google Scholar] [CrossRef]
- Aishwarya, V.; Sumathi, T. Enhanced blood–brain barrier transmigration using the novel chrysin embedded solid lipid nanoformulation: A salient approach on physico-chemical characterization, pharmacokinetics and biodistribution studies. Int. J. Pharm. Clin. Res. 2016, 8, 1574–1582. [Google Scholar]
- Yang, C.H.; Tang, L.; Lv, C.; Ye, L.; Xia, B.J.; Hu, M.; Liu, Z.Q. Sulfation of selected mono-hydroxyflavones by sulfotransferases in vitro: A species and gender comparison: Sulfation comparison of hydroxyflavones. J. Pharm. Pharmacol. 2011, 63, 967–970. [Google Scholar] [CrossRef]
- Punt, A.; Delatour, T.; Scholz, G.; Schilter, B.; van Bladeren, P.J.; Rietjens, I.M.C.M. Tandem Mass Spectrometry Analysis of N2-(trans-Isoestragol-3’-yl)-2’-deoxyguanosine as a Strategy to Study Species Differences in Sulfotransferase Conversion of the Proximate Carcinogen 1’-Hydroxyestragole. Chem. Res. Toxicol. 2007, 20, 991–998. [Google Scholar] [CrossRef]
- Wang, Q.; Ye, C.; Jia, R.; Owen, A.J.; Hidalgo, I.J.; Li, J. Inter-species comparison of 7-hydroxycoumarin glucuronidation and sulfation in liver S9 fractions. In Vitro Cell. Dev. Biol. Anim. 2006, 42, 8–12. [Google Scholar] [CrossRef]
- Noh, K.; Nepal, M.R.; Jeong, K.S.; Kim, S.A.; Um, Y.J.; Seo, C.S.; Kang, M.J.; Park, P.H.; Kang, W.; Jeong, H.G.; et al. Effects of baicalin on oral pharmacokinetics of caffeine in rats. Biomol. Ther. 2015, 23, 201–206. [Google Scholar] [CrossRef]
- Homma, M.; Oka, K.; Taniguchi, C.; Niitsuma, T.; Hayashi, T. Systematic analysis of post-administrative saiboku-to urine by liquid chromatography to determine pharmacokinetics of traditional Chinese medicine. Biomed. Chromatogr. BMC 1997, 11, 125–131. [Google Scholar] [CrossRef]
- Kang, M.J.; Ko, G.S.; Oh, D.G.; Kim, J.S.; Noh, K.; Kang, W.; Yoon, W.K.; Kim, H.C.; Jeong, H.G.; Jeong, T.C. Role of metabolism by intestinal microbiota in pharmacokinetics of oral baicalin. Arch. Pharm. Res. 2014, 37, 371–378. [Google Scholar] [CrossRef]
- Zhang, Q.; Zhang, S.; Meng, X.X.; Zhang, M.; Gao, X.L. Effects of intestinal flora imbalance on pharmacokinetic parameters of baicalin and baicalein in rats. Chin. Tradit. Herb. Drugs 2017, 48, 3783–3788. [Google Scholar]
- Xing, S.; Wang, M.; Peng, Y.; Li, X. Effects of intestinal microecology on metabolism and pharmacokinetics of oral wogonoside and Baicalin. Nat. Prod. Commun. 2017, 12, 509–514. [Google Scholar] [CrossRef]
- Jung, M.A.; Jang, S.E.; Hong, S.W.; Hana, M.J.; Kim, D.H. The role of intestinal microflora in anti-inflammatory effect of baicalin in mice. Biomol. Ther. 2012, 20, 36–42. [Google Scholar] [CrossRef]
- Pang, H.; Shi, A.; Li, M.; Xue, W.; Li, Y.; Cao, G.; Yan, B.; Dong, F.; Xiao, W.; He, G.; et al. Simultaneous Determination of Baicalein and Baicalin in Human Plasma by High Performance Liquid Chromatograph-Tandem Spectrometry and its Application in a Food-Effect Pharmacokinetic Study. Drug Res. 2016, 66, 394–401. [Google Scholar] [CrossRef]
- Li, C.R.; Zhang, L.; Wo, S.K.; Zhou, L.M.; Lin, G.; Zuo, Z. Pharmacokinetic interactions among major bioactive components in Radix Scutellariae via metabolic competition. Biopharm. Drug Dispos. 2012, 33, 487–500. [Google Scholar] [CrossRef]
- Kim, Y.H.; Jeong, D.W.; Kim, Y.C.; Sohn, D.H.; Park, E.S.; Lee, H.S. Pharmacokinetics of baicalein, baicalin and wogonin after oral administration of a standardized extract of Scutellaria baicalensis, PF-2405 in rats. Arch. Pharm. Res. 2007, 30, 260–265. [Google Scholar] [CrossRef]
- Huang, T.; Liu, Y.; Zhang, C. Pharmacokinetics and Bioavailability Enhancement of Baicalin: A Review. Eur. J. Drug Metab. Pharmacokinet. 2019, 44, 159–168. [Google Scholar] [CrossRef]
- Shi, R.; Zhou, H.; Liu, Z.; Ma, Y.; Wang, T.; Liu, Y.; Wang, C. Influence of coptis Chinensis on pharmacokinetics of flavonoids after oral administration of radix Scutellariae in rats. Biopharm. Drug Dispos. 2009, 30, 398–410. [Google Scholar] [CrossRef]
- Zuo, F.; Zhou, Z.M.; Zhang, Q.; Mao, D.; Xiong, Y.L.; Wang, Y.L.; Yan, M.Z.; Liu, M.L. Pharmacokinetic study on the multi-constituents of Huangqin-Tang decoction in rats. Biol. Pharm. Bull. 2003, 26, 911–919. [Google Scholar] [CrossRef]
- Chen, M.; Wei, S.; Luo, C.; Chen, F.; Song, S.; Shen, Q.; Mo, Z.; Wei, F. Simultaneous determination of wogonin, oroxylin a, schisandrin, paeoniflorin and emodin in rat serum by HPLC-MS/MS and application to pharmacokinetic studies. Biomed. Chromatogr. BMC 2017, 31. [Google Scholar] [CrossRef]
- Wang, L.; Shen, X.; Mi, L.; Jing, J.; Gai, S.; Liu, X.; Wang, Q.; Zhang, S. Simultaneous determinations of four major bioactive components in Acacia catechu (L.f.) Willd and Scutellaria baicalensis Georgi extracts by LC–MS/MS: Application to its herb–herb interactions based on pharmacokinetic, tissue distribution and excretion studies in rats. Phytomedicine 2019, 56, 64–73. [Google Scholar]
- Zhou, J.; Qu, F.; Yu, Y.; Nan, R. Whether co-administration of garlic has negative influence on Scutelaria baicalensis Georgi in treating models rats with pelvic inflammation? Afr. J. Tradit. Complement. Altern. Med. 2009, 6, 103–108. [Google Scholar]
- Kong, H.; Wang, X.; Wang, Q.; Zhao, Y.; Sun, Y.; Zhang, Y.; Xu, J.; Qu, H. Effect of Puerarin on the Pharmacokinetics of Baicalin in Gegen Qinlian Decoction in Mice. Chin. J. Integr. Med. 2018, 24, 525–530. [Google Scholar] [CrossRef]
- Wu, T.; Li, X.P.; Xu, Y.J.; Du, G.; Liu, D. Ursodeoxycholic acid pretreatment reduces oral bioavailability of the multiple drug resistance-associated protein 2 substrate baicalin in rats. Planta Med. 2013, 79, 1615–1619. [Google Scholar] [CrossRef]
- Ye, J.; Song, X.; Liu, Z.; Zhao, X.; Geng, L.; Bi, K.; Chen, X. Development of an LC–MS method for determination of three active constituents of Shuang-huang-lian injection in rat plasma and its application to the drug interaction study of Shuang-huang-lian freeze-dried powder combined with levofloxacin injection. J. Chromatogr. B 2012, 898, 130–135. [Google Scholar] [CrossRef]
- Zhou, J.; Qu, F.; Burrows, E.; Yu, Y.; Nan, R. Acupuncture can improve absorption of baicalin from extracts of Scutellaria baicalensis Georgi in rats. Phytother. Res. 2009, 23, 1415–1420. [Google Scholar] [CrossRef]
- Zhang, Y.; Zhang, Z.; Song, R. The Influence of Compatibility of Rhubarb and Radix Scutellariae on the Pharmacokinetics of Anthraquinones and Flavonoids in Rat Plasma. Eur. J. Drug Metab. Pharmacokinet. 2018, 43, 291–300. [Google Scholar] [CrossRef]
- Qiu, F.; He, Z.; Li, H. HPLC analyses and pharmacokinetic studies of baicalin and oxymatrine in rabbits. Pharmazie 2003, 58, 616–619. [Google Scholar]
- Di, B.; Feng, N.; Liu, W. Pharmacokinetic comparisons of Shuang-Huang-Lian with the different combinations of its constitutional herbs. J. Ethnopharmacol. 2006, 107, 401–405. [Google Scholar] [CrossRef]
- Zhu, Z.; Zhao, L.; Liu, X.; Chen, J.; Zhang, H.; Zhang, G.; Chai, Y. Comparative pharmacokinetics of baicalin and wogonoside by liquid chromatography-mass spectrometry after oral administration of Xiaochaihu Tang and Radix scutellariae extract to rats. J. Chromatogr. B Anal. Technol. Biomed. Life Sci. 2010, 878, 2184–2190. [Google Scholar] [CrossRef]
- Liang, X.L.; Zhang, J.; Zhao, G.W.; Li, Z.; Luo, Y.; Liao, Z.G.; Yan, D.M. Mechanisms of improvement of intestinal transport of baicalin and puerarin by extracts of Radix Angelicae Dahuricae. Phytother. Res. PTR 2015, 29, 220–227. [Google Scholar] [CrossRef]
- Yang, Y.F.; Li, Z.; Xin, W.F.; Wang, Y.Y.; Zhang, W.S. Pharmacokinetics and brain distribution differences of baicalin in rat underlying the effect of Panax notoginsenosides after intravenous administration. Chin. J. Nat. Med. 2014, 12, 632–640. [Google Scholar] [CrossRef]
- Shi, R.; Qiao, S.; Yu, D.; Shi, X.; Liu, M.; Jiang, X.; Wang, Q.; Zhang, L. Simultaneous determination of five flavonoids from Scutellaria Barbata extract in rat plasma by LC-MS/MS and its application to pharmacokinetic study. J. Chromatogr. B Anal. Technol. Biomed. Life Sci. 2011, 879, 1625–1632. [Google Scholar] [CrossRef]
- Li, M.; Shi, A.X.; Pang, H.X.; Xue, W.; Li, Y.; Cao, G.Y.; Yan, B.; Dong, F.; Xiao, W.; Du, G.H.; et al. Effect of food on the pharmacokinetic profile of baicalein chewable tablets in healthy volunteers. Chin. Pharm. J. 2015, 50, 163–166. [Google Scholar]
- Nishioka, Y.; Kyotani, S.; Miyamura, M.; Kusunose, M. Influence of time of administration of a Shosaiko-to extract granule on blood concentration of its active constituents. Chem. Pharm. Bull. 1992, 40, 1335–1337. [Google Scholar] [CrossRef]
- Yu, C.P.; Shia, C.S.; Tsai, S.Y.; Hou, Y.C. Pharmacokinetics and Relative Bioavailability of Flavonoids between Two Dosage Forms of Gegen-Qinlian-Tang in Rats. Evid. Based Complement. Altern. Med. ECAM 2012, 2012, 308018. [Google Scholar] [CrossRef]
- Zhang, Q.; Ma, Y.; Wang, Z.; Wang, C. Pharmacokinetics difference of multiple active constituents from decoction and maceration of Fuzi Xiexin Tang after oral administration in rat by UPLC-MS/MS. J. Pharm. Biomed. Anal. 2014, 92, 35–46. [Google Scholar] [CrossRef]
- Zhang, Q.; Ma, Y.; Wang, Z.; Wang, C. Differences in pharmacokinetics and anti-inflammatory effects between decoction and maceration of Sanhuang Xiexin Tang in rats and mice. Planta Med. 2013, 79, 1666–1673. [Google Scholar] [CrossRef]
- Cui, X.B.; Qian, X.C.; Huang, P.; Zhang, Y.X.; Li, J.S.; Yang, G.M.; Cai, B.C. Simultaneous determination of ten flavonoids of crude and wine-processed Radix Scutellariae aqueous extracts in rat plasma by UPLC-ESI-MS/MS and its application to a comparative pharmacokinetic study. Biomed. Chromatogr. BMC 2015, 29, 1112–1123. [Google Scholar] [CrossRef]
- Huang, P.; Tan, S.; Zhang, Y.; Li, J.; Chai, C.; Li, J.; Cai, B. The effects of wine-processing on ascending and descending: The distribution of flavonoids in rat tissues after oral administration of crude and wine-processed Radix scutellariae. J. Ethnopharmacol. 2014, 155, 649–664. [Google Scholar] [CrossRef]
- Huo, X.K.; Wang, B.; Zheng, L.; Cong, H.J.; Xiang, T.; Wang, S.M.; Sun, C.P.; Wang, C.; Zhang, L.; Deng, S.; et al. Comparative pharmacokinetic study of baicalin and its metabolites after oral administration of baicalin and Chaiqin Qingning capsule in normal and febrile rats. J. Chromatogr. B Anal. Technol. Biomed. Life Sci. 2017, 1059, 14–20. [Google Scholar] [CrossRef]
- Li, T.; Wang, Y.W.; Wang, Y.L.; Zhang, D.; Zhang, H.H.; Chen, L.; Zhuang, S.X.; Zhou, Z.M.; Yang, W.P. Pharmacokinetics and pharmacodynamics of huangqin tang in febrile rats. Yao Xue Xue Bao 2014, 49, 1418–1425. [Google Scholar]
- Liu, L.; Deng, Y.X.; Liang, Y.; Pang, X.Y.; Liu, X.D.; Liu, Y.W.; Yang, J.S.; Xie, L.; Wang, G.J. Increased oral AUC of baicalin in streptozotocin-induced diabetic rats due to the increased activity of intestinal beta-glucuronidase. Planta Med. 2010, 76, 70–75. [Google Scholar] [CrossRef]
- He, M.Y.; Deng, Y.X.; Shi, Q.Z.; Zhang, X.J.; Lv, Y. Comparative pharmacokinetic investigation on baicalin and wogonoside in type 2 diabetic and normal rats after oral administration of traditional Chinese medicine Huanglian Jiedu decoction. J. Ethnopharmacol. 2014, 155, 334–342. [Google Scholar] [CrossRef]
- Zhang, X.J.; Liu, S.; Xing, J.P.; Liu, Z.Q.; Song, F.R. Effect of type 2 diabetes mellitus on flavonoid pharmacokinetics and tissue distribution after oral administration of Radix Scutellaria extract in rats. Chin. J. Nat. Med. 2018, 16, 418–427. [Google Scholar] [CrossRef]
- Deng, Y.X.; Shi, Q.Z.; Chen, B.; Zhang, X.J.; Liu, S.Z.; Qiu, X.M. Comparative pharmacokinetics of baicalin in normal and the type 2 diabetic rats after oral administration of the Radix scutellariae extract. Fitoterapia 2012, 83, 1435–1442. [Google Scholar] [CrossRef]
- Xu, R.; Qi, J.; Zhan, R.J.; Zhou, G.S.; Hao, B.; Ma, J.; Wei, X.; Xu, A.J.; Zhang, J. Comparative pharmacokinetics of four active components on normal and diabetic rats after oral administration of Gandi capsules. RSC Adv. 2018, 8, 6620–6628. [Google Scholar] [CrossRef] [Green Version]
- Wei, X.Y.; Tao, J.H.; Cui, X.; Jiang, S.; Qian, D.W.; Duan, J.A. Comparative pharmacokinetics of six major bioactive components in normal and type 2 diabetic rats after oral administration of Sanhuang Xiexin Decoction extracts by UPLC-TQ MS/MS. J. Chromatogr. B Anal. Technol. Biomed. Life Sci. 2017, 1061–1062, 248–255. [Google Scholar] [CrossRef]
- Xu, J.; Zhao, M.; Qian, D.; Shang, E.; Jiang, S.; Guo, J.; Duan, J.; Du, L. Comparative metabolism of Radix scutellariae extract by intestinal bacteria from normal and type 2 diabetic mice in vitro. J. Ethnopharmacol. 2014, 153, 368–374. [Google Scholar] [CrossRef]
- Du, L.; Qian, D.; Shang, E.; Jiang, S.; Liu, P.; Guo, J.; Su, S.; Duan, J.; Xu, J.; Zhao, M. UPLC-MS based metabolite profiles of two major bioactive components in herb pair scutellaria-coptis metabolized by intestinal bacteria derived from healthy rats and rats with type 2 diabetes. Anal. Methods 2015, 7, 5574–5582. [Google Scholar] [CrossRef]
- Zhao, X.; Su, X.; Liu, C.; Jia, Y. Simultaneous Determination of Chrysin and Tectochrysin from Alpinia oxyphylla Fruits by UPLC-MS/MS and Its Application to a Comparative Pharmacokinetic Study in Normal and Dementia Rats. Molecules 2018, 23, 1702. [Google Scholar] [CrossRef]
- Baek, J.S.; Hwang, C.J.; Jung, H.W.; Park, Y.K.; Kim, Y.H.; Kang, J.S.; Cho, C.W. Comparative pharmacokinetics of a marker compound, baicalin in KOB extract after oral administration to normal and allergic-induced rats. Drug Deliv. 2014, 21, 453–458. [Google Scholar] [CrossRef] [Green Version]
- Zeng, M.; Pan, L.; Zhu, H.; Zhang, Q.; Guo, L. Comparative pharmacokinetics of baicalin in plasma after oral administration of Huang-Lian-Jie-Du-Tang or pure baicalin in MCAO and sham-operated rats. Fitoterapia 2010, 81, 490–496. [Google Scholar] [CrossRef]
- Li, N.; Feng, L.; Tan, Y.; Xiang, Y.; Zhang, R.; Yang, M. Preparation, Characterization, Pharmacokinetics and Biodistribution of Baicalin-Loaded Liposome on Cerebral Ischemia-Reperfusion after i.v. Administration in Rats. Molecules 2018, 23, 1747. [Google Scholar] [CrossRef]
- Ma, S.; Zhao, M.; Liu, H.; Wang, L.; Zhang, X. Pharmacokinetic Effects of Baicalin on Cerebral Ischemia-reperfusion after iv Administration in Rats. Chin. Herb. Med. 2012, 4, 53–57. [Google Scholar]
- Zhang, C.; Xu, Y.; Xiang, D.; Yang, J.; Lei, K.; Liu, D. Pharmacokinetic Characteristics of Baicalin in Rats with 17α-ethynyl-estradiol-induced Intrahepatic Cholestasis. Curr. Med. Sci. 2018, 38, 167–173. [Google Scholar] [CrossRef] [PubMed]
- Ling, X.; Xiang, Y.; Chen, F.; Tang, Q.; Zhang, W.; Tan, X. Intestinal absorption differences of major bioactive compounds of Gegenqinlian Decoction between normal and bacterial diarrheal mini-pigs in vitro and in situ. J. Chromatogr. B Anal. Technol. Biomed. Life Sci. 2018, 1083, 93–101. [Google Scholar] [CrossRef] [PubMed]
- Ling, X.; Xiang, Y.; Tang, Q.; Chen, F.; Tan, X. Comparative pharmacokinetics of eight major bioactive components in normal and bacterial diarrhea mini-pigs after oral administration of Gegen Qinlian Decoction. J. Chromatogr. B Anal. Technol. Biomed. Life Sci. 2017, 1044–1045, 132–141. [Google Scholar] [CrossRef] [PubMed]
- Ren, W.; Zuo, R.; Wang, Y.N.; Wang, H.J.; Yang, J.; Xin, S.K.; Han, L.Y.; Zhao, H.Y.; Han, S.Y.; Gao, B.; et al. Pharmacokinetic-Pharmacodynamic Analysis on Inflammation Rat Model after Oral Administration of Huang Lian Jie Du Decoction. PLoS ONE 2016, 11, e0156256. [Google Scholar] [CrossRef] [PubMed]
- Feng, S.X.; Li, X.H.; Wang, M.M.; Hao, R.; Li, M.M.; Zhang, L.; Wang, Z. A sensitive HPLC–MS method for simultaneous determination of thirteen components in rat plasma and its application to pharmacokinetic study of Tanreqing injection. J. Pharm. Biomed. Anal. 2018, 148, 205–213. [Google Scholar] [CrossRef] [PubMed]
- Walle, U.K.; Galijatovic, A.; Walle, T. Transport of the flavonoid chrysin and its conjugated metabolites by the human intestinal cell line Caco-2. Biochem. Pharmacol. 1999, 58, 431–438. [Google Scholar] [CrossRef]
- Ge, S.; Gao, S.; Yin, T.; Hu, M. Determination of pharmacokinetics of chrysin and its conjugates in wild-type FVB and Bcrp1 knockout mice using a validated LC-MS/MS method. J. Agric. Food Chem. 2015, 63, 2902–2910. [Google Scholar] [CrossRef] [PubMed]
- Noh, K.; Oh, D.G.; Nepal, M.R.; Jeong, K.S.; Choi, Y.; Kang, M.J.; Kang, W.; Jeong, H.G.; Jeong, T.C. Pharmacokinetic Interaction of Chrysin with Caffeine in Rats. Biomol. Ther. 2016, 24, 446–452. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, C.; Fong, S.Y.K.; Mei, Q.; Lin, G.; Zuo, Z. Influence of mefenamic acid on the intestinal absorption and metabolism of three bioactive flavones in Radix Scutellariae and potential pharmacological impact. Pharm. Biol. 2014, 52, 291–297. [Google Scholar] [CrossRef] [PubMed]
- Fong, S.Y.K.; Wong, Y.C.; Xie, C.; Zuo, Z. Herb-drug interactions between Scutellariae Radix and mefenamic acid: Simultaneous investigation of pharmacokinetics, anti-inflammatory effect and gastric damage in rats. J. Ethnopharmacol. 2015, 170, 106–116. [Google Scholar] [CrossRef] [PubMed]
- Dong, C.; Godwin, D.W.; Brennan, P.A.; Hegde, A.N. Protein kinase Calpha mediates a novel form of plasticity in the accessory olfactory bulb. Neuroscience 2009, 163, 811–824. [Google Scholar] [CrossRef] [PubMed]
- Yim, J.S.; Kim, Y.S.; Moon, S.K.; Cho, K.H.; Bae, H.S.; Kim, J.J.; Park, E.K.; Kim, D.H. Metabolic activities of ginsenoside Rb1, baicalin, glycyrrhizin and geniposide to their bioactive compounds by human intestinal microflora. Biol. Pharm. Bull. 2004, 27, 1580–1583. [Google Scholar] [CrossRef] [PubMed]
- Yang, G.; Ge, S.; Singh, R.; Basu, S.; Shatzer, K.; Zen, M.; Liu, J.; Tu, Y.; Zhang, C.; Wei, J.; et al. Glucuronidation: Driving factors and their impact on glucuronide disposition. Drug Metab. Rev. 2017, 49, 105–138. [Google Scholar] [CrossRef] [PubMed]
- Matsumoto, T.; Kaneko, A.; Koseki, J.; Matsubara, Y.; Aiba, S.; Yamasaki, K. Pharmacokinetic Study of Bioactive Flavonoids in the Traditional Japanese Medicine Keigairengyoto Exerting Antibacterial Effects against Staphylococcus aureus. Int. J. Mol. Sci. 2018, 19, 328. [Google Scholar] [CrossRef] [PubMed]
- Hu, M. Commentary: Bioavailability of flavonoids and polyphenols: Call to arms. Mol. Pharm. 2007, 4, 803–806. [Google Scholar] [CrossRef] [PubMed]



| Substance | Water Solubility |
|---|---|
| 5,7-dihydroxy-3-(3-methylbut-2-enyl)-flavone | 14.61 mg/L |
| 5,7-dihydroxy-3-[(2E)-5-methylhexa-2,4-dienyl]-flavone | 7.10 mg/L |
| 5,7-dimethoxyflavone | 0.016 g/L |
| 5-hydroxy-7-methoxy-3-methyl-flavone | 53.67 mg/L |
| 5-hydroxyflavone | 80.61 mg/L |
| 6,8-diprenyl-chrysin | 2.40 mg/L |
| 6-prenyl-chrysin | 13.66 mg/L |
| 7-hydroxyflavone | 84.92 mg/L |
| Alnetin | 28.80 mg/L |
| Baicalein | 0.15 g/L |
| Baicalin | 1.72 g/L |
| BA-j | 15.92 mg/L |
| Chrysin (5,7-dihydroxyflavone) | 0.1 g/L |
| Chrysin-5-methyl-ether | 51.66 mg/L |
| GL-V9 | 18.25 mgL |
| Mosloflavone | 40.04 mg/L |
| Moslosooflavone | 37.09 mg/L |
| Negletein | 66.94 mg/L |
| Norwogonin | 0.16 g/L |
| Oroxylin A | 66.60 mg/L |
| Oroxylin A-7-glucuronide | 1.20 g/L |
| Pediflavone (isowogonin) | 69.01 mg/L |
| Primetin | 0.11 g/L |
| Tectochrysin | 52.22 mg/L |
| Wogonin | 65.34 mg/L |
| Wogonin-7-glucuronide | 1.21 g/L |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ancuceanu, R.; Dinu, M.; Dinu-Pirvu, C.; Anuţa, V.; Negulescu, V. Pharmacokinetics of B-Ring Unsubstituted Flavones. Pharmaceutics 2019, 11, 370. https://0-doi-org.brum.beds.ac.uk/10.3390/pharmaceutics11080370
Ancuceanu R, Dinu M, Dinu-Pirvu C, Anuţa V, Negulescu V. Pharmacokinetics of B-Ring Unsubstituted Flavones. Pharmaceutics. 2019; 11(8):370. https://0-doi-org.brum.beds.ac.uk/10.3390/pharmaceutics11080370
Chicago/Turabian StyleAncuceanu, Robert, Mihaela Dinu, Cristina Dinu-Pirvu, Valentina Anuţa, and Vlad Negulescu. 2019. "Pharmacokinetics of B-Ring Unsubstituted Flavones" Pharmaceutics 11, no. 8: 370. https://0-doi-org.brum.beds.ac.uk/10.3390/pharmaceutics11080370