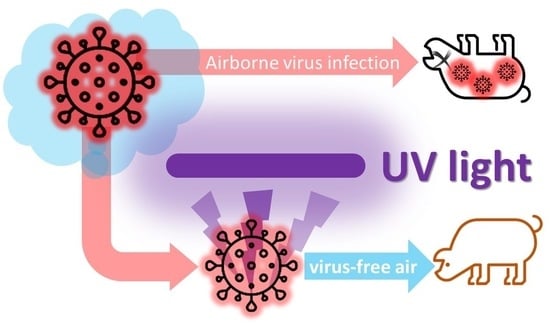
Mitigation of Airborne PRRSV Transmission with UV Light Treatment: Proof-of-Concept
Abstract
:1. Introduction
- Quantify and compare the inactivation of aerosolized PRRSV by UV-C germicidal (254 nm), UV-C “excimer” (222 nm), UV-A fluorescent (365 nm), and UV-A LED (365 nm).
- Estimate the UV-A and UV-C dose needed for 90, 99, and 99.9% reduction in infectious aerosolized PRRSV.
- Evaluate the techno-economic feasibility of UV treatment for airborne PRRSV in a swine barn inlet air.
2. Materials and Methods
2.1. Experiment Overview (Obj. 1)
2.2. PRRSV Propagation and Aerosolization (Preparation for Obj. 1)
2.3. UV Light Selections and Measurements (Obj. 1)
2.3.1. UV Light Selections
2.3.2. UV Light Intensity Measurement
2.4. UV Treatment of Aerosolized PRRSV
2.5. Post-UV-Irradiation Aerosol Collection, Recovery, and PRRSV Titer Calculation (Obj. 1)
2.6. UV Inactivation Models (Obj. 2)
- 1 − f = the fraction of the virus population that is more susceptible to UV treatment with an inactivation rate ;
- f = the fraction of the virus population that is more resistant to UV treatment with an inactivation rate ;
- k1 = inactivation rate for the susceptible fraction of the virus population under UV treatment;
- k2 = inactivation rate for the resistant fraction of the virus population under UV treatment;
- C2 = intercept for the two-stage model.
3. Results
3.1. Effectiveness of UV to Treat Airborne PRRSV (Obj. 1)
3.2. Estimations of UV Dose Needed for 90, 99, and 99.9% Airborne PRRSV Reduction (Obj. 2)
3.3. Preliminary Techno-Economic Analysis of Potential Farm-Scale Application (Obj. 3)
4. Discussion
4.1. UV Effectiveness and Inactivation Models
4.2. Exploring the UV Inactivation Mechanism
4.3. Techno-Economic Analysis
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A




Appendix B





References
- Terpstra, C.; Wensvoort, G.; Pol, J.M.A. Experimental reproduction of PEARS (mystery swine disease) by infection with Lelystad virus: Koch’s postulates fulfilled. Vet. Q. 1991, 13, 131–136. [Google Scholar] [CrossRef] [PubMed]
- Wensvoort, G.; Terpstra, C.; Pol, J.M.A.; ter Laak, E.A.; Bloemraad, M.; de Kluyver, E.P.; Kragten, C.; van Buiten, L.; den Besten, A.; Wagenaar, F. Mystery swine disease in the Netherlands: The isolation of Lelystad virus. Vet. Q. 1991, 13, 121–130. [Google Scholar] [CrossRef]
- Neumann, E.J.; Kliebenstein, J.B.; Johnson, C.D.; Mabry, J.W.; Bush, E.J.; Seitzinger, A.H.; Green, A.L.; Zimmerman, J.J. Assessment of the economic impact of porcine reproductive and respiratory syndrome on swine production in the United States. J. Am. Vet. Med Assoc. 2005, 227, 385–392. [Google Scholar] [CrossRef]
- Holtkamp, D.J.; Kliebenstein, J.B.; Zimmerman, J.J.; Neumann, E.; Rotto, H.; Yoder, T.K.; Johnson, C.D.; Mabry, J.W.; Bush, E.J.; Seitzinger, A.H. Assessment of the economic impact of porcine reproductive and respiratory syndrome virus on us pork producers. J. Swine Health Prod. 2013, 21, 72–84. [Google Scholar] [CrossRef]
- Miller, M. Pork Checkoff Report; Pork Checkoff: Des Moines, IA, USA, 2017; pp. 38–39. [Google Scholar]
- Nathues, H.; Alarcon, P.; Rushton, J.; Jolie, R.; Fiebig, K.; Jimenez, M.; Geurts, V.; Nathues, C. Cost of porcine reproductive and respiratory syndrome virus at individual farm level—An economic disease model. Prev. Vet. Med. 2017, 142, 16–29. [Google Scholar] [CrossRef]
- Lager, K.M.; Mengeling, W.L. Experimental aerosol transmission of pseudorabies virus and porcine reproductive and respiratory syndrome virus. In Proceedings of the American Association of Swine Practitioners 2000 Annual Meeting (AASP), Indianapolis, IN, USA, 22–24 June 2000; pp. 409–410. [Google Scholar]
- Otake, S.; Dee, S.A.; Jacobson, L.; Pijoan, C.; Torremorell, M. Evaluation of aerosol transmission of porcine reproductive and respiratory syndrome virus under controlled field conditions. Vet. Rec. 2002, 150, 804–808. [Google Scholar] [CrossRef]
- Torremorell, M.; Pijoan, C.; Janni, K.; Walker, R.; Joo, H.S. Airborne transmission of Actinobacillus pleuropneumoniae and porcine reproductive and respiratory syndrome virus in nursery pigs. Am. J. Vet. Res. 1997, 58, 828–832. [Google Scholar] [PubMed]
- Wills, R.W.; Zimmerman, J.J.; Swenson, S.L.; Yoon, K.J.; Hill, H.T.; Bundy, D.S.; McGinley, M.J. Transmission of PRRSV by direct, close, or indirect contact. J. Swine Health Prod. 1997, 5, 213–218. [Google Scholar]
- Dee, S.; Otake, S.; Oliveira, S.; Deen, J. Evidence of long-distance airborne transport of porcine reproductive and respiratory syndrome virus and Mycoplasma hyopneumoniae. Vet. Res. 2009, 40, 39. [Google Scholar] [CrossRef]
- Otake, S.; Dee, S.; Corzo, C.; Oliveira, S.; Deen, J. Long-distance airborne transport of infectious PRRSV and Mycoplasma hyopneumoniae from a swine population infected with multiple viral variants. Vet. Microbiol. 2010, 145, 198–208. [Google Scholar] [CrossRef]
- La, A.; Zhang, Q.; Levin, D.B.; Coombs, K.M. The effectiveness of air ionization in reducing bioaerosols and airborne prrs virus in a ventilated space. Trans. ASABE 2019, 62, 1299–1314. [Google Scholar] [CrossRef]
- Xia, T.; Lin, Z.; Lee, E.M.; Melotti, K.; Rohde, M.; Clack, H.L. Field operations of a pilot scale packed-bed non-thermal plasma (ntp) reactor installed at a pig barn on a Michigan farm to inactivate airborne viruses. In Proceedings of the Industry Applications Society Annual Meeting (IEEE), Baltimore, MD, USA, 29 September–3 October 2019; pp. 1–4. [Google Scholar]
- Dee, S.; Otake, S.; Deen, J. An evaluation of ultraviolet light (UV254) as a means to inactivate porcine reproductive and respiratory syndrome virus on common farm surfaces and materials. Vet. Microbiol. 2011, 150, 96–99. [Google Scholar] [CrossRef] [PubMed]
- Nan, Y.; Wu, C.; Gu, G.; Sun, W.; Zhang, Y.-J.; Zhou, E.-M. Improved Vaccine against PRRSV: Current Progress and Future Perspective. Front. Microbiol. 2017, 8. [Google Scholar] [CrossRef]
- Dee, S.; Joo, H. Prevention of the spread of porcine reproductive and respiratory syndrome virus in endemically infected pig herds by nursery depopulation. Vet. Rec. 1994, 135, 6–9. [Google Scholar] [CrossRef]
- Dee, S.; Batista, L.; Deen, J.; Pijoan, C. Evaluation of an air-filtration system for preventing aerosol transmission of porcine reproductive and respiratory syndrome virus. Can. J. Vet. Res. 2005, 69, 293–298. [Google Scholar] [PubMed]
- Dee, S.; Otake, S.; Deen, J. Use of a production region model to assess the efficacy of various air filtration systems for preventing airborne transmission of porcine reproductive and respiratory syndrome virus and Mycoplasma hyopneumoniae: Results from a 2-year study. Virus Res. 2010, 154, 177–184. [Google Scholar] [CrossRef] [PubMed]
- Bolton, J.R.; Cotton, C.A. The Ultraviolet Disinfection Handbook; AWWA: Denver, CO, USA, 2008. [Google Scholar]
- Holtkamp, D.J.; Johnson, C.; Koziel, J.A.; Li, P.; Murray, D.; Ruston, C.R.; Stephan, A.; Torremorell, M.; Wedel, K. Ultraviolet C (UVC) Standards and Best Practices for the Swine Industry. Agricultural and Biosystems Engineering Technical Reports and White Papers, 2020, 29. Available online: https://lib.dr.iastate.edu/abe_eng_reports/29 (accessed on 6 March 2021).
- Cutler, T.D.; Wang, C.; Hoff, S.J.; Zimmerman, J.J. Effect of temperature and relative humidity on ultraviolet (UV254) inactivation of airborne porcine respiratory and reproductive syndrome virus. Vet. Microbiol. 2012, 159, 47–52. [Google Scholar] [CrossRef] [PubMed]
- Cutler, T.; Wang, C.; Qin, Q.; Zhou, F.; Warren, K.; Yoon, K.-J.; Hoff, S.J.; Ridpath, J.; Zimmerman, J. Kinetics of UV254 inactivation of selected viral pathogens in a static system. J. Appl. Microbiol. 2011, 111, 389–395. [Google Scholar] [CrossRef]
- Buonanno, M.; Ponnaiya, B.; Welch, D.; Stanislauskas, M.; Randers-Pehrson, G.; Smilenov, L.; Lowy, F.D.; Owens, D.M.; Brenner, D.J. Germicidal efficacy and mammalian skin safety of 222-nm UV light. Radiat. Res. 2017, 187, 493–501. [Google Scholar] [CrossRef]
- Welch, D.; Buonanno, M.; Grilj, V.; Shuryak, I.; Crickmore, C.; Bigelow, A.W.; Randers-Pehrson, G.; Johnson, G.W.; Brenner, D.J. Far-UVC light: A new tool to control the spread of airborne-mediated microbial diseases. Sci. Rep. 2018, 8, 2752. [Google Scholar] [CrossRef]
- Yang, X.; Koziel, J.A.; Laor, Y.; Zhu, W.; van Leeuwen, J.; Jenks, W.S.; Hoff, S.J.; Zimmerman, J.; Zhang, S.; Ravid, U.; et al. VOC Removal from manure gaseous emissions with UV photolysis and UV-TiO2 photocatalysis. Catalysts 2020, 10, 607. [Google Scholar] [CrossRef]
- Lee, M.; Koziel, J.A.; Murphy, W.; Jenks, W.S.; Fonken, B.; Storjohann, R.; Chen, B.; Li, P.; Banik, C.; Wahe, L.; et al. Design and testing of mobile laboratory for mitigation of gaseous emissions from livestock agriculture with photocatalysis. Int. J. Environ. Res. Public Health 2021, 18, 1523. [Google Scholar] [CrossRef]
- Lee, M.; Li, P.; Koziel, J.A.; Ahn, H.; Wi, J.; Chen, B.; Meiirkhanuly, Z.; Banik, C.; Jenks, W.S. Pilot-scale testing of UV-A light treatment for mitigation of NH3, H2S, GHGs, VOCs, Odor, and O3 inside the poultry barn. Front. Chem. 2020, 8, 613. [Google Scholar] [CrossRef] [PubMed]
- Lee, M.; Wi, J.; Koziel, J.A.; Ahn, H.; Li, P.; Chen, B.; Meiirkhanuly, Z.; Banik, C.; Jenks, W. Effects of UV-A light treatment on Ammonia, Hydrogen Sulfide, Greenhouse Gases, and Ozone in simulated poultry barn conditions. Atmosphere 2020, 11, 283. [Google Scholar] [CrossRef]
- Maurer, D.; Koziel, J.A. On-farm pilot-scale testing of black ultraviolet light and photocatalytic coating for mitigation of odor, odorous VOCs, and greenhouse gases. Chemosphere 2019, 221, 778–784. [Google Scholar] [CrossRef] [PubMed]
- Zhu, W.; Koziel, J.A.; Maurer, D.L. Mitigation of livestock odors using black light and a new titanium dioxide-based catalyst: Proof-of-concept. Atmosphere 2017, 8, 103. [Google Scholar] [CrossRef]
- Li, P.; Koziel, J.A.; Zimmerman, J.; Hoff, S.; Zhang, J.; Cheng, T.; Yim-Im, W.; Lee, M.; Chen, B.; Jenks, W. Designing and testing of a system for aerosolization and recovery of viable porcine reproductive and respiratory syndrome virus (PRRSV): Theoretical and engineering considerations. Preprints 2021. [Google Scholar] [CrossRef]
- Koziel, J.A.; Zimmerman, J.J.; Jenks, W.S.; Hoff, S. Mitigation of PRRS transmission with UV light treatment of barn inlet air: Proof-of-concept. National Pork Board Des Moines IA 2020, 18–160. [Google Scholar] [CrossRef]
- Kim, H.S.; Kwang, J.; Yoon, I.J.; Joo, H.S.; Frey, M.L. Enhanced replication of porcine reproductive and respiratory syndrome (PRRS) virus in a homogeneous subpopulation of MA-104 cell line. Arch. Virol. 1993, 133, 477–483. [Google Scholar] [CrossRef]
- Hermann, J.R.; Hoff, S.J.; Yoon, K.J.; Burkhardt, A.C.; Evans, R.B.; Zimmerman, J.J. Optimization of a sampling system for recovery and detection of airborne porcine reproductive and respiratory syndrome virus and swine influenza virus. Appl. Environ. Microbiol. 2006, 72, 4811–4818. [Google Scholar] [CrossRef]
- Hamilton, M.A.; Russo, R.C.; Thurston, R.V. Trimmed Spearman-Karber method for estimating median lethal concentrations in toxicity bioassays. Environ. Sci. Technol. 1977, 11, 714–719. [Google Scholar] [CrossRef]
- Mc Auslan, B.R. Techniques in experimental virology. In Science; Harris, R.J.G., Ed.; Academic Press: New York, NY, USA, 1964; Volume 148, pp. 183–186. [Google Scholar]
- Karber, G. Beitrag zur kollektiven Behandlung pharmakologischer Reihenversuche. Naunyn-Schmiedebergs Arch. Exp. Pathol. Pharmakol. 1931, 162, 480–483. [Google Scholar] [CrossRef]
- Fox, J.; Weisberg, S. An R Companion to Applied Regression, 3rd ed.; Sage Publishers: Thousand Oaks, CA, USA, 2019; Available online: https://socialsciences.mcmaster.ca/jfox/Books/Companion (accessed on 6 March 2021).
- Elzhov, T.V.; Mullen, K.M.; Spiess, A.-N.; Bolker, B. minpack.lm: R Interface to the Levenberg-Marquardt Nonlinear Least-Squares Algorithm Found in MINPACK, Plus Support for Bounds. R Package Version 1.2-1. 2016. Available online: https://CRAN.R-project.org/package=minpack.lm (accessed on 6 March 2021).
- Pinheiro, J.; Bates, D.; DebRoy, S.; Sarkar, D. nlme: Linear and Nonlinear Mixed Effects Models. R Package Version 3.1-152. R Core Team, 2021. Available online: https://cran.r-project.org/web/packages/nlme/index.html (accessed on 6 March 2021).
- Kowalski, W.J.; Bahnfleth, W.P.; Witham, D.L.; Severin, B.F.; Whittam, T.S. Mathematical modeling of ultraviolet germicidal irradiation for air disinfection. Quant. Microbiol. 2000, 2, 249–270. [Google Scholar] [CrossRef]
- Riley, R.L.; Kaufman, J.E. Effect of relative humidity on the inactivation of airborne serratia marcescens by ultraviolet radiation. Appl. Microbiol. 1972, 23, 1113–1120. [Google Scholar] [CrossRef] [PubMed]
- Midwest Plan Service. Swine Housing and Equipment Handbook, 4th ed.; MWPS-8 Iowa State University: Ames, IA, USA, 1983. [Google Scholar]
- Stephan, A.B. Reduction in Swine Pathogen Numbers by a UVC Germicidal Chamber. Available online: https://www.nationalhogfarmer.com/animal-health/reduction-swine-pathogen-numbers-uvc-germicidal-chamber (accessed on 9 February 2021).
- Sinha, R.P.; Häder, D.-P. UV-induced DNA damage and repair: A review. Photochem. Photobiol. Sci. 2002, 1, 225–236. [Google Scholar] [CrossRef] [PubMed]
- Miller, R.L.; Plagemann, P.G. Effect of ultraviolet light on mengovirus: Formation of uracil dimers, instability and degradation of capsid, and covalent linkage of protein to viral RNA. J. Virol. 1974, 13, 729–739. [Google Scholar] [CrossRef] [PubMed]
- Sauerbier, W.; Hercules, K. Gene and transcription unit mapping by radiation effects. Annu. Rev. Genet. 1978, 12, 329–363. [Google Scholar] [CrossRef]
- Delrue, I.; Verzele, D.; Madder, A.; Nauwynck, H.J. Inactivated virus vaccines from chemistry to prophylaxis: Merits, risks and challenges. Expert Rev. Vaccines 2012, 11, 695–719. [Google Scholar] [CrossRef] [PubMed]
- Alonso, C.; Murtaugh, M.P.; Dee, S.A.; Davies, P.R. Epidemiological study of air filtration systems for preventing PRRSV infection in large sow herds. Prev. Vet. Med. 2013, 112, 109–117. [Google Scholar] [CrossRef] [PubMed]





| UV Light Intensity (mW/cm2) | ||||
|---|---|---|---|---|
| UV-C (254 nm) | UV-C (222 nm) | UV-A (365 nm, Fluorescent) | UV-A (365 nm, LED) | |
| Treatment 1 * | 3.43 | 1.10 | 0.57 | 1.71 |
| Treatment 2 | 4.40 | 1.36 | 0.70 | 1.93 |
| Treatment 3 | 5.04 | 1.49 | 0.77 | 2.00 |
| Treatment 4 | 5.35 | 1.49 | 0.80 | 2.02 |
| Treatment 5 | 5.35 | 1.41 | 0.79 | 2.01 |
| Treatment 6 | 5.06 | 1.33 | 0.74 | 1.99 |
| Treatment 7 | 4.53 | 1.19 | 0.66 | 1.90 |
| Treatment 8 | 3.57 | 1.04 | 0.49 | 1.66 |
| UV Types | UV-C (254 nm) | UV-C Excimer (222 nm) | UV-A (365 nm, Fluorescent) | UV-A (365 nm, LED) | |
|---|---|---|---|---|---|
| Parameters | |||||
| Two-stage inactivation model | |||||
| Intercept | −0.02367 | 0.0775 | 0.012422 | −0.02748 | |
| Susceptible virus population fraction (f) | 0.9675 | 0.9951 | 0.57417 | 1.72542 | |
| Resistant virus population fraction (1 − f) | 0.0325 | 0.0049 | 0.42583 | −0.72542 | |
| Inactivation rate (constant), , for resistant virus population (cm2/mJ) | 0.01927 | 0.3014 | −0.13585 | 0.88296 | |
| Inactivation rate (constant), , for susceptible virus population (cm2/mJ) | −0.58947 | −1.9189 | 2.89537 | 0.02075 | |
| Lack-of-fit test p-value | p = 0.8488 | p = 0.6565 | p = 0.2848 | p = 0.6532 | |
| One-stage inactivation model | |||||
| Intercept | −0.4601 | −0.1779 | −0.09103 | 0.08388 | |
| Inactivation rate, k (cm2/mJ) | −0.1307 | −1.0053 | 0.01556 | −0.02183 | |
| Lack-of-fit test p-value | p = 0.0153 | p = 0.01344 | p = 0.3336 | p = 0.7748 | |
| 90% (1-log) Reduction | 99% (2-log) Reduction | 99.9% (3-log) Reduction | ||||
|---|---|---|---|---|---|---|
| 1-Stage | 2-Stage | 1-Stage | 2-Stage | 1-Stage | 2-Stage | |
| UV-C (254 nm) | 4.131 | 1.933 | 11.782 | 2.662 | 19.433 a | 2.442 |
| UV-C (222 nm) | 0.818 | 0.581 | 1.812 | 1.036 | 2.807 | 1.044 |
| UV-A (365 nm, fluor.) | 58.42 | - | 122.684 | - | 186.952 | - |
| UV-A (365 nm, LED) | −49.651 b | 58.285 | −95.460 b | 106.478 | −141.268 b | 154.671 |
| UV Light | Measured Power Consumption (W) a | Electricity Consumption (kWh) b | Electricity Cost c | Cost of UV Lamps d |
|---|---|---|---|---|
| UV-C (254 nm) | 50.5 | 0.038 | USD 0.0023 | <USD 100 |
| UV-C (222 nm) | 250 | 0.19 | USD 0.0122 | ~USD 600 |
| UV-A (365 nm, fluor.) | 49.5 | 0.037 | USD 0.0022 | <USD 100 |
| UV-A (365 nm, LED) | 43.8 | 0.033 | USD 0.0019 | ~USD 200 e |
| Type | Capital Cost (Hot Weather a) | 1-Year Electricity Cost (Mixed Weather a) | Maintenance | Total Cost |
|---|---|---|---|---|
| UV light with pre-filters | USD 66,000 | USD 35,000 | USD 6600 | USD 107,600 |
| HEPA filters with pre-filters | USD 80,400 | N/A | USD 8040 | USD 88,440 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Li, P.; Koziel, J.A.; Zimmerman, J.J.; Zhang, J.; Cheng, T.-Y.; Yim-Im, W.; Jenks, W.S.; Lee, M.; Chen, B.; Hoff, S.J. Mitigation of Airborne PRRSV Transmission with UV Light Treatment: Proof-of-Concept. Agriculture 2021, 11, 259. https://0-doi-org.brum.beds.ac.uk/10.3390/agriculture11030259
Li P, Koziel JA, Zimmerman JJ, Zhang J, Cheng T-Y, Yim-Im W, Jenks WS, Lee M, Chen B, Hoff SJ. Mitigation of Airborne PRRSV Transmission with UV Light Treatment: Proof-of-Concept. Agriculture. 2021; 11(3):259. https://0-doi-org.brum.beds.ac.uk/10.3390/agriculture11030259
Chicago/Turabian StyleLi, Peiyang, Jacek A. Koziel, Jeffrey J. Zimmerman, Jianqiang Zhang, Ting-Yu Cheng, Wannarat Yim-Im, William S. Jenks, Myeongseong Lee, Baitong Chen, and Steven J. Hoff. 2021. "Mitigation of Airborne PRRSV Transmission with UV Light Treatment: Proof-of-Concept" Agriculture 11, no. 3: 259. https://0-doi-org.brum.beds.ac.uk/10.3390/agriculture11030259