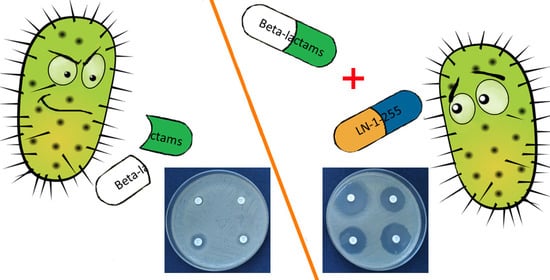
Activity of Imipenem, Meropenem, Cefepime, and Sulbactam in Combination with the β-Lactamase Inhibitor LN-1-255 against Acinetobacter spp.
Abstract
:1. Introduction
2. Results and Discussion
2.1. Carbapenems/LN-1-255
2.2. Cefepime/LN-1-255
2.3. Sulbactam/LN-1-255
3. Materials and Methods
3.1. Bacterial Isolates
3.2. Antimicrobial Susceptibility Testing
3.3. Multiplex PCR Assay
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Joly-Guillou, M.-L. Clinical impact and pathogenicity of Acinetobacter. Clin. Microbiol. Infect. 2005, 11, 868–873. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lupo, A.; Haenni, M.; Madec, J.-Y. Antimicrobial Resistance in Acinetobacter spp. and Pseudomonas spp. Antimicrob. Resist. Bact. Livest. Companion Anim. 2018, 6, 377–393. [Google Scholar] [CrossRef]
- Murray, G.L.; Peleg, A.Y.; Doi, Y. Acinetobacter baumannii: Evolution of Antimicrobial Resistance—Treatment Options. Semin. Respir. Crit. Care Med. 2015, 36, 85–98. [Google Scholar] [CrossRef] [Green Version]
- Pérez, A.; Pérez-Llarena, F.J.; García, P.; Kerff, F.; Beceiro, A.; Galleni, M.; Bou, G. New mutations in ADC-type β-lactamases from Acinetobacter spp. affect cefoxitin and ceftazidime hydrolysis. J. Antimicrob. Chemother. 2014, 69, 2407–2411. [Google Scholar] [CrossRef] [Green Version]
- Urban, C.; Go, E.; Mariano, N.; Rahal, J.J. Interaction of sulbactam, clavulanic acid and tazobactam with penicillin-binding proteins of imipenem-resistant and -susceptible acinetobacter baumannii. FEMS Microbiol. Lett. 1995, 125, 193–197. [Google Scholar] [CrossRef]
- Mendes, R.E.; Bell, J.M.; Turnidge, J.D.; Castanheira, M.; Jones, R.N. Emergence and widespread dissemination of OXA-23, -24/40 and -58 carbapenemases among Acinetobacter spp. in Asia-Pacific nations: Report from the SENTRY Surveillance Program. J. Antimicrob. Chemother. 2008, 63, 55–59. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rumbo, C.; Gato, E.; López, M.; De Alegría, C.R.; Fernández-Cuenca, F.; Martínez-Martínez, L.; Vila, J.; Pachón, J.; Cisneros, J.M.; Rodríguez-Baño, J.; et al. Contribution of Efflux Pumps, Porins, and β-Lactamases to Multidrug Resistance in Clinical Isolates of Acinetobacter baumannii. Antimicrob. Agents Chemother. 2013, 57, 5247–5257. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Viehman, J.A.; Nguyen, M.-H.; Doi, Y. Treatment Options for Carbapenem-Resistant and Extensively Drug-Resistant Acinetobacter baumannii Infections. Drugs 2014, 74, 1315–1333. [Google Scholar] [CrossRef] [Green Version]
- Tian, G.-B.; Adams-Haduch, J.M.; A Taracila, M.; Bonomo, R.A.; Wang, H.-N.; Doi, Y. Extended-Spectrum AmpC Cephalosporinase in Acinetobacter baumannii: ADC-56 Confers Resistance to Cefepime. Antimicrob. Agents Chemother. 2011, 55, 4922–4925. [Google Scholar] [CrossRef] [Green Version]
- Endimiani, A.; Perez, F.; A Bonomo, R. Cefepime: A reappraisal in an era of increasing antimicrobial resistance. Expert Rev. Anti-Infect. Ther. 2008, 6, 805–824. [Google Scholar] [CrossRef]
- Yang, Y.; Xu, Q.; Li, T.; Fu, Y.; Shi, Y.; Lan, P.; Zhao, D.; Chen, Q.; Zhou, Z.; Jiang, Y.; et al. OXA-23 Is a Prevalent Mechanism Contributing to Sulbactam Resistance in Diverse Acinetobacter baumannii Clinical Strains. Antimicrob. Agents Chemother. 2018, 63, 1–4. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yang, Y.; Fu, Y.; Lan, P.; Xu, Q.; Jiang, Y.; Chen, Y.; Ruan, Z.; Ji, S.; Hua, X.; Yu, Y. Molecular Epidemiology and Mechanism of Sulbactam Resistance in Acinetobacter baumannii Isolates with Diverse Genetic Backgrounds in China. Antimicrob. Agents Chemother. 2018, 62, e01947-17. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fernández-Cuenca, F.; Martínez-Martínez, L.; Conejo, M.C.; Ayala, J.A.; Perea, E.J.; Pascual, A. Relationship between beta-lactamase production, outer membrane protein and penicillin-binding protein profiles on the activity of carbapenems against clinical isolates of Acinetobacter baumannii. J. Antimicrob. Chemother. 2003, 51, 565–574. [Google Scholar] [CrossRef] [Green Version]
- Karlowsky, J.A.; Kazmierczak, K.M.; Bouchillon, S.K.; De Jonge, B.L.M.; Stone, G.G.; Sahm, D.F. In Vitro Activity of Ceftazidime-Avibactam against Clinical Isolates of Enterobacteriaceae and Pseudomonas aeruginosa Collected in Asia-Pacific Countries: Results from the INFORM Global Surveillance Program, 2012 to 2015. Antimicrob. Agents Chemother. 2018, 62, 02569-17. [Google Scholar] [CrossRef] [Green Version]
- Bush, K.; Jacoby, G.A.; Medeiros, A.A. A functional classification scheme for beta-lactamases and its correlation with molecular structure. Antimicrob. Agents Chemother. 1995, 39, 1211–1233. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tooke, C.L.; Hinchliffe, P.; Bragginton, E.C.; Colenso, C.K.; Hirvonen, V.H.; Takebayashi, Y.; Spencer, J. β-Lactamases and β-Lactamase Inhibitors in the 21st Century. J. Mol. Biol. 2019, 431, 3472–3500. [Google Scholar] [CrossRef] [PubMed]
- González-Bello, C.; Rodríguez, D.; Pernas, M.; Rodríguez, Á.; Colchón, E. β-Lactamase Inhibitors to Restore the Efficacy of Antibiotics against Superbugs. J. Med. Chem. 2020, 63, 1859–1881. [Google Scholar] [CrossRef]
- Shapiro, A.B.; Gao, N.; Jahić, H.; Carter, N.M.; Chen, A.; Miller, A.A. Reversibility of Covalent, Broad-Spectrum Serine β-Lactamase Inhibition by the Diazabicyclooctenone ETX2514. ACS Infect. Dis. 2017, 3, 833–844. [Google Scholar] [CrossRef] [PubMed]
- Tsivkovski, R.; Totrov, M.; Lomovskaya, O. Biochemical Characterization of QPX7728, a New Ultrabroad-Spectrum Beta-Lactamase Inhibitor of Serine and Metallo-Beta-Lactamases. Antimicrob. Agents Chemother. 2020, 64, 00130-20. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Drawz, S.M.; Bethel, C.R.; Doppalapudi, V.R.; Sheri, A.; Pagadala, S.R.R.; Hujer, A.M.; Skalweit, M.J.; Anderson, V.E.; Chen, S.G.; Buynak, J.D.; et al. Penicillin Sulfone Inhibitors of Class D β-Lactamases. Antimicrob. Agents Chemother. 2010, 54, 1414–1424. [Google Scholar] [CrossRef] [Green Version]
- Rodríguez, D.; Maneiro, M.; Vázquez-Ucha, J.C.; Beceiro, A.; González-Bello, C. 6-Arylmethylidene Penicillin-Based Sulfone Inhibitors for Repurposing Antibiotic Efficiency in Priority Pathogens. J. Med. Chem. 2020, 63, 3737–3755. [Google Scholar] [CrossRef] [PubMed]
- Vázquez-Ucha, J.C.; Maneiro, M.; Martínez-Guitián, M.; Buynak, J.; Bethel, C.R.; Bonomo, R.A.; Bou, G.; Poza, M.; González-Bello, C.; Beceiro, A. Activity of the β-Lactamase Inhibitor LN-1-255 against Carbapenem-Hydrolyzing Class D β-Lactamases from Acinetobacter baumannii. Antimicrob. Agents Chemother. 2017, 61, 1–17. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vázquez-Ucha, J.C.; Martínez-Guitián, M.; Maneiro, M.; Conde-Pérez, K.; Álvarez-Fraga, L.; Torrens, G.; Oliver, A.; Buynak, J.D.; Bonomo, R.A.; Bou, G.; et al. Therapeutic Efficacy of LN-1-255 in Combination with Imipenem in Severe Infection Caused by Carbapenem-Resistant Acinetobacter baumannii. Antimicrob. Agents Chemother. 2019, 63, 1–12. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nelson, K.; Rubio-Aparicio, D.; Tsivkovski, R.; Sun, D.; Totrov, M.; Dudley, M.; Lomovskaya, O. In Vitro Activity of the Ultra-Broad-Spectrum Beta-lactamase Inhibitor QPX7728 in Combination with Meropenem against Clinical Isolates of Carbapenem-Resistant Acinetobacter baumannii. Antimicrob. Agents Chemother. 2020, 1–31. [Google Scholar] [CrossRef]
- Lob, S.H.; Hackel, M.A.; Kazmierczak, K.M.; Young, K.; Motyl, M.R.; Karlowsky, J.A.; Sahm, D.F. In Vitro Activity of Imipenem-Relebactam against Gram-Negative ESKAPE Pathogens Isolated by Clinical Laboratories in the United States in 2015 (Results from the SMART Global Surveillance Program). Antimicrob. Agents Chemother. 2017, 61, e02209-16. [Google Scholar] [CrossRef] [Green Version]
- A Karlowsky, J.; Lob, S.H.; Kazmierczak, K.M.; Hawser, S.P.; Magnet, S.; Young, K.; Motyl, M.R.; Sahm, D.F. In vitro activity of imipenem/relebactam against Gram-negative ESKAPE pathogens isolated in 17 European countries: 2015 SMART surveillance programme. J. Antimicrob. Chemother. 2018, 73, 1872–1879. [Google Scholar] [CrossRef]
- Castanheira, M.; Huband, M.D.; Mendes, R.E.; Flamm, R.K. Meropenem-Vaborbactam Tested against Contemporary Gram-Negative Isolates Collected Worldwide during 2014, Including Carbapenem-Resistant, KPC-Producing, Multidrug-Resistant, and Extensively Drug-Resistant Enterobacteriaceae. Antimicrob. Agents Chemother. 2017, 61, e00567-17. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pattanaik, P.; Bethel, C.R.; Hujer, A.M.; Hujer, K.M.; Distler, A.M.; Taracila, M.; Anderson, V.E.; Fritsche, T.R.; Jones, R.N.; Pagadala, S.R.R.; et al. Strategic Design of an Effective β-Lactamase Inhibitor. J. Biol. Chem. 2009, 284, 945–953. [Google Scholar] [CrossRef] [Green Version]
- Hancock, R.E.W. Resistance Mechanisms inPseudomonas aeruginosaand Other Nonfermentative Gram-Negative Bacteria. Clin. Infect. Dis. 1998, 27, S93–S99. [Google Scholar] [CrossRef] [Green Version]
- Urban, C.; Go, E.; Mariano, N.; Berger, B.J.; Avraham, I.; Rubin, D.; Rahal, J.J. Effect of Sulbactam on Infections Caused by Imipenem-ResistantAcinetobacter calcoaceticusBiotypeanitratus. J. Infect. Dis. 1993, 167, 448–451. [Google Scholar] [CrossRef]
- Jimenez-Mejias, M.E.; Pachon, J.; Becerril, B.; Palomino-Nicas, J.; Rodriguez-Cobacho, A.; Revuelta, M. Treatment of Multidrug-Resistant Acinetobacter baumannii Meningitis with Ampicillin/Sulbactam. Clin. Infect. Dis. 1997, 24, 932–935. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Housman, S.T.; Hagihara, M.; Nicolau, D.P.; Kuti, J.L. In vitro pharmacodynamics of human-simulated exposures of ampicillin/sulbactam, doripenem and tigecycline alone and in combination against multidrug-resistant Acinetobacter baumannii. J. Antimicrob. Chemother. 2013, 68, 2296–2304. [Google Scholar] [CrossRef] [Green Version]
- Durand-Réville, T.F.; Guler, S.; Comita-Prevoir, J.; Chen, B.; Bifulco, N.; Huynh, H.; Lahiri, S.; Shapiro, A.B.; McLeod, S.M.; Carter, N.M.; et al. ETX2514 is a broad-spectrum β-lactamase inhibitor for the treatment of drug-resistant Gram-negative bacteria including Acinetobacter baumannii. Nat. Microbiol. 2017, 2, 17104. [Google Scholar] [CrossRef] [PubMed]
- Seifert, H.; Müller, C.; Stefanik, D.; Higgins, P.G.; Miller, A.; Kresken, M. In vitro activity of sulbactam/durlobactam against global isolates of carbapenem-resistant Acinetobacter baumannii. J. Antimicrob. Chemother. 2020, 75, 2616–2621. [Google Scholar] [CrossRef] [PubMed]
- Yang, Q.; Xu, Y.; Jia, P.; Zhu, Y.; Zhang, J.; Zhang, G.; Deng, J.; Hackel, M.; A Bradford, P.; Reinhart, H. In vitro activity of sulbactam/durlobactam against clinical isolates of Acinetobacter baumannii collected in China. J. Antimicrob. Chemother. 2020, 75, 1833–1839. [Google Scholar] [CrossRef] [PubMed]
- Buynak, J.D.; Rao, A.; Doppalapudi, V.R.; Adam, G.; Petersen, P.J.; Nidamarthy, S.D. The synthesis and evaluation of 6-alkylidene-2’β-substituted penam sulfones as β-lactamase inhibitors. Bioorganic Med. Chem. Lett. 1999, 9, 1997–2002. [Google Scholar] [CrossRef]
- CLSI. Performance Standards for Antimicrobial Susceptibility Testing, 30th ed.; M100; CLSI: New York, NY, USA, 2020. [Google Scholar]
- Woodford, N.; Ellington, M.J.; Coelho, J.M.; Turton, J.F.; Ward, M.E.; Brown, S.; Amyes, S.G.; Livermore, D.M. Multiplex PCR for genes encoding prevalent OXA carbapenemases in Acinetobacter spp. Int. J. Antimicrob. Agents 2006, 27, 351–353. [Google Scholar] [CrossRef]






| Isolates | Imipenem | Imipenem/LN-1-255 | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| MIC (mg/L) | CLSI Category | MIC (mg/L) | CLSI Category | |||||||||
| MIC50 | MIC90 | Range | %S | %I | %R | MIC50 | MIC90 | Range | %S | %I | %R | |
| All isolates (n = 148) | ≤0.5 | 16 | ≤0.5 to 32 | 64.9 | 3.8 | 28.4 | ≤0.5 | 2 | ≤0.5 to 4 | 91.2 | 8.1 | 0.0 |
| CHDL-producing A. baumannii (n = 41) | 16 | 32 | 4 to 32 | 0.0 | 4.9 | 95.1 | 2 | 4 | ≤0.5 to 4 | 68.3 | 31.7 | 0.0 |
| Non-CHDL-producing A. baumannii (n = 48) | ≤0.5 | 4 | ≤0.5 to 16 | 77.1 | 16.7 | 6.3 | ≤0.5 | 1 | ≤0.5 to 2 | 100 | 0.0 | 0.0 |
| Non-A. baumannii (n = 59) | ≤0.5 | ≤0.5 | ≤0.5 | 100 | 0.0 | 0.0 | ≤0.5 | ≤0.5 | ≤0.5 | 100 | 0.0 | 0.0 |
| Isolates | Meropenem | Meropenem/LN-1-255 | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| MIC (mg/L) | CLSI Category | MIC (mg/L) | CLSI Category | |||||||||
| MIC50 | MIC90 | Range | %S | %I | %R | MIC50 | MIC90 | Range | %S | %I | %R | |
| All isolates (n = 148) | ≤0.5 | 32 | ≤0.5 to ≥64 | 64.9 | 0.0 | 35.1 | ≤0.5 | 4 | ≤0.5 to 16 | 81.1 | 16.2 | 2.7 |
| CHDL-producing A. baumannii (n = 41) | 32 | ≥64 | 8 to ≥64 | 0.0 | 0.0 | 100 | 4 | 4 | ≤0.5 to 16 | 41.5 | 48.7 | 9.8 |
| Non-CHDL-producing A. baumannii (n = 48) | ≤0.5 | 16 | ≤0.5 to 16 | 77.1 | 0.0 | 22.9 | ≤0.5 | 2 | ≤0.5 to 4 | 91.7 | 8.3 | 0.0 |
| Non-A. baumannii (n = 59) | ≤0.5 | ≤0.5 | ≤0.5 | 100 | 0.0 | 0.0 | ≤0.5 | ≤0.5 | ≤0.5 | 100 | 0.0 | 0.0 |
| CHDLs | Number of A. baumannii Isolates Producing CHDLs (%) |
|---|---|
| OXA-23-like | 34 (82.92%) |
| OXA-24-like | 0 |
| OXA-58-like | 7 (17.08%) |
| OXA-148-like | 0 |
| OXA-235-like | 0 |
| Isolates | Cefepime | Cefepime/LN-1-255 | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| MIC (mg/L) | CLSI Category | MIC (mg/L) | CLSI Category | |||||||||
| MIC50 | MIC90 | Range | %S | %I | % R | MIC50 | MIC90 | Range | %S | %I | %R | |
| All isolates (n = 148) | 2 | 32 | ≤1 to ≥128 | 66.2 | 12.2 | 21.6 | 2 | 8 | ≤1 to ≥128 | 95.9 | 1.4 | 2.7 |
| CHDL-producing A. baumannii (n = 41) | 32 | 64 | 4 to ≥128 | 7.3 | 22.0 | 70.7 | 4 | 8 | ≤1 to ≥128 | 92.7 | 0.0 | 7.3 |
| Non-CHDL-producing A. baumannii (n = 48) | 2 | 16 | ≤1 to ≥128 | 79.2 | 14.6 | 6.3 | 2 | 8 | ≤1 to 32 | 95.8 | 2.1 | 2.1 |
| Non-A. baumannii (n = 59) | ≤1 | 4 | ≤1 to 16 | 96.6 | 3.4 | 0.0 | ≤ 1 | 2 | ≤1 to 16 | 98.3 | 1.7 | 0.0 |
| Isolates | Sulbactam | Sulbactam/LN-1-255 | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| MIC (mg/L) | CLSI Category | MIC (mg/L) | CLSI Category | |||||||||
| MIC50 | MIC90 | Range | %S | %I | %R | MIC50 | MIC90 | Range | %S | %I | %R | |
| All isolates (n = 148) | 0.5 | 8 | ≤0.25 to ≥32 | 82.4 | 14.9 | 2.7 | 0.5 | 2 | ≤0.25 to 8 | 99.3 | 0.7 | 0.0 |
| CHDL-producing A. baumannii (n = 41) | 8 | 16 | 2 to ≥32 | 36.6 | 53.7 | 9.8 | 1 | 4 | 0.5 to 8 | 97.6 | 2.4 | 0.0 |
| Non-CHDL-producing A. baumannii (n = 48) | 0.5 | 2 | ≤0.25 to 4 | 100 | 0.0 | 0.0 | 0.5 | 2 | ≤0.25 to 2 | 100 | 0.0 | 0.0 |
| Non-A. baumannii (n = 59) | 0.5 | 1 | ≤0.25 to 1 | 100 | 0.0 | 0.0 | 0.5 | 0.5 | ≤0.25 to 1 | 100 | 0.0 | 0.0 |
| Primer | Sequence (5′-3′) | Product Size (pb) | Reference |
|---|---|---|---|
| OXA-23likeFw | GATCGGATTGGAGAACCAGA | 501 | [38] |
| OXA-23likeRv | ATTTCTGACCGCATTTCCAT | ||
| OXA-24/40likeFw | GGTTAGTTGGCCCCCTTAAA | 246 | [38] |
| OXA-24/40likeRv | AGTTGAGCGAAAAGGGGATT | ||
| OXA-51likeFw | TAATGCTTTGATCGGCCTTG | 353 | [38] |
| OXA-51likeRv | TGGATTGCACTTCATCTTGG | ||
| OXA-58likeFw | AAGTATTGGGGCTTGTGCTG | 599 | [38] |
| OXA-58likeRv | CCCCTCTGCGCTCTACATAC | ||
| OXA-143likeFw | TACAACAACTGAGATTTTCA | 390 | This study |
| OXA-143likeRv | GGGGTTACATCCATTCC | ||
| OXA-235likeFw | ATGGGATGGCAAGAAGC | 239 | This study |
| OXA-235likeRv | GAGGCAAATTCGACTTCT |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lasarte-Monterrubio, C.; Vázquez-Ucha, J.C.; Maneiro, M.; Arca-Suárez, J.; Alonso, I.; Guijarro-Sánchez, P.; Buynak, J.D.; Bou, G.; González-Bello, C.; Beceiro, A. Activity of Imipenem, Meropenem, Cefepime, and Sulbactam in Combination with the β-Lactamase Inhibitor LN-1-255 against Acinetobacter spp. Antibiotics 2021, 10, 210. https://0-doi-org.brum.beds.ac.uk/10.3390/antibiotics10020210
Lasarte-Monterrubio C, Vázquez-Ucha JC, Maneiro M, Arca-Suárez J, Alonso I, Guijarro-Sánchez P, Buynak JD, Bou G, González-Bello C, Beceiro A. Activity of Imipenem, Meropenem, Cefepime, and Sulbactam in Combination with the β-Lactamase Inhibitor LN-1-255 against Acinetobacter spp. Antibiotics. 2021; 10(2):210. https://0-doi-org.brum.beds.ac.uk/10.3390/antibiotics10020210
Chicago/Turabian StyleLasarte-Monterrubio, Cristina, Juan C. Vázquez-Ucha, Maria Maneiro, Jorge Arca-Suárez, Isaac Alonso, Paula Guijarro-Sánchez, John D. Buynak, Germán Bou, Concepción González-Bello, and Alejandro Beceiro. 2021. "Activity of Imipenem, Meropenem, Cefepime, and Sulbactam in Combination with the β-Lactamase Inhibitor LN-1-255 against Acinetobacter spp." Antibiotics 10, no. 2: 210. https://0-doi-org.brum.beds.ac.uk/10.3390/antibiotics10020210