A Stress Syndrome Prototype Reflects Type 3 Diabetes and Ischemic Stroke Risk: The SABPA Study
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Design and Participants
2.2. Protocol
2.2.1. Fundus Imaging and Retinopathy
2.2.2. Diastolic Ocular Perfusion Pressure
2.2.3. Cognitive Executive Functioning Control
2.2.4. Anthropometry and Physical Activity Measures
2.2.5. Biochemical Analyses
2.3. Statistical Analyses
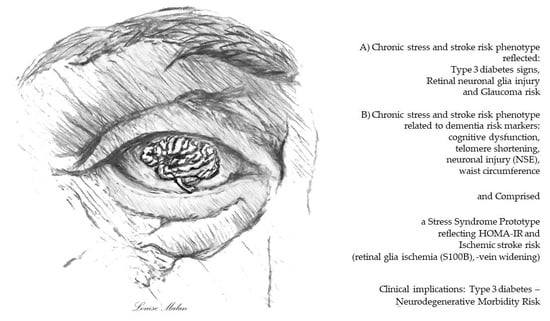
2.3.1. Chronic Stress and Stroke Risk Phenotype Contribution to T3D and Retinopathy Risk
2.3.2. Chronic Stress and Stroke Risk Phenotype-Related Dementia Risk Markers in the Devlopment of a Stress Syndrome Prototype
3. Results
3.1. Clinical Characteristics
3.1.1. Chronic Stress and Stroke Risk Phenotype Contribution to T3D and Retinopathy Risk
3.1.2. Chronic Stress and Stroke Risk Phenotype-Related Dementia Risk Markers and Development of a Stress Syndrome Prototype
4. Discussion
4.1. Chronic Stress and Stroke Risk Phenotype Contribution to T3D and Retinopathy Risk
4.2. Chronic Stress and Stroke Risk Phenotype-Related Dementia Risk Markers and Development of a Stress Syndrome Prototype
4.3. Translational Clinical Value
5. Conclusions
6. Patents
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Banks, W.A.; Owen, J.B.; Erickson, M.A. Insulin in the Brain: There and Back Again. Pharmacol. Ther. 2012, 136, 82–93. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Setyopranoto, I.; Bayuangga, H.F.; Panggabean, A.S.; Alifaningdyah, S.; Lazuardi, L.; Dewi, F.S.T.; Malueka, R.G. Prevalence of Stroke and Associated Risk Factors in Sleman District of Yogyakarta Special Region, Indonesia. Hindawi Stroke Res. Treat. 2019, 2642458. [Google Scholar] [CrossRef] [Green Version]
- Arnold, S.E.; Arvanitakis, Z.; Macauley-Rambach, S.L.; Koenig, A.M.; Wang, H.Y.; Ahima, R.S.; Craft, S.; Gandy, S.; Buettner, C.; Stoeckel, L.E.; et al. Brain Insulin Resistance in Type 2 Diabetes and Alzheimer Disease: Concepts and Conundrums. Nat. Rev. 2018, 14, 168–181. [Google Scholar] [CrossRef]
- Hölscher, C. Brain Insulin Resistance: Role in Neurodegenerative Disease and Potential for Targeting. Expert Opin. Investig. Drugs 2020, 29, 333–348. [Google Scholar] [CrossRef] [PubMed]
- Rhea, E.M.; Banks, W.A. Role of the Blood-Brain Barrier in Central Nervous System Insulin Resistance. Front. Neurosci. 2019, 13, 521. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Neergaard, J.S.; Dragsbæk, K.; Christiansen, C.; Nielsen, H.B.; Brix, S.; Karsdal, M.S.; Henriksen, K. Metabolic Syndrome, Insulin Resistance, and Cognitive Dysfunction: Does Your Metabolic Profile Affect Your Brain? Diabetes 2017, 66, 1957–1963. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Poulaki, V.; Qin, W.; Joussen, A.M.; Hurlbut, P.; Wiegand, S.J.; Rudge, J.; Yancopoulos, G.D.; Adamis, A.P. Acute Intensive Insulin Therapy Exacerbates Diabetic Blood-Retinal Barrier Breakdown via Hypoxia-inducible Factor-1α and VEGF. J. Clin Investig. 2002, 109, 805–815. [Google Scholar] [CrossRef]
- Ekblad, L.L.; Johansson, J.; Helin, S.; Viitanen, M.; Laine, H.; Puukka, P.; Jula, A.; Rinne, J.O. Midlife Insulin Resistance, APOE Genotype, and Late-life Brain Amyloid Accumulation. Neurology 2018, 90, e1150–e1157. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- de la Monte, S.M.; Wands, J.R. Alzheimer’s Disease is Type 3 Diabetes-Evidence Reviewed. J. Diabetes Sci. Technol. 2008, 2, 1101–1113. [Google Scholar] [CrossRef] [Green Version]
- American Diabetes Association. 2. Classification and Diagnosis of Diabetes: Standards of Medical Care in Diabetes—2020. Diab. Care 2020, 43 (Suppl. 1), S14–S31. [Google Scholar] [CrossRef] [Green Version]
- Mittal, K.; Mani, R.; Katare, D. Type 3 Diabetes: Cross Talk between Differentially Regulated Proteins of Type 2 Diabetes Mellitus and Alzheimer’s Disease. Sci. Rep. 2016, 6, 25589. [Google Scholar] [CrossRef]
- Nguyen, T.T.; Ta, Q.T.H.; Nguyen, T.K.O.; Nguyen, T.T.D.; Van Giau, V. Type 3 Diabetes and Its Role Implications in Alzheimer’s Disease. Int. J. Mol. Sci. 2020, 21, 3165. [Google Scholar] [CrossRef] [PubMed]
- Zhong, Z.L.; Chen, S. Indicating and Predicting Role of the Horizontal C/D Ratio in Preclinical Diabetic Retinopathy Associated with Chronic Angle-closure Glaucoma. Int. J. Ophthalmol. 2019, 12, 268–274. [Google Scholar] [CrossRef] [PubMed]
- Malan, L.; Hamer, M.; von Känel, R.; van Wyk, R.D.; Wentzel, A.; Steyn, H.S.; van Vuuren, P.; Malan, N.T. Retinal-Glia Ischemia and Inflammation Induced by Chronic Stress: The SABPA Study. Brain Behav. Immun. Health 2020, 2, 100027. [Google Scholar] [CrossRef]
- Malan, L.; Hamer, M.; von Känel, R.; Kotliar, K.; van Wyk, R.D.; Lambert, G.W.; Vilser, W.; Ziemssen, T.; Schlaich, M.P.; Smith, W.; et al. Delayed Retinal Vein Recovery Responses Reflect Non-adaptation to Stress; and an Increased Stroke Risk: The SABPA study. Cardiovasc. J. Afr. 2020, 31, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Haque, A.; Polcyn, R.; Matzelle, D.; Banik, N.L. New Insights into the Role of Neuron-Specific Enolase in Neuro-Inflammation, Neurodegeneration, and Neuroprotection. Brain Sci. 2018, 8, 33. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kuehn, S.; Meißner, W.; Grotegut, P.; Carsten, C.; Dick, H.B.; Joachim, S.C. Intravitreal S100B Injection Leads to Progressive Glaucoma Like Damage in Retina and Optic Nerve. Front. Cell Neurosci. 2018, 12, 312. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vujosevic, S.; Micera, A.; Bini, S.; Berton, M.; Esposito, G.; Midena, E. Aqueous Humor Biomarkers of Müller cell activation in diabetic eyes. Investig. Ophthalmol. Vis. Sci. 2015, 56, 3913–3918. [Google Scholar] [CrossRef] [Green Version]
- Chaves, M.L.; Camozzato, A.L.; Ferreira, E.D.; Piazenski, I.; Kochhann, R.; Dall’Igna, O.; Mazzini, G.S.; Souza, D.O.; Portela, L.V. Serum Levels of S100B and NSE Proteins in Alzheimer’s Disease Patients. J. Neuroinflamm. 2010, 7, 6. [Google Scholar] [CrossRef] [Green Version]
- Wang, S.-Y.; Zha, X.-J.; Zhu, X.-Y.; Li, W.-B.; Ma, J.; Wu, Z.-W.; Wu, H.; Jiang, M.-F.; Wen, Y.-F. Metabolic Syndrome and Its Components with Neuron-specific Enolase: A Cross Sectional Study in Large Health Check-up Population in China. Brit. Med. J. Open. 2018, 8, e020899. [Google Scholar] [CrossRef] [Green Version]
- Fania, L.; Hilal, S.; Sedaghata, S.; Broer, L.; Licher, S.; Arp, P.P.; van Meurs, J.B.J.; Ikram, M.K.; Ikram, M.A. Telomere Length and the Risk of Alzheimer’s Disease: The Rotterdam Study. J. Alz. Dis. 2020, 73, 707–714. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Buchtele, N.; Schwameis, M.; Gilbert, J.C.; Schörgenhofer, C.; Jilmam, B. Targeting von Willebrand Factor in Ischaemic Stroke: Focus on Clinical Evidence. Thromb. Haemost. 2018, 118, 959–978. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Benarroch, E.E. Brain Glucose Transporters: Implications for Neurologic Disease. Neurology 2014, 82, 1374–1379. [Google Scholar] [CrossRef] [PubMed]
- Pardridge, W.M.; Eisenberg, J.; Yang, J. Human Blood-brain Barrier Insulin Receptor. J. Neurochem. 1985, 44, 1771–1778. [Google Scholar] [CrossRef]
- Kotliar, K.; Hauser, C.; Ortner, M.; Muggenthaler, C.; Diehl-Schmid, J.; Angerman, S.; Hapfelmeier, A.; Schmaderer, C.; Grimmer, T. Altered Neurovascular Coupling as Measured by Optical Imaging: A Biomarker for Alzheimer’s Disease. Sci. Rep. 2017, 7, 12906. [Google Scholar] [CrossRef]
- Malan, L.; Hamer, M.; Frasure-Smith, N.; Steyn, H.S.; Malan, N.T. Cohort Profile: Sympathetic Activity and Ambulatory Blood Pressure in Africans (SABPA) Prospective Cohort Study. Int. J. Epidemiol. 2015, 44, 1814–1822. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Flammer, J.; Konieczka, K.; Bruno, R.M.; Virdis, A.; Flammer, A.J.; Taddei, S. The Eye and the Heart. Eur. Heart J. 2013, 34, 1270–1280. [Google Scholar] [CrossRef]
- Papastathopoulos, K.I.; Jonas, J.B. Follow up of focal narrowing of retinal arterioles in glaucoma. Brit. J. Ophthal. 1999, 83, 285–289. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stroop, J.R. Studies of Interference in Serial Verbal Reactions. J. Exp. Psych. 1935, 18, 643–662. [Google Scholar] [CrossRef]
- Hutchison, K.A.; Balota, D.A.; Duchek, J.M. The Utility of Stroop Task Switching as a Marker for Early-stage Alzheimer’s Disease. Psychol. Aging 2010, 25, 545–559. [Google Scholar] [CrossRef]
- Koss, E.; Ober, B.A.; Delis, D.C.; Friedland, R.P. The Stroop Color-Word Test: Indicator of Dementia Severity. Int. J. Neurosci. 1984, 24, 53–61. [Google Scholar] [CrossRef]
- Luchsinger, J.A.; Patel, B.; Tang, M.X.; Schupf, N.; Mayeux, R. Measures of Adiposity and Dementia Risk in Elderly Persons. Arch. Neurol. 2007, 64, 392–398. [Google Scholar] [CrossRef] [PubMed]
- Wolters, F.J.; Boender, J.; de Vries, P.S.; Sonneveld, M.A.; Koudstaal, P.J.; de Maat, M.P.; Franco, O.H.; Ikram, M.K.; Leebeek, F.W.; Ikram, M.A. Von Willebrand Factor and ADAMTS13 Activity in Relation to Risk of Dementia: A Population-based Study. Sci. Rep. 2018, 8, 5474. [Google Scholar] [CrossRef] [Green Version]
- Hazzouri, A.Z.A.; Haan, M.N.; Deng, Y.; Neuhaus, J.; Yaffe, K. Reduced Heart Variability is Associated with Worse Cognitive Performance in Elderly Mexican Americans. Hypertension 2014, 63, 181–187. [Google Scholar] [CrossRef] [Green Version]
- Gabin, J.M.; Saltvedt, I.; Tambs, K.; Holmen, J. The Association of High Sensitivity C-reactive Protein and Incident Alzheimer Disease in Patients 60 years and Older: The HUNT study, Norway. Immun. Ageing 2018, 15, 4. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jarvis, M.; Tunstall-Pedoe, H.; Feyerabend, C.; Vesey, C.; Salloojee, Y. Biochemical markers of smoke absorption and self-reported exposure to passive smoking. J. Epidemiol. Comm. Health 1984, 38, 335–359. [Google Scholar] [CrossRef] [Green Version]
- Hastedt, M.; Buchner, M.; Rothe, M.; Gapert, R.; Herre, S.; Krumbiegel, F.; Tsokos, M.; Kienast, T.; Heinz, A.; Hartwig, S. Detecting alcohol abuse: Traditional blood alcohol markers compared to ethyl glucuronide (EtG) and fatty acid ethyl esters (FAEEs) measurement in hair. Forensic. Sci. Med. Pathol. 2013, 9, 471–477. [Google Scholar] [CrossRef]
- Gomez, J.M. Growth hormone and insulin-like growth factor-I as an endocrine axis in Alzheimer’s disease. Endocr. Metab. Immun. Disord. Drug Targets 2008, 8, 143–151. [Google Scholar] [CrossRef]
- Wan, J.; Zhao, X.F.; Vojtek, A.; Goldman, D. Retinal Injury, Growth Factors, and Cytokines Converge on Beta-catenin and pStat3 Signaling to Stimulate Retina Redevelopment. Cell Rep. 2014, 9, 285–297. [Google Scholar] [CrossRef] [Green Version]
- Cersosimo, E.; Solis-Herrera, C.; Trautmann, M.E.; Malloy, J.; Triplitt, C.L. Assessment of pancreatic β-cell function: Review of methods and clinical applications. Curr. Diab. Rev. 2014, 10, 2–42. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- von Känel, R.; Hamer, M.; Van Der Westhuizen, F.H.; Malan, N.T.; Malan, L. Leukocyte Telomere Length and Hemostatic Factors in a South African Cohort: The SABPA Study. Thromb. Haemost. 2014, 12, 1975–1985. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Venter, M.; Malan, L.; van Dyk, E.; Elson, J.L.; van der Westhuizen, F.H. Using MutPred Derived mtDNA Load Scores to Evaluate mt DNA Variation in Hypertension and Diabetes in a Bi-ethnic Cohort: The SABPA Study. J. Genet. Genom. 2017, 44, 139–149. [Google Scholar] [CrossRef]
- Westen, D. Prototype diagnosis of psychiatric syndromes. World Psychiatry J. 2012, 11, 16–21. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hoebel, S.; Malan, L.; Botha, J.; Swanepoel, M. Optimizing Waist Circumference Cut-points for the Metabolic Syndrome and its Components in a South African Cohort at 3-year Follow-up: The SABPA Prospective Cohort. Endocrine 2014, 67, 959–961. [Google Scholar] [CrossRef]
- Gluck, M.E.; Ziker, C.; Schwegler, M.; Thearle, M.; Votruba, S.B.; Krakoff, J. Impaired Glucose Regulation is Associated with Poorer Performance on the Stroop Task. Physiol. Behav. 2013, 122, 113–119. [Google Scholar] [CrossRef] [Green Version]
- Stoeckel, L.E.; Arvanitakis, Z.; Gandy, S.; Small, D.; Kahn, C.R.; Pascual-Leone, A.; Pawlyk, A.; Sherwin, R.; Smith, P. Complex Mechanisms Linking Neurocognitive Dysfunction to Insulin Resistance and Other Metabolic Dysfunctions. F1000Research 2016, 15, 353. [Google Scholar] [CrossRef] [PubMed]
- Dybjer, E.; Nilsson, P.M.; Engström, G.; Helmer, C.; Nägga, K. Pre-diabetes and diabetes are independently associated with adverse cognitive test results: A cross-sectional, population-based study. BMC Endocr. Disord. 2018, 18, 91. [Google Scholar] [CrossRef] [Green Version]
- Price, R.B.; Duman, R. Neuroplasticity in Cognitive and Psychological Mechanisms of Depression: An Integrative Model. Mol. Psychiatry 2020, 25, 530–543. [Google Scholar] [CrossRef] [PubMed]
- Clarke, D.W.; Boyd, F.T., Jr.; Kappy, M.S.; Raizada, M.K. Insulin Binds to Specific Receptors and Stimulates 2-Deoxy-D-glucose Uptake in Cultured Glia Cells from Rat Brain. J. Biol. Chem. 1984, 259, 11672–11675. [Google Scholar] [CrossRef]
- Pouriamehr, S.; Barmaki, H.; Rastegary, M.; Lotfi, M.; Afjadi, M.N. Investigation of Insulin-like Growth Factors/Insulin-like Growth Factor Binding Proteins Regulation in Metabolic Syndrome Patients. BMC Res. Notes 2019, 12, 653. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Arroba, A.I.; Campos-Caro, A.; Aguilar-Diosdado, M.; Valverde, Á.M. IGF-1, Inflammation and Retinal Degeneration: A Close Network. Front. Aging Neurosci. 2018, 10, 203. [Google Scholar] [CrossRef] [PubMed]
- Lutty, G.A. Effects of Diabetes on the Eye. Investig. Ophthalmol. Vis. Sci. 2013, 54, ORSF81–ORSF87. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hansen, G.L.; Kofoed, P.K.; Munch, I.C.; Sillesen, H.; Jensen, L.P.; Iversen, H.K.; Larsen, M. Retinal Angiographic Blood Flow is Reduced in the Ocular Ischaemic Syndrome. Dan. Med. J. 2012, 60, A4716. [Google Scholar]
- Díaz-Coránguez, M.; Ramos, C.; Antonetti, D.A. The Inner Blood-Retinal Barrier: Cellular Basis and Development. Vis. Res. 2017, 139, 123–137. [Google Scholar] [CrossRef] [PubMed]
- Cristóvão, J.S.; Gomes, C.M. S100 Proteins in Alzheimer’s Disease. Front. Neurosci. 2019, 13, 463. [Google Scholar] [CrossRef] [PubMed]
- Yu, Z.W.; Liu, R.; Li, X.; Wang, Y.; Fu, Y.H.; Li, H.Y.; Yuan, Y.; Gao, X.Y. High Serum Neuron-Specific Enolase Level Is Associated with Mild Cognitive Impairment in Patients with Diabetic Retinopathy. Diabetes Met. Syndr. Obes. 2020, 13, 1359–1365. [Google Scholar] [CrossRef] [Green Version]
- Sharma, R.; Gupta, A.; Thungapathra, M.; Bansal, R. Telomere Mean Length in Patients with Diabetic Retinopathy. Sci. Rep. 2016, 5, 18368. [Google Scholar] [CrossRef]
- Saeed, S.; Waje-Andreassen, U.; Nilsson, P.M. The Association of the Metabolic Syndrome with Target Organ Damage: Focus on the Heart, Brain, and Central Arteries. Expert Rev. Cardiovasc. Ther. 2020, 18, 601–614. [Google Scholar] [CrossRef] [PubMed]
- Sumner, A.E.; Bagheri, M.H. Identifying the Waist Circumference of Risk in People of African Descent. Nat. Rev. Endocrinol. 2020, 16, 1–3. [Google Scholar] [CrossRef]
- Fitzpatrick, S.; Gilbert, S.; Serpell, L. Systematic Review: Are Overweight and Obese Individuals Impaired on Behavioural Tasks of Executive Functioning? Neuropsychol. Rev. 2013, 23, 138–156. [Google Scholar] [CrossRef] [PubMed]
- Gottesman, R.F.; Schneider, A.L.; Zhou, Y.; Coresh, J.; Green, E.; Gupta, N.; Knopman, D.S.; Mintz, A.; Rahmim, A.; Sharrett, A.R.; et al. Association Between Midlife Vascular Risk Factors and Estimated Brain Amyloid Deposition. JAMA 2017, 317, 1443–1450. [Google Scholar] [CrossRef] [PubMed]
- Björnson, E.; Adiels, M.; Taskinen, M.-R.; Borén, J. Kinetics of Plasma Triglycerides in Abdominal Obesity. Curr. Opin. Lipidol. 2017, 28, 11–18. [Google Scholar] [CrossRef]
- Joyal, M.; Wensing, T.; Levasseur-Moreau, J.; Leblond, J.T.; Sack, A.; Fecteau, S. Characterizing Emotional Stroop Interference in Posttraumatic Stress Disorder, Major Depression and Anxiety Disorders: A systematic Review and Meta-analysis. PLoS ONE 2019, 14, e0214998. [Google Scholar] [CrossRef] [PubMed]
- Malan, L.; Hamer, M.; von Känel, R.; Lambert, G.W.; Delport, R.; Steyn, H.S.; Malan, N.T. Chronic Defensiveness and Neuroendocrine Dysregulation Reflect a Novel Cardiac Troponin T Cut Point: The SABPA Study. Psychoneuroendocrinology 2017, 85, 20–27. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Malan, N.T.; von Känel, R.; Smith, W.; Lambert, G.W.; Vilser, W.; Eikelis, N.; Reimann, M.; Malan, L. A Challenged Sympathetic System is Associated with Retinal Vascular Calibre in a Black Male Cohort: The SABPA Study. In Microcirculation Revisited-From Molecules to Clinical Practice; Trdine, J., Rijeka, C., Eds.; Helena Lenasi, IntechOpen Limited: London, UK, 2016; pp. 135–153. ISBN 978-953-51-4801-2. [Google Scholar] [CrossRef] [Green Version]





| Stressed (N = 159) | Non-Stressed (N = 105) | p-Values | |
|---|---|---|---|
| Age (years) | 46 (±9) | 45 (±9) | 0.632 |
| Ethnicity: Black | 97 (61) | 21 (20) | <0.001 |
| Sex: Men | 114 (72) | 29 (28) | <0.001 |
| Total energy expenditure(kcal/7 days) | 3470 (±1275) | 3326 (±1502) | 0.405 |
| Smoking status | 45 (28) | 6 (6) | <0.001 |
| Gamma glutamyl tansferase (U/L) | 68.0 (±79.2) | 19.6 (13.5) | <0.001 |
| Alcohol abuse | 67 (42) | 3 (3) | <0.001 |
| Cardiometabolic risk markers | |||
| Ethnicity-specific waist circumference | 105 (66) | 54 (51) | 0.018 |
| Dyslipidemia | 77 (48) | 34 (32) | 0.011 |
| Low grade inflammation | 86 (54) | 40 (38) | 0.011 |
| Cognitiveexe-func score | 53 (±14) | 62 (±13) | <0.001 |
| Neuron-specific enolase/NSE (ng/mL) | 9.9 (±4.2) | 10.2 (±3.6) | 0.591 |
| S100B (ng/mL) | 54.6 (±39.2) | 43.7 (±20.5) | 0.009 |
| HbA1C (%) | 6.1 (±0.9) | 5.4 (±0.3) | <0.001 |
| Insulin (μU/mL) | 17.2 (±12) | 10 (±6) | <0.001 |
| Insulin-like growth factor 1 (ng/mL) | 155 (±60) | 171 (±58) | 0.031 |
| Insulin-like growth factor binding protein 3 (nmol/L) | 132 (±28) | 143 (±23) | 0.002 |
| Triglyceridemia | 55 (35) | 14 (13) | <0.001 |
| Hyperinsulinemia | 38 (24) | 6 (6) | <0.001 |
| Pre-diabetes | 108 (68) | 18 (17) | <0.001 |
| Diabetes | 20 (13) | 0 (0) | <0.001 |
| HOMA-IR | 5 (±4) | 3 (±2) | <0.001 |
| HOMA-IR median (interquartile ranges) | 4 (2, 6) | 2 (1, 3) | <0.001 |
| Upper quartile HOMA-IR (≥5) | 60 (38) | 11 (11) | <0.001 |
| 24-h Hypertension | 118 (74) | 32 (31) | <0.001 |
| Diabetic and Hypertensive retinopathy | 98 (62) | 46 (44) | 0.004 |
| Retinal vascular dysregulation at 3-y follow-up | |||
| Retinal artery (count) | 12 (±2) | 13 (±2) | 0.046 |
| Retinal vein (count) | 11 (±1.8) | 11 (±2.0) | 0.949 |
| Retinal artery caliber (MU) | 1490 (±12) | 153 (±12) | 0.011 |
| Retinal vein caliber (MU) | 244 (±20.9) | 239 (±17.2) | 0.041 |
| Focal narrowing | 4 (3) | 0 (0) | 0.965 |
| Arterio-venous nicking | 82 (74) | 29 (26) | <0.001 |
| Optic nerve cup/disc ratio (≥0.5) | 29 (19) | 22 (21) | 0.683 |
| Optic nerve damage | 49 (±40) | 44 (±34) | 0.362 |
| Diastolic ocular perfusion pressure (mmHg) | 73 (±11) | 66 (±11) | <0.001 |
| Self-reported medication | |||
| Diabetes | 8 (5) | 0 (0) | <0.001 |
| Hypertension | 48 (30) | 18 (17) | 0.017 |
| Anti-depressant | 1 (1) | 1 (1) | 0.767 |
| Stressed (N = 159) | p-Value | non-Stressed (N = 105) | p = Value | |||||
|---|---|---|---|---|---|---|---|---|
| Difference (±95% CI) | Difference (±95% CI) | |||||||
| Baseline Cognitiveexe-func score | ||||||||
| Baseline Telomere length (ng/μL) | ||||||||
| NSE (ng/mL) | +1.27 (0.52, 2.02) | ≤0.001 | −0.28 (−0.97, 0.41) | 0.423 | ||||
| S100B (ng/mL) | −0.07 (−3.80, 2.46) | 0.674 | +2.05 (−0.27, 4.37) | 0.083 | ||||
| WC (cm) | +3.45 (2.4, 4.6) | ≤0.001 | +3.40 (1.7, 5.1) | ≤0.001 | ||||
| CRP (ng/mL) | −0.93 (−3.1, 1.1) | 0.370 | −1.42 (−2.5, −0.4) | 0.009 | ||||
| VWF (%) | +16.35 (10.7, 22.0) | ≤0.001 | +18.94 (13.8, 24.1) | ≤0.001 | ||||
| 24-h HRV (ms) | −62.44 (170.9, 46.0) | 0.257 | −17.50 (−39.6, 4.6) | 0.120 | ||||
| McNemar’s case–control test | Incidence and recovery | |||||||
| HOMA-IR (Upper quartile ≥ 5) | ||||||||
| Incidence, n (%) | 31 (25) | 8 (8) | ||||||
| Recovery, n (%) | 3 (3) | 0 (0) | ||||||
| OR (95% CI), P | 10.33 (3.2, 33.8), ≤0.001 | To infinity | ||||||
| Model 1 | Retinal Arteries (MU) | Retinal Veins (MU) |
|---|---|---|
| Stressed Group (N = 145) | ||
| Adjusted R2 | 0.30 | 0.30 |
| ß (95% CI), p | ß (95% CI), p | |
| Age | - | - |
| Cognitiveexe-func score | - | −0.18 (−0.34, −0.02), p = 0.020 |
| NSE (ng/mL) | - | −0.14 (−0.28, 0.00), p = 0.045 |
| S100B (ng/mL) | - | 0.17 (0.03, 0.31), p = 0.024 |
| HOMA-IR | - | 0.23 (−1.57, 2.03), p = 0.016 |
| DOPP (mmHg) | −0.33 (−0.47, −0.19), p ≤ 0.001 | 0.20 (0.04, 0.36), p = 0.012 |
| Optic nerve cup–disc ratio | −0.17 (−0.31, −0.03), p = 0.018 | - |
| Retinal artery (count) | - | - |
| Model 2 | Non-Stressed Group (N = 96) | |
| Adjusted R2 | 0.50 | 0.47 |
| ß (95% CI), p | ß (95% CI), p | |
| Age | - | −0.23 (0.08), p = 0.003 |
| Cognitiveexe-func | - | - |
| NSE (ng/mL) | - | NS |
| S100B (ng/mL) | NS | - |
| HOMA-IR | - | - |
| DOPP (mmHg) | −0.16 (−0.34, −0.02), p = 0.029 | - |
| Optic nerve cup-disc ratio | - | - |
| Retinal artery (count) | 0.17 (0.01, 0.33), p = 0.027 | −0.21 (−0.37, −0.05), p = 0.008 |
| * Chronic Stress and Stroke Risk Phenotype (N = 264) | ||||
|---|---|---|---|---|
| Odds Ratio | 5th Percentile | 95th Percentile | p-Value | |
| Cognitiveexe-func | 0.96 | 0.93 | 0.98 | ≤0.001 |
| Telomere length | 0.03 | 0.002 | 0.36 | 0.007 |
| NSE (ng/mL) | 0.47 | 0.27 | 0.84 | 0.011 |
| Waist circumference (cm) | 37.29 | 8.87 | 156.79 | ≤0.001 |
| von Willebrand factor (%) | NS | |||
| C-reactive protein (mg/L) | NS | |||
| 24-h HRV-SDNN | NS | |||
| Mitochondrial DNA variation | 0.89 | 0.43 | 1.87 | 0.766 |
| Stress Syndrome Prototype (N = 252) | ||||
|---|---|---|---|---|
| Odds Ratio | 5th Percentile | 95th Percentile | p-Value | |
| HOMA-IR | 7.72 | 2.65 | 22.45 | ≤0.001 |
| S100B (ng/mL) | 1.27 | 1.06 | 1.52 | 0.022 |
| Retinal vein caliber | 1.03 | 1.00 | 1.05 | 0.026 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Malan, L.; Hamer, M.; von Känel, R.; van Wyk, R.D.; Sumner, A.E.; Nilsson, P.M.; Lambert, G.W.; Steyn, H.S.; Badenhorst, C.J.; Malan, N.T. A Stress Syndrome Prototype Reflects Type 3 Diabetes and Ischemic Stroke Risk: The SABPA Study. Biology 2021, 10, 162. https://0-doi-org.brum.beds.ac.uk/10.3390/biology10020162
Malan L, Hamer M, von Känel R, van Wyk RD, Sumner AE, Nilsson PM, Lambert GW, Steyn HS, Badenhorst CJ, Malan NT. A Stress Syndrome Prototype Reflects Type 3 Diabetes and Ischemic Stroke Risk: The SABPA Study. Biology. 2021; 10(2):162. https://0-doi-org.brum.beds.ac.uk/10.3390/biology10020162
Chicago/Turabian StyleMalan, Leoné, Mark Hamer, Roland von Känel, Roelof D. van Wyk, Anne E. Sumner, Peter M. Nilsson, Gavin W. Lambert, Hendrik S. Steyn, Casper J. Badenhorst, and Nico T. Malan. 2021. "A Stress Syndrome Prototype Reflects Type 3 Diabetes and Ischemic Stroke Risk: The SABPA Study" Biology 10, no. 2: 162. https://0-doi-org.brum.beds.ac.uk/10.3390/biology10020162