Is ABO-Incompatible Living Donor Liver Transplantation Really a Good Alternative for Pediatric Recipients?
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Basic Immunosuppressive Protocol
2.3. Immunosuppressive Protocol for ABOi Pediatric LDLT
2.4. Monitoring of Iso-Agglutinins in the Post-Transplant Period for ABOi Recipients and Adjustment of Immunosuppressive Therapy
2.5. Histopathological Studies on Post-LT Liver Biopsies for Suspected ACR
3. Statistical Analysis
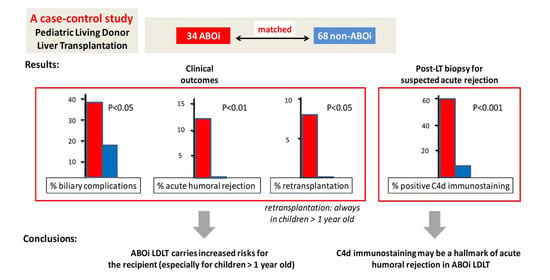
4. Results
4.1. Overall Results
4.2. Pre-Transplant Iso-Agglutinins and Immunosuppressive Preparation in ABOi LDLT Recipients
4.3. Post-Transplant Iso-Agglutinins and Additional Post-LT Immunosuppressive Treatments in ABOi LDLT Recipients
4.4. Post-LT Complications
4.5. Histopathologic Studies on Post-Transplant Liver Biopsies
5. Discussion
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Raut, V.; Uemoto, S. Management of ABO-incompatible living-donor liver transplantation: Past and present trends. Surg. Today 2011, 41, 317–322. [Google Scholar] [CrossRef]
- Starzl, T.E.; Koep, L.J.; Halgrimson, C.G.; Hood, J.; Schroter, G.P.J.; Porter, K.A.; Weil, R. Fifteen years of clinical liver transplantation. Gastroenterology 1979, 77, 375–388. [Google Scholar] [CrossRef]
- Demetris, A.J.; Jaffe, R.; Tzakis, A.; Ramsey, G.; Todo, S.; Belle, S.; Esquivel, C.; Shapiro, R.; Markus, B.; Mroczek, E.; et al. Antibody-mediated rejection of human orthotopic liver allografts: A study of liver transplantation across ABO blood group barriers. Am. J. Pathol. 1988, 132, 489. [Google Scholar] [PubMed]
- Sanchez-Urdazpal, L.; Sterioff, S.; Janes, C.; Schwerman, L.; Rosen, C. Increased bile duct complications in ABO incompatible liver transplant recipients. Transplant. Proc. 1991, 23, 1440–1441. [Google Scholar]
- Racusen, L.C.; Colvin, R.B.; Fogo, A.; Furness, P.; Gibson, I.; Glotz, D.; Hayry, P.; Hunsickern, L.; Kashgarian, M.; Kerman, R.; et al. Antibody-Mediated Rejection Criteria—An Addition to the Banff 97 Classification of Renal Allograft Rejection. Am. J. Transplant. 2003, 3, 708–714. [Google Scholar] [CrossRef]
- Takemoto, S.K.; Zeevi, A.; Platt, J.L.; Rabb, H.; Thistlethwaite, R.; Tyan, D.; Delmonico, F.L.; Feng, S.; Colvin, R.B.; Jordan, S.; et al. National Conference to Assess Antibody-Mediated Rejection in Solid Organ Transplantation. Am. J. Transplant. 2004, 4, 1033–1041. [Google Scholar] [CrossRef]
- Gugenheim, J.; Samuel, D.; Bismuth, H.; Reynes, M. Liver transplantation across ABO blood group barriers. Lancet 1990, 336, 519–523. [Google Scholar] [CrossRef]
- Farges, O.; Kalil, A.N.; Samuel, D.; Saliba, F.; Arulnaden, J.L.; Debat, P.; Bismuth, A.; Castaing, D.; Bismuth, H. The use of ABO-incompatible grafts in liver transplantation: A life-saving procedure in highly selected patients. Transplantation 1995, 59, 1124–1133. [Google Scholar] [CrossRef]
- Renard, T.H.; Andrews, W.S. An approach to ABO-incompatible liver transplantation in children. Transplantation 1992, 53, 116–120. [Google Scholar] [CrossRef]
- Yandza, T.; Lambert, T.; Alvarez, F.; Gauthier, F.; Jacolot, D.; Huault, G.; Fabre, M.; Valayer, J. Outcome of ABO-incompatible liver transplantation in children with no specific alloantibodies at the time of transplantation. Transplantation 1994, 58, 46–50. [Google Scholar] [CrossRef]
- Rieben, R.; Korchagina, E.Y.; Allmen, E.U.-V.; Hovinga, J.A.K.; Lämmle, B.; Jungi, T.W.; Bovin, N.V.; Nydegger, U.E. In vitro evaluation of the efficacy and biocompatibility of new, synthetic ABO immunoabsorbents. Transplantation 1995, 60, 425–430. [Google Scholar] [CrossRef]
- Egawa, H.; Teramukai, S.; Haga, H.; Tanabe, M.; Mori, A.; Ikegami, T.; Kawagishi, N.; Ohdan, H.; Kasahara, M.; Umeshita, K. Impact of Rituximab Desensitization on Blood-Type-Incompatible Adult Living Donor Liver Transplantation: A Japanese Multicenter Study. Am. J. Transplant. 2013, 14, 102–114. [Google Scholar] [CrossRef] [Green Version]
- Song, G.-W.; Lee, S.-G.; Hwang, S.; Kim, K.-H.; Ahn, C.-S.; Moon, D.-B.; Ha, T.-Y.; Jung, D.-H.; Park, G.-C.; Kang, S.-H.; et al. Biliary stricture is the only concern in ABO-incompatible adult living donor liver transplantation in the rituximab era. J. Hepatol. 2014, 61, 575–582. [Google Scholar] [CrossRef]
- Song, G.; Lee, S.; Sin, M.; Yoon, Y.; Kang, W.-H.; Tak, E.; Hwang, S.; Kim, K.; Ahn, C.; Moon, D.; et al. ABO-Incompatible Adult Living Donor Liver Transplantation under the Desensitization Protocol with Rituximab. Am. J. Transplant. 2015, 16, 157–170. [Google Scholar] [CrossRef] [Green Version]
- Okada, N.; Sanada, Y.; Hirata, Y.; Yamada, N.; Wakiya, T.; Ihara, Y.; Urahashi, T.; Miki, A.; Kaneda, Y.; Sasanuma, H.; et al. The impact of rituximab in ABO-incompatible pediatric living donor liver transplantation: The experience of a single center. Pediatr. Transplant. 2015, 19, 279–286. [Google Scholar] [CrossRef]
- Rana, A.; Kueht, M.L.; Nicholas, S.K.; Jindra, P.; Himes, R.; Desai, M.S.; Cotton, R.T.; Galvan, N.T.; O’Mahony, C.A.; Goss, J.A. Pediatric Liver Transplantation across the ABO Blood Group Barrier: Is It an Obstacle in the Modern Era? J. Am. Coll. Surg. 2016, 222, 681–689. [Google Scholar] [CrossRef]
- Otte, J.-B.; Goyet, J.D.V.; Reding, R.; Van Obbergh, L.; Veyckemans, F.; Carlier, M.; De Kock, M.; De Cléty, S.C.; Clapuyt, P.; Sokal, E.; et al. Pediatric liver transplantation: From the full-size liver graft to reduced, split, and living related liver transplantation. Pediatr. Surg. Int. 1998, 13, 308–318. [Google Scholar] [CrossRef]
- Evrard, V.; Otte, J.B.; Sokal, E.; Rochet, J.S.; Haccourt, F.; Gennari, F.; Latinne, D.; Jamart, J.; Reding, R. Impact of surgical and immunological parameters in pediatric liver transplantation: A multivariate analysis in 500 consecutive recipients of primary grafts. Ann. Surg. 2004, 239, 272–280. [Google Scholar] [CrossRef]
- Darwish, A.A.; Bourdeaux, C.; Kader, H.A.; Janssen, M.; Sokal, E.; Lerut, J.; Ciccarelli, O.; Veyckemans, F.; Otte, J.-B.; Goyet, J.D.V.D.; et al. Pediatric liver transplantation using left hepatic segments from living related donors: Surgical experience in 100 recipients at Saint-Luc University Clinics. Pediatr. Transplant. 2006, 10, 345–353. [Google Scholar] [CrossRef]
- de Magnee, C.; Bourdeaux, C.; De Dobbeleer, F.; Janssen, M.; Menten, R.; Clapuyt, P.; Reding, R. Impact of pre-transplant liver hemodynamics and portal reconstruction techniques on post-transplant portal vein complications in pediatric liver transplantation: A retrospective analysis in 197 recipients. Ann. Surg. 2011, 254, 55–61. [Google Scholar] [CrossRef]
- Reding, R.; Gennari, F.; Janssen, M.; Jamart, J.; Goyet, J.D.V.D.; Lerut, J.; Sokal, E.; Otte, J.B. The pediatric liver transplant program at the Université Catholique de Louvain, Cliniques Saint-Luc, Brussels: Overall results in 444 children (1984–1997). Acta Gastro-Enterol. Belg. 1999, 62, 285–289. [Google Scholar]
- Demetris, A.J.; Batts, K.P.; Dhillon, A.P.; Ferrell, L.; Fung, J.; Geller, S.A.; Hart, J.; Hayry, P.; Hofmann, W.J.; Hubscher, S.; et al. Banff schema for grading liver allograft rejection: An international consensus document. Hepatology 1997, 25, 658–663. [Google Scholar]
- Haga, H.; Egawa, H.; Shirase, T.; Miyagawa, A.; Sakurai, T.; Minamiguchi, S.; Yamabe, H.; Manabe, T.; Tanaka, K. Periportal edema and necrosis as diagnostic histological features of early humoral rejection in ABO-incompatible liver transplantation. Liver Transplant. 2004, 10, 16–27. [Google Scholar] [CrossRef] [Green Version]
- Morioka, D.; Sekido, H.; Kubota, K.; Sugita, M.; Tanaka, K.; Togo, S.; Yamanaka, S.; Sasaki, T.; Inayama, Y.; Shimada, H. Antibody-Mediated Rejection after Adult ABO-Incompatible Liver Transplantation Remedied by Gamma-Globulin Bolus Infusion Combined with Plasmapheresis. Transplantation 2004, 78, 1225–1228. [Google Scholar] [CrossRef]
- Neil, D.A.H.; Bellamy, C.O.; Smith, M.; Haga, H.; Zen, Y.; Sebagh, M.; Ruppert, K.; Lunz, J.; Hübscher, S.G.; Demetris, A.J. Global quality assessment of liver allograft C4d staining during acute antibody-mediated rejection in formalin-fixed, paraffin-embedded tissue. Hum. Pathol. 2018, 73, 144–155. [Google Scholar] [CrossRef] [Green Version]
- Snell, E.J. A Scaling Procedure for Ordered Categorical Data. Biometrics 1964, 20, 592–607. [Google Scholar] [CrossRef]
- Bell, R.M.; McCaffrey, D. Bias reduction in standard errors for linear regression with multi-stage samples. Surv. Methodol. 2002, 28, 169–181. [Google Scholar]
- Gordon, R.D.; Iwatsuki, S.; Esquivel, C.O.; Tzakis, A.; Todo, S.; Starzl, T.E. Liver transplantation across ABO blood groups. Surgery 1986, 100, 342–348. [Google Scholar]
- Hanto, D.W.; Fecteau, A.H.; Alonso, M.H.; Valente, J.F.; Whiting, J.F. ABO-incompatible liver transplantation with no immunological graft losses using total plasma exchange, splenectomy, and quadruple immunosuppression: Evidence for accommodation. Liver Transpl. 2003, 9, 22–30. [Google Scholar] [CrossRef]
- Stegall, M. ABO-incompatible liver transplant: Is it justifiable? Liver Transplant. 2003, 9, 31. [Google Scholar] [CrossRef]
- Usuda, M.; Fujimori, K.; Ishida, K.; Moriya, T.; Satomi, S.; Koyamada, N.; Fukumori, T.; Sekiguchi, S.; Kawagishi, N.; Akamatsu, Y.; et al. Successful Use of Anti-CD20 Monoclonal Antibody (Rituximab) for ABO-Incompatible Living-Related Liver Transplantation. Transplantation 2005, 79, 12–16. [Google Scholar] [CrossRef]
- Egawa, H.; Teramukai, S.; Haga, H.; Tanabe, M.; Fukushima, M.; Shimazu, M. Present status of ABO-incompatible living donor liver transplantation in Japan. Hepatology 2007, 47, 143–152. [Google Scholar] [CrossRef]
- Egawa, H.; Ohmori, K.; Haga, H.; Tsuji, H.; Yurugi, K.; Miyagawa-Hayashino, A.; Oike, F.; Fukuda, A.; Yoshizawa, J.; Takada, Y.; et al. B-cell surface marker analysis for improvement of rituximab prophylaxis in ABO-incompatible adult living donor liver transplantation. Liver Transplant. 2007, 13, 579–588. [Google Scholar] [CrossRef]
- Tanaka, A.; Tanaka, K.; Kitai, T.; Yanabu, N.; Tokuka, A.; Sato, B.; Mori, S.; Inomoto, T.; Shinohara, H.; Uemoto, S. Evaluation of circulation status with tissue near-infrared spectroscopy in living related liver transplantation across ABO blood groups. Transplantation 1995, 58, 548–553. [Google Scholar] [CrossRef]
- Varela-Fascinetto, G.; Treacy, S.; Lillehei, C.; Jonas, M.; Lund, D.; Kevy, S.; Pérez, A.; Zurakowski, D.; Vacanti, J. Long-term results in pediatric ABO-incompatible liver transplantation. Transplant. Proc. 1999, 31, 467–468. [Google Scholar] [CrossRef]
- Szymczak, M.; Kalicinski, P.; Kaminski, A.; Ismail, H.; Drewniak, T.; Nachulewicz, P.; Broniszczak-Czyszek, D. Liver transplantation across ABO blood groups in children. Transplant. Proc. 2003, 35, 2273–2274. [Google Scholar] [CrossRef] [PubMed]
- Cacciarelli, T.V.; So, S.K.; Lim, J.; Concepcion, W.; Cox, K.; Esquivel, C.O. A reassessment of ABO incompatibility in pediatric liver transplantation. Transplantion 1995, 60, 757–760. [Google Scholar] [CrossRef] [PubMed]
- Tokunaga, Y.; Tanaka, K.; Fujita, S.; Yamaguchi, T.; Savvada, H.I.; Kato, H.; Uemoto, S.; Yamaoka, Y.; Ozawa, K. Living related liver transplantation across ABO blood groups with FK506 and OKT3. Transpl. Int. 1993, 6, 313–318. [Google Scholar] [CrossRef]
- Gelas, T.; McKiernan, P.J.; Kelly, D.A.; Mayer, D.A.; Mirza, D.F.; Sharif, K. ABO-incompatible pediatric liver transplantation in very small recipients: Birmingham’s experience. Pediatr. Transplant. 2011, 15, 706–711. [Google Scholar] [CrossRef] [PubMed]
- Egawa, H.; Oike, F.; Buhler, L.; Shapiro, A.M.J.; Minamiguchi, S.; Haga, H.; Uryuhara, K.; Kiuchi, T.; Kaihara, S.; Tanaka, K. Impact of recipient age on outcome of ABO-incompatible living-donor liver transplantation. Transplantation 2004, 77, 403–411. [Google Scholar] [CrossRef]
- Eastlund, T. The histo-blood group ABO system and tissue transplantation. Transfusion 2003, 38, 975–988. [Google Scholar] [CrossRef] [PubMed]
- Yamada, Y.; Hoshino, K.; Morikawa, Y.; Okamura, J.; Hotta, R.; Komori, K.; Nakao, S.; Obara, H.; Kawachi, S.; Fuchimoto, Y.; et al. Successful liver transplantation across the ABO incompatibility barrier in 6 cases of biliary atresia. J. Pediatr. Surg. 2006, 41, 1976–1979. [Google Scholar] [CrossRef]
- Collins, A.B.; Schneeberger, E.E.; Pascual, M.A.; Saidman, S.L.; Williams, W.W.; Tolkoff-Rubin, N.; Cosimi, A.B.; Colvin, R.B. Complement activation in acute humoral renal allograft rejection: Diagnostic significance of C4d deposits in peritubular capillaries. J. Am. Soc. Nephrol. 1999, 10, 2208–2214. [Google Scholar] [CrossRef]
- Behr, T.M.; Feucht, H.E.; Richter, K.; Reiter, C.; Spes, C.H.; Pongratz, D.; Überfuhr, P.; Meiser, B.; Theisen, K.; Angermann, C.E. Detection of humoral rejection in human cardiac allografts by assessing the capillary deposition of complement fragment C4d in endomyocardial biopsies. J. Heart Lung Transplant. 1999, 18, 904–912. [Google Scholar] [CrossRef]
- Haga, H.; Egawa, H.; Fujimoto, Y.; Ueda, M.; Miyagawa-Hayashino, A.; Sakurai, T.; Okuno, T.; Koyanagi, I.; Takada, Y.; Manabe, T. Acute humoral rejection and C4d immunostaining in ABO blood type-incompatible liver transplantation. Liver Transplant. 2006, 12, 457–464. [Google Scholar] [CrossRef] [PubMed]



| ABOi LDLT (n = 34) | ABOc LDLT (n = 68) | p-Value | |
|---|---|---|---|
| Transplantation date | +129 days of median delay (compared to ABOc LDLT) | 0.18 (NS) | |
| Recipient sex | 17 girls/17 boys | 36 girls/32 boys | 0.79 (NS) |
| Median recipient age at transplantation (years) | 0.95 | 0.98 | 0.10 (NS) |
| Median recipient weight (kg) | 8.7 | 8 | 0.32 (NS) |
| Median recipient height (cm) | 71.7 | 70.7 | 0.98 (NS) |
| Median recipient PELD | 17 | 20 | 0.25 (NS) |
| Median donor age (years) | 31 | 34 | 0.28 (NS) |
| Median ischemia time (min) | 141 | 151 | 0.58 (NS) |
| Median graft weight/recipient weight (%) | 2.9 | 3.1 | 0.50 (NS) |
| ABOi LT (n = 34) | Matched ABOc LT (n = 68) | Hazard Ratio ABOi/ABOc (95% CI) | p-Value | |
|---|---|---|---|---|
| Hepatic artery complications | 2 (5.9%) | 4 (5.9%) | 1 (0.2–4.6) | NS |
| Portal vein complications | 3 (8.8%) | 5 (7.3%) | 1.2 (0.2–6.1) | NS |
| Budd–Chiari syndrome | 1 (2.9%) | 1 (1.5%) | 1.3 (0.1–13.8) | NS |
| Biliary complications | 13 (38.2%) | 11 (16.2%) | 3.2 (1.2–8.7) | <0.05 |
| Acute cellular rejection | 22 (64.7%) | 34 (50%) | 1.7 (0.7–4) | NS |
| Acute cellular rejection steroid resistant | 4 (11.8%) | 3 (4.4%) | 2.9 (0.5–15.6) | NS |
| Acute humoral rejection | 4 (11.8%) | 0 (0%) | - | <0.01 |
| Chronic rejection | 0 (0%) | 0 (0%) | - | NS |
| Post-LT lymphoproliferative disease | 3 (8.8%) | 4 (5.9%) | 1.5 (0.3–6.7) | NS |
| Retransplantation | 3 (8.8%) | 0 (0%) | 14 (1.5–132.9) | <0.05 |
| Death | 0 (0%) | 3 (4.4%) | 0.3 (0.02–4.6) | NS |
| ABOi LT Recipients <1 Year Old (n = 18) | ABOi LT Recipients ≥1 Year Old (n = 16) | Hazard Ratio Children ≥1 Year/Children <1 Year (95% CI) | p-Value | |
|---|---|---|---|---|
| Hepatic artery complications | 1 (5.5%) | 1 (6.2%) | 1.1 (0.01–94) | NS |
| Portal vein complications | 2 (11.1%) | 1 (6.2%) | 0.5 (0.008–11.4) | NS |
| Budd–Chiari syndrome | 0 (0%) | 1 (6.2%) | - | NS |
| Biliary complications | 5 (27.8%) | 8 (50%) | 2.5 (0.5–13.8) | NS |
| Acute cellular rejection | 13 (72.2%) | 11 (68.7%) | 0.8 (0.1–4.8) | NS |
| Acute cellular rejection steroid resistant | 2 (11.1%) | 2 (12.5%) | 1.1 (0.07–17.6) | NS |
| Acute humoral rejection | 1 (5.5%) | 3 (18.7%) | 3.7 (0.3–217.5) | NS |
| Chronic rejection | 0 (0%) | 0 (0%) | - | NS |
| Post-LT lymphoproliferative disease | 2 (11.1%) | 1 (6.2%) | 0.5 (0.008–11.5) | NS |
| Retransplantation | 0 (0%) | 3 (18.7%) | - | NS (p = 0.09) |
| Death | 0 (0%) | 0 (0%) | - | NS |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
de Magnée, C.; Brunée, L.; Tambucci, R.; Pire, A.; Scheers, I.; Sokal, E.M.; Baldin, P.; Zech, F.; Eeckhoudt, S.; Reding, R.; et al. Is ABO-Incompatible Living Donor Liver Transplantation Really a Good Alternative for Pediatric Recipients? Children 2021, 8, 600. https://0-doi-org.brum.beds.ac.uk/10.3390/children8070600
de Magnée C, Brunée L, Tambucci R, Pire A, Scheers I, Sokal EM, Baldin P, Zech F, Eeckhoudt S, Reding R, et al. Is ABO-Incompatible Living Donor Liver Transplantation Really a Good Alternative for Pediatric Recipients? Children. 2021; 8(7):600. https://0-doi-org.brum.beds.ac.uk/10.3390/children8070600
Chicago/Turabian Stylede Magnée, Catherine, Louise Brunée, Roberto Tambucci, Aurore Pire, Isabelle Scheers, Etienne M. Sokal, Pamela Baldin, Francis Zech, Stéphane Eeckhoudt, Raymond Reding, and et al. 2021. "Is ABO-Incompatible Living Donor Liver Transplantation Really a Good Alternative for Pediatric Recipients?" Children 8, no. 7: 600. https://0-doi-org.brum.beds.ac.uk/10.3390/children8070600