Multidisciplinary In-Depth Investigation in a Young Athlete Suffering from Syncope Caused by Myocardial Bridge
Abstract
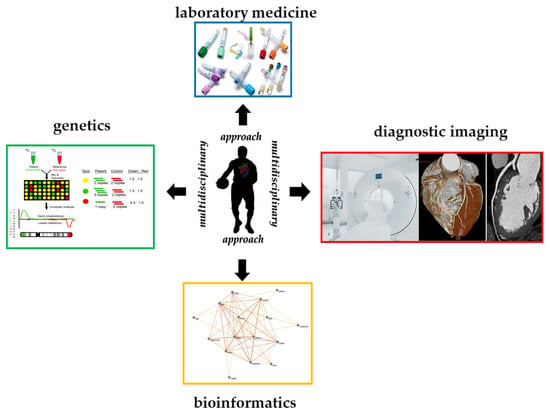
:1. Introduction
2. Materials and Methods
2.1. Ethical Approval
2.2. Cardiovascular Evaluation
- (1)
- Standard clinical evaluation, as a part of the pre-participation screening, which consisted of family and personal history, physical examination, electrocardiogram (ECG) and stress test, according to the current recommendations [34];
- (2)
- Additional clinical investigations in the presence of one or more clinical or instrumental markers suggestive of a pathologic condition potentially associated with an increased risk of sudden cardiac death during physical activity. The additional investigations included echocardiography, 24–48 ECG Holter, electrophysiological study, coronary computed tomographic angiogram (CTA) and exercise echocardiogram.
2.3. Clinical Laboratory Analysis
2.4. Genetic Test: Array-Comparative Genomic Hybridization
2.5. Genetic Test: Whole Exome Sequencing and DNA Variants Analysis
2.6. Genetic Test: Prediction of Disease-Causing Variant Combinations and Network Representation
3. Results
3.1. Clinical History
3.2. Instrumental Results
3.3. Clinical Laboratory Analysis
3.4. Analysis of Array-CGH
3.5. Exome Sequencing
3.6. Pathogenic Variant Predictions and Oligogenic Combination Network
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Lombardo, B.; Izzo, V.; Terracciano, D.; Ranieri, A.; Mazzaccara, C.; Fimiani, F.; Cesaro, A.; Gentile, L.; Leggiero, E.; Pero, R.; et al. Laboratory medicine: Health evaluation in elite athletes. Clin. Chem. Lab. Med. 2019, 57, 1450–1473. [Google Scholar] [CrossRef] [PubMed]
- Clénin, G.E.; Cordes, M. Laboratory analyses in sports medicine. Ther. Umsch. 2015, 72, 311–319. [Google Scholar] [CrossRef] [PubMed]
- Detta, N.; Frisso, G.; Limongelli, G.; Marzullo, M.; Calabrò, R.; Salvatore, F. Genetic analysis in a family affected by sick sinus syndrome may reduce the sudden death risk in a young aspiring competitive athlete. Int. J. Cardiol. 2014, 170, e63–e65. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mennitti, C.; Brancaccio, M.; Gentile, L.; Ranieri, A.; Terracciano, D.; Cennamo, M.; La Civita, E.; Liotti, A.; D’Alicandro, G.; Mazzaccara, C.; et al. Athlete’s Passport: Prevention of Infections, Inflammations, Injuries and Cardiovascular Diseases. J. Clin. Med. 2020, 9, 2540. [Google Scholar] [CrossRef] [PubMed]
- Barretta, F.; Mirra, B.; Monda, E.; Caiazza, M.; Lombardo, B.; Tinto, N.; Scudiero, O.; Frisso, G.; Mazzaccara, C. The Hidden Fragility in the Heart of the Athletes: A Review of Genetic Biomarkers. Int. J. Mol. Sci. 2020, 21, 6682. [Google Scholar] [CrossRef]
- Scudiero, O.; Gentile, L.; Ranieri, A.; Coppola, E.; Di Micco, P.; Mazzaccara, C.; D’alicandro, G.; Leggiero, E.; Frisso, G.; Pastore, L.; et al. Physical Activity and Thrombophilic Risk in a Short Series. J. Blood Med. 2020, 11, 39–42. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hull, C.M.; Harris, J.A. Venous Thromboembolism and Marathon Athletes. Circulation 2013, 128, e469–e471. [Google Scholar] [CrossRef]
- Ragozzino, E.; Brancaccio, M.; Di Costanzo, A.; Scalabrì, F.; Andolfi, G.; Wanderlingh, L.G.; Patriarca, E.J.; Minchiotti, G.; Altamura, S.; Summa, V.; et al. 6-Bromoindirubin-3′-oxime intercepts GSK3 signaling to promote and enhance skeletal muscle differentiation affecting miR-206 expression in mice. Sci. Rep. 2019, 9, 18091. [Google Scholar] [CrossRef]
- Poor, A.E.; Roedl, J.B.; Zoga, A.C.; Meyers, W.C. Core Muscle Injuries in Athletes. Curr. Sports Med. Rep. 2018, 17, 54–58. [Google Scholar] [CrossRef]
- Brancaccio, M.; Mennitti, C.; Laneri, S.; Franco, A.; De Biasi, M.G.; Cesaro, A.; Fimiani, F.; Moscarella, E.; Gragnano, F.; Mazzaccara, C.; et al. Methicillin-Resistant Staphylococcus aureus: Risk for General Infection and Endocarditis among Athletes. Antibiotics 2020, 9, 332. [Google Scholar] [CrossRef]
- Scudiero, O.; Brancaccio, M.; Mennitti, C.; Laneri, S.; Lombardo, B.; De Biasi, M.G.; De Gregorio, E.; Pagliuca, C.; Colicchio, R.; Salvatore, P.; et al. Human Defensins: A Novel Approach in the Fight against Skin Colonizing Staphylococcus aureus. Antibiotics 2020, 9, 198. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Scudiero, O.; Lombardo, B.; Brancaccio, M.; Mennitti, C.; Cesaro, A.; Fimiani, F.; Gentile, L.; Moscarella, E.; Amodio, F.; Ranieri, A.; et al. Exercise, Immune System, Nutrition, Respiratory and Cardiovascular Diseases during COVID-19: A Complex Combination. Int. J. Environ. Res. Public Health 2021, 18, 904. [Google Scholar] [CrossRef] [PubMed]
- Laneri, S.; Brancaccio, M.; Mennitti, C.; De Biasi, M.G.; Pero, M.E.; Pisanelli, G.; Scudiero, O.; Pero, R. Antimicrobial Peptides and Physical Activity: A Great Hope against COVID 19. Microorganisms 2021, 9, 1415. [Google Scholar] [CrossRef]
- Brancaccio, M.; Mennitti, C.; Cesaro, A.; Fimiani, F.; Moscarella, E.; Caiazza, M.; Gragnano, F.; Ranieri, A.; D’Alicandro, G.; Tinto, N.; et al. Dietary Thiols: A Potential Supporting Strategy against Oxidative Stress in Heart Failure and Muscular Damage during Sports Activity. Int. J. Environ. Res. Public Health 2020, 17, 9424. [Google Scholar] [CrossRef]
- Lee, E.C.; Fragala, M.S.; Kavouras, S.A.; Queen, R.M.; Pryor, J.L.; Casa, D.J. Biomarkers in Sports and Exercise: Tracking Health, Performance, and Recovery in Athletes. J. Strength Cond. Res. 2017, 31, 2920–2937. [Google Scholar] [CrossRef] [Green Version]
- Pero, R.; Brancaccio, M.; Mennitti, C.; Gentile, L.; Arpino, S.; De Falco, R.; Leggiero, E.; Ranieri, A.; Pagliuca, C.; Colicchio, R.; et al. Urinary Biomarkers: Diagnostic Tools for Monitoring Athletes’ Health Status. Int. J. Environ. Res Public Health 2020, 17, 6065. [Google Scholar] [CrossRef]
- Pero, R.; Brancaccio, M.; Mennitti, C.; Gentile, L.; Franco, A.; Laneri, S.; De Biasi, M.G.; Pagliuca, C.; Colicchio, R.; Salvatore, P.; et al. HNP-1 and HBD-1 as Biomarkers for the Immune Systems of Elite Basketball Athletes. Antibiotics 2020, 9, 306. [Google Scholar] [CrossRef] [PubMed]
- Papa, L.; Ramia, M.M.; Edwards, D.; Johnson, B.D.; Slobounov, S.M. Systematic Review of Clinical Studies Examining Biomarkers of Brain Injury in Athletes after Sports-Related Concussion. J. Neurotrauma 2015, 32, 661–673. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shin, K.A.; Parkm, K.D.; Ahn, J.; Park, Y.B.; Kim, Y.J. Comparison of Changes in Biochemical Markers for Skeletal Muscles; Hepatic Metabolism; and Renal Function after Three Types of Long-distance Running: Observational Study. Medicine 2016, 95, e3657. [Google Scholar] [CrossRef] [PubMed]
- Djaoui, L.; Haddad, M.; Chamari, K.; Dellal, A. Monitoring training load and fatigue in soccer players with physiological markers. Physiol. Behav. 2017, 181, 86–94. [Google Scholar] [CrossRef]
- Brancaccio, P.; Maffulli, N.; Limongelli, F.M. Creatine kinase monitoring in sport medicine. Br. Med. Bull. 2007, 81, 209–230. [Google Scholar] [CrossRef]
- Girolami, F.; Frisso, G.; Benelli, M.; Crotti, L.; Iascone, M.; Mango, R.; Mazzaccara, C.; Pilichou, K.; Arbustini, E.; Tomberli, B.; et al. Contemporary genetic testing in inherited cardiac disease: Tools; ethical issues; and clinical applications. J. Cardiovasc. Med. 2018, 19, 1–11. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kraemer, W.J.; Ratamess, N.A.; Hymer, W.C.; Nindl, B.C.; Fragala, M.S. Growth Hormone(s), Testosterone, Insulin-Like Growth Factors, and, Cortisol: Roles and Integration for Cellular Development and Growth With Exercise. Front. Endocrinol. 2020, 11, 33. [Google Scholar] [CrossRef] [PubMed]
- Barbara, M.; Anna, K.; Agnieszka, Z.L. The Impact of Professional Sports Activity on GH-IGF-I Axis in Relation to Testosterone Level. Am. J. Mens. Health 2020, 14. [Google Scholar] [CrossRef] [Green Version]
- Abrams, G.D.; Feldman, D.; Safran, M.R. Effects of Vitamin D on Skeletal Muscle and Athletic Performance. J. Am. Acad. Orthop. Surg. 2018, 26, 278–285. [Google Scholar] [CrossRef]
- Owens, D.J.; Allison, R.J.; Close, G.L. Vitamin D and the Athlete: Current Perspectives and New Challenges. Sports Med. 2018, 48 (Suppl. 1), 3–16. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fogante, M.; Agliata, G.; Basile, M.C.; Compagnucci, P.; Volpato, G.; Falanga, U.; Stronati, G.; Guerra, F.; Vignale, D.; Esposito, A.; et al. Cardiac Imaging in Athlete’s Heart: The Role of the Radiologist. Medicina 2021, 57, 455. [Google Scholar] [CrossRef] [PubMed]
- De Innocentiis, C.; Ricci, F.; Khanji, M.Y.; Aung, N.; Tana, C.; Verrengia, E.; Petersen, S.E.; Gallina, S. Athlete’s Heart: Diagnostic Challenges and Future Perspectives. Sports Med. 2018, 48, 2463–2477. [Google Scholar] [CrossRef] [PubMed]
- Thorborg, K.; Reiman, M.P.; Weir, A.; Kemp, J.L.; Serner, A.; Mosler, A.B.; Hölmich, P. Clinical Examination; Diagnostic Imaging; and Testing of Athletes With Groin Pain: An Evidence-Based Approach to Effective Management. J. Orthop. Sports Phys. Ther. 2018, 4, 239–249. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Justin, W.; Arner, J.W.; Li, R.; Disantis, A.; Zuckerbraun, B.S.; Mauro, C.S. Evaluation and treatment of groin pain syndromes in athletes. Ann. Jt. 2020, 5, 17. [Google Scholar]
- Coris, E.E.; Moran, B.K.; De Cuba, R.; Farrar, T.; Curtis, A.B. Left ventricular non-compaction in athletes: To play or not to play. Sports Med. 2016, 46, 1249–1259. [Google Scholar] [CrossRef]
- Limongelli, G.; Nunziato, M.; D’Argenio, V.; Esposito, M.V.; Monda, E.; Mazzaccara, C.; Caiazza, M.; D’Aponte, A.; D’Andrea, A.; Bossone, E.; et al. Yield and clinical significance of genetic screening in elite and amateur athletes. Eur. J. Prev. Cardiol. 2020, 2, 1081–1090. [Google Scholar] [CrossRef] [PubMed]
- Limongelli, G.; Monda, E.; Nunziato, M.; Salvatore, F. Genetic evaluation in athletes and cascade family screening: Reply. Eur. J. Prev. Cardiol. 2021, 22, zwaa150. [Google Scholar] [CrossRef] [PubMed]
- Mont, L.; Pelliccia, A.; Sharma, S.; Biffi, A.; Borjesson, M.; Brugada Terradellas, J.; Carré, F.; Guasch, E.; Heidbuchel, H.; La Gerche, A.; et al. Pre-participation cardiovascular evaluation for athletic participants to prevent sudden death: Position paper from the EHRA and the EACPR; branches of the ESC. Endorsed by APHRS; HRS; and SOLAECE. Eur. J. Prev. Cardiol. 2017, 24, 41–69. [Google Scholar] [CrossRef]
- Richards, S.; Aziz, N.; Bale, S.; Bick, D.; Das, S.; Gastier-Foster, J.; Grody, W.W.; Hegde, M.; Lyon, E.; Spector, E.; et al. Standards and guidelines for the interpretation of sequence variants: A joint consensus recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Genet. Med. 2015, 17, 405–424. [Google Scholar] [CrossRef]
- Renaux, A.; Papadimitriou, S.; Versbraegen, N.; Nachtegael, C.; Boutry, S.; Nowé, A.; Smits, G.; Lenaerts, T. ORVAL: A novel platform for the prediction and exploration of disease-causing oligogenic variant combinations. Nucleic Acids Res. 2019, 47, W93–W98. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bomba, L.; Walter, K.; Soranzo, N. The impact of rare and low-frequency genetic variants in common disease. Genome Biol. 2017, 18, 77. [Google Scholar] [CrossRef]
- Papadimitriou, S.; Gazzo, A.; Versbraegen, N.; Nachtegael, C.; Aerts, J.; Moreau, Y.; Van Dooren, S.; Nowé, A.; Smits, G.; Lenaerts, T. Predicting disease-causing variant combinations. Proc. Natl. Acad. Sci. USA 2019, 116, 11878–11887. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gazzo, A.M.; Daneels, D.; Cilia, E.; Bonduelle, M.; Abramowicz, M.; Van Dooren, S.; Smits, G.; Lenaerts, T. DIDA: A curated and annotated digenic diseases database. Nucleic Acids Res. 2016, 44, D900–D907. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Itan, Y.; Shang, L.; Boisson, B.; Patin, E.; Bolze, A.; Moncada-Vélez, M.; Scott, E.; Ciancanelli, M.J.; Lafaille, F.G.; Markle, J.G.; et al. The human gene damage index as a gene-level approach to prioritizing exome variants. Proc. Natl. Acad. Sci. USA 2015, 112, 13615–13620. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Versbraegen, N.; Fouché, A.; Nachtegael, C.; Papadimitriou, S.; Gazzo, A.; Smits, G.; Lenaerts, T. Using game theory and decision decomposition to effectively discern and characterise bi-locus diseases. Artif. Intell. Med. 2019, 99, 101690. [Google Scholar] [CrossRef] [PubMed]
- Gazzo, A.; Raimondi, D.; Daneels, D.; Moreau, Y.; Smits, G.; Van Dooren, S.; Lenaerts, T. Understanding mutational effects in digenic diseases. Nucleic Acids Res. 2017, 45, e140. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Veres, D.V.; Gyurkó, D.M.; Thaler, B.; Szalay, K.Z.; Fazekas, D.; Korcsmáros, T.; Csermely, P. ComPPI: A cellular compartment-specific database for protein-protein interaction network analysis. Nucleic Acids Res. 2015, 43, D485–D493. [Google Scholar] [CrossRef] [Green Version]
- Corrado, D.; Pelliccia, A.; Bjørnstad, H.H.; Vanhees, L.; Biffi, A.; Borjesson, M.; Panhuyzen-Goedkoop, N.; Deligiannis, A.; Solberg, E.; Dugmore, D.; et al. Cardiovascular pre-participation screening of young competitive athletes for prevention of sudden death: Proposal for a common European protocol. Consensus Statement of the Study Group of Sport Cardiology of the Working Group of Cardiac Rehabilitation and Exercise Physiology and the Working Group of Myocardial and Pericardial Diseases of the European Society of Cardiology. Eur. Heart J. 2005, 26, 516–524. [Google Scholar] [PubMed] [Green Version]
- Brignole, M.; Moya, A.; de Lange, F.J.; Deharo, J.C.; Elliott, P.M.; Fanciulli, A.; Fedorowski, A.; Furlan, R.; Kenny, R.A.; Martín, A.; et al. 2018 ESC Guidelines for the diagnosis and management of syncope. Eur. Heart J. 2018, 39, 1883–1948. [Google Scholar] [CrossRef]
- Šupak-Smolčić, V.; Antončić, D.; Ožanić, D.; Vladilo, I.; Bilić-Zulle, L. Influence of a prolonged fasting and mild activity on routine laboratory tests. Clin. Biochem. 2015, 48, 85–88. [Google Scholar] [CrossRef]
- Lombardo, B.; D’Argenio, V.; Monda, E.; Vitale, A.; Caiazza, M.; Sacchetti, L.; Pastore, L.; Limongelli, G.; Frisso, G.; Mazzaccara, C. Genetic analysis resolves differential diagnosis of a familial syndromic dilated cardiomyopathy: A new case of Alström syndrome. Mol. Genet. Genom. Med. 2020, 8, e1260. [Google Scholar] [CrossRef]
- Woolf, K.; St Thomas, M.M.; Hahn, N.; Vaughan, L.A.; Carlson, A.G.; Hinton, P. Iron status in highly active and sedentary young women. Int. J. Sport Nutr. Exerc. Metab. 2009, 1, 519–535. [Google Scholar] [CrossRef] [PubMed]
- Cohen-Solal, A.; Leclercq, C.; Deray, G.; Lasocki, S.; Zambrowski, J.J.; Mebazaa, A.; de Groote, P.; Damy, T.; Galinier, M. Iron deficiency: An emerging therapeutic target in heart failure. Heart 2014, 100, 1414–1420. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mazzaccara, C.; Limongelli, G.; Petretta, M.; Vastarella, R.; Pacileo, G.; Bonaduce, D.; Salvatore, F.; Frisso, G. A common polymorphism in the SCN5A gene is associated with dilated cardiomyopathy. J. Cardiovasc. Med. 2018, 19, 344–350. [Google Scholar] [CrossRef] [PubMed]
- Skierka, J.M.; Kotzer, K.E.; Lagerstedt, S.A.; O’Kane, D.J.; Baudhuin, L.M.J. UGT1A1 genetic analysis as a diagnostic aid for individuals with unconjugated hyperbilirubinemia. J. Pediatr. 2013, 6, 1146–1152. [Google Scholar] [CrossRef] [PubMed]
- Stojanović, E.; Radovanović, D.; Hew-Butler, T.; Hamar, D.; Jakovljević, V. Vitamin D in Basketball Players: Current Evidence and Future Directions. Sports Health 2021, 4. [Google Scholar] [CrossRef]
- Hamilton, B. Vitamin D and human skeletal muscle. Scand. J. Med. Sci. Sport. 2010, 20, 182–190. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gordon-thomson, C.; Tongkao-on, W.; Mason, R.S. Vitamin D and its role in. Curr. Opin. Clin. Nutr. Metab. Care 2001, 12, 165–184. [Google Scholar]
- Lombardi, G.; Vitale, J.A.; Logoluso, S.; Logoluso, G.; Cocco, N.; Cocco, G.; Banfi, G. Circannual rhythm of plasmatic vitamin D levels and the association with markers of psychophysical stress in a cohort of Italyn professional soccer players. Chronobiol. Int. 2017, 34, 471–479. [Google Scholar] [CrossRef] [PubMed]
- Longstrom, J.M.; Colenso-Semple, L.M.; Waddell, B.J.; Mastrofini, G.; Trexler, E.T.; Campbell, B.I. Physiological; Psychological and Performance-Related Changes Following Physique Competition: A Case-Series. J. Funct. Morphol. Kinesiol. 2020, 5, 27. [Google Scholar] [CrossRef] [PubMed]
- Larson-Meyer, D.E.; Gostas, D.E. Thyroid Function and Nutrient Status in the Athlete. Curr. Sports Med. Rep. 2020, 19, 84–94. [Google Scholar] [CrossRef] [PubMed]
- Garber, J.R.; Cobin, R.H.; Gharib, H.; Hennessey, J.V.; Klein, I.; Mechanick, J.I.; Pessah-Pollack, R.; Singer, P.A.; Woeber, K.A.; American Association of Clinical Endocrinologists and American Thyroid Association Taskforce on Hypothyroidism in Adults. Clinical practice guidelines for hypothyroidism in adults: Cosponsored by the American Association of Clinical Endocrinologists and the American Thyroid Association. Endocr. Pract. 2012, 18, 988–1028. [Google Scholar] [CrossRef] [Green Version]
- Ross, D.S. Laboratory Assessment of Thyroid Function; Wolters Kluwer; UpToDate, Inc.: Waltham, MA, USA, 2017. [Google Scholar]
- Babić Leko, M.; Gunjača, I.; Pleić, N.; Zemunik, T. Environmental Factors Affecting Thyroid-Stimulating Hormone and Thyroid Hormone Levels. Int. J. Mol. Sci. 2021, 22, 6521. [Google Scholar] [CrossRef] [PubMed]
- Huang, W.S.; Yu, M.D.; Lee, M.S.; Cheng, C.Y.; Yang, S.P.; Chin, H.M.L.; Wu, S.Y. Effect of treadmill exercise on circulating thyroid hormone measurements. Med. Princ. Pract. 2004, 13, 15–19. [Google Scholar] [CrossRef] [Green Version]
- Benso, A.; Broglio, F.; Aimaretti, G.; Lucatello, B.; Lanfranco, F.; Ghigo, E.; Grottoli, S. Endocrine and metabolic responses to extreme altitude and physical exercise in climbers. Eur. J. Endocrinol. 2007, 157, 733–740. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Altaye, K.Z.; Mondal, S.; Legesse, K.; Abdulkedir, M. Effects of aerobic exercise on thyroid hormonal change responses among adolescents with intellectual disabilities. BMJ Open Sport Exerc. Med. 2019, 5, 524. [Google Scholar] [CrossRef] [Green Version]
- Ciloglu, F.; Peker, I.; Pehlivan, A.; Karacabey, K.; Ilhan, N.; Sayglin, O.; Ozmerdivenli, R. Exercise intensity and its effects on thyroid hormones. Neuro Endocrinol. Lett. 2005, 26, 830–834. [Google Scholar]
- Moro, T.; Tinsley, G.; Bianco, A.; Marcolin, G.; Pacelli, Q.F.; Battaglia, G.; Palma, A.; Gentil, P.; Neri, M.; Paoli, A. Effects of eight weeks of time-restricted feeding (16/8) on basal metabolism; maximal strength; body composition; inflammation; and cardiovascular risk factors in resistance-trained males. J. Transl. Med. 2016, 14, 290. [Google Scholar] [CrossRef]
- Stratton, M.T.; Tinsley, G.M.; Alesi, M.G.; Hester, G.M.; Olmos, A.A.; Serafini, P.R.; Modjeski, A.S.; Mangine, G.T.; King, K.; Savage, S.N.; et al. Four Weeks of Time-Restricted Feeding Combined with Resistance Training Does Not Differentially Influence Measures of Body Composition; Muscle Performance; Resting Energy Expenditure; and Blood Biomarkers. Nutrients. 2020, 12, 1126. [Google Scholar] [CrossRef] [PubMed]
- Narla, A.; Kaiser, K.; Tannock, L.R. Extremely low testosterone due to relative energy deficiency in sport: A case report. AACE Clin. Case Rep. 2018, 5, e129–e131. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hostiuc, S.; Rusu, M.C.; Hostiuc, M.; Negoi, R.I.; Negoi, I. Cardiovascular consequences of myocardial bridging: A meta-analysis and meta-regression. Sci. Rep. 2017, 7, 14644. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Corrado, D.; Thiene, G.; Cocco, P.; Frescura, C. Non-atherosclerotic coronary artery disease and sudden death in the young. Br. Heart J. 1992, 68, 601–607. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pelliccia, A.; Sharma, S.; Gati, S.; Back, M.; Borjesson, M.; Caselli, S.; Collet, J.P.; Corrado, D.; Drezner, J.A.; Halle, M.; et al. 2020 ESC Guidelines on sports cardiology and exercise in patients with cardiovascular disease. Eur. Heart J. 2021, 42, 17–96. [Google Scholar] [CrossRef] [PubMed]
- Sanna, V.; Ceglia, C.; Tarsitano, M.; Lombardo, B.; Coppola, A.; Zarrilli, F.; Castaldo, G.; Di Minno, G. Aberrant F8 gene intron 1 inversion with concomitant duplication and deletion in a severe hemophilia A patient from Southern Italy. J. Thromb. Haemost. 2013, 11, 195–197. [Google Scholar] [CrossRef] [PubMed]
- Iossa, S.; Costa, V.; Corvino, V.; Auletta, G.; Barruffo, L.; Cappellani, S.; Ceglia, C.; Cennamo, G.; D’Adamo, A.P.; D’Amico, A.; et al. Phenotypic and genetic characterization of a family carrying two Xq21.1–21.3 interstitial deletions associated with syndromic hearing loss. Mol. Cytogenet. 2015, 8, 18. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lahm, H.; Jia, M.; Dreßen, M.; Wirth, F.; Puluca, N.; Gilsbach, R.; Keavney, B.D.; Cleuziou, J.; Beck, N.; Bondareva, O.; et al. Congenital heart disease risk loci identified by genome-wide association study in European patients. J. Clin. Investig. 2021, 131, e141837. [Google Scholar] [CrossRef] [PubMed]
- Ware, A.W.; Cheung, T.T.; Rasulov, S.; Burstein, E.; McDonald, F.J. Epithelial NaC Channel: Reciprocal Control by COMMD10 and Nedd4-2. Front. Physiol. 2018, 9, 793. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fan, Y.; Zhang, L.; Sun, Y.; Yang, M.; Wang, X.; Wu, X.; Huang, W.; Chen, L.; Pan, S.; Guan, J. Expression profile and bioinformatics analysis of COMMD10 in BALB/C mice and human. Cancer Gene Ther. 2020, 27, 216–225. [Google Scholar] [CrossRef]
- Schlieben, L.D.; Prokisch, H.; Yépez, V.A. How Machine Learning and Statistical Models Advance Molecular Diagnostics of Rare Disorders via Analysis of RNA Sequencing Data. Front. Mol. Biosci. 2021, 8, 647277. [Google Scholar] [CrossRef] [PubMed]
- Krittanawong, C.; Virk, H.U.H.; Bangalore, S.; Wang, Z.; Johnson, K.W.; Pinotti, R.; Zhang, H.; Kaplin, S.; Narasimhan, B.; Kitai, T.; et al. Machine learning prediction in cardiovascular diseases: A meta-analysis. Sci. Rep. 2020, 10, 16057. [Google Scholar] [CrossRef]
- 1000 Genomes Project Consortium; Auton, A.; Brooks, L.D.; Durbin, R.M.; Garrison, E.P.; Kang, H.M.; Korbel, J.O.; Marchini, J.L.; McCarthy, S.; McVean, G.A.; et al. A global reference for human genetic variation. Nature 2015, 526, 68–74. [Google Scholar]
- Ghassemi, M.; Naumann, T.; Schulam, P.; Beam, A.L.; Chen, I.Y.; Ranganath, R. A Review of Challenges and Opportunities in Machine Learning for Health. AMIA Jt. Summits Transl. Sci. Proc. 2020, 2020, 191–200. [Google Scholar] [PubMed]
- Koumakis, L. Deep learning models in genomics; are we there yet? Comput. Struct. Biotechnol. J. 2020, 18, 1466–1473. [Google Scholar] [CrossRef]






| Reference Values | 0 Month | 2 Month |
|---|---|---|
| Iron (65–175 µg/dL) * | 58 | 119 |
| UIBC (69–240 µg/dL) * | 309 | 220 |
| Ferritin (22–275 ng/dL) * | 10 | 10 |
| Total Bilirubin (0.2–1.2 mg/dL) * | 1.86 | 2.2 |
| Direct Bilirubin (0–0.5 mg/dL) * | 0.59 | 0.69 |
| Vitamin D (>30 mg/dL) * | 22.7 | 17.3 |
| FT3 (2.3–4.3 pg/mL) * | 4.6 | 2.5 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Brancaccio, M.; Mennitti, C.; Cesaro, A.; Monda, E.; D’Argenio, V.; Casaburi, G.; Mazzaccara, C.; Ranieri, A.; Fimiani, F.; Barretta, F.; et al. Multidisciplinary In-Depth Investigation in a Young Athlete Suffering from Syncope Caused by Myocardial Bridge. Diagnostics 2021, 11, 2144. https://0-doi-org.brum.beds.ac.uk/10.3390/diagnostics11112144
Brancaccio M, Mennitti C, Cesaro A, Monda E, D’Argenio V, Casaburi G, Mazzaccara C, Ranieri A, Fimiani F, Barretta F, et al. Multidisciplinary In-Depth Investigation in a Young Athlete Suffering from Syncope Caused by Myocardial Bridge. Diagnostics. 2021; 11(11):2144. https://0-doi-org.brum.beds.ac.uk/10.3390/diagnostics11112144
Chicago/Turabian StyleBrancaccio, Mariarita, Cristina Mennitti, Arturo Cesaro, Emanuele Monda, Valeria D’Argenio, Giorgio Casaburi, Cristina Mazzaccara, Annaluisa Ranieri, Fabio Fimiani, Ferdinando Barretta, and et al. 2021. "Multidisciplinary In-Depth Investigation in a Young Athlete Suffering from Syncope Caused by Myocardial Bridge" Diagnostics 11, no. 11: 2144. https://0-doi-org.brum.beds.ac.uk/10.3390/diagnostics11112144