The English Version of the Health Profession Communication Collective Efficacy Scale (HPCCE Scale) by Capone and Petrillo, 2012
Abstract
:1. Introduction
1.1. Communication in Health Organization
1.2. Collective Efficacy in Working Group and Organization
1.3. Aims and Hypothesis
2. Materials and Methods
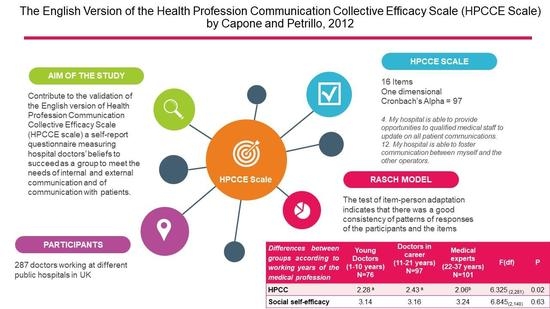
2.1. The English Version of Health Profession Communication Collective Efficacy Scale
2.2. Participants
2.3. Measures
2.4. Procedure
3. Results
3.1. Exploratory Analysis
3.2. Mono-Dimensionality Tested through the Rasch Model
3.3. Construct Validity
3.4. Descriptive Data for the Whole Sample
3.5. Differences between Groups According to Length of Service
4. Discussion
5. Limitation
6. Conclusions
Author Contributions
Funding
Conflicts of Interest
Appendix A
| ➀ | ➁ | ➂ | ➃ | ➄ |
|---|---|---|---|---|
| Nothing | Little | Enough | Very | Completely |
| 1. My hospital is able to provide contacts between the company and users by implementing effective health promotion campaigns on the territory. |
| 2. My hospital can achieve the goal of good communication by providing a Service Charter that is comprehendible and accessible. |
| 3. My hospital is able to facilitate communication with other public and social services operating in the area. |
| 4. My hospital is able to provide opportunities to qualified medical staff to update on all patient communications. |
| 5. My hospital knows how to foster information to various operational units, in the exchange of patient information quickly, while keeping privacy in respect. |
| 6. The hospital where I work is able to face difficult issues, confronting operators to develop viable solutions. |
| 7. The hospital where I work is able to demonstrate, with clear communication and motivation, strengths, and those that could be improved through joint work. |
| 8. My hospital is capable of sending out a positive image of itself. |
| 9. My hospital is able to achieve the goal of ensuring that optimum communication operators in the front office are knowledgeable and helpful. |
| 10. The various health workers of the hospital where I work, know that working together can ensure optimal communication with the patient. |
| 11. The hospital where I work is able to meet the needs and gather any reports or complaints by patients. |
| 12. My hospital is able to foster communication between myself and the other operators. |
| 13. The hospital where I work is able to ensure adequate communication between health professionals and administration. |
| 14. My hospital is able to ascertain the strengths and weaknesses of the company by doing surveys among operators and analyzing the information provided. |
| 15. My hospital is able to ensure that inner hospital communication ensures adequate organization with the patients, such as avoiding overcrowded waiting rooms. |
| 16. My hospital is able to provide adequate space to allow communication with patients in quiet and privacy. |
References
- Capone, V.; Petrillo, G. Le Aspettative di Risultato Nella Comunicazione Medica: Un nuovo strumento di misura. G. Ital. di Psicol. 2014, 4, 833–861. [Google Scholar] [CrossRef]
- Capone, V.; Petrillo, G. Teachers’ perceptions of fairness, well-being and burnout. Int. J. Educ. Manag. 2016, 30, 864–880. [Google Scholar] [CrossRef]
- Levinson, W. Physician-patient communication. The relationship with malpractice claims among primary care physicians and surgeons. JAMA 1997, 277, 553–559. [Google Scholar] [CrossRef] [PubMed]
- Silverman, J.; Kurtz, S.; Draper, J. Skills for Communicating with Patients; Informa UK Limited: Colchester, UK, 2016. [Google Scholar]
- Maguire, P. Key communication skills and how to acquire them. BMJ 2002, 325, 697–700. [Google Scholar] [CrossRef] [Green Version]
- Timmermans, S. The Engaged Patient: The Relevance of Patient–Physician Communication for Twenty-First-Century Health. J. Health Soc. Behav. 2020, 61, 259–273. [Google Scholar] [CrossRef]
- Capone, V.; Petrillo, G. Costruzione e validazione della Health Profession Communication Collective Efficacy Scale. G. Ital. di Psicol. 2012, 3, 903–927. [Google Scholar] [CrossRef]
- Fioravanti, M. La comunicazione nell’attività sanitaria: Obiettivi, finalità e disparità di condizioni. In Proceedings of the Conferenza Sulla Comunicazione Per La Salute, Milan, Italy, 1–3 December 2005. [Google Scholar]
- World Health Organizations. Strengthening integrated, people-centred health services. In Proceedings of the Sixty-Ninth World Health Assembly, Geneva, Switzerland, 28 May 2016.
- Guerra, G. Psicosociologia Dell’Ospedale. Analisi Organizzativa E Processi Di Cambiamento; Carocci Editore: Rome, Italy, 2007. [Google Scholar]
- Bandura, A. Self-Efficacy; The Exercise of Control; Freeman: New York, NY, USA, 1997. [Google Scholar]
- Little, B.L.; Madigan, R.M. The Relationship between Collective Efficacy and Performance in Manufacturing Work Teams. Small Group Res. 1997, 28, 517–534. [Google Scholar] [CrossRef]
- Goddard, R.D.; Hoy, W.K.; Hoy, A.W. Collective Teacher Efficacy: Its Meaning, Measure, and Impact on Student Achievement. Am. Educ. Res. J. 2000, 37, 479–507. [Google Scholar] [CrossRef]
- Goddard, R.D.; Hoy, W.K.; Hoy, A.W. Collective Efficacy Beliefs:Theoretical Developments, Empirical Evidence, and Future Directions. Educ. Res. 2004, 33, 3–13. [Google Scholar] [CrossRef] [Green Version]
- Borgogni, L.; Petitta, L.; Steca, P. Efficacia personale e collettiva nei contesti organizzativi. In La Valutazione Dell’autoefficacia: Costrutti E Strumenti; Caprara, G.V., Ed.; Edizioni Erikson: Trento, Italy, 2001; pp. 123–145. [Google Scholar]
- Bohn, J.G. Development and exploratory validation of an organizational efficacy scale. Hum. Resour. Dev. Q. 2010, 21, 227–251. [Google Scholar] [CrossRef]
- Capone, V.; Petrillo, G. Organizational efficacy, job satisfaction and well-being. J. Manag. Dev. 2015, 34, 374–394. [Google Scholar] [CrossRef]
- Egenberg, S.; Øian, P.; Eggebø, T.M.; Arsenovic, M.G.; Bru, L.E. Changes in self-efficacy, collective efficacy and patient outcome following interprofessional simulation training on postpartum haemorrhage. J. Clin. Nurs. 2017, 26, 3174–3187. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Carayon, P.; Bass, E.J.; Bellandi, T.; Gurses, A.P.; Hallbeck, M.S.; Mollo, V. Sociotechnical systems analysis in health care: A research agenda. IIE Trans. Heal. Syst. Eng. 2011, 1, 145–160. [Google Scholar] [CrossRef] [PubMed]
- Communication systems in healthcare. Guide Health Inform. 2003, 27, 89–98. [CrossRef] [Green Version]
- Freeman, R.E. Strategic Management: A Stakeholder Approach; Cambridge University Press: Cambridge, UK, 2010. [Google Scholar]
- Creixans, J.-T.; Gallardo, D.-V.; Arimany, N.-S. Social Responsibility, Communication and Financial Data of Hospitals: A Structural Modelling Approach in a Sustainability Scope. Sustainability 2020, 12, 4857. [Google Scholar] [CrossRef]
- Vecchio, L. Comunicare e organizzare. In Psicologia Delle Organizzazioni; Argentero, P., Cortese, G.C., Eds.; Raffaello Cortina Editore: Milan, Italy, 2018; pp. 21–53. [Google Scholar]
- Gully, S.M.; Incalcaterra, K.A.; Joshi, A.; Beaubien, J.M. A meta-analysis of team-efficacy, potency, and performance: Interdependence and level of analysis as moderators of observed relationships. J. Appl. Psychol. 2002, 87, 819–832. [Google Scholar] [CrossRef] [Green Version]
- Effken, J.A. Different lenses, improved outcomes: A new approach to the analysis and design of healthcare information systems. Int. J. Med. Informatics 2002, 65, 59–74. [Google Scholar] [CrossRef]
- Weisz, U.; Haas, W.; Schmied, H.; Pelikan, J. Sustainable Hospitals: A Socio-Ecological Approach. GAIA—Ecol. Perspect. Sci. Soc. 2011, 20, 191–198. [Google Scholar] [CrossRef] [Green Version]
- Phillips, J.; Gully, M.S. Organizational Behavior: Tools for Success; South-Western Cengage Learning: Boston, MA, USA, 2012. [Google Scholar]
- Conrad, C.; Sollitto, M. History of Organizational Communication. Int. Encycl. Organ. Commun. 2017, 22, 1–32. [Google Scholar] [CrossRef]
- Blazenaite, A. Effective Organizational Communication: In Search of a System. Soc. Sci. 2012, 74, 84–101. [Google Scholar] [CrossRef] [Green Version]
- Harrison, J.S.; Bosse, D.A.; Phillips, R.A. Managing for stakeholders, stakeholder utility functions, and competitive advantage. Strat. Manag. J. 2010, 31, 58–74. [Google Scholar] [CrossRef]
- Rolando, S. La Comunicazione Di Pubblica Utilità; Franco Angeli: Milano, Italy, 2004. [Google Scholar]
- Moja, E.A.; Vegni, E. La Visita Medica Centrata sul Paziente; Cortina Editore: Milano, Italy, 2000. [Google Scholar]
- Capone, V.; Petrillo, G. Patient’s Communication Perceived Self-Efficacy Scale (PCSS): Construction and validation of a new measure in a socio-cognitive perspective. Patient Educ. Couns. 2014, 95, 340–347. [Google Scholar] [CrossRef]
- Capone, V. Patient communication self-efficacy, self-reported illness symptoms, physician communication style and mental health and illness in hospital outpatients. J. Health Psychol. 2014, 21, 1271–1282. [Google Scholar] [CrossRef] [PubMed]
- Burley, L.; Hampton, A. Talking Matters. Developing the Communication Skills of Doctors; Scottish Executive: Edinburgh, Scotland, 2003. [Google Scholar]
- Rolando, S. Teoria E Tecniche Della Comunicazione Pubblica; Etas: Milano, Italy, 2001. [Google Scholar]
- Coordinatori delle Reti Nazionali e Regionali HPH. Le Raccomandazioni di Vienna sugli Ospedali per la Promozione della Salute. In Proceedings of the 3^ Workshop dei Coordinatori delle Reti Nazionali e Regionali HPH, Vienna, Austria, 17 April 1997.
- Weiner, S.; Barnet, B.; Cheng, T.L.; Daaleman, T.P. Processes for Effective Communication in Primary Care. Ann. Intern. Med. 2005, 142, 709–714. [Google Scholar] [CrossRef] [Green Version]
- Capone, V. La percezione di autoefficacia nella comunicazione con il paziente: Uno studio esplorativo tra i medici ospedalieri campani. Psicol. della Salut. 2009, 2, 81–97. [Google Scholar] [CrossRef]
- Bandura, A. Adolescent development from an agent perspective. In Self-Efficacy Beliefs of Adolescents; Pajares, T., Urdan, T., Eds.; Information Age Publishing: Greenwich, UK, 2006; pp. 1–44. [Google Scholar]
- Donizzetti, A.R.; Petrillo, G. Burnout degli insegnanti: Il ruolo protettivo dei fattori contestuali e delle percezioni riferite all’efficacia scolastica e alle risorse del territorio. Psicol. DELLA Salut. 2013, 2, 96–119. [Google Scholar] [CrossRef]
- Caprara, G.V. La Valutazione Dell’autoefficacia: Costrutti E Strumenti; Erickson: Trento, Italy, 2001. [Google Scholar]
- Stajkovic, A.D.; Lee, D.; Nyberg, A.J. Collective efficacy, group potency, and group performance: Meta-analyses of their relationships, and test of a mediation model. J. Appl. Psychol. 2009, 94, 814–828. [Google Scholar] [CrossRef]
- Bandura, A. Social Cognitive Theory: An Agentic Perspective. Annu. Rev. Psychol. 2000, 52, 1–26. [Google Scholar] [CrossRef] [Green Version]
- Lim, S.; Eo, S. The mediating roles of collective teacher efficacy in the relations of teachers’ perceptions of school organizational climate to their burnout. Teach. Teach. Educ. 2014, 44, 138–147. [Google Scholar] [CrossRef]
- Kim, M.; Shin, Y. Collective efficacy as a mediator between cooperative group norms and group positive affect and team creativity. Asia Pac. J. Manag. 2015, 32, 693–716. [Google Scholar] [CrossRef]
- Carroll, J.M.; Rosson, M.B.; Zhou, J. Collective efficacy as a measure of community. In Proceedings of the 27th International Conference on Human Factors in Computing Systems, Boston, MA, USA, 4–9 April 2009; pp. 1579–1588. [Google Scholar]
- Whyte, G. Recasting Janis’s Groupthink Model: The Key Role of Collective Efficacy in Decision Fiascoes. Organ. Behav. Hum. Decis. Process. 1998, 73, 185–209. [Google Scholar] [CrossRef] [PubMed]
- Zacarro, S.J.; Blair, V.; Peterson, C.; Zazanis, M. Collective Efficacy. In Self-Efficacy, Adaptation and Adjustment: Theory, Research, and Application; Maddux, J.E., Ed.; Plenum Press: New York, NY, USA, 1995; pp. 305–327. [Google Scholar]
- Karrasch, A.I. Lessons Learned on Collective Efficacy in Multinational Teams, Technical Report 1137 (AD A414 109); U.S. Army Research Institute for the Behavioural and Social Sciences: Alexandria, VA, USA, 2003. [Google Scholar]
- Bandura, A.; Locke, E.A. Negative self-efficacy and goal effects revisited. J. Appl. Psychol. 2003, 88, 87–99. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bandura, A. Self-efficacy mechanism in human agency. Am. Psychol. 1982, 37, 122–147. [Google Scholar] [CrossRef]
- Prussia, G.; Kinicki, A.J. A motivational investigation of group effectiveness using social-cognitive theory. J. Appl. Psychol. 1996, 81, 187–198. [Google Scholar] [CrossRef]
- Little, B.L.; Madigan, R.M. Motivation in work teams: A test of deconstruct of collective efficacy. In Proceedings of the Annual Meeting of the Academy of Management, Houston, TX, USA, 6–11August 1994. [Google Scholar]
- Boca, S.; Bocchiaro, P.; Scaffidi, C.A. Introduzione Alla Psicologia Sociale; Il Mulino: Bologna, Italy, 2010. [Google Scholar]
- Boca, S.; Ruggieri, S.; Ingoglia, S. Metodologia Della Ricerca Psicosociale; Laterza: Bari-Roma, Italy, 2007. [Google Scholar]
- Capone, V.; Petrillo, G. Health Promotion in International Documents: Strengths and Weaknesses from the Perspective of Community Empowerment. J. Community Appl. Soc. Psychol. 2011, 23, 98–114. [Google Scholar] [CrossRef]
- Capone, V.; Petrillo, G.; Romano, A. La soddisfazione lavorativa e per la vita di medici e infermieri ospedalieri: Relazioni con il senso di appartenenza all’azienda ospedaliera, le percezioni di efficacia collettiva e il sostegno sociale percepito. Psicol. DELLA Salut. 2013, 3, 115–130. [Google Scholar] [CrossRef]
- Gray, D.E. Doing Research in the Real World, 4th ed.; SAGE: Thousand Oakes, CA, USA; London, UK, 2018. [Google Scholar]
- Pastorelli, C.; Picconi, L. Autoefficacia scolastica, sociale e regolatoria. In La Valutazione Dell’autoefficacia: Costrutti E Strumenti; Caprara, G.V., Ed.; Edizioni Erikson: Trento, Italy, 2001; pp. 87–104. [Google Scholar]
- Gallucci, M.; Leone, L.; Perugini, M. Navigare in Spss Per Windows; KAPPA: Roma, Italy, 1999. [Google Scholar]
- Andrich, D.; Sheridan, B.; Luo, G. (1997–2012) RUMM2030: Rasch Unidimensional Models for Measurement; RUMM Laboratory: Perth, Australia, 2014. [Google Scholar]
- Bandura, A. Exercise of Human Agency through Collective Efficacy. APS 2000, 9, 75–78. [Google Scholar] [CrossRef]
- Caprara, G.V.; Barbaranelli, C.; Borgogni, L.; Steca, P. Efficacy Beliefs as Determinants of Teachers’ Job Satisfaction. J. Educ. Psychol. 2003, 95, 821–832. [Google Scholar] [CrossRef]
- Caso, D.; Donizzetti, A.R. Le scale di autoefficacia specifiche per la salute: Un contributo alla validazione con il modello di Rasch. Psicol. Della Salut. 2004, 2, 161–176. [Google Scholar]
- Capone, V. Autoefficacia comunicativa dei pazienti e stili comunicativi del medico di base: Relazioni con l’aderenza alla terapia e il benessere psicosociale dei pazienti. Psicol. Della Salut. 2015, 1, 131–148. [Google Scholar] [CrossRef]
- Borgogni, L. Efficacia Organizzativa; Guerini: Milano, Italy, 2001. [Google Scholar]
- Watson, C.B.; Chemers, M.M.; Preiser, N. Collective efficacy: A multilevel analysis. PSPB 2001, 27, 1057–1068. [Google Scholar] [CrossRef]
- Spector, P.E. Method variance in organizational research: Truth or urban legend? Organ. Res. Methods 2006, 9, 221–232. [Google Scholar] [CrossRef]
- Zodwa, M.M.; van Aswegen, J.E. Factors affecting working conditions in public hospitals: A literature review. IJANS 2017, 6, 28–38. [Google Scholar] [CrossRef]
- Statista Inc. Number of Registered Doctors in the United Kingdom (UK) in 2019, by Gender and Specialty. Available online: https://0-www-statista-com.brum.beds.ac.uk/statistics/698260/registered-doctors-united-kingdom-uk-by-gender-and-specialty/ (accessed on 9 November 2020).
- Roccato, M. L’inchiesta E Il Sondaggio Nella Ricerca Psicosociale; Il Mulino: Bologna, Italy, 2006. [Google Scholar]
| Factors’ Loading | Item-Total Correlation | Cronbach’s Alpha If Item Deleted | |
|---|---|---|---|
| Item 12 | 0.82 | 0.81 | 0.97 |
| Item 4 | 0.82 | 0.80 | 0.97 |
| Item 2 | 0.81 | 0.79 | 0.97 |
| Item 10 | 0.80 | 0.79 | 0.97 |
| Item 6 | 0.80 | 0.79 | 0.97 |
| Item16 | 0.80 | 0.79 | 0.97 |
| Item15 | 0.79 | 0.78 | 0.97 |
| Item 3 | 0.79 | 0.77 | 0.97 |
| Item11 | 0.78 | 0.77 | 0.97 |
| Item 8 | 0.77 | 0.76 | 0.97 |
| Item 9 | 0.77 | 0.76 | 0.97 |
| Item 13 | 0.77 | 0.75 | 0.97 |
| Item 7 | 0.76 | 0.75 | 0.97 |
| Item 5 | 0.75 | 0.74 | 0.97 |
| Item 14 | 0.75 | 0.74 | 0.97 |
| Item 1 | 0.75 | 0.74 | 0.97 |
| Item | Location | FitResid | ChiSq | DF | Prob |
|---|---|---|---|---|---|
| 8 | –0.506 | –0.39 | 4.624 | 4 | 0.33 |
| 11 | –0.495 | –0.30 | 7.774 | 4 | 0.10 |
| 5 | –0.266 | 1.82 | 2.710 | 4 | 0.61 |
| 13 | –0.238 | 1.72 | 9.017 | 4 | 0.06 |
| 16 | –0.234 | –1.39 | 8.037 | 4 | 0.09 |
| 6 | –0.202 | –0.47 | 0.576 | 4 | 0.97 |
| 9 | –0.148 | 0.10 | 1.598 | 4 | 0.81 |
| 15 | –0.097 | –0.59 | 6.898 | 4 | 0.14 |
| 2 | –0.065 | –0.17 | 0.184 | 4 | 1.00 |
| 3 | 0.101 | 0.17 | 2.134 | 4 | 0.71 |
| 4 | 0.132 | –0.40 | 5.038 | 4 | 0.28 |
| 1 | 0.208 | 1.43 | 1.442 | 4 | 0.84 |
| 7 | 0.284 | 0.54 | 1.874 | 4 | 0.76 |
| 12 | 0.302 | 1.05 | 7.977 | 4 | 0.09 |
| 14 | 0.323 | –1.65 | 6.663 | 4 | 0.15 |
| 10 | 0.903 | –1.83 | 1.993 | 4 | 0.74 |
| ITEMS | PERSONS | |||
|---|---|---|---|---|
| Location | Fit Residual | Location | Fit Residual | |
| Mean | 0.00 | –0.06 | –1.58 | –0.46 |
| Standard dev | 0.36 | 1.13 | 1.94 | 1.77 |
| Young Doctors N = 76 | Doctors in Career N = 97 | Medical Experts N = 101 | F(df) | p | |
|---|---|---|---|---|---|
| HPCC | 2.28 a | 2.43 a | 2.06 b | 6.325 (2,281) | 0.02 |
| Social self-efficacy | 3.14 | 3.16 | 3.24 | 6.845 (2,140) | 0.63 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Capone, V.; Marino, L.; Donizzetti, A.R. The English Version of the Health Profession Communication Collective Efficacy Scale (HPCCE Scale) by Capone and Petrillo, 2012. Eur. J. Investig. Health Psychol. Educ. 2020, 10, 1065-1079. https://0-doi-org.brum.beds.ac.uk/10.3390/ejihpe10040075
Capone V, Marino L, Donizzetti AR. The English Version of the Health Profession Communication Collective Efficacy Scale (HPCCE Scale) by Capone and Petrillo, 2012. European Journal of Investigation in Health, Psychology and Education. 2020; 10(4):1065-1079. https://0-doi-org.brum.beds.ac.uk/10.3390/ejihpe10040075
Chicago/Turabian StyleCapone, Vincenza, Leda Marino, and Anna Rosa Donizzetti. 2020. "The English Version of the Health Profession Communication Collective Efficacy Scale (HPCCE Scale) by Capone and Petrillo, 2012" European Journal of Investigation in Health, Psychology and Education 10, no. 4: 1065-1079. https://0-doi-org.brum.beds.ac.uk/10.3390/ejihpe10040075