The Public Health Responsibility Deal: Using a Systems-Level Analysis to Understand the Lack of Impact on Alcohol, Food, Physical Activity, and Workplace Health Sub-Systems
Abstract
:1. Introduction
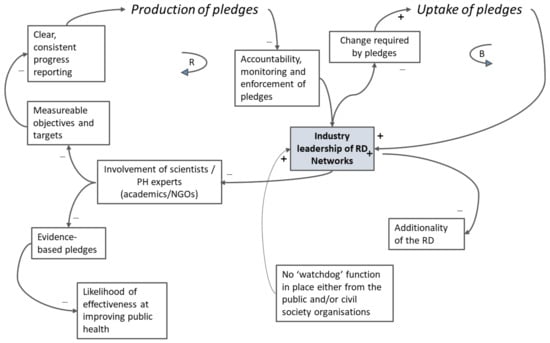
2. Methods and Materials
- (1)
- What are the causal pathways involved in the RD and how did they help or hinder it?
- (2)
- What were the RD structures, processes and interests at play?
- (3)
- What were the feedback loops, and did they suppress or potentiate effects of the RD on the outcomes of interest?
- (4)
- How resilient was the system to change and what was its ability to “absorb” externally directed change?
3. Results
3.1. What Were the Causal Pathways Involved, and How Did They Help or Hinder the Intervention (the Responsibility Deal)?
3.2. What Were the Responsibility Deal Structures, Processes and Interests at Play?
3.2.1. Structures Driving the RD
3.2.2. Organisations Involved and Their Rationale for Doing so
3.3. What Were the Feedback Loops and Did They Suppress or Potentiate Effects of the RD on the Outcomes of Interest?
3.4. How Resilient Was the System to Change and What was Its Ability to “Absorb” Externally Directed Change?
4. Discussion
4.1. The RD in the Context of the Wider Literature on Public-Private Partnerships
- (1)
- evidence-informed and rights-based targets that are in the interest of public health, and that are developed in a transparent manner and SMART in design (i.e., specific, measurable, attributable, realistic and time-bound);
- (2)
- independent, rigorous monitoring of compliance, progress and public health impact;
- (3)
- transparent reporting with clear consequences and independent measures of accountability to the government and to the public;
- (4)
- sufficient scope for impact, through the participation of leading corporate players and applied as widely as possible to cover the largest possible proportion of those exposed to risk of ill-health and the market.
- (5)
- range of contributors: “…self-regulatory regimes should have inputs from governments, scientists and civil society, particularly in target and standard-setting and ensuring accountability” [2].
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
| CLD | causal loop diagram |
| PPP | public–private partnership |
| RD | the Public Health Responsibility Deal |
| SMART | specific, measurable, attributable, realistic, and time-bound |
References
- Kraak, V.I.; Harrigan, P.B.; Lawrence, M.; Harrison, P.J.; Jackson, M.A.; Swinburn, B. Balancing the benefits and risks of public-private partnerships to address the global double burden of malnutrition. Public Health Nutr. 2012, 15, 503–517. [Google Scholar] [CrossRef] [PubMed]
- Buse, K.; Tanaka, S.; Hawkes, S. Healthy people and healthy profits? Elaborating a conceptual framework for governing the commercial determinants of non-communicable diseases and identifying options for reducing risk exposure. Global. health 2017, 13, 34. [Google Scholar] [CrossRef] [PubMed]
- Alcohol Strategy and the Drinks Industry A Partnership for Prevention? Available online: https://www.jrf.org.uk/report/alcohol-strategy-and-drinks-industry-partnership-prevention (accessed on 8 December 2018).
- Knai, C.; James, L.; Petticrew, M.; Eastmure, E.; Durand, M.A.; Mays, N. An evaluation of a public–private partnership to reduce artificial trans fatty acids in England, 2011–16. Eur. J. Public Health 2017, 27, 605–608. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Petticrew, M.; Douglas, N.; Knai, C.; Maani Hessari, N.; Durand, M.A.; Eastmure, E.; Mays, N. Provision of information to consumers about the calorie content of alcoholic drinks: Did the Responsibility Deal pledge by alcohol retailers and producers increase the availability of calorie information? Public Health 2017, 149, 159–166. [Google Scholar] [CrossRef] [PubMed]
- Petticrew, M.; Douglas, N.; Knai, C.; Durand, M.A.; Eastmure, E.; Mays, N. Health information on alcoholic beverage containers: Has the alcohol industry’s pledge in England to improve labelling been met? Addiction 2016, 111, 51–55. [Google Scholar] [CrossRef] [PubMed]
- Knai, C.; Scott, C.; D’Souza, P.; James, L.; Mehrotra, A.; Petticrew, M.; Eastmure, E.; Durand, M.A.; Mays, N. The Public Health Responsibility Deal: Making the workplace healthier? J. Public Health 2016, 39, 373–386. [Google Scholar] [CrossRef] [PubMed]
- Knai, C.; Petticrew, M.; Durand, M.; Scott, C.; James, L.; Mehrotra, A.; Eastmure, E.; Mays, N. Has a public–private partnership resulted in action on healthier diets in England? An analysis of the Public Health Responsibility Deal food pledges Food Policy 2015, 54, 1–10. [Google Scholar]
- Durand, M.A.; Petticrew, M.; Goulding, L.; Eastmure, E.; Knai, C.; Mays, N. An evaluation of the Public Health Responsibility Deal: Informants’ experiences and views of the development, implementation and achievements of a pledge-based, public-private partnership to improve population health in England. Health Policy 2015, 119, 1506–1514. [Google Scholar] [CrossRef]
- Knai, C.; Petticrew, M.; Durand, M.A.; Eastmure, E.; Mays, N. Are the Public Health Responsibility Deal alcohol pledges likely to improve public health? An evidence synthesis. Addiction 2015, 110, 1232–1246. [Google Scholar] [CrossRef] [Green Version]
- Knai, C.; Petticrew, M.; Durand, M.A.; Scott, C.; James, L.; Mehrotra, A.; Eastmure, E.; Mays, N. The Public Health Responsibility deal: Has a public–private partnership brought about action on alcohol reduction? Addiction 2015, 110, 1217–1225. [Google Scholar] [CrossRef]
- Bryden, A.; Petticrew, M.; Mays, N.; Eastmure, E.; Knai, C. Voluntary agreements between government and business—A scoping review of the literature with specific reference to the Public Health Responsibility Deal. Health Policy 2013, 110, 186–197. [Google Scholar] [CrossRef]
- Knai, C.; Petticrew, M.; Scott, C.; Durand, M.A.; Eastmure, E.; James, L.; Mehrotra, A.; Mays, N. Getting England to be more physically active: Are the Public Health Responsibility Deal’s physical activity pledges the answer? Int. J. Behav. Nutr. Phys. Act. 2015, 12, 107. [Google Scholar] [CrossRef]
- Rietveld, L.C.; Siri, J.G.; Chakravarty, I.; Arsenio, A.M.; Biswas, R.; Chatterjee, A. Improving health in cities through systems approaches for urban water management. Environ. Health 2016, 15 (Suppl. 1), 31. [Google Scholar] [CrossRef]
- Macmillan, A.; Davies, M.; Shrubsole, C.; Luxford, N.; May, N.; Chiu, L.F.; Trutnevyte, E.; Bobrova, Y.; Chalabi, Z. Integrated decision-making about housing, energy and wellbeing: A qualitative system dynamics model. Environ. Health 2016, 15 (Suppl. 1), 37. [Google Scholar] [CrossRef]
- Allender, S.; Owen, B.; Kuhlberg, J.; Lowe, J.; Nagorcka-Smith, P.; Whelan, J.; Bell, C. A Community Based Systems Diagram of Obesity Causes. PLoS ONE 2015, 10, e0129683. [Google Scholar] [CrossRef] [PubMed]
- Johnston, L.M.; Matteson, C.L.; Finegood, D.T. Systems science and obesity policy: A novel framework for analyzing and rethinking population-level planning. Am. J. Public Health 2014, 104, 1270–1278. [Google Scholar] [CrossRef] [PubMed]
- Adam, T.; Savigny, D. Systems thinking for strengthening health systems in LMICs: Need for a paradigm shift. Health Policy Plan 2012, 27. [Google Scholar] [CrossRef] [PubMed]
- Meadows, D. Thinking in Systems: A. Primer; Earthscan: London, UK, 2008; ISBN 978-1-84407-726-7. [Google Scholar]
- Leverage Points: Place to Intervene in a System. Available online: http://drbalcom.pbworks.com /w/file/fetch/35173014/Leverage_Points.pdf (accessed on 6 December 2018).
- UK Department of Health. The Public Health Responsibility Deal. Available online: https://webarchive.nationalarchives.gov.uk/20180201175643/https://responsibilitydeal.dh.gov.uk/ (accessed on 8 December 2018).
- Diez Roux, A.V. Complex systems thinking and current impasses in health disparities research. Am. J. Public Health 2011, 101, 1627–1634. [Google Scholar] [CrossRef]
- Petticrew, M.; Eastmure, E.; Mays, N.; Knai, C.; Durand, M.; Nolte, E. The Public Health Responsibility Deal: How should such a complex public health policy be evaluated? J. Public Health 2013, 35, 495–501. [Google Scholar] [CrossRef]
- Douglas, N.; Knai, C.; Petticrew, M.; Eastmure, E.; Durand, M.; Mays, N. How the food, beverage and alcohol industries presented the Public Health Responsibility Deal in UK print and online media reports. Crit. Public Health 2018, 28, 377–387. [Google Scholar] [CrossRef]
- Vennix, J. Group model-building: Tackling messy problems. Syst. Dyn. Rev. 1999, 15, 379–401. [Google Scholar] [CrossRef]
- Beall, A.; Ford, A. Reports from the field: Assessing the art and science of participatory environmental modeling. Int. J. Info. Sys. Soc. Change 2010, 1, 72–89. [Google Scholar] [CrossRef]
- Systems concepts in evaluation. An Expert Anthology. American Evaluation Association. Available online: http://www.managingforimpact.org/sites/default/files/resource/system_concepts_in_evaluation.pdf (accessed on 8 December 2018).
- Waters Foundation. The Waters Foundation. Systems. Thinking in Education. Available online: http://watersfoundation.org/. (accessed on 8 December 2018).
- Causal Loop Construction: The Basics. Available online: https://thesystemsthinker.com/causal-loop-construction-the-basics/ (accessed on 8 December 2018).
- Public Health: Ethical Issues. Available online: http://nuffieldbioethics.org/wp-content/uploads/2014/07/ Public-health-ethical-issues.pdf (accessed on 8 December 2018).
- ’Responsibility Deal’ Announced as Health Groups Withdraw. Available online: http://www.alcoholpolicy.net/ 2011/03/respsonsibilty-deals-announced-but-health-groups-withdraw-.html (accessed on 8 December 2018).
- Hawe, P.; Shiell, A.; Riley, T. Theorising interventions as events in systems. Am. J. Community Psychol. 2009, 43, 267–276. [Google Scholar] [CrossRef] [PubMed]
- Noel, J.; Babor, T.; Robaina, K. Industry self-regulation of alcohol marketing: A systematic review of content and exposure research. Addiction 2017, 112 (Suppl. 1), 28–50. [Google Scholar] [CrossRef]
- Ronit, K.; Jensen, D. Obesity and industry self-regulation of food and beverage marketing: A literature review. Eur. J. Clin. Nutr. 2014, 68, 753–759. [Google Scholar] [CrossRef] [PubMed]
- Downs, S.; Thow, A.; Leeder, S. The effectiveness of policies for reducing dietary trans fat: A systematic review of the evidence. Bull. World Health Org. 2013, 91, 262–269H. [Google Scholar] [CrossRef] [PubMed]
- Jensen, J.; Ronit, K. The EU pledge for responsible marketing of food and beverages to children: Implementation in food companies. Eur. J. Clin. Nutr. 2015, 69, 896–901. [Google Scholar] [CrossRef]
- Kunkel, D.; Castonguay, J.; Filer, C. Evaluating Industry Self-Regulation of Food Marketing to Children. Am. J. Prev. Med. 2015, 49, 181–187. [Google Scholar] [CrossRef]
- Risse, T.; Börzel, T.A. Public-Private Partnerships. Effective and Legitimate Tools of International Governance? In Complex Sovereignty. Reconstituting Political Authority in the Twenty-First Centur; Grande, E., Pauly, L., Eds.; University of Toronto Press: Toronto, ON, Canada, 2005; pp. 195–216. [Google Scholar]
- Bartlett, O.; Garde, A. The EU Platform and the EU Forum: New Modes of Governance or a Smokescreen for the Promotion of Conflicts of Interest? In Regulating Lifestyle Risks: The EU, Alcohol, Tobacco and Unhealthy Diets; Alemanno, A., Garde, A., Eds.; Cambridge University Press: Cambridge, UK, 2015; Volume 13, pp. 283–308. ISBN 9781107063426. [Google Scholar]
- Tangled up in Blue: Corporate Partnerships at the United Nations. Available online: http://s3.amazonaws.com/corpwatch.org/downloads/tangled.pdf (accessed on 8 December 2018).






| RD Evaluation Components | System Attributes which these Data Illuminate (Adapted from [20]) |
|---|---|
| Logic model built on initial description of how RD would work [23], and scoping review [12] | Causal pathways within the RD systems (food, alcohol, physical activity, health at work) |
| Participant interviews [9] Analysis of organisational case studies including documents and interviews Media analysis [24] | Structures and processes in place Interests at play Feedback loops, and barriers to change |
| Qualitative systems dynamic modelling [15,25,26] using Causal Loop Diagrams (as an analytic tool) [27] built on data from pledge analyses, progress report analyses, qualitative data from interviews and organisational case studies (created as part of the current paper) | Drivers, interests, ways of working |
| Analysis of RD pledges [4,5,6,7,8,9,10,11,13,24] | |
| Analyses of evidence base [4,5,6,7,8,9,10,11,13,24] | Probability of system changing in response to specific pledges |
| Analyses of specific pledges [4,5,6,7,8,9,10,11,13,24] | Identifying whether change happened in a particular part of the system |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Knai, C.; Petticrew, M.; Douglas, N.; Durand, M.A.; Eastmure, E.; Nolte, E.; Mays, N. The Public Health Responsibility Deal: Using a Systems-Level Analysis to Understand the Lack of Impact on Alcohol, Food, Physical Activity, and Workplace Health Sub-Systems. Int. J. Environ. Res. Public Health 2018, 15, 2895. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph15122895
Knai C, Petticrew M, Douglas N, Durand MA, Eastmure E, Nolte E, Mays N. The Public Health Responsibility Deal: Using a Systems-Level Analysis to Understand the Lack of Impact on Alcohol, Food, Physical Activity, and Workplace Health Sub-Systems. International Journal of Environmental Research and Public Health. 2018; 15(12):2895. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph15122895
Chicago/Turabian StyleKnai, Cécile, Mark Petticrew, Nick Douglas, Mary Alison Durand, Elizabeth Eastmure, Ellen Nolte, and Nicholas Mays. 2018. "The Public Health Responsibility Deal: Using a Systems-Level Analysis to Understand the Lack of Impact on Alcohol, Food, Physical Activity, and Workplace Health Sub-Systems" International Journal of Environmental Research and Public Health 15, no. 12: 2895. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph15122895