Short-Term Associations of Fine Particulate Matter and Synoptic Weather Types with Cardiovascular Mortality: An Ecological Time-Series Study in Shanghai, China
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Setting
2.2. Data Collection
2.3. Statistical Analyses
2.4. Ethical Consideration and Data Availability
3. Results
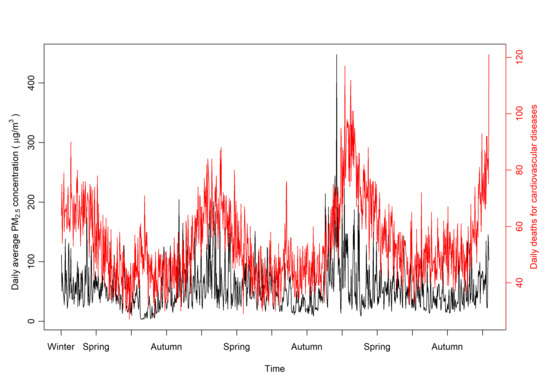
3.1. Characteristics of CVD Mortality, PM2.5 Concentration, and Meteorological Conditions
3.2. Effects of PM2.5, SWT, and Their Interactions on CVD Mortality
3.3. Lag Effect of PM2.5 on CVD Mortality
3.4. Sensitivity Analysis
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Brunekreef, B.; Beelen, R.; Hoek, G.; Schouten, L.; Bausch-Goldbohm, S.; Fischer, P.; Armstrong, B.; Hughes, E.; Jerrett, M.; van den Brandt, P. Effects of long-term exposure to traffic-related air pollution on respiratory and cardiovascular mortality in the Netherlands: The NLCS-AIR study. Res. Rep. Health Eff. Inst. 2009, 139, 5–71. [Google Scholar]
- Meo, S.A.; Suraya, F. Effect of environmental air pollution on cardiovascular diseases. Eur. Rev. Med. Pharmacol. Sci. 2015, 19, 4890–4897. [Google Scholar] [PubMed]
- Shang, Y.; Sun, Z.; Cao, J.; Wang, X.; Zhong, L.; Bi, X.; Li, H.; Liu, W.; Zhu, T.; Huang, W. Systematic review of Chinese studies of short-term exposure to air pollution and daily mortality. Environ. Int. 2013, 54, 100–111. [Google Scholar] [CrossRef] [PubMed]
- Pinault, L.L.; Weichenthal, S.; Grouse, D.L.; Brauer, M.; Erickson, A.; van Donkelaar, A.; Martin, R.V.; Hystad, P.; Chen, H.; Fines, P.; et al. Associations between fine particulate matter and mortality in the 2001 Canadian Census Health and Environment Cohort. Environ. Res. 2017, 159, 406–415. [Google Scholar] [CrossRef]
- Huang, C.; Moran, A.E.; Coxson, P.G.; Yang, X.; Liu, F.; Cao, J.; Chen, K.; Wang, M.; He, J.; Goldman, L.; et al. Potential Cardiovascular and Total Mortality Benefits of Air Pollution Control in Urban China. Circulation 2017, 136, 1575–1584. [Google Scholar] [CrossRef]
- Liu, C.; Chen, R.; Sera, F.; Vicedo-Cabrera, A.M.; Guo, Y.; Tong, S.; Coelho, M.; Saldiva, P.H.N.; Lavigne, E.; Matus, P.; et al. Ambient Particulate Air Pollution and Daily Mortality in 652 Cities. N. Engl. J. Med. 2019, 381, 705–715. [Google Scholar] [CrossRef]
- Bourdrel, T.; Bind, M.A.; Bejot, Y.; Morel, O.; Argacha, J.F. Cardiovascular effects of air pollution. Arch. Cardiovasc. Dis. 2017, 110, 634–642. [Google Scholar] [CrossRef]
- Argacha, J.F.; Bourdrel, T.; van de Borne, P. Ecology of the cardiovascular system: A focus on air-related environmental factors. Trends Cardiovasc. Med. 2018, 28, 112–126. [Google Scholar] [CrossRef]
- Kim, H.; Kim, J.; Kim, S.; Kang, S.H.; Kim, H.J.; Kim, H.; Heo, J.; Yi, S.M.; Kim, K.; Youn, T.J.; et al. Cardiovascular Effects of Long-Term Exposure to Air Pollution: A Population-Based Study with 900,845 Person-Years of Follow-up. J. Am. Heart Assoc. 2017, 6. [Google Scholar] [CrossRef] [Green Version]
- Zhao, L.; Liang, H.R.; Chen, F.Y.; Chen, Z.; Guan, W.J.; Li, J.H. Association between air pollution and cardiovascular mortality in China: A systematic review and meta-analysis. Oncotarget 2017, 8, 66438–66448. [Google Scholar] [CrossRef] [Green Version]
- Vidale, S.; Arnaboldi, M.; Bosio, V.; Corrado, G.; Guidotti, M.; Sterzi, R.; Campana, C. Short-term air pollution exposure and cardiovascular events: A 10-year study in the urban area of Como, Italy. Int. J. Cardiol. 2017, 248, 389–393. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Yu, C.; Bao, J.; Li, X. Impact of temperature on mortality in Hubei, China: A multi-county time series analysis. Sci. Rep. 2017, 7, 45093. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhang, Y.; Yu, C.; Yang, J.; Zhang, L.; Cui, F. Diurnal Temperature Range in Relation to Daily Mortality and Years of Life Lost in Wuhan, China. Int. J. Environ. Res. Public Health 2017, 14, 891. [Google Scholar] [CrossRef]
- Zhang, Y.; Peng, M.; Wang, L.; Yu, C. Association of diurnal temperature range with daily mortality in England and Wales: A nationwide time-series study. Sci. Total Environ. 2018, 619, 291–300. [Google Scholar] [CrossRef]
- Zhang, Y.; Yu, C.; Bao, J.; Li, X. Impact of temperature variation on mortality: An observational study from 12 counties across Hubei Province in China. Sci. Total Environ. 2017, 587, 196–203. [Google Scholar] [CrossRef] [PubMed]
- Zeng, J.; Zhang, X.H.; Yang, J.; Bao, J.Z.; Xiang, H.; Dear, K.; Liu, Q.Y.; Lin, S.; Lawrence, W.R.; Lin, A.H.; et al. Humidity May Modify the Relationship between Temperature and Cardiovascular Mortality in Zhejiang Province, China. Int. J. Environ. Res. Public Health 2017, 14, 1383. [Google Scholar] [CrossRef] [Green Version]
- Liu, C.; Yavar, Z.; Sun, Q. Cardiovascular response to thermoregulatory challenges. Am. J. Physiol. Heart Circ. Physiol. 2015, 309, H1793–H1812. [Google Scholar] [CrossRef] [Green Version]
- Song, X.; Wang, S.; Hu, Y.; Yue, M.; Zhang, T.; Liu, Y.; Tian, J.; Shang, K. Impact of ambient temperature on morbidity and mortality: An overview of reviews. Sci. Total Environ. 2017, 586, 241–254. [Google Scholar] [CrossRef]
- Mendez-Lazaro, P.A.; Perez-Cardona, C.M.; Rodriguez, E.; Martinez, O.; Taboas, M.; Bocanegra, A.; Mendez-Tejeda, R. Climate change, heat, and mortality in the tropical urban area of San Juan, Puerto Rico. Int. J. Biometeorol. 2018, 62, 699–707. [Google Scholar] [CrossRef]
- Tian, L.; Qiu, H.; Sun, S.; Lin, H. Emergency Cardiovascular Hospitalization Risk Attributable to Cold Temperatures in Hong Kong. Circ. Cardiovasc. Qual. Outcomes 2016, 9, 135–142. [Google Scholar] [CrossRef] [PubMed]
- Giang, P.N.; Dung, D.O.; Giang, K.B.; Vinh, H.H.; Rocklov, J. The effect of temperature on cardiovascular disease hospital admissions among elderly people in Thai Nguyen Province, Vietnam. Glob. Health Action 2014, 7, 59–65. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ponjoan, A.; Blanch, J.; Alves-Cabratosa, L.; Marti-Lluch, R.; Comas-Cufi, M.; Parramon, D.; Del Mar Garcia-Gil, M.; Ramos, R.; Petersen, I. Effects of extreme temperatures on cardiovascular emergency hospitalizations in a Mediterranean region: A self-controlled case series study. Environ. Health 2017, 16, 32. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Plavcova, E.; Kysely, J. Effects of sudden air pressure changes on hospital admissions for cardiovascular diseases in Prague, 1994–2009. Int. J. Biometeorol. 2014, 58, 1327–1337. [Google Scholar] [CrossRef] [PubMed]
- Tsangari, H.; Paschalidou, A.K.; Kassomenos, A.P.; Vardoulakis, S.; Heaviside, C.; Georgiou, K.E.; Yamasaki, E.N. Extreme weather and air pollution effects on cardiovascular and respiratory hospital admissions in Cyprus. Sci. Total Environ. 2016, 542, 247–253. [Google Scholar] [CrossRef]
- Onozuka, D.; Hagihara, A. Within-summer variation in out-of-hospital cardiac arrest due to extremely long sunshine duration. Int. J. Cardiol. 2017, 231, 120–124. [Google Scholar] [CrossRef]
- Fang, X.; Fang, B.; Wang, C.F.; Xia, T.; Bottai, M.; Fang, F.; Cao, Y. Relationship between fine particulate matter, weather condition and daily non-accidental mortality in Shanghai, China: A Bayesian approach. PLoS ONE 2017, 12, e0187933. [Google Scholar] [CrossRef] [Green Version]
- Shanghai Bureau of Statistics. Shanghai Statistical Yearbook; China Statistics Press: Beijing, China, 2017.
- Liu, J.; Han, Y.; Tang, X.; Zhu, J.; Zhu, T. Estimating adult mortality attributable to PM2.5 exposure in China with assimilated PM2.5 concentrations based on a ground monitoring network. Sci. Total Environ. 2016, 568, 1253–1262. [Google Scholar] [CrossRef]
- Vanos, J.K.; Cakmak, S.; Bristow, C.; Brion, V.; Tremblay, N.; Martin, S.L.; Sheridan, S.S. Synoptic weather typing applied to air pollution mortality among the elderly in 10 Canadian cities. Environ. Res. 2013, 126, 66–75. [Google Scholar] [CrossRef] [Green Version]
- Ravindra, K.; Rattan, P.; Mor, S.; Aggarwal, A.N. Generalized additive models: Building evidence of air pollution, climate change and human health. Environ. Int. 2019, 132, 104987. [Google Scholar] [CrossRef]
- Thelen, B.; French, N.H.F.; Koziol, B.W.; Billmire, M.; Owen, R.C.; Johnson, J.; Ginsberg, M.; Loboda, T.; Wu, S.L. Modeling acute respiratory illness during the 2007 San Diego wildland fires using a coupled emissions-transport system and generalized additive modeling. Environ. Health 2013, 12, 94. [Google Scholar] [CrossRef] [Green Version]
- Dehghan, A.; Khanjani, N.; Bahrampour, A.; Goudarzi, G.; Yunesian, M. The relation between air pollution and respiratory deaths in Tehran, Iran- using generalized additive models. BMC Pulm. Med. 2018, 18, 49. [Google Scholar] [CrossRef] [PubMed]
- Dominici, F.; McDermott, A.; Zeger, S.L.; Samet, J.M. On the use of generalized additive models in time-series studies of air pollution and health. Am. J. Epidemiol. 2002, 156, 193–203. [Google Scholar] [CrossRef] [PubMed]
- Gasparrini, A.; Armstrong, B.; Kenward, M.G. Distributed lag non-linear models. Stat. Med. 2010, 29, 2224–2234. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schwartz, J. Harvesting and long term exposure effects in the relation between air pollution and mortality. Am. J. Epidemiol. 2000, 151, 440–448. [Google Scholar] [CrossRef]
- World Health Organization. WHO Air Quality Guidelines for Particulate Matter, Ozone, Nitrogen Dioxide and Sulfur Dioxide: Global Update 2005: Summary of Risk Assessment; World Health Organization: Geneva, Switzerland, 2006. [Google Scholar]
- Lu, F.; Xu, D.; Cheng, Y.; Dong, S.; Guo, C.; Jiang, X.; Zheng, X. Systematic review and meta-analysis of the adverse health effects of ambient PM2.5 and PM10 pollution in the Chinese population. Environ. Res. 2015, 136, 196–204. [Google Scholar] [CrossRef]
- Achilleos, S.; Kioumourtzoglou, M.A.; Wu, C.D.; Schwartz, J.D.; Koutrakis, P.; Papatheodorou, S.I. Acute effects of fine particulate matter constituents on mortality: A systematic review and meta-regression analysis. Environ. Int. 2017, 109, 89–100. [Google Scholar] [CrossRef]
- Lee, H.; Honda, Y.; Hashizume, M.; Guo, Y.L.; Wu, C.F.; Kan, H.; Jung, K.; Lim, Y.H.; Yi, S.; Kim, H. Short-term exposure to fine and coarse particles and mortality: A multicity time-series study in East Asia. Environ. Pollut. 2015, 207, 43–51. [Google Scholar] [CrossRef]
- Guo, Y.S.; Ma, Y.; Ji, J.J.; Liu, N.; Zhou, G.H.; Fang, D.K.; Huang, G.W.; Lan, T.; Peng, C.Q.; Yu, S.Y. The relationship between extreme temperature and emergency incidences: A time series analysis in Shenzhen, China. Environ. Sci. Pollut. Res. 2018, 25, 36239–36255. [Google Scholar] [CrossRef]
- Vanos, J.K.; Hebbern, C.; Cakmak, S. Risk assessment for cardiovascular and respiratory mortality due to air pollution and synoptic meteorology in 10 Canadian cities. Environ. Pollut. 2014, 185, 322–332. [Google Scholar] [CrossRef] [Green Version]
- Chen, K.; Wolf, K.; Breitner, S.; Gasparrini, A.; Stafoggia, M.; Samoli, E.; Andersen, Z.J.; Bero-Bedada, G.; Bellander, T.; Hennig, F.; et al. Two-way effect modifications of air pollution and air temperature on total natural and cardiovascular mortality in eight European urban areas. Environ. Int. 2018, 116, 186–196. [Google Scholar] [CrossRef]
- Kim, J. Particulate Matter Mortality Rates and Their Modification by Spatial Synoptic Classification. Int. J. Environ. Res. Public Health 2019, 16, 1904. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Talbott, E.O.; Rager, J.R.; Benson, S.; Brink, L.A.; Bilonick, R.A.; Wu, C. A case-crossover analysis of the impact of PM2.5 on cardiovascular disease hospitalizations for selected CDC tracking states. Environ. Res. 2014, 134, 455–465. [Google Scholar] [CrossRef] [PubMed]
- Amsalu, E.; Wang, T.Q.; Li, H.B.; Liu, Y.; Wang, A.X.; Liu, X.T.; Tao, L.X.; Luo, Y.X.; Zhang, F.; Yang, X.H.; et al. Acute effects of fine particulate matter (PM2.5) on hospital admissions for cardiovascular disease in Beijing, China: A time-series study. Environ. Health 2019, 18, 70. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Seaton, A.; MacNee, W.; Donaldson, K.; Godden, D. Particulate air pollution and acute health effects. Lancet 1995, 345, 176–178. [Google Scholar] [CrossRef]
- Franchini, M.; Mannucci, P.M. Air pollution and cardiovascular disease. Thromb. Res. 2012, 129, 230–234. [Google Scholar] [CrossRef] [PubMed]
- Kan, H.D.; Wong, C.M.; Vichit-Vadakan, N.; Qian, Z.M.; Teams, P.P. Short-term association between sulfur dioxide and daily mortality: The Public Health and Air Pollution in Asia (PAPA) study. Environ. Res. 2010, 110, 258–264. [Google Scholar] [CrossRef] [Green Version]
- Lin, H.L.; Zhang, Y.H.; Liu, T.; Xiao, J.P.; Xu, Y.J.; Xu, X.J.; Qian, Z.M.; Tong, S.L.; Luo, Y.; Zeng, W.L.; et al. Mortality reduction following the air pollution control measures during the 2010 Asian Games. Atmos. Environ. 2014, 91, 24–31. [Google Scholar] [CrossRef]
- Sun, D.; Fang, J.; Sun, J.Q. Health-related benefits of air quality improvement from coal control in China: Evidence from the Jing-Jin-Ji region. Resour. Conserv. Recycl. 2018, 129, 416–423. [Google Scholar] [CrossRef]
- Cherrie, J.W.; Apsley, A.; Cowie, H.; Steinle, S.; Mueller, W.; Lin, C.; Horwell, C.J.; Sleeuwenhoek, A.; Loh, M. Effectiveness of face masks used to protect Beijing residents against particulate air pollution. Occup. Environ. Med. 2018, 75, 446–452. [Google Scholar] [CrossRef]
- Tong, H. Dietary and pharmacological intervention to mitigate the cardiopulmonary effects of air pollution toxicity. Biochim. Biophys. Acta 2016, 1860, 2891–2898. [Google Scholar] [CrossRef]
- Rainham, D.G.; Smoyer-Tomic, K.E.; Sheridan, S.C.; Burnett, R.T. Synoptic weather patterns and modification of the association between air pollution and human mortality. Int. J. Environ. Health Res. 2005, 15, 347–360. [Google Scholar] [CrossRef] [PubMed]


| Variable | Risk Ratio (RR) for Cardiovascular Mortality | |||
|---|---|---|---|---|
| Model without SO2, NO2 | Model with SO2, NO2 | |||
| RR (95% CI) | P-Value | RR (95% CI) | P-Value | |
| PM2.5 (per 10 μ g/m3) | 1.0126 (1.0040, 1.0212) | 0.004 | 1.0121 (1.0027, 1.0215) | 0.011 |
| SO2 | 1.0007 (0.9993, 1.0021) | 0.310 | ||
| NO2 | 0.9998 (0.9990, 1.0005) | 0.544 | ||
| Synoptic weather types | ||||
| Hot dry (Ref) | ||||
| Warm humid | 0.9945 (0.9359, 1.0567) | 0.858 | 0.9971 (0.9378, 1.0603) | 0.927 |
| Cold dry | 0.9894 (0.9191, 1.0651) | 0.778 | 0.9861 (0.9149, 1.0628) | 0.714 |
| Cool dry | 0.9954 (0.9308, 1.0645) | 0.893 | 0.9978 (0.9327, 1.0674) | 0.948 |
| Cool humid | 1.0369 (0.9666, 1.1123) | 0.311 | 1.0378 (0.9675, 1.1133) | 0.300 |
| Cold humid | 1.0138 (0.9438, 1.0891) | 0.707 | 1.0157 (0.9451, 1.0914) | 0.672 |
| Day of week | ||||
| Sunday (Ref) | ||||
| Monday | 1.0269 (0.9963, 1.0585) | 0.085 | 1.0269 (0.9963, 1.0585) | 0.086 |
| Tuesday | 1.0178 (0.9874, 1.0491) | 0.254 | 1.0182 (0.9876, 1.0497) | 0.246 |
| Wednesday | 1.0350 (1.0043, 1.0667) | 0.025 | 1.0352 (1.0041, 1.0672) | 0.026 |
| Thursday | 1.0139 (0.9835, 1.0453) | 0.373 | 1.0143 (0.9837, 1.0458) | 0.363 |
| Friday | 1.0058 (0.9756, 1.0369) | 0.712 | 1.0065 (0.9761, 1.0378) | 0.681 |
| Saturday | 1.0315 (1.0008, 1.0632) | 0.044 | 1.0320 (1.0012, 1.0637) | 0.042 |
| Interaction | ||||
| PM2.5 × Hot dry (Ref) | ||||
| PM2.5 × Warm humid | 0.9924 (0.9822, 1.0027) | 0.149 | 0.9926 (0.9822, 1.0030) | 0.162 |
| PM2.5 × Cold dry | 0.9853 (0.9761, 0.9946) | 0.002 | 0.9852 (0.9758, 0.9946) | 0.002 |
| PM2.5 × Cool dry | 0.9905 (0.9802, 1.0009) | 0.074 | 0.9904 (0.9800, 1.0009) | 0.072 |
| PM2.5 × Cool humid | 0.9889 (0.9762, 1.0019) | 0.093 | 0.9893 (0.9764, 1.0022) | 0.104 |
| PM2.5 × Cold humid | 0.9855 (0.9764, 0.9948) | 0.002 | 0.9853 (0.9760, 0.9946) | 0.002 |
| Lag Day | Single Day Effect | Cumulative Effect |
|---|---|---|
| Lag 0 | 1.0001 (0.9978, 1.0024) | 1.0001 (0.9978, 1.0024) |
| Lag 1 | 1.0005 (1.0000, 1.0029) | 1.0016 (0.9980, 1.0051) |
| Lag 2 | 1.0019 (1.0004, 1.0033) | 1.0035 (0.9990, 1.0080) |
| Lag 3 | 1.0017 (1.0003, 1.0032) | 1.0052 (0.9997, 1.0108) |
| Lag 4 | 1.0012 (0.9997, 1.0027) | 1.0065 (0.9998, 1.0132) |
| Lag 5 | 1.0006 (0.9990, 1.0021) | 1.0070 (0.9991, 1.0150) |
| Lag 6 | 1.0000 (0.9983, 1.0016) | 1.0070 (0.9978, 1.0164) |
| Lag 7 | 0.9995 (0.9978, 1.0013) | 1.0066 (0.9959, 1.0174) |
| Lag 8 | 0.9993 (0.9975, 1.0012) | 1.0059 (0.9937, 1.0182) |
| Lag 9 | 0.9994 (0.9978, 1.0012) | 1.0053 (0.9916, 1.0192) |
| Lag 10 | 0.9997 (0.9979, 1.0015) | 1.0050 (0.9898, 1.0204) |
| Lag 11 | 1.0002 (0.9983, 1.0020) | 1.0051 (0.9884, 1.0221) |
| Lag 12 | 1.0007 (0.9989, 1.0025) | 1.0058 (0.9877, 1.0243) |
| Lag 13 | 1.0011 (0.9993, 1.0029) | 1.0070 (0.9874, 1.0268) |
| Lag 14 | 1.0013 (0.9995, 1.0031) | 1.0082 (0.9873, 1.0296) |
| Lag 15 | 1.0008 (0.9983, 1.0033) | 1.0091 (0.9866, 1.0320) |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tian, Q.; Li, M.; Montgomery, S.; Fang, B.; Wang, C.; Xia, T.; Cao, Y. Short-Term Associations of Fine Particulate Matter and Synoptic Weather Types with Cardiovascular Mortality: An Ecological Time-Series Study in Shanghai, China. Int. J. Environ. Res. Public Health 2020, 17, 1111. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph17031111
Tian Q, Li M, Montgomery S, Fang B, Wang C, Xia T, Cao Y. Short-Term Associations of Fine Particulate Matter and Synoptic Weather Types with Cardiovascular Mortality: An Ecological Time-Series Study in Shanghai, China. International Journal of Environmental Research and Public Health. 2020; 17(3):1111. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph17031111
Chicago/Turabian StyleTian, Qing, Mei Li, Scott Montgomery, Bo Fang, Chunfang Wang, Tian Xia, and Yang Cao. 2020. "Short-Term Associations of Fine Particulate Matter and Synoptic Weather Types with Cardiovascular Mortality: An Ecological Time-Series Study in Shanghai, China" International Journal of Environmental Research and Public Health 17, no. 3: 1111. https://0-doi-org.brum.beds.ac.uk/10.3390/ijerph17031111