Effectiveness of Hypochlorous Acid to Reduce the Biofilms on Titanium Alloy Surfaces in Vitro
Abstract
:1. Introduction
2. Results
2.1. Antibacterial Effectiveness of HOCl
2.1.1. HOCl Volume Effect
2.1.2. HOCl Durability
2.2. Antibacterial Activities on Titanium Alloy
2.2.1. Live/Dead Staining
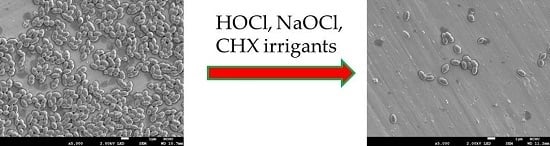
2.2.2. SEM Observation
2.2.3. AlamarBlue Assay
2.2.4. LPS Detection
3. Discussion
4. Materials and Methods
4.1. Irrigants and Microorganisms
4.2. Antibacterial Effectiveness of HOCl
4.3. Preparation of Titanium Alloy
4.4. Live/Dead Staining on Titanium Alloy
4.5. Morphology Observation on Titanium Alloy
4.6. AlamarBlue Assay on Titanium Alloy
4.7. LPS Detection on Titanium Alloy
4.8. Statistical Analysis
5. Conclusions
Author Contributions
Conflicts of Interest
References
- Berglundh, T.; Persson, L.; Klinge, B. A systematic review of the incidence of biological and technical complications in implant dentistry reported in prospective longitudinal studies of at least 5 years. J. Clin. Periodontol. 2002, 29, 197–212. [Google Scholar] [CrossRef] [PubMed]
- Lang, N.P.; Ptjetursson, B.E.; Tank, K.; Brägger, U.; Egger, M.; Zwahlen, M. A systematic review of the survival and complication rates of fixed partial dentures (FPDs) after an observation period of at least 5 years. II. Combined tooth-implant-supported FPDs. Clin. Oral Implants Res. 2004, 15, 643–653. [Google Scholar] [CrossRef] [PubMed]
- Ho, C.C.; Ding, S.J. Novel SiO2/PDA hybrid coatings to promote osteoblast-like cell expression on titanium implants. J. Mater. Chem. B 2015, 3, 2698–2707. [Google Scholar] [CrossRef]
- Hegedűs, C.; Ho, C.C.; Csík, A.; Biri, S.; Ding, S.J. Enhanced physicochemical and biological properties of ion-implanted titanium using electron cyclotron resonance ion sources. Materials 2016, 9, 25. [Google Scholar] [CrossRef]
- Mombelli, A.; Lang, N.P. The diagnosis and treatment of peri-implantitis. Periodontol. 2000 1998, 17, 63–76. [Google Scholar] [CrossRef] [PubMed]
- Renvert, S.; Polyzois, I.; Claffey, N. Surgical therapy for the control of periimplantitis. Clin. Oral Implants Res. 2012, 23, 84–94. [Google Scholar] [CrossRef] [PubMed]
- Furst, M.M.; Salvi, G.E.; Lang, N.P.; Persson, G.R. Bacterial colonization immediately after installation on oral titanium implants. Clin. Oral Implants Res. 2007, 18, 501–508. [Google Scholar] [CrossRef] [PubMed]
- Charalampakis, G.; Ramberg, P.; Dahlén, G.; Berglundh, T.; Abrahamsson, I. Effect of cleansing of biofilm formed on titanium discs. Clin. Oral Implants Res. 2015, 26, 931–936. [Google Scholar] [CrossRef] [PubMed]
- Zablotsky, M.H.; Diedrich, D.L.; Meffert, R.M. Detoxification of endotoxin-contaminated titanium and hydroxyapatite-coated surfaces utilizing various chemotherapeutic and mechanical modalities. Implant Dent. 1992, 1, 154–158. [Google Scholar] [CrossRef] [PubMed]
- Ntrouka, V.I.; Slot, D.E.; Louropoulou, A.; Van der Weijden, F. The effect of chemotherapeutic agents on contaminated titanium surfaces: A systematic review. Clin. Oral Implants Res. 2011, 22, 681–690. [Google Scholar] [CrossRef] [PubMed]
- Teughels, W.; Van Assche, N.; Sliepen, I.; Quirynen, M. Effect of material characteristics and or surface topography on biofilm development. Clin. Oral Implants Res. 2006, 17, 68–81. [Google Scholar] [CrossRef] [PubMed]
- Renvert, S.; Roos-Jansäker, A.M.; Claffey, N. Non-surgical treatment of peri-implant mucositis and peri-implantitis: A literature review. J. Clin. Periodontol. 2008, 35, 305–315. [Google Scholar] [CrossRef] [PubMed]
- Ntrouka, V.; Hoogenkamp, M.; Zaura, E.; van der Weijden, F. The effect of chemotherapeutic agents on titanium-adherent biofilms. Clin. Oral Implants Res. 2011, 22, 1227–1234. [Google Scholar] [CrossRef] [PubMed]
- Bürgers, R.; Witecy, C.; Hahnel, S.; Gosau, M. The effect of various topical peri-implantitis antiseptics on Staphylococcus epidermidis, Candida albicans, and Streptococcus sanguinis. Arch. Oral Biol. 2012, 57, 940–947. [Google Scholar] [CrossRef] [PubMed]
- Dennison, D.K.; Huerzeler, M.B.; Quinones, C.; Caffesse, R.G. Contaminated implant surfaces: An in vitro comparison of implant surface coating and treatment modalities for decontamination. J. Periodontol. 1994, 65, 942–948. [Google Scholar] [CrossRef] [PubMed]
- Stewart, P.S.; Franklin, M.J. Physiological heterogeneity in biofilms. Nat. Rev. Microbiol. 2008, 6, 199–210. [Google Scholar] [CrossRef] [PubMed]
- Lapenna, D.; Cuccurullo, F. Hypochlorous acid and its pharmacological antagonism: An update picture. Gen. Pharmacol. 1996, 27, 1145–1147. [Google Scholar] [CrossRef]
- Wang, L.; Bassiri, M.; Najafi, R.; Najafi, K.; Yang, J.; Khosrovi, B.; Hwong, W.; Barati, E.; Belisle, B.; Celeri, C.; et al. Hypochlorous acid as a potential wound care agent. Part I. Stabilized hypochlorous acid: A component of the inorganic armamentarium of innate immunity. J. Burns Wounds 2007, 6, 65–79. [Google Scholar]
- Rossi-Fedele, G.; Guastalli, A.R.; Doğramacı, E.J.; Steier, L.; De Figueiredo, J.A.P. Influence of pH changes on chlorine containing endodontic irrigating solutions. Int. Endod. J. 2011, 44, 792–799. [Google Scholar] [CrossRef] [PubMed]
- Mainnemare, A.; Megarbane, B.; Soueidan, A.; Daniel, A.; Chapple, I.L.C. Hypochlorous acid and taurine-N-monochloramine in periodontal diseases. J. Dent. Res. 2004, 83, 823–831. [Google Scholar] [CrossRef] [PubMed]
- Quirynen, M.; de Soete, M.; van Steenberghe, D. Infectious risks for oral implants: A review of the literature. Clin. Oral Implants Res. 2002, 13, 1–19. [Google Scholar] [CrossRef] [PubMed]
- Winkel, A.; Dempwolf, W.; Gellermann, E.; Sluszniak, M.; Grade, S.; Heuer, W.; Eisenburger, M.; Menzel, H.; Stiesch, M. Introducing a semi-coated model to investigate antibacterial effects of biocompatible polymers on titanium surfaces. Int. J. Mol. Sci. 2015, 16, 4327–4342. [Google Scholar] [CrossRef] [PubMed]
- Pier-Francesco, A.; Adams, R.J.; Waters, M.G.J.; Williams, DW. Titanium surface modification and its effect on the adherence of Porphyromonas gingivalis: An in vitro study. Clin. Oral Implants Res. 2006, 17, 633–637. [Google Scholar] [CrossRef] [PubMed]
- Chau, N.P.T.; Chung, N.H.; Jeon, J.G. Relationships between the antibacterial activity of sodium hypochlorite and treatment time and biofilm age in early Enterococcus faecalis biofilms. Int. Endod. J. 2015, 48, 782–789. [Google Scholar] [CrossRef] [PubMed]
- Gomes, B.P.F.A.; Ferraz, C.C.R.; Vianna, M.E.; Berber, V.B.; Teixeira, F.B.; Souza-Filho, F.J. In vitro antimicrobial activity of several concentrations of sodium hypochlorite and chlorhexidine gluconate in the elimination of Enterococcus faecalis. Int. Endod. J. 2001, 34, 424–428. [Google Scholar] [CrossRef] [PubMed]
- Claffey, N.; Clarke, E.; Polyzois, I.; Renvert, S. Surgical treatment of peri-implantitis. J. Clin. Periodontol. 2008, 35, 316–332. [Google Scholar] [CrossRef] [PubMed]
- Zablotsky, M.H.; Wittrig, E.E.; Diedrich, D.L.; Layman, D.L; Meffert, R.M. Fibroblastic growth and attachment on hydroxyapatite-coated titanium surfaces following the use of various detoxification modalities. Part II: Contaminated hydroxyapatite. Implant Dent. 1992, 1, 195–202. [Google Scholar] [CrossRef] [PubMed]
- Ingle, J.I.; Bakland, L.; Baumgartner, J. Ingle’s Endodontics, 6th ed.; BC Decker Inc.: Hamilton, ON, Canada, 2008; pp. 997–998. [Google Scholar]
- Gera, I. The bacterial biofilm and the possibilities of chemical plaque control: Literature review. Fogorv. Szle. 2008, 101, 91–99. [Google Scholar]
- Rutala, W.A.; Weber, D.J. Uses of inorganic hypochlorite (bleach) in health-care facilities. Clin. Microbiol. Rev. 1997, 10, 597–610. [Google Scholar] [PubMed]
- Hoffman, P.N.; Death, J.E.; Coates, D. The stability of sodium hypochlorite solutions. In Disinfectants: Their Use and Evaluation of Effectiveness; Collins, C.H., Allwood, M.C., Bloomfield, S.F., Fox, A., Eds.; Academic Press: London, UK, 1981; pp. 77–83. [Google Scholar]
- Gallo, J.; Holinka, M.; Moucha, C.S. Antibacterial surface treatment for orthopaedic implants. Int. J. Mol. Sci. 2014, 15, 13849–13880. [Google Scholar] [CrossRef] [PubMed]
- Mombelli, A. Microbiology and antimicrobial therapy of peri-implantitis. Periodontol. 2000 2002, 28, 177–189. [Google Scholar] [CrossRef] [PubMed]
- Pullar, J.M.; Vissers, M.C.M.; Winterbourne, C.C. Living with a killer: The effects of hypochlorous acid on mammalian cells. IUBMB Life 2000, 50, 259–266. [Google Scholar] [CrossRef] [PubMed]
- Spickett, C.M.; Jerlich, A.; Panasenko, O.M.; Arnhold, J.; Pitt, A.R.; Stelmaszynska, T.; Schaur, R.J. The reactions of hypochlorous acid, the reactive oxygen species produced by myeloperoxidase, with lipids. Acta Biochim. Pol. 2000, 47, 889–899. [Google Scholar] [PubMed]









© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chen, C.-J.; Chen, C.-C.; Ding, S.-J. Effectiveness of Hypochlorous Acid to Reduce the Biofilms on Titanium Alloy Surfaces in Vitro. Int. J. Mol. Sci. 2016, 17, 1161. https://0-doi-org.brum.beds.ac.uk/10.3390/ijms17071161
Chen C-J, Chen C-C, Ding S-J. Effectiveness of Hypochlorous Acid to Reduce the Biofilms on Titanium Alloy Surfaces in Vitro. International Journal of Molecular Sciences. 2016; 17(7):1161. https://0-doi-org.brum.beds.ac.uk/10.3390/ijms17071161
Chicago/Turabian StyleChen, Chun-Ju, Chun-Cheng Chen, and Shinn-Jyh Ding. 2016. "Effectiveness of Hypochlorous Acid to Reduce the Biofilms on Titanium Alloy Surfaces in Vitro" International Journal of Molecular Sciences 17, no. 7: 1161. https://0-doi-org.brum.beds.ac.uk/10.3390/ijms17071161