90 Days of COVID-19 Social Distancing and Its Impacts on Air Quality and Health in Sao Paulo, Brazil
Abstract
:1. Introduction
2. Materials and Methods
3. Results
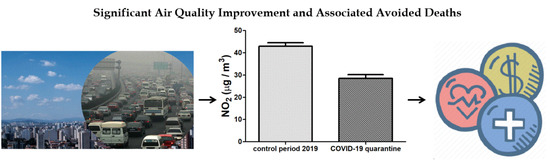
3.1. Air Quality Improvement during 90 Days of COVID-19 Social Distancing
3.2. Associated Health Economics Outcomes
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Brida, M.; Chessa, M.; Gu, H.; Gatzoulis, M.A. The globe on the spotlight: Coronavirus disease 2019 (Covid-19). Int. J. Cardiol. 2020, 310, 170–172. [Google Scholar] [CrossRef] [PubMed]
- Tu, H.; Tu, S.; Gao, S.; Shao, A.; Sheng, J. Current epidemiological and clinical features of COVID-19; a global perspective from China. J. Infect. 2020, 81, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Martini, M.; Gazzaniga, V.; Bragazzi, N.L.; Barberis, I. The Spanish Influenza Pandemic: A lesson from history 100 years after 1918. J. Prev. Med. Hyg. 2019, 60, E64–E67. [Google Scholar] [CrossRef]
- Dhama, K.; Verma, A.K.; Rajagunala, S.; Deb, R.; Karthik, K.; Kapoor, S.M.; Tiwari, R.; Panwar, P.K.; Chakrabort, S. Swine flu is back again: A review. Pakistan J. Biol. Sci. 2012, 15, 1001–1009. [Google Scholar] [CrossRef] [Green Version]
- World Health Organization. Influenza Updates; World Health Organization: Geneva, Switzerland, 2020; Available online: https://www.who.int/influenza/surveillance_monitoring/updates/en/ (accessed on 18 June 2020).
- Centers for Disease Control and Prevention. Influenza (Flu). 2009 H1N1 Pandemic; Centers for Disease Control and Prevention: Atlanta, GA, USA, 2009. Available online: https://www.cdc.gov/flu/pandemic-resources/2009-h1n1-pandemic.html (accessed on 18 June 2020).
- Bradley, K.C.; Jones, C.A.; Tompkins, S.M.; Tripp, R.A.; Russell, R.J.; Gramer, M.R.; Heimburg-Molinaro, J.; Smith, D.F.; Cummings, R.D.; Steinhauer, D.A. Comparison of the receptor binding properties of contemporary swine isolates and early human pandemic H1N1 isolates (Novel 2009 H1N1). Virology 2011, 413, 169–182. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chowell, G.; Ammon, C.E.; Hengartner, N.W.; Hyman, J.M. Estimation of the reproductive number of the Spanish flu epidemic in Geneva, Switzerland. Vaccine 2006, 24, 6747–6750. [Google Scholar] [CrossRef]
- World Health Organization. Coronavirus Disease (COVID-19) Dashboard; World Health Organization: Geneva, Switzerland, 2020; Available online: https://covid19.who.int/ (accessed on 18 June 2020).
- Velavan, T.P.; Meyer, C.G. The COVID-19 epidemic. Trop. Med. Int. Health 2020, 25, 278–280. [Google Scholar] [CrossRef] [Green Version]
- Candido, D.D.S.; Watts, A.; Abade, L.; Kraemer, M.U.G.; Pybus, O.G.; Croda, J.; de Oliveira, W.; Khan, K.; Sabino, E.C.; Faria, N.R. Routes for COVID-19 importation in Brazil. J. Travel Med. 2020, 27. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Singhal, T. A review of coronavirus disease-2019 (COVID-19). Indian J. Pediatr. 2020, 87, 281–286. [Google Scholar] [CrossRef] [Green Version]
- Ahmed, K.; Hayat, S.; Dasgupta, P. Global challenges to urology practice during the COVID-19 pandemic. BJU Int. 2020. [Google Scholar] [CrossRef]
- Rothan, H.A.; Byrareddy, S.N. The epidemiology and pathogenesis of coronavirus disease (COVID-19) outbreak. J. Autoimmun. 2020, 109, 102433. [Google Scholar] [CrossRef] [PubMed]
- Lake, M.A. What we know so far: COVID-19 current clinical knowledge and research. Clin. Med. (Northfield. Il) 2020, 20, 124–127. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Conticini, E.; Frediani, B.; Caro, D. Can atmospheric pollution be considered a co-factor in extremely high level of SARS-CoV-2 lethality in northern Italy? Environ. Pollut. 2020, 261, 114465. [Google Scholar] [CrossRef] [PubMed]
- Frontera, A.; Martin, C.; Vlachos, K.; Sgubin, G. Regional air pollution persistence links to COVID-19 infection zoning. J. Infect. 2020, 81, 318–356. [Google Scholar] [CrossRef]
- Tavella, R.A.; da Silva Júnior, F.M. COVID-19 and air pollution: What do we know so far? Vittalle–Rev. Ciências da Saúde 2020, 1, 22–31. [Google Scholar] [CrossRef]
- Wu, X.; Nethery, R.C.; Sabath, B.M.; Braun, D.; Dominici, F. Exposure to air pollution and COVID-19 mortality in the United States: A nationwide cross-sectional study. medRxiv 2020. [Google Scholar] [CrossRef] [Green Version]
- Urrutia-Pereira, M.; Mello-da-Silva, C.A.; Solé, D. COVID-19 and air pollution: A dangerous association? Allergol. Immunopathol. (Madrid) 2020. [Google Scholar] [CrossRef]
- Brazilian Institute of Statistics and Geography. Estimativa da População-Diretoria de Pesquisas, Coordenação de População e Indicadores Sociais; Brazilian Institute of Statistics and Geography: Rio de Janeiro, Brasil, 2018. Available online: https://www.ibge.gov.br/cidades-e-estados.html (accessed on 18 June 2020).
- Companhia Ambiental do Estado de São Paulo. Qualidade do ar no Estado de São Paulo; Companhia Ambiental do Estado de São Paulo: São Paulo, Brasil, 2019. Available online: https://cetesb.sp.gov.br/ar/publicacoes-relatorios/ (accessed on 18 June 2020).
- Andrade, M.F.; Kumar, P.; de Freitas, E.D.; Ynoue, R.Y.; Martins, J.; Martins, L.D.; Nogueira, T.; Perez-Martinez, P.; de Miranda, R.M.; Albuquerque, T.; et al. Air quality in the megacity of São Paulo: Evolution over the last 30 years and future perspectives. Atmos. Environ. 2017, 159, 66–82. [Google Scholar] [CrossRef] [Green Version]
- Sao Paulo Transit State Department. São Paulo Vehicle Fleet; Sao Paulo Transit State Department: Sao Paulo, Brasil, 2011. Available online: https://www.detran.sp.gov.br/ (accessed on 18 June 2020).
- IEMA. Inventário De Emissões Atmosféricas Do Transporte Rodoviário De Passageiros No Município De São Paulo; IEMA: Sao Paulo, Brasil, 2020. Available online: http://emissoes.energiaeambiente.org.br/graficos (accessed on 18 June 2020).
- Scovronick, N.; França, D.; Alonso, M.; Almeida, C.; Longo, K.; Freitas, S.; Rudorff, B.; Wilkinson, P. Air quality and health impacts of future ethanol production and use in São Paulo State, Brazil. Int. J. Environ. Res. Public Health 2016, 13, 695. [Google Scholar] [CrossRef] [Green Version]
- Abe, K.; Miraglia, S. Health Impact assessment of air pollution in São Paulo, Brazil. Int. J. Environ. Res. Public Health 2016, 13, 694. [Google Scholar] [CrossRef] [Green Version]
- Leirião, L.F.L.; Debone, D.; Pauliquevis, T.; Rosário, N.M.É.; Miraglia, S.G.E.K. Environmental and public health effects of vehicle emissions in a large metropolis: Case study of a truck driver strike in Sao Paulo, Brazil. Atmos. Pollut. Res. 2020. [Google Scholar] [CrossRef]
- Rizzoli, A.; Tagliapietra, V.; Cagnacci, F.; Marini, G.; Arnoldi, D.; Rosso, F.; Rosà, R. Parasites and wildlife in a changing world: The vector-host-pathogen interaction as a learning case. Int. J. Parasitol. Parasites Wildl. 2019, 9, 394–401. [Google Scholar] [CrossRef] [PubMed]
- Allen, T.; Murray, K.A.; Zambrana-Torrelio, C.; Morse, S.S.; Rondinini, C.; Di Marco, M.; Breit, N.; Olival, K.J.; Daszak, P. Global hotspots and correlates of emerging zoonotic diseases. Nat. Commun. 2017, 8, 1124. [Google Scholar] [CrossRef]
- Guo, F.; Bonebrake, T.C.; Gibson, L. Land-use change alters host and vector communities and may elevate disease risk. Ecohealth 2019, 16, 647–658. [Google Scholar] [CrossRef] [PubMed]
- Loh, E.H.; Zambrana-Torrelio, C.; Olival, K.J.; Bogich, T.L.; Johnson, C.K.; Mazet, J.A.K.; Karesh, W.; Daszak, P. Targeting transmission pathways for emerging zoonotic disease surveillance and control. Vector Borne Zoonotic Dis. 2015, 15, 432–437. [Google Scholar] [CrossRef] [Green Version]
- D’Adamo, I.; Falcone, P.M.; Martin, M.; Rosa, P. A Sustainable revolution: Let’s go sustainable to get our globe cleaner. Sustainability 2020, 12, 4387. [Google Scholar] [CrossRef]
- Companhia Ambiental do Estado de São Paulo. QUALAR. Sistema de Informações da Qualidade do Ar; CETESB: São Paulo, Brasil, 2020. Available online: https://qualar.cetesb.sp.gov.br/qualar/home.do (accessed on 18 June 2020).
- AGRITEMPO. Brazilian Agro-Meteorological Monitoring System; AGRITEMPO: Rio de Janeiro, Brasil, 2019. Available online: https://www.agritempo.gov.br/agritempo/index.jsp (accessed on 18 June 2020).
- Sánchez-Ccoyllo, O.R.; de Fátima Andrade, M. The influence of meteorological conditions on the behavior of pollutants concentrations in São Paulo, Brazil. Environ. Pollut. 2002, 116, 257–263. [Google Scholar] [CrossRef]
- Zeri, M.; Carvalho, V.S.B.; Cunha-Zeri, G.; Oliveira-Júnior, J.F.; Lyra, G.B.; Freitas, E.D. Assessment of the variability of pollutants concentration over the metropolitan area of São Paulo, Brazil, using the wavelet transform. Atmos. Sci. Lett. 2016, 17, 87–95. [Google Scholar] [CrossRef] [Green Version]
- Carneseca, E.C.; Achcar, J.A.; Martinez, E.Z. Association between particulate matter air pollution and monthly inhalation and nebulization procedures in Ribeirão Preto, São Paulo State, Brazil. Cad. Saude Publica 2012, 28, 1591–1598. [Google Scholar] [CrossRef] [Green Version]
- Tanzer-Gruener, R.; Li, J.; Eilenberg, S.R.; Robinson, A.L.; Presto, A.A. Impacts of modifiable factors on ambient air pollution: A case study of COVID-19 shutdowns. Environ. Sci. Technol. Lett. 2020, 7, 554–559. [Google Scholar] [CrossRef]
- Freitas, E.D.; Ibarra-Espinosa, S.A.; Gavidia-Calderón, M.E.; Rehbein, A.; Abou Rafee, S.A.; Martins, J.A.; Martins, L.D.; Santos, U.P.; Ning, M.F.; Andrade, M.F. Mobility restrictions and air quality under COVID-19 pandemic in São Paulo, Brazil. Earth Sci. 2020. [Google Scholar] [CrossRef]
- Wang, C.; Wang, T.; Wang, P.; Rakitin, V. Comparison and validation of TROPOMI and OMI NO2 Observations over China. Atmosphere (Basel) 2020, 11, 636. [Google Scholar] [CrossRef]
- Lopez, J.; Branch, J.W.; Chen, G. Line-based image segmentation method: A new approach to segment VHSR remote sensing images automatically. Eur. J. Remote Sens. 2019, 52, 613–631. [Google Scholar] [CrossRef] [Green Version]
- Ciobotaru, A.-M.; Andronache, I.; Ahammer, H.; Radulovic, M.; Peptenatu, D.; Pintilii, R.-D.; Drăghici, C.-C.; Marin, M.; Carboni, D.; Mariotti, G.; et al. Application of Fractal and gray-level co-occurrence matrix indices to assess the forest dynamics in the curvature Carpathians—Romania. Sustainability 2019, 11, 6927. [Google Scholar] [CrossRef] [Green Version]
- Sistema de Monitoramento Inteligente do Governo de São Paulo. Available online: https://www.saopaulo.sp.gov.br/coronavirus/isolamento/ (accessed on 27 June 2020).
- Abe, K.C.; dos Santos, G.M.S.; Coêlho, M.; de Sousa, Z.S.; Miraglia, S.G.E.K. PM10 exposure and cardiorespiratory mortality–estimating the effects and economic losses in São Paulo, Brazil. Aerosol Air Qual. Res. 2018, 18, 3127–3133. [Google Scholar] [CrossRef] [Green Version]
- Bell, M.L.; Ebisu, K.; Peng, R.D.; Samet, J.M.; Dominici, F. Hospital admissions and chemical composition of fine particle air pollution. Am. J. Respir. Crit. Care Med. 2009, 179, 1115–1120. [Google Scholar] [CrossRef]
- Hemminki, K.; Pershagen, G. Cancer risk of air pollution: Epidemiological evidence. Environ. Health Perspect. 1994, 102, 187–192. [Google Scholar] [CrossRef] [PubMed]
- Hoek, G.; Brunekreef, B.; Goldbohm, S.; Fischer, P.; van den Brandt, P.A. Association between mortality and indicators of traffic-related air pollution in the Netherlands: A cohort study. Lancet 2002, 360, 1203–1209. [Google Scholar] [CrossRef] [Green Version]
- Jerrett, M.; Burnett, R.T.; Ma, R.; Pope, C.A.; Krewski, D.; Newbold, K.B.; Thurston, G.; Shi, Y.; Finkelstein, N.; Calle, E.E.; et al. Spatial analysis of air pollution and mortality in Los Angeles. Epidemiology 2005, 16, 727–736. [Google Scholar] [CrossRef] [PubMed]
- Nyhan, M.M.; Kloog, I.; Britter, R.; Ratti, C.; Koutrakis, P. Quantifying population exposure to air pollution using individual mobility patterns inferred from mobile phone data. J. Expo. Sci. Environ. Epidemiol. 2019, 29, 238–247. [Google Scholar] [CrossRef] [PubMed]
- Ostro, B.; Malig, B.; Broadwin, R.; Basu, R.; Gold, E.B.; Bromberger, J.T.; Derby, C.; Feinstein, S.; Greendale, G.A.; Jackson, E.A.; et al. Chronic PM2.5 exposure and inflammation: Determining sensitive subgroups in mid-life women. Environ. Res. 2014, 132, 168–175. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mudu, P.; Gapp, C.; Dunbar, M. AirQ+ 1.0 Example of Calculations; World Health Organization: Geneva, Switzerland, 2016. [Google Scholar]
- Mead, R.W.; Brajer, V. Rise of the Automobiles: The costs of increased NO 2 pollution in China’s changing urban environment. J. Contemp. China 2006, 15, 349–367. [Google Scholar] [CrossRef]
- Ostro, B.; Prüss-Ustün, A.; Campbell-lendrum, D.; Corvalán, C.; Woodward, A. Outdoor Air Pollution: Assessing the Environmental Burden of Disease at National and Local Levels; World Health Organization: Geneva, Switzerland, 2004; pp. 1–54. ISBN 92 4 159146 3. [Google Scholar]
- Debone, D.; Leirião, L.F.L.; Miraglia, S.G.E.K. Air quality and health impact assessment of a truckers’ strike in Sao Paulo state, Brazil: A case study. Urban. Clim. 2020, 34, 100687. [Google Scholar] [CrossRef]
- DATASUS. Brazilian Health System Database (TABNET). Available online: http://datasus.saude.gov.br/informacoes-de-saude/tabnet (accessed on 18 June 2020).
- Coogan, P.F.; White, L.F.; Yu, J.; Burnett, R.T.; Seto, E.; Brook, R.D.; Palmer, J.R.; Rosenberg, L.; Jerrett, M. PM2. 5 and diabetes and hypertension incidence in the Black Women’s Health Study. Epidemiology 2016, 27, 202. [Google Scholar] [PubMed] [Green Version]
- Li, R.; Zhou, R.; Zhang, J. Function of PM2. 5 in the pathogenesis of lung cancer and chronic airway inflammatory diseases. Oncol. Lett. 2018, 15, 7506–7514. [Google Scholar] [PubMed] [Green Version]
- SEADE. State Data Analysis System. Available online: https://www.seade.gov.br/institucional/ (accessed on 27 June 2020).
- Alberini, A.; Hunt, A.; Markandya, A. Willingness to pay to reduce mortality risks: Evidence from a three-country contingent valuation study. Environ. Resour. Econ. 2006, 33, 251–264. [Google Scholar] [CrossRef] [Green Version]
- Ding, D.; Xing, J.; Wang, S.; Liu, K.; Hao, J. Estimated contributions of emissions controls, meteorological factors, population growth, and changes in baseline mortality to reductions in ambient PM2.5 and PM2.5-related mortality in China, 2013–2017. Environ. Health Perspect. 2019, 127, 067009. [Google Scholar] [CrossRef]
- Ran, T.; Nurmagambetov, T.; Sircar, K. Economic implications of unintentional carbon monoxide poisoning in the United States and the cost and benefit of CO detectors. Am. J. Emerg. Med. 2018, 36, 414–419. [Google Scholar] [CrossRef]
- Robinson, L.A. Estimating the values of mortality risk reductions in low-and middle-income countries. J. Benefit Cost Anal. 2017, 8, 205–214. [Google Scholar] [CrossRef] [Green Version]
- Wolfe, P.; Davidson, K.; Fulcher, C.; Fann, N.; Zawacki, M.; Baker, K.R. Monetized health benefits attributable to mobile source emission reductions across the United States in 2025. Sci. Total Environ. 2019, 650, 2490–2498. [Google Scholar] [CrossRef]
- Roy, R.; Braathen, N.A. The Rising Cost of Ambient Air Pollution thus far in the 21st Century: Results from the BRIICS and the OECD Countries; OECD Environ. Working Paper; OECD: Paris, France, 2017; Available online: https://0-www-oecd--ilibrary-org.brum.beds.ac.uk/ (accessed on 27 June 2020).
- Isaifan, R.J. The dramatic impact of Coronavirus outbreak on air quality: Has it saved as much as it has killed so far? Glob. J. Environ. Sci. Manag. 2020, 6, 275–288. [Google Scholar]
- Anjum, N.A. Good in the worst: COVID-19 restrictions and ease in global air pollution. 2020; preprint. [Google Scholar] [CrossRef]
- Xu, K.; Cui, K.; Young, L.-H.; Hsieh, Y.-K.; Wang, Y.-F.; Zhang, J.; Wan, S. Impact of the COVID-19 event on air quality in central China. Aerosol Air Qual. Res. 2020, 20, 915–929. [Google Scholar] [CrossRef] [Green Version]
- Chou, S.C.; Bustamante, J.F.; Gomes, J.L. Evaluation of Eta Model seasonal precipitation forecasts over South America. Nonlinear Process. Geophys. 2005, 12, 537–555. [Google Scholar] [CrossRef] [Green Version]
- Pellon de Miranda, F.; Marmol, A.M.Q.; Pedroso, E.C.; Beisl, C.H.; Welgan, P.; Morales, L.M. Analysis of RADARSAT-1 data for offshore monitoring activities in the Cantarell Complex, Gulf of Mexico, using the unsupervised semivariogram textural classifier (USTC). Can. J. Remote Sens. 2004, 30, 424–436. [Google Scholar] [CrossRef]
- Ramis, J.E.; dos Santos, E.A. The impact of thermal comfort in the perceived level of service and energy costs of three Brazilian airports. J. Transp. Lit. 2013, 7, 192–206. [Google Scholar] [CrossRef] [Green Version]
- Yu, K.-P. Enhancement of the deposition of ultrafine secondary organic aerosols by the negative air ion and the effect of relative humidity. J. Air Waste Manag. Assoc. 2012, 62, 1296–1304. [Google Scholar] [CrossRef] [Green Version]
- Markandya, A.; Sampedro, J.; Smith, S.J.; Van Dingenen, R.; Pizarro-Irizar, C.; Arto, I.; González-Eguino, M. Health co-benefits from air pollution and mitigation costs of the Paris Agreement: A modelling study. Lancet Planet. Heal. 2018, 2, e126–e133. [Google Scholar] [CrossRef] [Green Version]
- Sharma, S.; Zhang, M.; Anshika; Gao, J.; Zhang, H.; Kota, S.H. Effect of restricted emissions during COVID-19 on air quality in India. Sci. Total Environ. 2020, 728, 138878. [Google Scholar] [CrossRef]
- Dantas, G.; Siciliano, B.; França, B.B.; da Silva, C.M.; Arbilla, G. The impact of COVID-19 partial lockdown on the air quality of the city of Rio de Janeiro, Brazil. Sci. Total Environ. 2020, 729, 139085. [Google Scholar] [CrossRef]
- Grande, G.; Ljungman, P.L.S.; Eneroth, K.; Bellander, T.; Rizzuto, D. Association between cardiovascular disease and long-term exposure to air pollution with the risk of dementia. JAMA Neurol. 2020. [Google Scholar] [CrossRef] [Green Version]
- Watts, N.; Amann, M.; Arnell, N.; Ayeb-Karlsson, S.; Belesova, K.; Berry, H.; Bouley, T.; Boykoff, M.; Byass, P.; Cai, W.; et al. The 2018 report of the Lancet Countdown on health and climate change: Shaping the health of nations for centuries to come. Lancet 2018, 392, 2479–2514. [Google Scholar] [CrossRef]
- Baldwin, R.E.; di Mauro, W. Mitigating the COVID Economic Crisis; CEPR Press: Washington, DC, USA, 2020; Available online: https://iheid.tind.io/record/298223 (accessed on 18 June 2020).
- OECD. OECD Economic Outloo; OECD: Paris, France, 2020; Volume 2020, ISBN 9789264524156. [Google Scholar]
- Fernandes, N. Economic effects of coronavirus outbreak (COVID-19) on the world economy. SSRN Electron. J. 2020. [Google Scholar] [CrossRef]
- WHO. Quantification of Health Effects of Exposure to Air Pollution: Report on a WHO Working Group, Bilthoven, Netherlands 20–22 November 2000; World Health Organization: Geneva, Switzerland, 2000; Available online: https://apps.who.int/iris/handle/10665/108463 (accessed on 18 June 2020).
- Blangiardo, M.; Pirani, M.; Kanapka, L.; Hansell, A.; Fuller, G. A hierarchical modelling approach to assess multi pollutant effects in time-series studies. PLoS ONE 2019, 14, e0212565. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Koehl, A. Urban transport and COVID-19: Challenges and prospects in low-and middle-income countries. Cities Heath 2020, 4, 1–6. [Google Scholar]
- D’Adamo, I.; Rosa, P. How do you see infrastructure? Green energy to provide economic growth after COVID-19. Sustainability 2020, 12, 4738. [Google Scholar] [CrossRef]
- Chen, S.; Bloom, D.E. The macroeconomic burden of noncommunicable diseases associated with air pollution in China. PLoS ONE 2019, 14, e0215663. [Google Scholar] [CrossRef]
- Neira, M.; Prüss-Ustün, A.; Mudu, P. Reduce air pollution to beat NCDs: From recognition to action. Lancet 2018, 392, 1178–1179. [Google Scholar] [CrossRef]







| Precipitation (mm) | Wind (m/s) | Temperature (°C) | ||||
|---|---|---|---|---|---|---|
| Control Period | Quarantine | Control Period | Quarantine | Control Period | Quarantine | |
| N | 91 | 91 | 91 | 91 | 91 | 91 |
| Mean (SD) | 3.7 (8.1) | 1.5 (4.3) | 1.8 (0.4) | 1.9 (0.4) | 26.4 (3.3) | 25.3 (3.2) |
| Median | 0.1 | 0 | 1.9 | 2.0 | 27.5 | 25.7 |
| Minimum | 0 | 0 | 1 | 1 | 17.8 | 15.8 |
| Maximum | 37.2 | 25.7 | 2.8 | 3.6 | 32.4 | 32.2 |
| Weeks | Precipitation (mm) | Wind (m/s) | Temperature (°C) | |||
|---|---|---|---|---|---|---|
| Control Period | Quarantine | Control Period | Quarantine | Control Period | Quarantine | |
| 1 | 2.6 (1.7) | 5.2 (9.6) | 2.3 (0.1) | 2.2 (0.1) | 26.5 (1.7) | 28.5 (1.2) |
| 2 | 0.8 (1.6) | 2.6 (6.9) | 2.1 (0.2) | 2.3 (0.2) | 28.6 (0.9) | 26.9 (0.6) |
| 3 | 0.05 (0.1) | 1.7 (4.6) | 2.0 (0.2) | 2.2 (0.2) | 29.5 (0.8) | 28.6 (0.4) |
| 4 | 1.9 (3.4) | 0.5 (1.2) | 1.9 (0.1) | 2.1 (0.1) | 26.3 (1.9) | 24.3 (1.2) |
| 5 | 0.4 (0.9) | 0.8 (1.7) | 1.8 (0.1) | 2.1 (0.1) | 28.5 (0.5) | 24.3 (0.7) |
| 6 | 0.4 (0.7) | 0 (0) | 1.8 (0.1) | 1.7 (0.1) | 28.7 (0.3) | 26.9 (0.6) |
| 7 | 0.2 (0.3) | 0.03 (0.1) | 1.6 (0.1) | 1.9 (0.1) | 27.9 (0.8) | 26.1 (0.8) |
| 8 | 0.5 (0.7) | 0.5 (1.2) | 1.8 (0.2) | 1.9 (0.1) | 26.7 (1.1) | 23.4 (1.4) |
| 9 | 2.4 (1.6) | 0.5 (1) | 1.9 (0.1) | 1.7 (0.2) | 26.1 (1.4) | 23.7 (1.3) |
| 10 | 0.9 (1.3) | 1.2 (2.6) | 1.9 (0.2) | 2.3 (0.3) | 24.9 (1.2) | 23.9 (1.5) |
| 11 | 1.3 (3.1) | 0.03 (0.1) | 2.1 (0.2) | 2.1 (0.3) | 25.2 (1.6) | 22.6 (1.0) |
| 12 | 0 (7.1) | 5.5 (7.4) | 2.1 (0.2) | 1.6 (0.1) | 20.4 (1.3) | 23 (1.0) |
| 13 | 0.4 (0.7) | 0.7 (1.3) | 1.3 (0.1) | 1.8 (0.2) | 25.2 (0.8) | 26.2 (1.3) |
| Relative Risks and Attributable Fractions | ||||||
|---|---|---|---|---|---|---|
| Weeks | PM10 | PM2.5 | NO2 | |||
| RR | AF (%) | RR | AF (%) | RR | AF (%) | |
| 1 | 0.998 | −0.13 | 0.997 | −0.26 | 0.996 | −0.37 |
| 2 | 1.007 | 0.72 | 1.016 | 1.60 | 1.023 | 2.30 |
| 3 | 1.013 | 1.38 | 1.036 | 3.56 | 1.039 | 3.77 |
| 4 | 1.002 | 0.29 | 1.017 | 1.74 | 1.024 | 2.39 |
| 5 | 1.002 | 0.28 | 1.013 | 1.34 | 1.018 | 1.84 |
| 6 | 1.008 | 0.84 | 1.029 | 2.86 | 1.026 | 2.63 |
| 7 | 1.004 | 0.47 | 1.029 | 2.86 | 1.030 | 2.96 |
| 8 | 1.006 | 0.60 | 1.032 | 3.18 | 1.019 | 1.90 |
| 9 | 0.996 | −0.36 | 0.996 | −0.38 | 1.004 | 0.46 |
| 10 | 1.007 | 0.79 | 1.037 | 3.62 | 1.039 | 3.75 |
| 11 | 1.000 | 0.01 | 1.002 | 0.20 | 1.004 | 0.44 |
| 12 | 0.993 | −0.70 | 0.984 | −1.61 | 1.003 | 0.37 |
| 13 | 1.010 | 1.07 | 1.055 | 5.22 | 1.027 | 2.71 |
| Deaths | Economic Outcome (US $million) * | |
|---|---|---|
| COVID-19 deaths | 5623 | 10,571.2 (−) |
| PM10 avoided deaths | 78 | 146.6 (+) |
| PM2.5 avoided deaths | 337 | 633.6 (+) |
| NO2 avoided deaths | 383 | 720.0 (+) |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Debone, D.; da Costa, M.V.; Miraglia, S.G.E.K. 90 Days of COVID-19 Social Distancing and Its Impacts on Air Quality and Health in Sao Paulo, Brazil. Sustainability 2020, 12, 7440. https://0-doi-org.brum.beds.ac.uk/10.3390/su12187440
Debone D, da Costa MV, Miraglia SGEK. 90 Days of COVID-19 Social Distancing and Its Impacts on Air Quality and Health in Sao Paulo, Brazil. Sustainability. 2020; 12(18):7440. https://0-doi-org.brum.beds.ac.uk/10.3390/su12187440
Chicago/Turabian StyleDebone, Daniela, Mariana V. da Costa, and Simone G. E. K. Miraglia. 2020. "90 Days of COVID-19 Social Distancing and Its Impacts on Air Quality and Health in Sao Paulo, Brazil" Sustainability 12, no. 18: 7440. https://0-doi-org.brum.beds.ac.uk/10.3390/su12187440