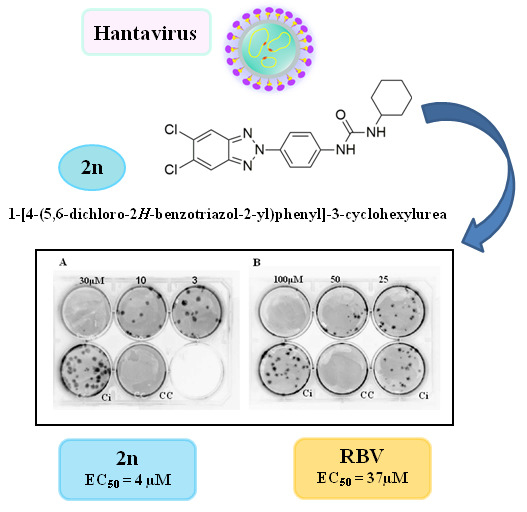
5,6-Dichloro-2-Phenyl-Benzotriazoles: New Potent Inhibitors of Orthohantavirus
Abstract
:1. Introduction
2. Materials and methods
2.1. Chemistry
2.2. General Procedure for Preparation of Derivatives 3f, j and 4f, j.
2.2.1. N-(4-(2H-benzo[d][1,2,3]triazol-2-yl)phenyl)-4-methylbenzamide (3f)
2.2.2. N-(4-(2H-benzo[d][1,2,3]triazol-2-yl)phenyl)-3,4,5-trimethoxybenzamide (3j)
2.2.3. N-(4-(5,6-dimethyl-2H-benzo[d][1,2,3]triazol-2-yl)phenyl)-4-methylbenzamide (4f)
2.2.4. N-(4-(5,6-dimethyl-2H-benzo[d][1,2,3]triazol-2-yl)phenyl)-3,4,5-trimethoxybenzamide (4j)
2.3. Cells, Viruses, Reagents
2.4. Cytotoxicity Assays
2.5. Orthohantavirus Antiviral Screening Assay
2.6. Yield Reduction assay
2.7. Statistical Analysis
3. Results and Discussion
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Schmaljohn, C.; Hooper, J.W. Bunyaviridae: The viruses and their replication. In Fields Virology, 4th ed.; Knipe, D.M., Howley, P.M., Griffin, D.E., Lamb, R.A., Martin, M.A., Roizman, B., Straus, S.E., Eds.; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2001; pp. 1581–1602. [Google Scholar]
- Shi, M.; Lin, X.D.; Chen, X.; Tian, J.H.; Chen, L.J.; Li, K.; Wang, W.; Eden, J.S.; Shen, J.J.; Liu, L.; et al. The evolutionary history of vertebrate RNA viruses. Nature 2018, 556, 197–202. [Google Scholar] [CrossRef] [PubMed]
- Jonsson, C.B.; Figueiredo, L.T.M.; Vapalahti, O. A Global Perspective on Hantavirus Ecology, Epidemiology, and Disease. Clin. Microbiol. Rev. 2010, 23, 412–441. [Google Scholar] [CrossRef] [Green Version]
- Hjelle, B.; Torres-Pérez, F. Hantaviruses in the Americas and Their Role as Emerging Pathogens. Viruses 2010, 2, 2559–2586. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gavrilovskaya, I.N.; Brown, E.J.; Ginsberg, M.H.; Mackow, E.R. Cellular entry of hantaviruses which cause hemorrhagic fever with renal syndrome is mediated by β3 integrins. J. Virol. 1999, 73, 3951–3959. [Google Scholar] [CrossRef] [Green Version]
- Jonsson, C.B.; Schmaljohn, C.S. Replication of hantaviruses. Curr. Top. Microbiol. Immunol. 2001, 256, 15–32. [Google Scholar]
- Sidwell, R.W.; Smee, D.F. Viruses of the Bunya- and Togaviridae families: Potential as bioterrorism agents and means of control. Antivir. Res. 2003, 57, 101–111. [Google Scholar] [CrossRef]
- Ogg, M.; Jonsson, C.B.; Camp, J.V.; Hooper, J.W. Ribavirin Protects Syrian Hamsters against Lethal Hantavirus Pulmonary Syndrome—After Intranasal Exposure to Andes Virus. Viruses 2013, 5, 2704–2720. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Krüger, D.H.; Schönrich, G.; Klempa, B. Human pathogenic hantaviruses and prevention of infection. Hum. Vaccin. 2011, 7, 685–693. [Google Scholar] [CrossRef] [Green Version]
- Huggins, J.W.; Hsiang, C.M.; Cosgri, T.M.; Guang, M.Y.; Smith, J.I.; Wu, Z.O.; LeDuc, J.W.; Zheng, Z.M.; Meegan, J.M.; Wang, Q.N.; et al. Prospective, double-blind, concurrent, placebo-controlled clinical trial of intravenous ribavirin therapy of hemorrhagic fever with renal syndrome. J. Infect. Dis. 1991, 164, 1119–1127. [Google Scholar] [CrossRef]
- Malinin, O.V.; Platonov, A.E. Insufficient efficacy and safety of intravenous ribavirin in treatment of haemorrhagic fever with renal syndrome caused by puumala virus. Infect. Dis. 2017, 49, 514–520. [Google Scholar] [CrossRef]
- Chapman, L.E.; Mertz, G.J.; Peters, C.J. Intravenous ribavirin for hantavirus pulmonary syndrome: Safety and tolerance during 1 year of open-label experience. Ribavirin Study Group. Antivir. Ther. 1999, 4, 211–219. [Google Scholar] [PubMed]
- Chung, D.H.; Kumarapperuma, S.C.; Sun, Y.; Li, Q.; Chu, Y.K.; Arterburn, J.B.; Parker, W.B.; Smith, J.; Spik, K.; Ramanathan, H.N.; et al. Synthesis of 1-beta-D-ribofuranosyl-3-ethynyl-[1,2,4]triazole and its in vitro and in vivo efficacy against Hantavirus. Antivir. Res. 2008, 79, 19–27. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brocato, R.L.; Hooper, J.W. Progress on the Prevention and Treatment of Hantavirus Disease. Viruses 2019, 11, 610. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Carta, A.; Loriga, G.; Piras, S.; Paglietti, G.; Ferrone, M.; Fermeglia, M.; Pricl, S.; La Colla, P.; Secci, B.; Collu, G.; et al. Synthesis and in vitro evaluation of the anti-viral activity of N-[4-(1H(2H) benzotriazol-1(2)-yl)phenyl]alkylcarboxamides. Med. Chem. 2006, 2, 577–589. [Google Scholar] [CrossRef] [PubMed]
- Carta, A.; Loriga, M.; Piras, S.; Paglietti, G.; Ferrone, M.; Fermeglia, M.; Pricl, S.; La Colla, P.; Collu, G.; Sanna, T.; et al. Synthesis and anti-picornaviridae in vitro activity of a new class of helicaseinhibitors the N,N’-bis[4 -(1H(2H)-benzotriazol-1(2)-yl)phenyl] alkyldicarboxamides. Med. Chem. 2007, 3, 520–532. [Google Scholar] [CrossRef]
- Carta, A.; Pricl, S.; Piras, S.; Fermeglia, M.; La Colla, P.; Loddo, R. Activity and molecular modeling of a new small molecule active against NNRTI-resistant HIV-1 mutants. Eur. J. Med. Chem. 2009, 44, 5117–5122. [Google Scholar] [CrossRef]
- Carta, A.; Briguglio, I.; Piras, S.; Corona, P.; Boatto, G.; Nieddu, M.; Giunchedi, P.; Marongiu, M.E.; Giliberti, G.; Iuliano, F.; et al. Quinolinetricyclic derivatives. Design, synthesis and evaluation of the antiviral activity of three new classes of RNA-dependent RNA polymerase inhibitors. Bioorg. Med. Chem. 2011, 19, 7070–7084. [Google Scholar] [CrossRef]
- Briguglio, I.; Piras, S.; Corona, P.; Gavini, E.; Nieddu, M.; Boatto, G.; Carta, A. Benzotriazole: An overview on its versatile biological behavior. Eur. J. Med. Chem. 2015, 97, 612–648. [Google Scholar] [CrossRef]
- Piras, S.; Sanna, G.; Carta, A.; Corona, P.; Ibba, R.; Loddo, R.; Madeddu, S.; Caria, P.; Aulic, S.; Laurini, E.; et al. Dichloro-phenyl-benzotriazoles: A new selective class of humanrespiratory syncytial virus entry inhibitors. Front. Chem. 2019, 7, 247. [Google Scholar] [CrossRef]
- Piras, S.; Corona, P.; Ibba, R.; Riu, F.; Sanna, G.; Madeddu, S.; Delogu, I.; Loddo, R.; Carta, A. Novel Benzotriazole Derivatives as Selective Inhibitors of Coxsackies B5 virus: 1-[4-(5,6-dimethyl(H)-1H(2H)-benzotriazol-1(2)-yl)phenyl]-3-alkyl(aryl)urea. Med. Chem. 2020, 16, 1. [Google Scholar] [CrossRef]
- Heider, H.; Ziaja, B.; Priemer, C.; Lundkvist, A.; Neyts, J.; Krüger, D.H.; Ulrich, R. A chemiluminescence detection method of hantaviral antigens in neutralisation assays and inhibitor studies. J. Virol. Methods 2001, 96, 17–23. [Google Scholar] [CrossRef]
- Ye, C.; Wang, D.; Liu, H.; Ma, H.; Dong, Y.; Yao, M.; Wang, Y.; Zhang, H.; Zhang, L.; Cheng, L.; et al. An Improved Enzyme-Linked Focus Formation Assay Revealed Baloxavir Acid as a Potential Antiviral Therapeutic Against Hantavirus Infection. Front. Pharmacol. 2019, 10, 1203. [Google Scholar] [CrossRef] [PubMed]






© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sanna, G.; Piras, S.; Madeddu, S.; Busonera, B.; Klempa, B.; Corona, P.; Ibba, R.; Murineddu, G.; Carta, A.; Loddo, R. 5,6-Dichloro-2-Phenyl-Benzotriazoles: New Potent Inhibitors of Orthohantavirus. Viruses 2020, 12, 122. https://0-doi-org.brum.beds.ac.uk/10.3390/v12010122
Sanna G, Piras S, Madeddu S, Busonera B, Klempa B, Corona P, Ibba R, Murineddu G, Carta A, Loddo R. 5,6-Dichloro-2-Phenyl-Benzotriazoles: New Potent Inhibitors of Orthohantavirus. Viruses. 2020; 12(1):122. https://0-doi-org.brum.beds.ac.uk/10.3390/v12010122
Chicago/Turabian StyleSanna, Giuseppina, Sandra Piras, Silvia Madeddu, Bernardetta Busonera, Boris Klempa, Paola Corona, Roberta Ibba, Gabriele Murineddu, Antonio Carta, and Roberta Loddo. 2020. "5,6-Dichloro-2-Phenyl-Benzotriazoles: New Potent Inhibitors of Orthohantavirus" Viruses 12, no. 1: 122. https://0-doi-org.brum.beds.ac.uk/10.3390/v12010122