Published online Aug 28, 2005. doi: 10.3748/wjg.v11.i32.5084
Revised: April 5, 2005
Accepted: April 9, 2005
Published online: August 28, 2005
We herein describe the case of a 27-year-old female, who presented with a large mass of the upper left abdominal cavity discovered incidentally, through an annual health examination. Preoperative studies including abdominal ultrasonography and magnetic resonance imaging were performed, but they could not accurately determine the nature of the tumor. At laparotomy, a large cystic tumor of the small bowel mesentery was found. Histopathologic examination diagnosed the tumor as a cystic lymphangioma. Although lymphangiomas are rare, especially in the abdomen of adults, they may sometimes present as acute abdomen, causing complications that require emergent surgery.
- Citation: Chen CW, Hsu SD, Lin CH, Cheng MF, Yu JC. Cystic lymphangioma of the jejunal mesentery in an adult: A case report. World J Gastroenterol 2005; 11(32): 5084-5086
- URL: https://www.wjgnet.com/1007-9327/full/v11/i32/5084.htm
- DOI: https://dx.doi.org/10.3748/wjg.v11.i32.5084
Lymphangiomas are rare benign tumors. They are preferentially located in the head, neck, and axilla in children. However, lymphangiomas in the peritoneal cavity are extremely rare, particularly in adults. This report describes a case of an adult with a large lymphangioma of the jejunal mesentery.
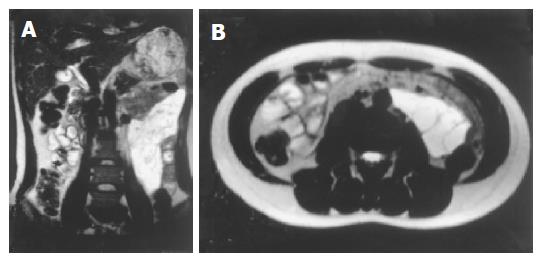
A 27-year-old female was referred to us on April 10, 2003 due to an intra-abdominal mass lesion found incidentally, during her annual health examination. Recently, she had begun to experience epigastralgia and abdominal fullness especially after having meals. Her family and medical history were unremarkable. She had no history of previous abdominal surgery. On physical examination, a soft, non-tender mass was palpated in the upper left abdomen. Auscultation of the abdomen revealed normal bowel sounds. Laboratory data including tumor markers were within normal limits. A plain film of the abdomen showed several loops of small intestine without dilatation or air-fluid level. Abdominal ultrasonography revealed a large, multilocular, cystic mass with an obscure margin. MRI of the abdomen showed a large homogeneous mass measuring 16 cm×7 cm×5 cm in size with multiple enhancement septa by contrast medium. This lesion was located at the anterior aspect of the left kidney and descending colon, causing compression and stretching of the small bowel (Figure 1). A cystic neoplasm of the mesentery was considered.
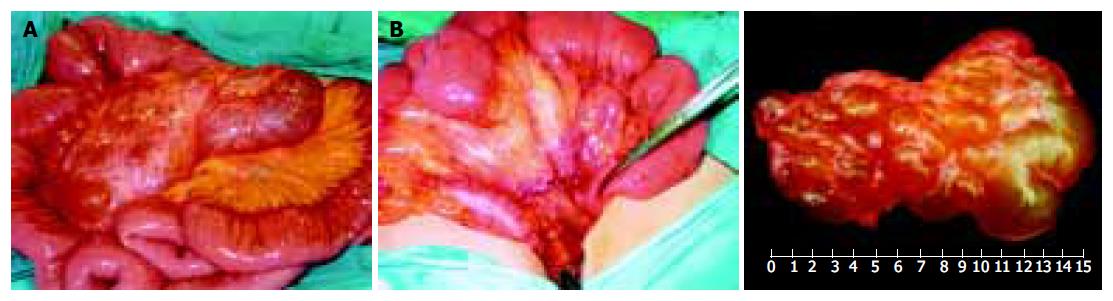
At laparotomy, a yellowish cystic tumor with soft consistency was found in the mesentery of the jejunum, about 30 cm distal to Treitz’s ligament. The tumor was not adhered to the wall of the intestine or adjacent organs. No ascites was seen in the peritoneal cavity, nor was there any dilatation or inflammatory change of the intestines or mesentery. With careful dissection of the mesenteric arteries, the tumor was resected completely without resection of the intestine. The specimen consisted of one piece of cystic tumor in the mesentery measuring 15 cm×8 cm×6 cm. Macroscopically, it was yellowish in color and soft in consistency (Figure 2). Microscopically, the sections showed numerous dilated lymphatic channels of varying sizes within loose fibroconnective tissue and a few disorganized bundles of smooth muscle present in the wall of the larger channels. Immunohistochemical stains were positive for Factor VIII and actin. The same cells did not react to cytokeratin. These findings were consistent with a cystic lymphangioma (Figure 3). The patient had an uneventful postoperative course, and no evidence of recurrence, 18 mo after the operation.
Lymphangiomas are uncommon and occur mainly in children; approximately 80-90% are diagnosed within the first few years of life and adult cases are rare[1]. They are commonly found in the head, neck, and axillary region. However, isolated occurrence in the mesentery of the small intestine is encountered even less frequently, comprising less than 1% of all lymphangiomas[2]. The most common location of such intraperitoneal lymphatic tumor appears to be the mesentery of the small bowel, accounting for 70% of all such tumors[3,4].
The etiology of lymphangiomas is probably a congenital abnormality of the lymphatic system, causing sequestrations of lymphatic tissue during embryologic development[2]. This theory would explain why lymphangiomas occur primarily in children. However, it is suggested that abdominal trauma, lymphatic obstruction, inflammatory process, surgery, or radiation therapy may lead to the secondary formation of such a tumor[4,5]. Traditionally, lymphangiomas are classified as simple, cavernous, or cystic. The simple type is usually situated superficially in the skin and composed of small thin-walled lymphatic vessels. The cavernous type is composed of dilated lymphatic vessels and lymphoid stroma, and has a connection with spaces of various normal adjacent lymphatics. Lastly, the cystic type consists of lymphatic spaces of various sizes that contains fascicles of smooth muscle and collagen bundles, but has no connection with adjacent normal lymphatics. However, cystic lymphangioma is not always clearly differentiated from cavernous type because the cystic type may also contain cavernous areas[6]
Mesenteric lymphangiomas are usually asymptomatic until they enlarge. Abdominal pain and distention seem to be the most common symptoms, but the clinical presentation of mesenteric lymphangiomas varies[7]. Although benign in nature, mesenteric lymphangiomas may cause significant morbidity or mortality due to their large size and critical location, when they compress the adjacent structures. In addition, complications such as secondary infection, rupture with hemorrhage, volvulus, or intestinal obstruction have all been reported[8-11]. The ultrasonographic presentation of a mesenteric lymphangioma is described as a cystic lesion with multiple thin septa. On CT imaging, mesenteric lymphangiomas appear as a uni- or multilocular mass with enhancement of the wall and septum by contrast medium[12]. These studies help to determine, if the tumor is cystic as well as its size and location, but they are insufficient to establish an accurate diagnosis preoperatively. One report suggested that fine needle aspiration of a milky fluid containing lymphoid cells could confirm a preoperative diagnosis of lymphangioma[13].
Mesenteric lymphangiomas may behave in an aggressively invasive manner and grow to an enormous size. The optimal treatment is radical excision, even when asymptomatic. However, mesenteric lymphangiomas may cause complications such as infiltration of the intestine, or involvement of the main branch of mesenteric arteries or adjacent organs that necessitate segmental resection of the intestine. Sometimes radical resection might be technically impossible[14]. Mesenteric lymphangiomas are very rare, but they can cause acute abdomen that requires an emergent surgery. Therefore, they should be included in the differential diagnosis of acute abdomen.
Science Editor Guo SY Language Editor Elsevier HK
| 1. | Hanagiri T, Baba M, Shimabukuro T, Hashimoto M, Takemoto H, Inoue A, Sugitani A, Shirakusa T. Lymphangioma in the small intestine: report of a case and review of the Japanese literature. Surg Today. 1992;22:363-367. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 24] [Cited by in F6Publishing: 29] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 2. | Roisman I, Manny J, Fields S, Shiloni E. Intra-abdominal lymphangioma. Br J Surg. 1989;76:485-489. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 118] [Cited by in F6Publishing: 128] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 3. | Chin S, Kikuyama S, Hashimoto T, Tomita T, Hasegawa T, Ohno Y. Lymphangioma of the jejunal mesentery in an adult: a case report and a review of the Japanese literature. Keio J Med. 1993;42:41-43. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 15] [Cited by in F6Publishing: 14] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 4. | Hardin WJ, Hardy JD. Mesenteric cysts. Am J Surg. 1970;119:640-645. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 52] [Cited by in F6Publishing: 55] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 5. | Daniel S, Lazarevic B, Attia A. Lymphangioma of the mesentery of the jejunum: report of a case and a brief review of the literature. Am J Gastroenterol. 1983;78:726-729. [PubMed] [Cited in This Article: ] |
| 6. | Rieker RJ, Quentmeier A, Weiss C, Kretzschmar U, Amann K, Mechtersheimer G, Bläker H, Herwart OF. Cystic lymphangioma of the small-bowel mesentery: case report and a review of the literature. Pathol Oncol Res. 2000;6:146-148. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 41] [Cited by in F6Publishing: 50] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 7. | Bliss DP, Coffin CM, Bower RJ, Stockmann PT, Ternberg JL. Mesenteric cysts in children. Surgery. 1994;115:571-577. [PubMed] [Cited in This Article: ] |
| 8. | Ricca RJ. Infected mesenteric lymphangioma. N Y State J Med. 1991;91:359-361. [PubMed] [Cited in This Article: ] |
| 9. | Porras-Ramirez G, Hernandez-Herrera MH. Hemorrhage into mesenteric cyst following trauma as a cause of acute abdomen. J Pediatr Surg. 1991;26:847-848. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 10] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 10. | Yoon HK, Han BK. Chronic midgut volvulus with mesenteric lymphangioma: a case report. Pediatr Radiol. 1998;28:611. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 18] [Cited by in F6Publishing: 19] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 11. | Troum S, Solis MM. Mesenteric lymphangioma causing bowel obstruction in a child. South Med J. 1996;89:808-809. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 5] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 12. | Davidson AJ, Hartman DS. Lymphangioma of the retroperitoneum: CT and sonographic characteristic. Radiology. 1990;175:507-510. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 130] [Cited by in F6Publishing: 136] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 13. | Sadola E. Cystic lymphangioma of the jejunal mesentery in an adult. J Clin Ultrasound. 1987;15:542-543. [PubMed] [DOI] [Cited in This Article: ] |