Published online Jan 7, 2006. doi: 10.3748/wjg.v12.i1.82
Revised: June 28, 2005
Accepted: July 20, 2005
Published online: January 7, 2006
AIM: To compare two different daily doses of lansoprazole given for 12 weeks and to assess the role of gastrointestinal (GI) investigations as criteria for selecting patients.
METHODS: Out of 45 patients referred for unexplained chronic persistent cough, 36 had at least one of the GI investigations (endoscopy, 24-h esophageal pH-metry and a 4-week trial of proton pump inhibitor (PPI) therapy) positive and were randomly assigned to receive either 30 mg lansoprazole o.d. or 30 mg lansoprazole b.i.d. for 12 weeks. Symptoms were evaluated at baseline (visit 1) after the PPI test (visit 2) and after the 12-week lansoprazole treatment period (visit 3).
RESULTS: Thirty-five patients completed the study protocol. Twenty-one patients (60.0%) reported complete relief from their cough with no difference between the two treatment groups (58.8% and 61.1% had no cough in 30 mg lansoprazole and 60 mg lansoprazole groups, respectively). More than 80% of the patients who had complete relief from their cough at the end of the treatment showed a positive response to the PPI test.
CONCLUSION: Twelve weeks of lansoprazole treatment even at a standard daily dose, is effective in patients with chronic persistent cough. A positive response to an initial PPI test seems to be the best criterion for selecting patients who respond to therapy.
- Citation: Baldi F, Cappiello R, Cavoli C, Ghersi S, Torresan F, Roda E. Proton pump inhibitor treatment of patients with gastroesophageal reflux-related chronic cough: A comparison between two different daily doses of lansoprazole. World J Gastroenterol 2006; 12(1): 82-88
- URL: https://www.wjgnet.com/1007-9327/full/v12/i1/82.htm
- DOI: https://dx.doi.org/10.3748/wjg.v12.i1.82
There is increasing evidence that many otolaryngologic or pulmonary conditions, ranging from very mild symptoms such as hoarseness to very severe diseases such as cancer, may be caused by gastroesophageal reflux (GER)[1]. In particular, GER seems to account for a relevant proportion of patients with asthma, cough, and laryngitis. Chronic persistent cough is a very common and disabling complaint for which patients seek medical care. It has been shown that in non-smoking patients with a normal chest X-ray and not taking angiotensin-converting enzyme (ACE) inhibitors the four most common causes of cough are post-nasal drip syndrome (PNDS), asthma, GER and chronic bronchitis[2]. These four conditions may account for as many as 90% of the cases of chronic cough. Moreover, GER by itself has been found to be responsible for 10%-40% of them even in the absence of reflux symptoms[3]. For these reasons, antisecretory drugs have been proposed for the treatment of patients with chronic cough possibly due to GER. Most studies on this topic have been performed with proton pump inhibitors (PPIs) at higher daily doses and for generally longer periods than those usually employed for typical GER disease. These studies have shown better results in terms of symptom resolution and improvement of laryngeal signs for PPIs vs placebo, but the success rate has been relatively low and quite variable, ranging from 35% to 60%[4-6]. This variability in response may be due to the differences either in selection criteria or in treatment regimens. Since the poorest outcomes[4] have been obtained in the study in which PPIs were given at the highest daily dose and for the longest period, patient selection may be the critical factor.
Thus, published studies suggest that antireflux treatment of patients with GER-related respiratory symptoms, particularly chronic cough, must be carried out with profound and prolonged acid inhibition in order to achieve satisfactory results in about two-thirds of the cases. However, the optimal treatment regimen and the criteria for patient selection need to be better defined.
The aim of our study was to evaluate the relative efficacy of two different daily doses of lansoprazole given for 12 weeks to patients with chronic persistent cough that could be reasonably ascribed to GER, and to assess the role of gastrointestinal ( GI ) investigations ( endoscopy, 24-h esophageal pH-metry and a 4-week trial of empiric PPI treatment ) as criteria for selecting patients with chronic cough who could benefit from antireflux treatment.
The study protocol was approved by the Ethics Committee of the S. Orsola-Malpighi Hospital, Bologna, Italy and all participants gave their written informed consent. A pretrial analysis determined that 15 patients were required in each treatment to demonstrate equivalence between 30 and 60 mg/d lansoprazole treatment groups in terms of cough severity and frequency with 80% power at an alfa level of 0.05.
Patients aged 18-70 years with unexplained chronic persistent cough ( i.e. for at least 3 days per week for a minimum of 3 months ) were enrolled in the study over a period of 1 year (from June 2002 to June 2003). All patients were consecutively referred by otolaryngologists and pulmonologists after the exclusion of oropharyngeal or respiratory diseases potentially responsible for the cough (particularly asthma and PNDS) by means of a diagnostic evaluation which included medical history, physical examination, methacholine challenge test, chest X-ray and fiber-optic laryngoscopy. Patients were excluded if they were pregnant or breastfeeding; had systemic diseases, cardiac and pulmonary disorders, viral and bacterial or fungal infections, neoplasia or Zollinger–Ellison syndrome; or received previous treatment with drugs that interfered with their gastric acid secretion (H2-antagonists, PPIs) and chronic treatment with NSAIDs, phenytoin, warfarin, tricyclic antidepressants, reserpine, beta-agonists, anticholinergics, antihistamines, inhaled steroids, or ACE inhibitors. Patients with chronic alcohol or drug abuse were also excluded, as were smokers.
After an initial clinical evaluation aimed at assessing the presence of associated typical reflux symptoms (heartburn and regurgitation) and the severity of cough, all patients underwent a diagnostic work-up which included upper GI endoscopy, 24 h esophageal pH-metry and a trial of empiric PPI therapy (PPI test, 30 mg lansoprazole b.i.d. for 4 weeks). The investigations were always performed in the same sequence, i.e. in the order of endoscopy, pH-metry and the PPI test.
A patient was considered eligible for 12 wk of lansoprazole treatment if at least one of the GI investigations was positive.
The severity of cough was evaluated according to a visual analog scale (VAS) graded from 0 to 10 and to a four-level scoring system, regarding the previous week, calculated as follows:
● Overall frequency: 0 = absent, 1 = occasional (<3 d/wk), 2 = often (3-6 d/wk), 3 = every day
● Daily frequency: 0 = absent, 1 = 1 episode, 2 = 2-3 episodes, 3 = >3 episodes
● Severity: 0 = absent, 1 = mild (not interfering with daily activities), 2 = moderate (sometimes interfering with daily activities), 3 = severe (regularly interfering with daily activities and/or sleep).
Symptoms were evaluated at baseline (visit 1), after a 4-wk PPI trial (visit 2) and a 12-week lansoprazole treatment period (visit 3).
All patients underwent upper GI endoscopy performed by the same gastroenterologist. The presence of esophagitis was noted and graded according to the Savary-Miller classification: grade I = single erosive or exudative lesion, oval or linear, on only one longitudinal fold; grade II = non-circular multiple erosions or exudative lesions on more than one longitudinal fold with or without confluence; grade III = circular erosive or exudative lesions; grade IV = chronic lesions, ulcers, strictures, or short esophagus, isolated or associated with grade I-III lesions; grade V = Barrett’s epithelium, isolated or associated with grade I-III lesions[7]. Grades I-IV were considered diagnostic of erosive esophagitis and endoscopy was considered positive for the purpose of this study.
After an overnight fast, two glass electrodes previously calibrated with buffer solutions at pH 7.0 and 1.0, were assembled with the sensors 15 cm apart and introduced into the stomach by the nasopharyngeal route. The distal electrode was positioned 5 cm above the lower esophageal sphincter (LES) so that the proximal one was located distal to the upper esophageal sphincter (UES). The location of the LES was determined by a combination of pH step-up technique, manometry (always performed in patients with hiatus hernia; 8 cases) and visualization under fluoroscopy if needed. The probe was connected to a digital portable recording unit (pH-day, Menfis, Italy) with a sampling frequency of one signal every second. Patients were asked to maintain their usual lifestyle and diet. They were provided with a diary card to record timing of meals, duration of nocturnal rest, time of cough occurrence and type of symptoms. Moreover, they were instructed to push an event marker button on the recording unit at the time of occurrence of their major complaint (cough). The pH-metry was stopped after 23-24 h. After being extracted, the electrodes were calibrated again with buffer solutions at pH 7.0 and 1.0. GER was evaluated as acid exposure fraction time (percent of time with pH <4). For the purpose of this study, pH-metry was considered positive if the percentage of total time with pH <4 was >4.73%[8] at the distal recording site or >1.00% at the proximal site (these values exceeded the 95th percentile of those previously obtained in normal subjects in our laboratory). In patients with normal values at both recording sites, we calculated the symptom index (SI), i.e., the number of cough episodes associated with acid reflux (that was simultaneous with or occurring within 5 min before or after the reflux episode) divided by the total number of cough episodes multiplied by 100, together with the symptom sensitivity index (SSI), i.e., the number of cough episodes associated with acid reflux, divided by the total number of reflux episodes multiplied by 100. We considered the investigation positive, if the SI was >50% with a SSI >20%[9].
After endoscopy and 24-h pH -metry, all patients received a 4-week open-label course of 30 mg lansoprazole administered before breakfast and dinner. Before PPI trial (visit 1) was started and at the end of the treatment course (visit 2) the patients were interviewed regarding their main symptom, i.e., cough, and asked to rate symptom severity during the previous week on a VAS graded 0-10[10]. The test was considered positive, if the post-treatment value was 0 or if the difference between the pre- and post-treatment values was ≥5.
Patients with a positive finding in at least one of the three assessments (endoscopy, pH-metry and symptom relief during a 4-week PPI trial) were randomized to either 30 mg lansoprazole oral capsules in the morning and identical placebo capsules in the evening or 30 mg lansoprazole in the morning and 30 mg lansoprazole in the evening before meals for 12 wk. Active drug and placebo were both supplied by Takeda Italia Pharmaceuticals (Rome, Italy). Both patients and investigators were blinded to the treatment status. Patients were interviewed and VAS was assessed at the end of treatment, and pill counting was performed to check for compliance with treatment.
Symptomatic response was defined as complete (VAS and score values = 0), partial (VAS value ≥ 1 but ≤ 50% of the baseline value and score value <5) or absent.
Data were analyzed by the Student’s t test for independent data of continuous variables, by the Mann-Whitney’s non-parametric test for discrete variables and by the χ2 test for nominal variables reported as contingency tables[11]. The Wilcoxon’s rank-sum test or the Friedman test was used for the comparison of symptom scores. A two-sided significance level of 0.05 was chosen.
Equivalence between the two treatment regimens was determined using the Schuirman one-sided test procedure. Mean VAS values recorded at visit 3 (after 12 wk of double-blind therapy) in the reference group (60 mg/day lansoprazole) were transformed to 100, and then the same transformation equation was applied to the mean VAS values at visit 3 in the 30 mg/d lansoprazole group. Equivalence was demonstrated if the 90% confidence intervals (CIs) for the difference between the transformed mean VAS values in each group were within the standard deviation (± 20).
Forty-five patients (7 men, mean age 54.5 ± 11.1 years, age range 29-70 years) referred for unexplained chronic persistent cough underwent the GI investigations aimed at the detection of GER disease (Table 1). Most of the patients were middle-aged females and 25 (55.5%) also reported typical reflux symptoms (heartburn and/or regurgitation occurring at least once per week). Thirty-six (80%) patients were positive for at least one test. Only a few patients (n = 7, 15.5%) had endoscopy-proven esophagitis, while about 50% had pathological GER and a positive PPI test. Twenty-four patients (53.3%) were found to have pathological reflux, 12 at both recording sites, 10 at the distal site only and just 2 at the proximal site only. Two out of 21 patients with negative pH-metry were found to have a positive SI and considered as positive for pH-metry. Twenty-three patients had a positive PPI test, five of them reported complete disappearance of cough, while the remaining 18 had a reduction in cough symptoms of 76.8% ± 10.1%. There was no association between an abnormal result of any of the aforementioned tests and the presence or absence of associated GER symptoms. There was a lack of concordance between the results of pH-metry and those of the PPI test (Table 2). In fact, 12 patients were positive for both tests and 8 were negative for both tests (44.4%), while in the other 25 cases the tests provided opposite results.
| All patients | GERD symptoms | ||
| Present | Absent | ||
| Subjects | 45 | 25 | 20 |
| Age (mean±SD) | 54.5 ± 11.1 | 54.6 ± 12.8 | 54.4 ± 8.6 |
| Gender, male (%) | 7 (15.5) | 3 (12.0) | 4 (20.0) |
| Upper endoscopy positive (%) | 7 (15.5) | 3 (12.0) | 4 (20.0) |
| pH-metry positive (%) | 26 (57.8) | 13 (52.0) | 13 (65.0) |
| PPI test positive (%) | 23 (51.1) | 13 (52.0) | 10 (50.0) |
| 24 h pH-metry | Total | ||
| Positive | Negative | ||
| PPI test positive | 12 | 11 | 23 |
| PPI test negative | 14 | 8 | 22 |
| Total | 26 | 19 | |
Of the 36 patients who satisfied the criteria for admission to the 12-week lansoprazole treatment, 12 had positive PPI test and pH-metry, 11 had a positive PPI test only and 13 had positive pH-metry only. Esophagitis was not the only pathological finding in any of the patients. One of the patients did not continue the study due to unwillingness, while the remaining 35 completed the study protocol (17 on 30 mg/d lansoprazole and 18 on 60mg/d lansoprazole) and were considered for our efficacy analysis. There was no statistically significant difference between the two treatment groups with regard to age, gender, presence of esophagitis, or 24-h pH-metry and PPI trial outcome (Table 3).
| Lansoprazole (30 mg/d)(n = 17) | Lansoprazole (60 mg/d)(n = 18) | |
| Age (mean±SD) | 57.5 ± 11.9 | 52.4±10.0 |
| Gender, male (% ) | 3 (17.6) | 2 (11.1) |
| Upper endoscopy positive (%) | 4 (23.5) | 3 (16.7) |
| pH-metry positive (%) | 13 (76.5) | 10 (55.5) |
| PPI test positive (%) | 11 (64.7) | 11 (61.1) |
Patients’ symptoms as assessed with both the subjective (VAS) and the objective (score) system, improved significantly at the end of the 12-wk treatment period vs baseline in both treatment groups, with no statistically significant difference either between the two groups or between the values at visits 2 and 3 (Table 4). The 90%CIs of the difference in the transformed mean VAS scores at 12 wk were within the standard deviation, thereby demonstrating equivalence of the two regimens.
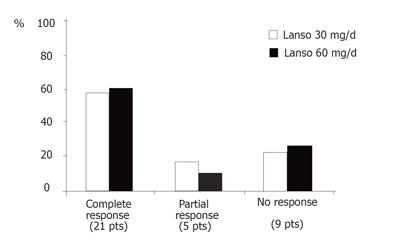
At the end of the 12-wk treatment period 21 patients (60.0%) reported complete relief of their cough with no difference between the two treatment groups (10/17 and 11/18 had no cough in the 30 mg/d lansoprazole and 60 mg/d lansoprazole groups, respectively, Figure 1). In patients selected for the 12-wk course of lansoprazole a PPI was actually taken for 16 wk (including the 4-wk PPI test). At the end of the PPI test, 10 (28.6%) of the 35 patients who continued to complete 12 wk of therapy showed complete relief of their cough. During the following course of PPI the percentage of symptom-free patients increased up to about 60% at the end of the 3-mo period, independently of the daily dose of the drug.
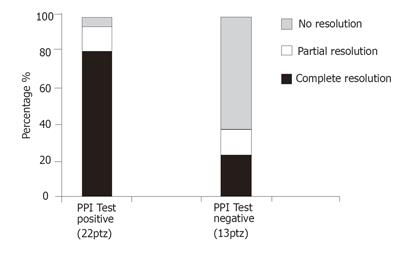
In order to determine the factors that may have influenced the treatment outcome, we compared the characteristics of patients who achieved complete relief of their symptoms with those who showed only partial relief or no symptomatic response (Table 5). As shown in the table, the positivity of the PPI test was significantly different between the two groups. In fact, more than 80% of patients who had complete relief of their cough at the end of treatment had a positive response to the PPI trial in comparison to only 28.6% of those who did not satisfactorily respond. None of the other factors, including the daily lansoprazole dose, was significantly correlated with the positive outcome of the treatment. Moreover, the rate of complete symptom relief at the end of the 12-wk course in patients classified as PPI test-positive was 81.8% in comparison to only 23.1% in those with a negative test (Figure 2).
| Responders [n = 21 (%)] | Non-responders [n = 14 (%)] | |
| GER symptoms | 14 (66.7) | 5(35.7) |
| Treatment with | 11 (52.4) | 7(50.0) |
| 60 mg/d lansoprazole | ||
| Erosive esophagitis | 5 (23.8) | 2(14.3) |
| pH-metry positive | 10 (47.6) | 13(92.8) |
| PPI test positive | 18 (85.7) | 4(28.6)b |
The correlation between respiratory or otolaryngologic symptoms and GER is usually ascertained in patients with unexplained chronic cough by the exclusion of other common causes such as asthma and PNDS, and the finding of pathognomonic signs such as posterior laryngitis, also called “reflux laryngitis”, as well as the demonstration of pathological reflux[4-6].
In our study, the pathogenetic role of reflux was suspected after the exclusion of common otolaryngologic or pneumological causes and after a careful work-up aimed at the detection of GER disease. The presence of posterior laryngitis was not included in our criteria because the sensitivity of this finding is generally thought to be low, while its specificity is ill-defined[12]. About 50% of our patients complained of typical reflux symptoms, such as heartburn and regurgitation, but this finding seemed to be of little relevance, since it was not correlated with the presence of esophagitis, pathological reflux or specifically, a positive response to the PPI trial (Table 1).
As expected, only a few patients had endoscopically proven esophagitis. This is in agreement with the previous observations in patients with so-called extra-esophageal manifestations of GER disease, showing that endoscopic evidence of esophagitis is found in 25%-40% of patients with asthma[13-14] and in only 10%-25% of patients with otolaryngologic disorders[6,15]. Therefore, upper GI endoscopy has a very low sensitivity in patients with atypical GER symptoms and, in the absence of other clinical indications, should not be included in the diagnostic work-up of these patients.
Ambulatory 24-h esophageal pH-metry is considered the gold standard for GER detection, with a high sensitivity in patients with typical symptoms[16]. Studies performed in patients with extra-esophageal symptoms showed that diagnostic sensitivity ranges 50%-80% in patients with asthma[17,18] and otolaryngologic manifestations, such as laryngitis or cough[4,6,19]. Moreover, the use of a double esophageal probe has been proposed in the latter patient group[19]. However, the usefulness of proximal pH-metry has been questioned since its sensitivity and reproducibility are too low[14,20]. Our results have confirmed the findings of others, showing that the diagnostic gain provided by dual-channel pH-metry is very low[4].
Since the presence of “physiological” reflux does not necessarily imply the absence of a casual link between reflux and symptoms, the diagnostic sensitivity of 24-h pH-metry may be improved by including the evaluation of a symptom/reflux correlation (SI), especially in patients with atypical symptoms, such as non-cardiac chest pain[21]. On the other hand, the SI has two major potential limitations: (1) it is feasible only in patients with symptoms during the recording period and this is not always the case (in our patient group 77.7% reported cough episodes during pH-metry), and (2) its value may be questioned if patients have only few symptomatic episodes during the recording period. For this reason, as suggested by previous studies[22], we considered a correlation between a given symptom and a reflux event to be present for SI values > 50% together with a SSI > 20%. We performed this evaluation as part of the analysis of our 24 h pH-metry tracings and found that 17 of the 21 patients with negative pH-metry reported cough during the recording period, with 2 of them showing a positive SI, thus increasing the diagnostic value of this investigation.
An empirical trial with PPIs (the so called “omeprazole or PPI test”) has been recently proposed for the diagnosis of GER disease in patients with various clinical presentations, especially those with atypical or extra-esophageal symptoms. The diagnostic sensitivity of this test is generally validated vs 24-h pH-metry as a gold standard. The variability of results reported thus far depends on the differences in treatment schedules (daily doses, duration) and the outcomes chosen (cut-off point for symptom improvement, VAS, questionnaires, etc.). Doses used in clinical studies range 40-80 mg of omeprazole or 60 mg of lansoprazole daily from 1 to 14 d in patients with symptoms suggestive of GER disease or non-cardiac chest pain[23-29] and from 7 to 90 d in patients with extra-esophageal manifestations[4,30,31]. In patients with laryngeal symptoms, in which a longer duration and a high daily dosage are considered necessary for obtaining a significant symptom improvement, the test is in general fairly sensitive, with values ranging 62.5%-81%[4,30,31]. Thus, our PPI test consisted of 4-week administration of 60 mg/d lansoprazole. According to a similar study[28] we used a VAS graded 0-10 to assess as objectively as possible the severity of symptoms perceived by our patients and we considered the PPI test positive if symptoms disappeared (grade 0) or were reduced by at least 50% in comparison to the pre-administration value. In our study the test was positive in 63.9% of patients with a sensitivity similar to that previously reported.
In our study there was a lack of concordance between the results of the 24 h esophageal pH-metry and those of the PPI test (Table 2). In fact there was agreement in only 20 patients (44.4%). It was reported that there is a significant direct correlation between pH-metry and response to the omeprazole test in patients with typical reflux symptoms (65.8% of patients with concordant results, P = 0.04)[23]. In contrast, a study[4] performed in patients with chronic cough showed concordance between the two tests in only half the cases (52.2%). This lack of concordance is not surprising and may depend on the intrinsic limitations of both pH-metry (i.e. absence of symptoms during the recording period in patients with “physiological” reflux) and the PPI test (inadequacy of treatment dose or duration). It may also depend on the simultaneous and independent existence of two conditions, GER and cough, not causally linked.
For all these reasons in our study, we proposed that at least one of the GI investigations (endoscopy, pH-metry, PPI test) had to be positive in order to select the cough patients in whom a 12-wk lansoprazole course could be reasonably proposed as a treatment choice.
The efficacy of PPI treatment in patients with extra-esophageal manifestations has been previously established[4-6]. Our study showed that both lansoprazole regimens significantly reduced symptom scores in comparison to baseline values (Table 4). There was a further reduction of the values recorded at visit 3 in comparison to those at visit 2, but the difference was not statistically significant. Moreover, it is interesting to note that there was a good concordance between the subjective (VAS) and objective (score) analysis, suggesting that they can be used interchangeably for symptom assessment. The success rate was also evaluated on an individual basis in terms of symptom resolution (Figure 1) which was graded on three levels according to the complete, partial or poor improvement of the symptoms. At the end of the 12-week treatment course about 60% of the patients reported complete relief of their cough (58.8% and 61.1% had no cough in the 30 mg/d lansoprazole and 60 mg/d lansoprazole groups, respectively). We did not find significant differences between the two treatment regimens but our study was only powered to show equivalence rather than efficacy. Studies performed in patients with chronic cough treated with PPIs have reported a complete relief of the symptom in a percentage of patients ranging 26%-43%[4,5] but the comparison among the studies is difficult because of different patient selection criteria and treatment regimens. A study that used the same drug and treatment duration as the present study[6] has reported a complete resolution of symptoms in 50% of patients with idiopathic laryngitis, which is very similar to our results.
In our study, the patients selected for the 12-wk course of PPI after the test period actually took lansoprazole for 16 weeks, and some of these patients experienced symptom relief at the end of the first 4 weeks, 10 of them showing complete resolution of their cough. This suggests that 1-month PPI administration at a double daily dose may be an effective therapy in about one-third of these cases. The percentage of symptom-free patients increased up to about 60% at the end of the 12-wk period, independently of the daily dose of the drug.
The analysis of factors that could have influenced the outcome (Table 5) clearly showed that the positivity of the PPI test was significantly different between complete and incomplete responders to PPI treatment. None of the other factors, particularly the presence of GER symptoms ,seemed to be associated with the positive outcome of treatment. This is in agreement with previous studies in patients with cough[4-6] and laryngitis[6]. Indeed, the response to an initial treatment with a PPI has been suggested as the best method for identifying patients with GER-related chronic cough[4]. Our results show that PPI test may predict response to a longer course of PPI treatment in patients with atypical reflux symptoms. The rate of complete symptom relief at the end of the 12-week course in our patients classified as PPI test-positive was 81.8% (the highest, to our knowledge, among those reported in similar studies) in comparison to only 23.1% of those with a negative test (Figure 2).
In conclusion, a 12-wk course of lansoprazole is effective in relieving symptoms of patients with unexplained chronic persistent cough. A positive response to an initial 4-wk administration of PPI at a double daily dose seems to be an effective criterion for selecting patients who obtain the best results from the PPI treatment.
S- Editor Wang XL and Guo SY L- Editor Elsevier HK E- Editor Wang J
| 1. | Richter JE. Extraesophageal presentations manifestations of gastroesophageal reflux disease. Semin Gastrointest Gastroenterol Dis. 1997;8:75-89. [Cited in This Article: ] |
| 2. | Irwin RS, Richter JE. Gastroesophageal reflux and chronic cough. Am J Gastroenterol. 2000;95:S9-14. [PubMed] [Cited in This Article: ] |
| 3. | Irwin RS, Curley FJ, French CL. Chronic cough. The spectrum and frequency of causes, key components of the diagnostic evaluation, and outcome of specific therapy. Am Rev Respir Dis. 1990;141:640-647. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 521] [Cited by in F6Publishing: 552] [Article Influence: 16.2] [Reference Citation Analysis (0)] |
| 4. | Ours TM, Kavuru MS, Schilz RJ, Richter JE. A prospective evaluation of esophageal testing and a double-blind, randomized study of omeprazole in a diagnostic and therapeutic algorithm for chronic cough. Am J Gastroenterol. 1999;94:3131-3138. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 172] [Cited by in F6Publishing: 185] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 5. | Kiljander TO, Salomaa ER, Hietanen EK, Terho EO. Chronic cough and gastro-oesophageal reflux: a double-blind placebo-controlled study with omeprazole. Eur Respir J. 2000;16:633-638. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 99] [Cited by in F6Publishing: 109] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 6. | El-Serag HB, Lee P, Buchner A, Inadomi JM, Gavin M, McCarthy DM. Lansoprazole treatment of patients with chronic idiopathic laryngitis: a placebo-controlled trial. Am J Gastroenterol. 2001;96:979-983. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 166] [Cited by in F6Publishing: 171] [Article Influence: 7.4] [Reference Citation Analysis (0)] |
| 7. | Armstrong D, Blum AL, Savary M. Reflux disease and Barrett's oesophagus. Endoscopy. 1992;24:9-17. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 15] [Cited by in F6Publishing: 15] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 8. | Baldi F, Ferrarini F, Longanesi A, Bersani G. Ambulatory 24-hour oesophageal pH monitoring in normal subjects: a multicentre study in Italy. G.I.S.M.A.D. GOR Study Group. Ital J Gastroenterol. 1991;23:477-480. [PubMed] [Cited in This Article: ] |
| 9. | Singh S, Richter JE, Bradley LA, Haile JM. The symptom index. Differential usefulness in suspected acid-related complaints of heartburn and chest pain. Dig Dis Sci. 1993;38:1402-1408. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 85] [Cited by in F6Publishing: 78] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 10. | Nyrén O, Adami HO, Bates S, Bergström R, Gustavsson S, Lööf L, Sjödén PO. Self-rating of pain in nonulcer dyspepsia. A methodological study comparing a new fixed-point scale and the visual analogue scale. J Clin Gastroenterol. 1987;9:408-414. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 15] [Cited by in F6Publishing: 14] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 11. | Armitage P, Berry G, Matthews JNS. Statistical Methods in Medical Research. 4rd Edition. Oxford: Blackwell Scientific Publications 2002; . [Cited in This Article: ] |
| 12. | Young JL, Shaw GY, Searl JP, Miner PB. Laryngeal manifestations of gastroesophageal reflux disease: endoscopic appearance and management. Gastrointest Endosc. 1996;43:225-230. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 21] [Cited by in F6Publishing: 20] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 13. | Larrain A, Carrasco E, Galleguillos F, Sepulveda R, Pope CE. Medical and surgical treatment of nonallergic asthma associated with gastroesophageal reflux. Chest. 1991;99:1330-1335. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 177] [Cited by in F6Publishing: 178] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 14. | Sontag SJ, Schnell TG, Miller TQ, Khandelwal S, O'Connell S, Chejfec G, Greenlee H, Seidel UJ, Brand L. Prevalence of oesophagitis in asthmatics. Gut. 1992;33:872-876. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 123] [Cited by in F6Publishing: 129] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 15. | Richter JE, Hicks DM. Unresolved issues in gastroesophageal reflux-related ear, nose, and throat problems. Am J Gastroenterol. 1997;92:2143-2144. [PubMed] [Cited in This Article: ] |
| 16. | Jamieson JR, Stein HJ, DeMeester TR, Bonavina L, Schwizer W, Hinder RA, Albertucci M. Ambulatory 24-h esophageal pH monitoring: normal values, optimal thresholds, specificity, sensitivity, and reproducibility. Am J Gastroenterol. 1992;87:1102-1111. [PubMed] [Cited in This Article: ] |
| 17. | Sontag SJ, O'Connell S, Khandelwal S, Miller T, Nemchausky B, Schnell TG, Serlovsky R. Most asthmatics have gastroesophageal reflux with or without bronchodilator therapy. Gastroenterology. 1990;99:613-620. [PubMed] [Cited in This Article: ] |
| 18. | Schnatz PF, Castell JA, Castell DO. Pulmonary symptoms associated with gastroesophageal reflux: use of ambulatory pH monitoring to diagnose and to direct therapy. Am J Gastroenterol. 1996;91:1715-1718. [PubMed] [Cited in This Article: ] |
| 19. | Koufman JA. The otolaryngologic manifestations of gastroesophageal reflux disease (GERD): a clinical investigation of 225 patients using ambulatory 24-hour pH monitoring and an experimental investigation of the role of acid and pepsin in the development of laryngeal injury. Laryngoscope. 1991;101:1-78. [PubMed] [Cited in This Article: ] |
| 20. | Vaezi MF, Richter JE. Twenty-four-hour ambulatory esophageal pH monitoring in the diagnosis of acid reflux-related chronic cough. South Med J. 1997;90:305-311. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 45] [Cited by in F6Publishing: 50] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 21. | Hewson EG, Sinclair JW, Dalton CB, Richter JE. Twenty-four-hour esophageal pH monitoring: the most useful test for evaluating noncardiac chest pain. Am J Med. 1991;90:576-583. [PubMed] [Cited in This Article: ] |
| 22. | Breumelhof R, Smout AJ. The symptom sensitivity index: a valuable additional parameter in 24-hour esophageal pH recording. Am J Gastroenterol. 1991;86:160-164. [PubMed] [Cited in This Article: ] |
| 23. | Schenk BE, Kuipers EJ, Klinkenberg-Knol EC, Festen HP, Jansen EH, Tuynman HA, Schrijver M, Dieleman LA, Meuwissen SG. Omeprazole as a diagnostic tool in gastroesophageal reflux disease. Am J Gastroenterol. 1997;92:1997-2000. [PubMed] [Cited in This Article: ] |
| 24. | Fass R, Fennerty MB, Ofman JJ, Gralnek IM, Johnson C, Camargo E, Sampliner RE. The clinical and economic value of a short course of omeprazole in patients with noncardiac chest pain. Gastroenterology. 1998;115:42-49. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 287] [Cited by in F6Publishing: 241] [Article Influence: 9.3] [Reference Citation Analysis (0)] |
| 25. | Johnsson F, Weywadt L, Solhaug JH, Hernqvist H, Bengtsson L. One-week omeprazole treatment in the diagnosis of gastro-oesophageal reflux disease. Scand J Gastroenterol. 1998;33:15-20. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 101] [Cited by in F6Publishing: 101] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 26. | Fass R, Ofman JJ, Sampliner RE, Camargo L, Wendel C, Fennerty MB. The omeprazole test is as sensitive as 24-h oesophageal pH monitoring in diagnosing gastro-oesophageal reflux disease in symptomatic patients with erosive oesophagitis. Aliment Pharmacol Ther. 2000;14:389-396. [PubMed] [Cited in This Article: ] |
| 27. | Cremonini F, Wise J, Moayyedi P, Talley NJ. Diagnostic and therapeutic use of proton pump inhibitors in non-cardiac chest pain: a metaanalysis. Am J Gastroenterol. 2005;100:1226-1232. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 116] [Cited by in F6Publishing: 108] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 28. | Juul-Hansen P, Rydning A, Jacobsen CD, Hansen T. High-dose proton-pump inhibitors as a diagnostic test of gastro-oesophageal reflux disease in endoscopic-negative patients. Scand J Gastroenterol. 2001;36:806-810. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 38] [Cited by in F6Publishing: 39] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 29. | Pandak WM, Arezo S, Everett S, Jesse R, DeCosta G, Crofts T, Gennings C, Siuta M, Zfass A. Short course of omeprazole: a better first diagnostic approach to noncardiac chest pain than endoscopy, manometry, or 24-hour esophageal pH monitoring. J Clin Gastroenterol. 2002;35:307-314. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 76] [Cited by in F6Publishing: 67] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 30. | Metz DC, Childs ML, Ruiz C, Weinstein GS. Pilot study of the oral omeprazole test for reflux laryngitis. Otolaryngol Head Neck Surg. 1997;116:41-46. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 55] [Cited by in F6Publishing: 57] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 31. | Jaspersen D, Diehl KL, Geyer P, Martens E. [Diagnostic omeprazole test in suspected reflux-associated chronic cough]. Pneumologie. 1999;53:438-441. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 7] [Article Influence: 0.3] [Reference Citation Analysis (0)] |