Published online Oct 14, 2012. doi: 10.3748/wjg.v18.i38.5476
Revised: June 20, 2012
Accepted: August 14, 2012
Published online: October 14, 2012
Despite its abundant vascularization and extensive circulatory communication with neighboring organs, metastases to the penis are a rare event. A 57-year-old male, who had undergone total pelvic exenteration for rectal cancer sixteen months earlier, demonstrated an abnormal uptake within his penis by positron emission tomography/computed tomography. A single elastic nodule of the middle penis shaft was noted deep within Bucks fascia. No other obvious recurrent site was noted except the penile lesion. Total penectomy was performed as a curative resection based on a diagnosis of isolated penile metastasis from rectal cancer. A histopathological examination revealed an increase of well differentiated adenocarcinoma in the corpus spongiosum consistent with his primary rectal tumor. The immunohistochemistry of the tumor cells demonstrated positive staining for cytokeratin 20 and negative staining for cytokeratin 7, which strongly supported a diagnosis of penile metastasis from the rectum. The patient is alive more than two years without any recurrence.
- Citation: Kimura Y, Shida D, Nasu K, Matsunaga H, Warabi M, Inoue S. Metachronous penile metastasis from rectal cancer after total pelvic exenteration. World J Gastroenterol 2012; 18(38): 5476-5478
- URL: https://www.wjgnet.com/1007-9327/full/v18/i38/5476.htm
- DOI: https://dx.doi.org/10.3748/wjg.v18.i38.5476
The penis is an uncommon site of metastasis, and only around 300 such cases have been reported in the English-language literature[1,2]. A comprehensive review of the 305 reported cases showed the most frequent primary sites of metastatic penile tumors to be the bladder (34.7%), prostate (29.8%), rectum and sigmoid colon (15.7%), and kidney (6.5%)[1]. Approximately 50 cases of penile metastasis from either rectal or sigmoid colon cancer have been reported[1-3]. Ketata et al[4] reported the 20th case of penile metastasis from rectal cancer in 2007, and thereafter five other cases have been reported[5-9]. One-third of all penile metastases are synchronous, whereas the remaining two-thirds are detected a mean of 18 mo after discovery of the primary tumor[7]. About 90% of reported cases of penile metastasis are a part of widespread disease[2], thus isolated metastatic penile carcinomas are exceptionally rare. This report presents a case of metachronous isolated penile metastasis from rectal cancer after total pelvic exenteration, which was treated with a curative penile resection.
A 57-year-old male had a large rectal cancer which occupied the pelvis minor with massive invasion to both the bladder and prostate. He underwent sigmoid colostomy twenty three months previously. Nine courses of chemotherapy [oxaliplatin 100 mg intravenous (iv) on day 1, levofolinate 125 mg iv on day 1, 5-fluorouracil (5-FU) 500 mg iv bolus on day 1 and 5-FU 750 mg iv continuous infusion on days 1 and 2] had been administered after the first operation and the tumor slightly decreased in size without showing any distant metastasis. The patient underwent total pelvic exenteration, ileal conduit and pelvic reconstruction with a gracilis muscular flap sixteen months ago. There was no clinical or radiological evidence of distant metastasis at the time of resection. The histopathological examination revealed a moderately differentiated adenocarcinoma of the rectum invading to the bladder and prostate without lymph node metastasis (none out of 57). The disease was staged as T4 N0 M0 stage II (Dukes Classification B). He made an uneventful recovery and was discharged on the nineteenth postoperative day.
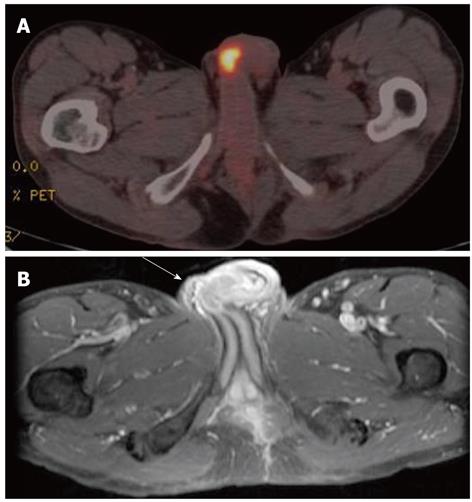
No clinical or radiological evidence of recurrence was observed for nine months after total pelvic exenteration until he started complaining of intermittent bloody discharge from his penis. Positron emission tomography/computed tomography (PET/CT) showed high 18-F fluorodeoxyglucose uptake in the penis (Figure 1A). A physical examination at that time showed a single 4 cm elastic nodule of the penis shaft in the middle, deep within Bucks fascia, which had slight tenderness. Penile magnetic resonance imaging (MRI) showed a low intensity lesion on a gadolinium-enhanced fat-suppressed T1-weighted image (Figure 1B). Contrast enhanced computed tomography (CECT) revealed neither other distant metastases nor local recurrence, and the serum tumor marker carcinoembryonic antigen was within normal limits.
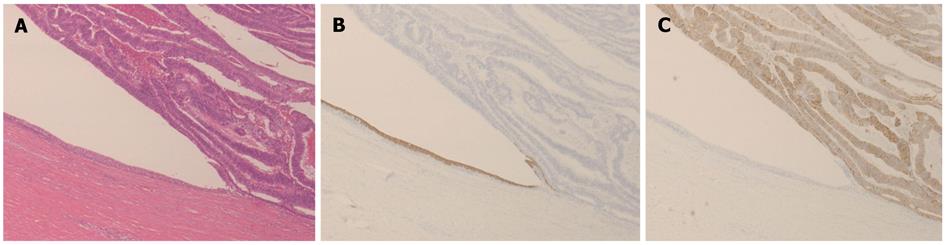
The patient underwent total penectomy based on the diagnosis of penile metastasis from rectal cancer with the resection of all the residual urethra, as a curative resection. The tumor was localized in the corpus spongiosum, and had almost completely replaced it (Figure 2). A histopathological examination of the resected specimen revealed an increase of well differentiated adenocarcinoma in the corpus spongiosum, consistent with his primary rectal tumor. Immunohistochemistry of tumor cells demonstrated positive staining for cytokeratin 20 and negative staining for cytokeratin 7 (Figure 3), which supported the diagnosis because the majority of rectal cancer does not stain for cytokeratin 7, but instead does stain for cytokeratin 20, and also because urothelial cells commonly shows positive staining for cytokeratin 7[4]. He underwent adjuvant chemotherapy, and now is good in health for more than two years since the last surgery with no recurrence.
A metastatic penile tumor is rare despite the rich vascularity and the end arterial nature of its supply. Various mechanisms of penile metastasis have been suggested; retrograde venous spread, retrograde lymphatic spread, arterial spread, implantation and secondary to instrumentation or direct extension[1]. Among these mechanisms, retrograde venous spread from the pudendal venous system into the dorsal venous system of the penis appears to be the most common mode of spread[7]. Retrograde lymphatic spread into penile lymphatic channels after obstruction of inguinal and hypogastric nodes, is also considered[2]. One or both corpora cavernosa is the most common site of penile metastasis, and the glans penis and corpus spongiosum are rarely involved[1,10]. However, the current tumor was localized not in the corpora cavernosa but in the corpus spongiosum without widely disseminated disease, which seems to be extremely rare. These findings suggest that cancer cells in the residual urine at the time of total pelvic exenteration had likely become implanted in the corpus spongiosum.
Penile metastasis tends to show a poor prognosis because metastasis to the penis, in most cases, tends to be part of widely disseminated disease. The majority of patients die within one year[5]. Therefore, many treatment algorithms against penile metastases are described. The treatment is essentially palliative, and the combination of radiotherapy with chemotherapy produces only occasional responses. Some cases are treated by penectomy, an aggressive surgical excision, in order to palliate such symptoms as priapism and pain. Penectomy can offer the possibility of cure in patients with disease localized to the penis, like the current patient, even though such cases may be rare.
In conclusion, this report described a case of penile metastasis from rectal cancer. The patient underwent a complete cure resection with subsequent adjuvant chemotherapy, rather than palliative treatment. Penile involvement is usually a marker of widespread hematogenous dissemination which indicates a poor prognosis, but such a prognosis does not seem applicable in the current case.
Peer reviewers: Nadia Peparini, MD, PhD, Department of General Surgery “Francesco Durante”, La Sapienza University, Viale del Policlinico,155, 00161 Rome, Italy; Joerg Trojan, MD, Professor, Medical Department 1, Johann Wolfgang Goethe-University Medical Center, Theodor-Stern-Kai 7, D-60590 Frankfurt, Germany
S- Editor Shi ZF L- Editor A E- Editor Zhang DN
| 1. | Hizli F, Berkmen F. Penile metastasis from other malignancies. A study of ten cases and review of the literature. Urol Int. 2006;76:118-121. [PubMed] [Cited in This Article: ] |
| 2. | Cherian J, Rajan S, Thwaini A, Elmasry Y, Shah T, Puri R. Secondary penile tumours revisited. Int Semin Surg Oncol. 2006;3:33. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 68] [Cited by in F6Publishing: 84] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 3. | Appu S, Lawrentschuk N, Russell JM, Bright NF. Metachronous metastasis to the penis from carcinoma of the rectum. Int J Urol. 2006;13:659-661. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 14] [Cited by in F6Publishing: 19] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 4. | Ketata S, Boulaire JL, Soulimane B, Bargain A. Metachronous metastasis to the penis from a rectal adenocarcinoma. Clin Colorectal Cancer. 2007;6:657-659. [PubMed] [Cited in This Article: ] |
| 5. | Murhekar KM, Majhi U, Mahajan V, Satheesan B. Penile metastasis from rectal carcinoma. Indian J Cancer. 2007;44:155-156. [PubMed] [Cited in This Article: ] |
| 6. | Chung TS, Chang HJ, Kim DY, Jung KH, Lim SB, Choi HS, Jeong SY. Synchronous penile metastasis from a rectal carcinoma. Int J Colorectal Dis. 2008;23:333-334. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 7. | Park JC, Lee WH, Kang MK, Park SY. Priapism secondary to penile metastasis of rectal cancer. World J Gastroenterol. 2009;15:4209-4211. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 20] [Cited by in F6Publishing: 25] [Article Influence: 1.7] [Reference Citation Analysis (1)] |
| 8. | Chaux A, Amin M, Cubilla AL, Young RH. Metastatic tumors to the penis: a report of 17 cases and review of the literature. Int J Surg Pathol. 2011;19:597-606. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 73] [Cited by in F6Publishing: 85] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 9. | Maestro MA, Martínez-Piñeiro L, Moreno SS, Rodríguez JD, Quevedo AL. Penile metastasis of rectal carcinoma. Case report and bibliographic review. Arch Esp Urol. 2011;64:981-984. [PubMed] [Cited in This Article: ] |
| 10. | Dubocq FM, Tefilli MV, Grignon DJ, Pontes JE, Dhabuwala CB. High flow malignant priapism with isolated metastasis to the corpora cavernosa. Urology. 1998;51:324-326. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 31] [Cited by in F6Publishing: 39] [Article Influence: 1.5] [Reference Citation Analysis (0)] |