Published online Jul 7, 2014. doi: 10.3748/wjg.v20.i25.8317
Revised: February 25, 2014
Accepted: April 5, 2014
Published online: July 7, 2014
Although acute appendicitis is a common disease, retroperitoneal abscesses are rarely observed. Here, we report a case consisting of a psoas abscess and cutaneous fistula caused by appendicitis. The patient was a 56-year-old male who was introduced to our institution due to an intractable right psoas abscess. Imaging tests had been performed over the previous 3 years; however, clinicians could not find the origin of the abscess and failed to resolve the problem. A successful operation was performed via a laparoscopic approach, and 17 mo have passed without recurrence. The advantage of laparoscopic surgery is well understood in cases of appendicitis with abscesses. However, the indication for laparoscopic approach is not clear for retroperitoneal abscesses. From our experience, we can conclude that appendicitis with retroperitoneal abscesses can be managed and treated using a laparoscopic approach.
Core tip: A psoas abscess caused from appendicitis is sometimes observed, and it has a high mortality rate because of the difficulty in diagnosing the origin of the abscess preoperatively. In our case, the patient had been previously treated for 3 years; however, the clinicians could not find the origin of the abscess and failed to resolve the problem. We successfully treated the patient using a laparoscopic approach. Only a small number of similar cases have treated patients using a laparoscopic method. We believe that this method helps diagnose the origin of the abscess and successfully treat complicated cases.
- Citation: Otowa Y, Sumi Y, Kanaji S, Kanemitsu K, Yamashita K, Imanishi T, Nakamura T, Suzuki S, Tanaka K, Kakeji Y. Appendicitis with psoas abscess successfully treated by laparoscopic surgery. World J Gastroenterol 2014; 20(25): 8317-8319
- URL: https://www.wjgnet.com/1007-9327/full/v20/i25/8317.htm
- DOI: https://dx.doi.org/10.3748/wjg.v20.i25.8317
Acute appendicitis is one of the most common causes of abdominal pain. Computed tomography (CT) and ultrasonography (US) are often used to support a clinical diagnosis. Sensitivity and specificity of preoperative evaluations of CT and US are 96.4 %, 95.4 % and 99.1 %, 96.5 %, respectively[1]. Psoas abscesses due to acute appendicitis are occasionally observed (14.6 %)[2]. CT and magnetic resonance imaging (MRI) scans can provide an excellent diagnosis of retroperitoneal abscess for the majority of cases[3,4]. However, the presenting symptoms of a retroperitoneal abscess can be nonspecific, making it difficult to provide an accurate diagnosis preoperatively[2]. The mortality rate in cases of a secondary psoas abscess, such as in acute appendicitis, remains high (19 %)[4]. To prevent this fatal outcome, detection of disease symptoms, accurate diagnosis and prompt treatment are required.
A 56-year-old male was sent to our institution due to an intractable right psoas abscess. The patient had right hip pain for 3 years prior to his visit and was diagnosed with a right psoas abscess by an orthopedist. Abscess drainage was preformed two times followed by a psoas curettage. The bacteria culture revealed Streptococcus sp (species), Escherichia coli, Bacteroides sp, Enterococcus avium, Clostridium ramosum, Enterobacter cloacae, Peptostreptococcus prevotii infections. CT and MRI were performed; however, no signs of appendicitis were confirmed.
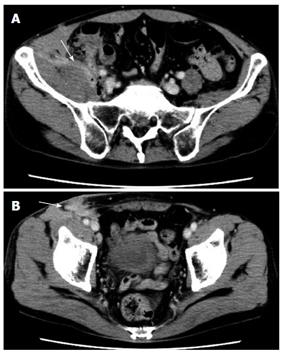
Laboratory tests were within normal limits when the patient visited our institution. There was no abdominal pain, but a discharge of pus was observed in the right inguinal region. An abdominal contrast CT showed a psoas abscess, a swollen appendix near the psoas muscle and a cutaneous fistula in the right inguinal region (Figure 1). We failed to image the cutaneous fistula from the appendicitis; however, a leakage of air was heard. The diagnosis of a psoas abscess and cutaneous fistula caused by appendicitis was made, and an elective laparoscopic surgery was scheduled. The patient was given sulbactum sodium/ampicillin sodium (SBT/ABPC) 12000 mg/d intravenously until the operation and was in stable condition during this time.
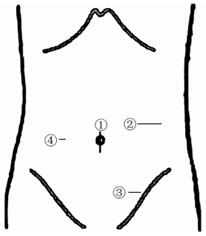
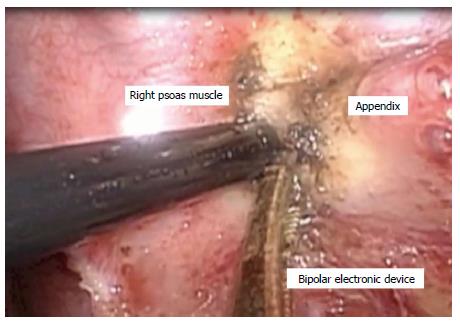
Under general anesthesia, the patient was placed in a supine position. The surgeon stood on the left side of the patient, and a video monitor was set up on the right side of the patient. A 12-mm blunt trocar was inserted into the umbilicus, two working trocars were placed in left abdomen, including a 12-mm trocar and 5-mm trocar, and 1 puncture was made in the right abdomen (Figure 2). We confirmed that the blind end of the appendix was strongly adhered into the right psoas muscle. We used a bipolar electronic device to completely decorticate the adhesion (Figure 3), and no pus was observed. An ileocecal resection was performed because the oral side of the appendix was damaged by inflammation. Indigo carmine was injected in the cutaneous fistula. No leakage was observed from the abscess wall, and an 8 Fr. drainage tube was inserted into the cutaneous fistula. SBT/ABPC was given continuously after the operation. The antibiotics were changed to the oral intake of amoxicillin (AMPC) 1500 mg/d and potassium clavulanate 325 mg/d for a total of 4 wk after the operation because the postoperative course was uneventful. The patient was discharged on the 18th postoperative day. At the time of manuscript submission, a total of 17 mo have passed without recurrence.
We sought to determine whether we can treat retroperitoneal abscess with a laparoscopic approach. To answer the question, we conducted a Pubmed search of the English language literature from 1955 to 2012 using the key words “appendicitis”, “retroperitoneal abscess”, and “psoas abscess”. A total of 27 cases were reported. In most cases, an open appendectomy with drainage was performed. Only 1 case consisted of a laparoscopic surgery. From these results, we suggest that an indication of laparoscopic surgery for appendicitis with retroperitoneal abscess is not clear. In the single case in which a laparoscopic operation was performed, a left retroperitoneal abscess was observed from the preoperative CT, and the laparoscopic examination revealed a focal perforation and pus at the tip of the appendix. A laparoscopic appendectomy and biopsy of the retroperitoneal abscess were performed. There was no discussion on the indication of how to treat retroperitoneal abscess[5]. In our case, we were able to perform a laparoscopic ileocecal resection regardless of the severe adhesion due to the chronic symptoms and psoas abscess. The postoperative course was uneventful, no surgical site infection was observed, and the right cutaneous fistula was alleviated without further invasive treatment.
Many studies have reported that there are no differences in the surgical outcomes of a laparoscopic appendectomy and an open appendectomy. Laparoscopic patients have better outcomes of less abdominal pain, less wound infection and a shorter hospital stay[6,7]. A laparoscopic approach is a feasible method to treat even complicated cases, such as appendiceal perforation and abscesses. The benefits of laparoscopic surgery do not differ between complicated and uncomplicated cases and do not increase the risk of postoperative complications[7,8].
To treat appendicitis with a retroperitoneal abscess, the most import considerations are managing the infection source and adequately draining the retroperitoneal abscess. A laparoscopic approach provides a magnified view that enables detection of the infection source and helps determine the resection area. From our experience in this case, a laparoscopic approach can manage the infection source even with the presence of a retroperitoneal abscess.
We conclude that the laparoscopic approach is less invasive and can manage appendicitis with retroperitoneal abscesses.
A 56-year-old male with a history of right leg pain had been previously treated for 3 years.
A pus discharge was observed in the right inguinal region.
Psoas abscess, appendicitis, tuberculosis.
Values were WBC 4.6 K/uL, HGB 15.2 gm/dL and CRP 0.65 mg/dL. Other laboratory tests were within normal limits when the patient visited our institution.
Abdominal contrast computed tomography showed a psoas abscess, a swollen appendix near the psoas muscle and a cutaneous fistula in the right inguinal region.
The patient underwent elective laparoscopic ileocecal resection.
There are no uncommon terms used in this manuscript.
A laparoscopic approach decreases postoperative pain and also aids in the detection of the cause of the retroperitoneal abscess.
This article demonstrates that a laparoscopic approach is less invasive and can manage appendicitis with a retroperitoneal abscess.
P- Reviewer: Sartelli M S- Editor: Wen LL L- Editor: A E- Editor: Liu XM
| 1. | Park JS, Jeong JH, Lee JI, Lee JH, Park JK, Moon HJ. Accuracies of diagnostic methods for acute appendicitis. Am Surg. 2013;79:101-106. [PubMed] [Cited in This Article: ] |
| 2. | Ricci MA, Rose FB, Meyer KK. Pyogenic psoas abscess: worldwide variations in etiology. World J Surg. 1986;10:834-843. [PubMed] [Cited in This Article: ] |
| 3. | Navarro López V, Ramos JM, Meseguer V, Pérez Arellano JL, Serrano R, García Ordóñez MA, Peralta G, Boix V, Pardo J, Conde A. Microbiology and outcome of iliopsoas abscess in 124 patients. Medicine (Baltimore). 2009;88:120-130. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 98] [Cited by in F6Publishing: 108] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 4. | Mallick IH, Thoufeeq MH, Rajendran TP. Iliopsoas abscesses. Postgrad Med J. 2004;80:459-462. [PubMed] [Cited in This Article: ] |
| 5. | Lu Y, Fox J, Dunphy M. Coincidental presentations of ganglioneuroma and atypical perforated appendicitis detected by fluorodeoxyglucose positron emission tomography/computed tomography. Clin Nucl Med. 2009;34:719-721. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 11] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 6. | Sporn E, Petroski GF, Mancini GJ, Astudillo JA, Miedema BW, Thaler K. Laparoscopic appendectomy--is it worth the cost? Trend analysis in the US from 2000 to 2005. J Am Coll Surg. 2009;208:179-185.e2. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 86] [Cited by in F6Publishing: 91] [Article Influence: 6.1] [Reference Citation Analysis (0)] |
| 7. | Brügger L, Rosella L, Candinas D, Güller U. Improving outcomes after laparoscopic appendectomy: a population-based, 12-year trend analysis of 7446 patients. Ann Surg. 2011;253:309-313. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 26] [Cited by in F6Publishing: 28] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 8. | Dimitriou I, Reckmann B, Nephuth O, Betzler M. Single institution’s experience in laparoscopic appendectomy as a suitable therapy for complicated appendicitis. Langenbecks Arch Surg. 2013;398:147-152. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 16] [Cited by in F6Publishing: 17] [Article Influence: 1.4] [Reference Citation Analysis (0)] |