Development of a self-treatment approach for patients with COPD and comorbidities: an ongoing learning process
Introduction
COPD is a leading cause of death and disability internationally (1) that affects approximately 1:10 adults in the developed world and is increasing in prevalence globally (2). High financial and social burdens have been associated with COPD in general (3,4) and COPD exacerbations in particular (5,6). COPD exacerbations, defined by episodes of acute deterioration in respiratory health (7), are also a major contributor to a step-wise worsening of quality of life in patients (7).
The latest Cochrane systematic review of COPD self-management (SM) has documented that COPD-specific SM interventions are associated with a reduction in hospital admissions (8). Patient-initiated action plans are an important component of SM interventions (8,9). When used appropriately, they can lead to accelerated initiation of appropriate treatment (10) and therefore reduce the exacerbation severity (11). When integrated into SM interventions, these action plans have proven to effectively reduce exacerbation severity, hospitalisations, and costs and improve health status (11-13).
Comorbidities are the rule rather than the exception in COPD (14,15). Over two-thirds of COPD patients (68.4%) suffer from at least one comorbidity, about 16% have at least two comorbid conditions (15), and one third of the COPD patients admitted to hospital have at least four coded comorbidities (16-18).
Because the symptoms of COPD and common co-occurring diseases overlap, a “one size fits all” approach that focuses solely on traditional symptoms of COPD is inadequate. For example, increased dyspnoea could relate to either a COPD exacerbation or a sudden deterioration of cardiovascular disease (e.g., heart failure) (19,20). Reliance on specifically designed for COPD symptoms and actions/treatments could therefore lead to the initiation of incorrect or delayed treatment.
The latter is highlighted by a recent study evaluating COPD-specific action plans in a COPD population with comorbidities (21). The study was terminated because of significantly higher mortality rates in the intervention group. No definite reason for this has emerged and the findings contrast positive outcomes of a comparable SM study (22). Nevertheless, the study (21) has resulted in controversy regarding the effectiveness of SM interventions, especially in patients with high burden of disease and co-morbidities (23). In these patients, SM interventions may be more challenging and not without risk of serious adverse events (23). It underlines the need for further evaluation of action plans in COPD patients with comorbidities.
In this paper we provide an insight into how we have used our experiences with our previous SM studies to develop a novel COPD self-treatment (ST) approach for patients with COPD and co-morbidities.
The COPE studies
During the last 15 years we have performed three large randomized controlled trials to explore effects of SM: the COPE-I (24), COPE-II (11,25), and COPE-III study (26). COPE stands for ‘COPD study at Department of Pulmonology Enschede. Whereas the COPE-I and COPE-II study were performed in the Netherlands, COPE-III is a joint Dutch - Australian research project. Experiences from COPE-I and COPE-II have been used to develop the design for the COPE-III study. Details of all three COPE studies have been summarized in Table 1.
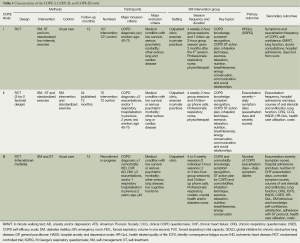
Full table
COPE-I
In the COPE-I study the effects of a comprehensive SM interventions were evaluated in 248 patients with moderate to severe COPD and no severe comorbidities (24). The intervention involved an individualized treatment plan that incorporated smoking cessation, optimisation of pulmonary status by pharmacotherapy, a standardised low-intensity exercise program, and a written ST action plan for COPD exacerbations that was based on symptom perception. If patients experienced an increase of respiratory symptoms and normally would have called their physician, they could start with a short course of oral prednisolone, and with onset of purulent sputum a course of antibiotics for which prescriptions were supplied (24). The study results showed no effects on quality of life and exercise capacity, and an increased number of exacerbations, defined as an increase of respiratory symptoms treated with prednisolone and/or antibiotics in the intervention group. However, because daily symptoms were not recorded in either study groups, it could not be clarified whether this meant that there was an over-treatment in the intervention group or an under-treatment in the control group (24).
COPE-II
In the COPE-II study (11), the extra value of a COPD SM component was evaluated. A group of patients who received a SM intervention that included specific training in ST (intervention group; n=70) was compared to a group of patients who received a similar SM intervention without this specific training (control group; n=72). The ST training component incorporated training in COPD symptom recognition (with the help of a daily symptom diary) and use of an action plan. The concerns from the COPE-I study regarding over-treatment in the intervention group were taken into consideration and the start of a COPD exacerbation was defined as ‘a clear negative change in two major symptoms or one major and one minor symptom from baseline, for at least two consecutive days’ [major symptoms: breathlessness, sputum production, sputum color; and minor symptoms: cough, wheeze, running nose, sore throat, and fever (>38.5 °C) (27)] (11). This meant ST was only initiated 48 hours after an initial change in symptoms. Similar to the COPE-I study (24), COPE-II data showed a significantly higher use of courses of prednisolone and antibiotics in the ST group. However, the number of reported courses in the ST group was still lower than the actual number of exacerbations reported in the diaries, meaning that prednisolone was not used during every exacerbation. The final COPE-II study results therefore indicated that this approach did not lead to overtreatment, and indeed less COPD exacerbation days and lower costs occurred in the intervention group (11). In summary, the COPE-II study demonstrated that specific COPD ST training within a more general COPD SM training intervention leads to less exacerbation days and lower costs (11). However, these study results cannot be generalized to the large population of COPD patients with comorbidities.
COPE-III
The COPE-III SM intervention incorporates (I) patient-initiated action plans that are tailored to the individual’s co-morbid disease(s) as well as their COPD, and (II) phone support from case-managers. The design of the COPE-III study, an international randomised controlled multi-centre trial, has previously been published and the intervention is currently under evaluation in both the Netherlands and Australia (26). Patient recruitment takes place in five hospitals [Netherlands: Enschede (Medisch Spectrum Twente) and Nijmegen (Canisius-Wilhelmina Ziekenhuis); Australia (Adelaide: Repatriation General Hospital, Flinders Medical Centre, Royal Adelaide Hospital)]. We expect that data collection will be completed by the end of 2015.
In the COPE-III study, we have incorporated at similar COPD ST component to that evaluated in the COPE-II study and combined this with action plans for common comorbidities [chronic heart failure (CHF), anxiety, depression, ischemic heart disease (IHD), and diabetes]. The comorbid action plan components have been developed in collaboration with multiple disease-experts (Cardiologist, Cardiac Nurse Practitioner, Endocrinologist, Psychiatrist, and Psychologist). In COPE-III, extensive patient training directed towards individualized materials is provided.
COPE-III ST approach
The COPE-III intervention involves a total of 8-9 hours of SM session time and several additional follow-up phone calls. A more specific description of the intervention has been provided in a previous paper (26). Because of the adjustment of intervention materials for comorbidities, materials are more complex than the ones used in previous two studies. It has therefore become necessary to deliver half the COPE-III training sessions individually instead of in a group and to allocate relatively more session time towards specific ST training compared to previous interventions. ST materials include a ‘what are my usual symptoms’ card, a daily symptom diary, and an action plan. During training in the use of these materials, hypothetical scenarios were incorporated to engage the patient in practicing the completion of the diaries and understanding appropriate use of the action plans.
As in previous studies, SM training is provided by case-managers (respiratory nurses). Patients are provided with information on how to contact the case-manager if they have any doubts or questions. Access to case-managers is available during office hours and patients are advised to contact their GP or Emergency Department during out of office hours. The case-manager also acts as a triage nurse when the cause of the change in symptoms is unclear and additional advice is necessary (26).
COPE-III ST materials
Even when stable, many patients with COPD experience symptoms of their respiratory disease and comorbidities, especially patients with moderate to severe disease (19). In the COPE-III intervention, the nurse and patient define together the patient’s symptoms during a stable health state and summarize these findings in the patients’ ‘what are my usual symptoms’ card. The patient is advised to use this card while completing the daily symptom diary and to indicate whether symptoms have changed compared with their stable health state. So as in COPE-II (11), ST actions are linked to changes in symptoms rather than to existing symptoms. This approach requires that patients have skills and knowledge to recognize deterioration in their symptoms (28).
Patients are asked to complete the symptom diary that includes respiratory symptoms and relevant comorbid symptoms, every day. When patients do not experience deterioration in any of the predetermined symptoms listed in the diary during the last 24 hours, they are instructed to tick the box ‘no change in symptoms’ (indicating no further actions are required). Whenever they experience deterioration in any symptom listed in the diary, they are asked to report the level of change for each of the listed symptoms and if this change is of sufficient magnitude, consult their tailored action plan (26).
Besides the COPD component, all daily symptom diaries and action plans include one or more comorbid components in a pre-defined order: (I) CHF; (II) anxiety and/or depression (AD); (III) IHD; and (IV) diabetes. Diabetes action plans differ for patients with type 1, type 2 and prednisolone-induced diabetes. As such, there are 21 possible action plans that can be instigated.
Cardiac component
Similar action plans are provided for two cardiac comorbidities, IHD and CHF, in both Australia and the Netherlands.
For CHF three questions are included in the daily symptom diary regarding fluid retention (weight, swelling of ankles and abdomen, and waking up at night short of breath). According to the action plan, patients should increase/start their diuretic medication when they record ‘a significant change’ for two consecutive days for at least one of these questions. The expert team agreed that a change in weight of at least one kilogram in 24 hours should be considered a significant change. Patients are asked to contact the case-manager if symptoms do not decrease with diuretic therapy, or if they think they need more than the 3-day diuretic course as directed in the action plan. In the Netherlands patients are asked to contact their cardiac nurse directly.
A second CHF action plan component is included for safety reasons. Patients are asked to contact the case-manager (or cardiac nurse for Dutch patients) if they become more light-headed and/or dizzy. Consequently, the case-manager contacts the cardiac nurse to see if further actions are required (possible causes for these symptoms include rhythm disorder, over diuresis or a side effect of medication).
The existing action plan for IHD, developed by the ‘National Heart Foundation of Australia’, is being used with minor adjustments in lay-out (29).
Anxiety and depression
The action plan for anxiety and depression advises patients to commence relaxation exercises (which are practiced during the SM courses) if they experience increased AD. If symptoms do not improve after 5 days patients are asked to contact the case-manager (Dutch patients could directly contact the mental health worker). When necessary, their predefined ‘plan’ (e.g., seeing their GP to discuss their symptoms and management) is activated and/or a consult with a psychologist arranged.
Prior to inclusion patients are screened with the Hospital Anxiety and Depression Scale (HADS) (30). Patients with scores meeting recognized clinical cut-off points (exceeding 10 per subscale) of the HADS (30) are offered psychological counseling prior to the baseline measurement.
Although experiencing suicidal ideation is an exclusion criterion for the COPE-III study, standardised action plans are used if patients develop suicidal ideation during the study. For example, patients may contact nurses who conduct a risk assessment and patients are also provided with an emergency 24-hour phone number for specialised counselling for suicidal ideation.
Diabetes
Prednisolone treatment of COPD exacerbations increases blood glucose levels (BGLs), especially in patients with pre-existing diabetes. Hyperglycaemia in patients treated with prednisolone predominantly occurs between midday and midnight (31). Higher glucose concentrations are associated with increased mortality, morbidity and length of hospital stay during a COPD exacerbation (32,33).
Separate diabetes action plan components were developed for type 1, type 2 and prednisolone-induced diabetes. In contrast with the other comorbidities, the diabetes action plans are not linked to a change in ‘diabetes’ symptoms, but to the start of a COPD exacerbation. When taking prednisolone, patients are advised to check their BGL four times per day (before breakfast, lunch, dinner, and bed time). Extra training on blood glucose monitoring and insulin injections is then arranged with a diabetes nurse if required.
There are differences in the action plans for diabetes used in Australia and the Netherlands, in order to mimic as much as possible usual care in both countries and simplify possible future implementation.
In Australia, patient management plans have been developed for two main groups of patients: (I) patients with diet-controlled diabetes or taking oral hypoglycaemic agents; and (II) patients already taking insulin. If patients record one BGL above 15 mmol/liter or two measurements above 10 mmol/liter, the action plan directs them to contact the case-manager who then contacts an endocrinologist. Patients who are not already taking insulin are taught to administer insulin isophane during COPD exacerbations, with dosing adjustments by an endocrinologist based on ongoing BGL recordings. Patients who are already taking insulin have their current insulin regimen doses adjusted by the endocrinologist.
In the Netherlands, patients with diet-controlled diabetes or taking oral hypoglycaemic agents are instructed to use insulin injections temporarily if they experience a high BGL (one BGL measurement above 15 mmol/liter or three measurements above 10 mmol/liter during a 24-hour period). Insulin dosing schedules are patient-fitted by the diabetes nurse and discussed during SM training. Patients have a tailored insulin dosing schedule (as advised by the diabetes nurse) or they are instructed to administer short-acting subcutaneous insulin using a sliding scale regimen.
Optimising of the COPE-III ST intervention
Prior to the start of the randomized controlled trial, the COPE-III ST intervention was tested in six patients with severe COPD to further optimize the intervention. Recruited patients were already included in an intensive nurse-led case-management program to which the COPE-III ST intervention was added. During the pilot, study nurses and patients were asked to provide frank feedback on the materials. During and after the pilot, significant adjustments were made to the ST materials. We have summarized an overview of these adjustments in Table 2. The intervention materials were adjusted to ensure that the intervention could be easily implemented in different health care systems.
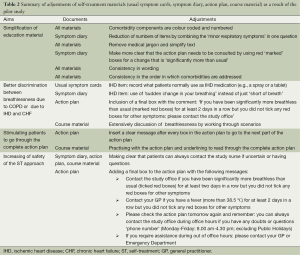
Full table
Training of the health care providers
Both the COPE-I and COPE-II studies were extensively piloted (by groups of health care providers and patients). Besides optimising the intervention, the goal of these pilots was to train all health care providers in ‘SM’. In addition, all involved health care providers in the COPE-III study attended a half day course regarding the guidance of group sessions. The content of this course included discussion of behavioural change techniques that were embedded in the SM sessions: components of education, training, modelling, and enablement, which target desirable and specific behaviours including individualised diary use, patient recognition of deterioration in symptoms, and the correct and timely use of an action plan (26). Ongoing, regular follow-up meetings (approximately once a month) were planned with the health care providers involved.
The COPE-III study was also extensively piloted by patients and health care providers. The education in comorbidities was provided by disease experts in both countries (approximately 2-3 hours per comorbidity) and predominantly directed towards triaging of problems that could occur in these complicated COPD patients. Overlap in disease symptoms was discussed intensively. The training in SM and behaviour change principles was provided by an Australian psychologist during a 2-hour group meeting. This meeting was recorded, so it could also be viewed by the study nurse in the Netherlands.
Separate training in the diaries and action plans was provided by the study investigators in both countries (approximately 4 hours), with frequent follow-up meetings, that were especially important during the first year of the study.
Discussion
The COPE-III study is focused on treatment of COPD and common comorbid diseases. The intervention was developed and adjusted by using experiences and knowledge learnt from two previous COPE studies and by a pilot study. Although the action plans used in COPE-III are established and cannot be changed during evaluation, we are aware that we can continue learning from our experiences with COPD ST.
In the COPE-III study, we are attempting to deal with two of the most important lingering issues within ST, namely dealing with comorbidities and ensuring patient safety. We believe that a ‘one size fits all’ approach that focuses solely on traditional symptoms of COPD is inadequate and in fact, potentially dangerous in patients with (numerous and severe) comorbidities. This was the rationale underpinning the COPE-III approach. We have tried to optimize patient safety by ensuring a case-manager who is accessible to patients throughout the study. This is emphasized during patient training and highlighted on all ST materials. We also incorporated fallback procedures into the action plans, such as contacting usual health care providers for unresolved or worsening breathlessness or fever (see Table 2). The safety of the study is monitored by a Data and Safety Monitoring Board.
Another recommendation is that ST approaches have to be included in a formal SM training intervention (10) that includes behavioural change techniques (9) and is tailored to the patient’s individual needs (9). The COPE-III intervention meets all of these criteria. Behavioural change techniques are included in an extensive patient training intervention (e.g., education, training, modeling, individualised action plans, behavioural enablement, individualised goal setting, and feedback on behaviour). Although ST of co-morbidities is patient-tailored, the content of the SM training is part of an intervention with set components (e.g., disease education, relaxation, and breathing techniques). In COPE-III we have utilised a ST approach that provides appropriate tools, training in necessary skills, and the possibility to incorporate the approach in existing health care support systems (9).
Additionally, health literacy of patients should also be taken into account. Literature suggests that only a third of patients with low literacy are able to comply with simple written instruction such as ‘Take two tablets by mouth twice daily’ (34). We are acutely aware that our ST materials are much more complicated than this instruction, and we concede that SM is not an approach that would be suitable for all patients with chronic diseases like COPD. However, lessons were learnt during the pilot study and the patient materials were simplified. Although we exclude patients who are non-literate and those assessed as having an impaired cognitive function (26), we have not excluded people with low health literacy in any of the COPE studies.
For ST of COPD exacerbations it is also important to keep in mind that patients should be able to use their action plans regularly. If their symptoms are not varying with some frequency, amounting to repeated exacerbations, there are no opportunities for them to refer to their action plan and therefore learn from or receive feedback on their actions. In COPE-II and COPE-III it was therefore decided to include only frequently exacerbating COPD patients (patients who had at least three exacerbations or one respiratory related hospitalization in 2-year previous to inclusion).
At present there is no general agreement on the specifics of training health care providers to deliver optimal SM interventions, although experts agree that training of health care providers is crucial. In preparation for COPE-III, a psychologist was asked to provide a discussion session regarding behavioural change techniques that could be included in the COPE-III intervention. As this is an important aspect of SM, additional follow-up meetings were organized to discuss behavioural change techniques.
Finally, little is known about the factors influencing the success and failure of SM interventions, although understanding is growing as we acknowledge the intricacies of human behaviour and what drives behaviour change. Perhaps even less is known of the factors influencing the success and failure of ST interventions, and further studies will hopefully shed more light on this in the near future.
Acknowledgements
We would like to thank all disease-experts in respiratory and cardiovascular disease, diabetes, and anxiety and depression for their expertise regarding the development and adjustments of the action plans: Robert Minson, Malcolm Battersby, Marie-Jose Pouwels, Elly Wajon, Hermien ten Bolscher, Anneke van Veen, Janneke Roukema, Anna Weierink and Astrid Brilleman. Finally we would like to thank the data managers Betty Rinsma, Petra Meerlo, Sylvia Punte and Anne Southwell, and the nurses Chantal Bergman, Kim Klieverik, Marin Bilgic, Judith Grooters, Alice Grooten-Nijkamp, Saskia van Diepenbeek, Diana Verstralen, Jacqueline Kloek-Verweij, Ilse Bosman, Marijke van de Pavert, Adrienne Beverley, Cheryl Parton for their support in running the current study and previous studies.
Funding from the Netherlands Lung Foundation, the Lung Foundation Australia, and the Repat Foundationhas made it possible to develop and perform this study.
Disclosure: The authors declare no conflict of interest.
References
- Australia’s health 2010: The twelfth biennial health report of the Australian Institute of Health and Welfare. Canberra: The Australian Institute of Health and Welfare 2010.
- Jemal A, Ward E, Hao Y, et al. Trends in the leading causes of death in the United States, 1970-2002. JAMA 2005;294:1255-9. [PubMed]
- Economic Impact of COPD and Cost-Effective Solutions. Available online: http://www.rnig.org.au/docs/EconomicImpactofCOPDandCostEffectiveSolutions-226.pdf
- Frith PA, Cafarella PA, Duffy JM. Chronic obstructive pulmonary disease (COPD) is a major personal and public health burden in Australia. Aust N Z J Public Health 2008;32:139-41. [PubMed]
- Foster TS, Miller JD, Marton JP, et al. Assessment of the economic burden of COPD in the U.S.: a review and synthesis of the literature. COPD 2006;3:211-8. [PubMed]
- Wilson DH, Tucker G, Frith P, et al. Trends in hospital admissions and mortality from asthma and chronic obstructive pulmonary disease in Australia, 1993-2003. Med J Aust 2007;186:408-11. [PubMed]
- Celli BR, Barnes PJ. Exacerbations of chronic obstructive pulmonary disease. Eur Respir J 2007;29:1224-38. [PubMed]
- Zwerink M, Brusse-Keizer M, van der Valk PD, et al. Self management for patients with chronic obstructive pulmonary disease. Cochrane Database Syst Rev 2014;3:CD002990. [PubMed]
- Effing TW, Bourbeau J, Vercoulen J, et al. Self-management programmes for COPD: moving forward. Chron Respir Dis 2012;9:27-35. [PubMed]
- Walters JA, Turnock AC, Walters EH, et al. Action plans with limited patient education only for exacerbations of chronic obstructive pulmonary disease. Cochrane Database Syst Rev 2010;CD005074. [PubMed]
- Effing T, Kerstjens H, van der Valk P, et al. (Cost)-effectiveness of self-treatment of exacerbations on the severity of exacerbations in patients with COPD: the COPE II study. Thorax 2009;64:956-62. [PubMed]
- Rice KL, Dewan N, Bloomfield HE, et al. Disease management program for chronic obstructive pulmonary disease: a randomized controlled trial. Am J Respir Crit Care Med 2010;182:890-6. [PubMed]
- Trappenburg JC, Monninkhof EM, Bourbeau J, et al. Effect of an action plan with ongoing support by a case manager on exacerbation-related outcome in patients with COPD: a multicentre randomised controlled trial. Thorax 2011;66:977-84. [PubMed]
- Barnes PJ, Celli BR. Systemic manifestations and comorbidities of COPD. Eur Respir J 2009;33:1165-85. [PubMed]
- Anecchino C, Rossi E, Fanizza C, et al. Prevalence of chronic obstructive pulmonary disease and pattern of comorbidities in a general population. Int J Chron Obstruct Pulmon Dis 2007;2:567-74. [PubMed]
- Holguin F, Folch E, Redd SC, et al. Comorbidity and mortality in COPD-related hospitalizations in the United States, 1979 to 2001. Chest 2005;128:2005-11. [PubMed]
- Crockett AJ, Cranston JM, Moss JR, et al. An association between length of stay and co-morbidity in chronic airflow limitation. Int J Qual Health Care 2000;12:41-6. [PubMed]
- Australian Centre for Asthma Monitoring 2006. Asthma and chronic obstructive pulmonary disease among older people in Australia: deaths and hospitalisations. AIHW cat. no. ACM 7. Canberra: AIHW.
- Global Initiative for Chronic Obstructive Lung Disease (GOLD). Global Strategy for the Diagnosis, Management and Prevention of COPD. 2014. Available online: http://www.goldcopd.com/uploads/users/files/GOLD_Report_2014_Oct30.pdf
- Dickstein K, Cohen-Solal A, Filippatos G, et al. ESC guidelines for the diagnosis and treatment of acute and chronic heart failure 2008: the Task Force for the diagnosis and treatment of acute and chronic heart failure 2008 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association of the ESC (HFA) and endorsed by the European Society of Intensive Care Medicine (ESICM). Eur J Heart Fail 2008;10:933-89. [PubMed]
- Fan VS, Gaziano JM, Lew R, et al. A comprehensive care management program to prevent chronic obstructive pulmonary disease hospitalizations: a randomized, controlled trial. Ann Intern Med 2012;156:673-83. [PubMed]
- Rice KL, Dewan N, Bloomfield HE, et al. Disease management program for chronic obstructive pulmonary disease: a randomized controlled trial. Am J Respir Crit Care Med 2010;182:890-6. [PubMed]
- Bourbeau J, Saad N. Integrated care model with self-management in chronic obstructive pulmonary disease: from family physicians to specialists. Chron Respir Dis 2013;10:99-105. [PubMed]
- Monninkhof E, van der Valk P, van der Palen J, et al. Effects of a comprehensive self-management programme in patients with chronic obstructive pulmonary disease. Eur Respir J 2003;22:815-20. [PubMed]
- Effing T, Zielhuis G, Kerstjens H, et al. Community based physiotherapeutic exercise in COPD self-management: a randomised controlled trial. Respir Med 2011;105:418-26. [PubMed]
- Lenferink A, Frith P, van der Valk P, et al. A self-management approach using self-initiated action plans for symptoms with ongoing nurse support in patients with Chronic Obstructive Pulmonary Disease (COPD) and comorbidities: the COPE-III study protocol. Contemp Clin Trials 2013;36:81-9. [PubMed]
- Anthonisen NR, Manfreda J, Warren CP, et al. Antibiotic therapy in exacerbations of chronic obstructive pulmonary disease. Ann Intern Med 1987;106:196-204. [PubMed]
- Fowler C, Kirschner M, Van Kuiken D, et al. Promoting self-care through symptom management: a theory-based approach for nurse practitioners. J Am Acad Nurse Pract 2007;19:221-7. [PubMed]
- National Heart Foundation of Australia. New Heart attack action plan. In: National Heart Foundation of Australia, editor 2009.
- Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand 1983;67:361-70. [PubMed]
- Burt MG, Roberts GW, Aguilar-Loza NR, et al. Continuous monitoring of circadian glycemic patterns in patients receiving prednisolone for COPD. J Clin Endocrinol Metab 2011;96:1789-96. [PubMed]
- Baker EH, Janaway CH, Philips BJ, et al. Hyperglycaemia is associated with poor outcomes in patients admitted to hospital with acute exacerbations of chronic obstructive pulmonary disease. Thorax 2006;61:284-9. [PubMed]
- Burt MG, Roberts GW, Aguilar-Loza NR, et al. Relationship between glycaemia and length of hospital stay during an acute exacerbation of chronic obstructive pulmonary disease. Intern Med J 2013;43:721-4. [PubMed]
- Davis TC, Wolf MS, Bass PF 3rd, et al. Literacy and misunderstanding prescription drug labels. Ann Intern Med 2006;145:887-94. [PubMed]


