Published online Sep 15, 2017. doi: 10.4251/wjgo.v9.i9.372
Peer-review started: February 8, 2017
First decision: May 3, 2017
Revised: May 20, 2017
Accepted: July 14, 2017
Article in press: July 17, 2017
Published online: September 15, 2017
To assess the usefulness of en bloc right hemicolectomy with pancreaticoduodenectomy (RHCPD) for locally advanced right-sided colon cancer (LARCC).
We retrospectively reviewed the database of Saitama Medical Center, Jichi Medical University, between January 2009 and December 2016. During this time, 299 patients underwent radical right hemicolectomy for right-sided colon cancer. Among them, 5 underwent RHCPD for LARCC with tumor infiltration to adjacent organs. Preoperative computed tomography (CT) was routinely performed to evaluate local tumor infiltration into adjacent organs. During the operation, we evaluated the resectability and the amount of infiltration into the adjacent organs without dissecting the adherent organs from the cancer. When we confirmed that radical resection was feasible and could lead to R0 resection, we performed RHCPD. The clinical data were carefully reviewed, and the demographic variables, intraoperative data, and postoperative parameters were recorded.
The median age of the 5 patients who underwent RHCPD for LARCC was 70 years. The tumors were located in the ascending colon (three patients) and transverse colon (two patients). Preoperative CT revealed infiltration of the tumor into the duodenum in all patients, the pancreas in four patients, the superior mesenteric vein (SMV) in two patients, and tumor thrombosis in the SMV in one patient. We performed RHCPD plus SMV resection in three patients. Major postoperative complications occurred in 3 patients (60%) as pancreatic fistula (grade B and grade C, according to International Study Group on Pancreatic Fistula Definition) and delayed gastric empty. None of the patients died during their hospital stay. A histological examination confirmed malignant infiltration into the duodenum and/or pancreas in 4 patients (80%), and no patients showed any malignant infiltration into the SMV. Two patients were histologically confirmed to have tumor thrombosis in the SMV. All of the tumors had clear resection margins (R0). The median follow-up time was 77 mo. During this period, two patients with tumor thrombosis died from liver metastasis. The overall survival rates were 80% at 1 year and 60% at 5 years. All patients with node-negative status (n = 2) survived for more than seven years.
This study showed that the long-term survival is possible for patients with LARCC if RHCPD is performed successfully, particularly in those with node-negative status.
Core tip: In this study, we retrospectively assessed the usefulness of en bloc right hemicolectomy with pancreaticoduodenectomy (RHCPD) in five patients with locally advanced right-sided colon cancer (LARCC) with malignant infiltration into adjacent organs. A histological examination confirmed malignant infiltration into the duodenum and/or pancreas in four patients, with no malignant infiltration into the superior mesenteric vein. The OS rates were 80% at 1 year and 60% at 5 years. All patients with node-negative status survived more than seven years without recurrence. The long-term survival is possible for patients, particularly node-negative ones, with LARCC if the RHCPD is performed successfully.
- Citation: Kaneda Y, Noda H, Endo Y, Kakizawa N, Ichida K, Watanabe F, Kato T, Miyakura Y, Suzuki K, Rikiyama T. En bloc pancreaticoduodenectomy and right hemicolectomy for locally advanced right-sided colon cancer. World J Gastrointest Oncol 2017; 9(9): 372-378
- URL: https://www.wjgnet.com/1948-5204/full/v9/i9/372.htm
- DOI: https://dx.doi.org/10.4251/wjgo.v9.i9.372
Locally advanced colorectal cancers invading into adjacent organs account for 5.5%-16.7% of all colorectal cancers[1-3]. Incomplete resection and separation of colon cancer from adherent organs are considered to lead to tumor recurrence and a poor prognosis[4,5]. Locally advanced right-sided colon cancer (LARCC) can invade the duodenum, pancreas, and other organs, and in this situation, en bloc right hemicolectomy with pancreaticoduodenectomy (RHCPD) is necessary to achieve R0 resection.
RHCPD for LARCC was first reported in 1953[6], and high-volume centers, including our hospital, have reported acceptable outcomes with RHCPD[7-9]. However, the number of reports describing the long-term survival and histological findings is limited given the few cases of LARCC treated with RHCPD[7,10,11].
In the present study, we retrospectively reviewed the preoperative and intraoperative assessments of LARCC with malignant infiltration into adjacent organs and the clinical outcomes of RHCPD in these cases.
We retrospectively reviewed the database of Saitama Medical Center, Jichi Medical University, between January 2009 and December 2016. During this period, 299 patients underwent radical right hemicolectomy (RHC) for right-sided colon cancer. Among them, 5 patients underwent RHCPD because of LARCC with direct infiltration to the duodenum and/or pancreas. Preoperative computed tomography (CT) was routinely performed to evaluate local tumor infiltration into adjacent organs. The preoperative carcinoembryonic antigen (CEA) and cancer antigen 19-9 (CA19-9) levels were routinely tested in all patients. Preoperative upper endoscopy, colonoscopy, and histological confirmation of the diagnosis were performed in all patients. The optimal treatment strategies for LARCC were discussed in a multidiscipline forum including surgeons, oncologists and radiologists.
The indications for RHCPD were as follows: (1) histological confirmation of colon cancer; (2) colon cancer that could not be dissociated from the pancreas and/or duodenum because of tumor infiltration; (3) radical resection deemed feasible on preoperative imaging and intraoperative exploration; and (4) no secondary or recurrent tumors.
After the Cattell-Braasch maneuver, a Kocher maneuver was performed to fully mobilize the duodenum. We evaluated the resectability of the LARCC and the amount of infiltration into the duodenum and/or pancreas without dissecting the adherent organs from the cancer. After confirming that radical resection was feasible and could lead to R0 resection, we performed RHCPD.
First, RHC was performed in accordance with the standard procedure. Pancreaticoduodenectomy (PD) was then performed via the standard procedure, and if the superior mesenteric vein (SMV) was involved, we performed en bloc SMV resection and end-to-end anastomosis of the SMV. Reconstruction was carried out in accordance with the modified Child’s reconstruction method. End-to-side anastomosis was made between the proximal stump of the pancreas and jejunum. The stent of the pancreatic duct was routinely used in pancreatojejunostomy. Finally, reconstruction of the bowel was performed via stapled side-to-side anastomosis of the ileum and transverse colon. After reconstruction, rubber drains were placed near the biliary and pancreatic anastomoses, and the abdominal wall wounds were closed.
The overall survival (OS) was considered the primary outcome. The disease-free survival (DFS), 30-d postoperative mortality, and major complications were considered the secondary outcomes. The staging process was based on the tumor-lymph node-metastasis (TNM) classification proposed by the American Joint Committee of Cancer[12]. Postoperative pancreatic fistula were categorized according to the International Study Group on Pancreatic Fistula Definition (ISGPFD)[13].
Clinical data were carefully reviewed. Demographic variables, intraoperative data, and postoperative parameters were recorded. Numerical data were presented as the median (range).
All patients were examined at three-month intervals at our outpatient department. The patients were followed up in accordance with the standard protocol, including CEA and CA19-9 measurement, abdominal ultrasound or CT, and annual colonoscopy.
The study design and procedures were approved by the Ethics Committee of Saitama Medical Center, Jichi Medical University.
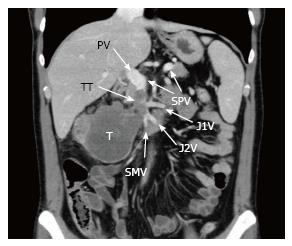
The characteristics of the patients in this series are shown in Table 1. Between 2009 and 2016, five patients (two male and three female) underwent RHCPD for LARCC with direct infiltration into adjacent organs in our hospital. The median age of the patients was 70 years (range, 47-74 years). The tumors were located in the ascending colon (three patients) and transverse colon (two patients). The histological results confirmed the diagnosis of right-sided colon cancer in all of the patients. The preoperative CEA values were 12.3 ng/mL (range, 0.5-120.8 ng/mL) and CA19-9 values were 22.5 IU/mL (range, 13.7-196.8 IU/mL). None of the patients received preoperative chemotherapy. Preoperative CT revealed infiltration of the tumor into the duodenum in all patients, the pancreas in four patients (Cases 2-5), and the SMV in two patients (Cases 4 and 5). Distant metastasis was not observed on preoperative imaging assessment in four patients (Cases 1-4). Although tumor thrombosis in the SMV was noted in one patient (Case 5), we were unable to administer preoperative chemotherapy because of tumor bleeding and stenosis (Figure 1).
| Case | Gender | Age (yr) | Site of colon cancer | Adjacent organ infiltration on preoperative CT | Preoperative CEA (ng/mL) | Preoperative CA19-9 (IU/mL) |
| 1 | Female | 73 | T | Du | 120.8 | 22.5 |
| 2 | Female | 74 | A | Du + Pa + St | 36.6 | 20.3 |
| 3 | Male | 70 | A | Du + Pa | 0.5 | 49.2 |
| 4 | Female | 57 | T | Du + Pa + Gb + SMV | 2.6 | 13.7 |
| 5 | Male | 47 | A | Du + Pa + SMV1 | 12.3 | 196.8 |
The perioperative data of the patients are listed in Table 2. Because infiltration of the tumor into the SMV was suspected based on preoperative CT findings or surgical exploration, we performed RHCPD plus SMV resection in three patients (Cases 2, 4 and 5) and added removal of tumor thrombosis in one patient (Case 5). In one patient (Case 1), we added distal pancreatectomy to RHCPD because of a neuroendocrine tumor in the pancreatic tail. The median operative time was 506 minutes (range, 304-538 minutes), and the median operative blood loss was 940 mL (range, 200-2760 mL). Major postoperative complications occurred in 3 patients (60%) as pancreatic fistula (grade B and grade C, according to ISGPFD) and delayed gastric empty (DGE). After the operation, the postoperative hospital stay was 35 d (range, 27-39 d). The postoperative course was fair in all patients, and none of the patients died during their hospital stay.
| Case | Operation | Adjacent organ infiltration in surgical exploration | OT (min) | OBL (mL) | DHS (d) | Complications |
| 1 | PD + RHC + DP | Du | 406 | 940 | 35 | PF (B) |
| 2 | PD + RHC + SMVR | Du + Pa + St + SMV | 524 | 840 | 27 | PF (C) |
| 3 | PD + RHC | Du + Pa + Gb | 304 | 200 | 33 | PF (A), DGE |
| 4 | PD + RHC + SMVR | Du + Pa + Gb + SMV | 538 | 2760 | 36 | PF (A) |
| 5 | PD + RHC + SMVR | Du + Pa + SMV1 | 506 | 2470 | 39 | PF (A) |
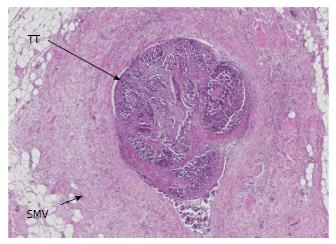
The histological characteristics are listed in Table 3. According to the TNM classification, stage T4bN0M0 (Cases 3 and 4), stage T4bN0M1a (Case 1, with metastasis of peripancreatic lymph node), stage T4bN1bM1b (Case 2, with metastasis of periduodenal lymph node and tumor thrombosis in SMV), and stage T4bN1aM1a (Case 5, with tumor thrombosis in SMV) were defined. A histological examination confirmed direct infiltration into the duodenum and/or pancreas head in four patients. Even though direct infiltration into the SMV was suspected by preoperative CT in two patients (Cases 4 and 5) or by surgical exploration in three patients (Cases 2, 4 and 5), no malignant infiltration into the SMV was confirmed. However, two patients (Cases 2 and 5) were histologically confirmed to have tumor thrombosis in the SMV (Figure 2). Well-differentiated adenocarcinoma (Cases 3, 4 and 5), moderately differentiated adenocarcinoma (Case 1), and mucinous adenocarcinoma (Case 2) were confirmed histologically. All of the tumors had clear resection margins (R0).
The chemotherapy regimens and outcomes are listed in Table 4. One patient received adjuvant chemotherapy with capecitabine treatment (Case 1). Two patients did not wish to receive adjuvant chemotherapy (Cases 3 and 4). One patient could not receive adjuvant chemotherapy because of appetite loss, but we introduced chemotherapy with cetuximab treatment for liver metastasis (Case 2). One patient had early recurrence with liver metastasis, and we introduced chemotherapy with capecitabine plus oxaliplatin and bevacizumab treatment (Case 5). The median follow-up time was 77 mo (range, 11-95 mo). No patients were lost to follow-up. During this period, two patients with tumor thrombosis died from liver metastasis (Cases 2 and 5). The OS rates were 80% at 1 year and 60% at 5 years. Three patients survived more than six years with no recurrence (Cases 1, 3 and 4). All patients without lymph node metastasis survived more than seven years (Cases 3 and 4). On the other hand, only one patient with lymph node metastasis achieved a long-term survival (Case 1).
| Case | ACT | DFS (mo) | CT | OS (mo) | Status | CD |
| 1 | Cape | 77 | - | 77 | Alive | |
| 2 | - | 5 | Cetu | 11 | Dead | LM |
| 3 | - | 95 | - | 95 | Alive | |
| 4 | - | 85 | - | 85 | Alive | |
| 5 | - | 1 | Cape + OX + Beva | 11 | Dead | LM |
To distinguish between inflammatory adhesion and malignant infiltration is difficult by preoperative imaging assessments or surgical exploration. With the development of CT technology, preoperative CT provides accurate information about the staging of colon cancer and invasion beyond the muscularis propria into adjacent organs[14]. However, preoperative CT and surgical exploration often cannot distinguish inflammatory adhesions from malignant infiltration[10,11,15-18]. In our series, malignant infiltration to the duodenum was suspected in all 5 cases by preoperative CT and surgical exploration and subsequently confirmed in 4 cases (80%) by a histological examination. However, malignant infiltration into the pancreas was suspected in 4 cases by preoperative CT and surgical exploration but only confirmed in 2 cases (50%) by a histological examination. Furthermore, malignant infiltration into the SMV was suspected in 2 cases by preoperative CT and 3 cases by surgical exploration but not confirmed in any cases (0%) by a histological examination. Therefore, in our series, both preoperative CT and surgical exploration were found to be unreliable for identifying malignant infiltration, and this phenomenon is in line with the findings of previous studies.
In the right-sided colon cancer, the rate of malignant infiltration in adhesion between the cancer and adjacent organs has been reported to range from 71%-94%[7,10,11,19]. In addition, separation of colon cancer from the adherent organs may lead to tumor recurrence rates of 90%-100%[4,5]. Therefore, adhesion between the colon cancer and adjacent organs should be assumed to be malignant infiltration. When LARCC is suspected of having infiltrated the adjacent organs, RHCPD should be performed as long as radical operation is possible. While a few authors maintain that SMV invasion is not an indication for RHCPD[20,21], we advise against hesitating to perform RHCPD with SMV resection to achieve R0 resection[8,22].
Previous studies have reported that en bloc multivisceral resection can lead to a good prognosis, with a 5-year survival rate ranging from 21%-55%, for patients with LARCC invading adjacent organs[7,10,11,20]. In our series, all patients underwent RHCPD, and three additionally underwent SMV resection to achieve R0 resection. In all patients, R0 resection was achieved, and the OS rate at 5 years was favorable (60%). Interestingly, the patients with node-negative status survived for more than seven years without recurrence (Cases 3 and 4). Saiura et al[7] reported that patients with node-negative status achieved a significantly longer survival than node-positive patients. Similarly, in another study, the patients that survived for more than seven years all had node-negative status[10].
Some colorectal cancers may behave in a locally aggressive invasion instead of causing lymphatic or hematogenous spread[7,11,23,24]. As such, RHCPD seems to provide a favorable survival for LARCC patients with this condition. In our series, only one patient (Case 1) with node-positive status survived for more than six years without recurrence, and this patient received adjuvant chemotherapy with capecitabine. Even if a patient has node-positive status, en bloc multivisceral resection plus adjuvant chemotherapy might be able to improve their prognosis. In our series, all patients with node-negative status had well-differentiated adenocarcinoma (Cases 3 and 4). Furthermore, the patient with mucinous adenocarcinoma had node-positive status in not only the regional lymph nodes but also the periduodenal lymph nodes (Case 2). In a previous report, the rate of lymph node metastasis was significantly lower for well-differentiated adenocarcinoma than mucinous or poorly differentiated adenocarcinoma in LARCC with direct infiltration into adjacent organs[7]. These previous results and our findings suggest that the histological type of tumor may affect the lymph node metastasis and prognosis in patients with LARCC.
In our series, two patients with tumor thrombosis in SMV relapsed with liver metastasis soon after operation (Cases 2 and 5). A previous review of colorectal cancer with venous tumor thrombosis found that the incidence of synchronous liver metastasis was as high as 19.5%, and the incidence of liver metastatic recurrence after complete surgical resection of the tumor was as high as 24.4%, while the liver metastatic recurrence rate of general colorectal cancer was 7.1%[25]. Tumor thrombosis in the SMV therefore seems to be a strong risk factor of synchronous and metachronous liver metastasis, leading to a poor prognosis. In the FOxTROT trial, preoperative chemotherapy resulted in significant higher rates of downstaging (55%) and R0 resection (96%) than postoperative chemotherapy for locally advanced colon cancer[26]. In another previous study, preoperative chemotherapy achieved a tumor volume reduction (62.5% of volume), R0 resection (100%), and an encouraging prognosis (3- to 5-year DFS of 88.9%-85.6% and OS of 95.3%) for locally advanced colon cancer[27]. Given the findings of these recent reports, it may thus be better to perform preoperative chemotherapy for LARCC patients with tumor thrombosis in the SMV than preemptive surgery. The role of induction preoperative chemotherapy, which might be indicated in T4b colon cancer, has not been discussed in previous reports of LARCC. In the era of advanced chemotherapy for colorectal cancer, preoperative chemotherapy might result in a better prognosis for LARCC patients with severe invasion, lymph node metastasis, or tumor thrombosis in the SMV. This issue merits further studies in the near future.
Several limitations associated with the present study warrant mention. First, the number of patients in this study was small. Because cases of LARCC undergoing RHCPD are rare, the number of patients per medical institution tends to be small. Large-scale studies may produce more reliable results. Second, the chemotherapy regimens varied among patients. In this era of advanced chemotherapy, administering the same regimen for a long-term study seems unfeasible. However, the present study also has several strengths. First, all of the patients were followed up, and the assessment of the prognosis proved to be accurate. Second, a histological examination was performed in detail, and we were able to evaluate the relationship between the preoperative CT findings, surgical exploration, and prognosis and histological findings.
In conclusion, we found that a long-term survival was therefore possible for patients with LARCC infiltrating adjacent organs, provided that RHCPD was successfully performed. This aggressive approach may help improve the prognosis, particularly in patients with node-negative status. Large-scale and long-term studies may produce more reliable results.
In locally advanced colorectal cancers invading the adjacent organs, incomplete resection and the separation of colon cancer from any adherent organs are considered to lead to tumor recurrence and a poor prognosis. The number of reports describing the long-term survival and histological findings is limited given the few cases of locally advanced right-sided colon cancer (LARCC) treated by en bloc right hemicolectomy with pancreaticoduodenectomy (RHCPD).
This is a retrospective single center experience regarding the long-term survival and histological findings of LARCC treated with RHCPD.
Long-term survival was possible for patients with LARCC that had successfully undergone RHCPD. RHCPD may help improve the prognosis of patients with LARCC, particularly in patients with a node-negative status.
The present study suggests that LARCC patients with a node-negative status are indicated for RHCPD. If a patient has tumor thrombosis in SMV, then the possibility of early recurrence should also be considered.
This manuscript deals with RHCPD for LARCC. The authors have described the preoperative assessment, intraoperative assessment, histological findings and prognosis.
Manuscript source: Invited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: Japan
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P- Reviewer: Agresta F, Horesh N S- Editor: Gong ZM L- Editor: A E- Editor: Lu YJ
| 1. | Curley SA, Carlson GW, Shumate CR, Wishnow KI, Ames FC. Extended resection for locally advanced colorectal carcinoma. Am J Surg. 1992;163:553-559. [PubMed] [Cited in This Article: ] |
| 2. | Eldar S, Kemeny MM, Terz JJ. Extended resections for carcinoma of the colon and rectum. Surg Gynecol Obstet. 1985;161:319-322. [PubMed] [Cited in This Article: ] |
| 3. | Staniunas RJ, Schoetz DJ Jr. Extended resection for carcinoma of colon and rectum. Surg Clin North Am. 1993;73:117-129. [PubMed] [Cited in This Article: ] |
| 4. | Hunter JA, Ryan JA Jr, Schultz P. En bloc resection of colon cancer adherent to other organs. Am J Surg. 1987;154:67-71. [PubMed] [Cited in This Article: ] |
| 5. | Perez RO, Coser RB, Kiss DR, Iwashita RA, Jukemura J, Cunha JE, Habr-Gama A. Combined resection of the duodenum and pancreas for locally advanced colon cancer. Curr Surg. 2005;62:613-617. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 23] [Cited by in F6Publishing: 21] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 6. | Van Prohaska J, Govostis MC, Wasick M. Multiple organ resection for advanced carcinoma of the colon and rectum. Surg Gynecol Obstet. 1953;97:177-182. [PubMed] [Cited in This Article: ] |
| 7. | Saiura A, Yamamoto J, Ueno M, Koga R, Seki M, Kokudo N. Long-term survival in patients with locally advanced colon cancer after en bloc pancreaticoduodenectomy and colectomy. Dis Colon Rectum. 2008;51:1548-1551. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 40] [Cited by in F6Publishing: 37] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 8. | Noda H, Kato T, Kamiyama H, Toyama N, Konishi F. En bloc right hemicolectomy and pancreaticoduodenectomy with superior mesenteric vein resection for advanced right-sided colon cancer. Clin J Gastroenterol. 2010;3:259-261. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 7] [Cited by in F6Publishing: 6] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 9. | Noda H, Kato T, Kamiyama H, Toyama N, Konishi F. Middle-preserving pancreatectomy for advanced transverse colon cancer invading the duodenun and non-functioning endocrine tumor in the pancreatic tail. Clin J Gastroenterol. 2011;4:24-27. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 10. | Zhang J, Leng JH, Qian HG, Qiu H, Wu JH, Liu BN, Li CP, Hao CY. En bloc pancreaticoduodenectomy and right colectomy in the treatment of locally advanced colon cancer. Dis Colon Rectum. 2013;56:874-880. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 21] [Cited by in F6Publishing: 23] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 11. | Kapoor S, Das B, Pal S, Sahni P, Chattopadhyay TK. En bloc resection of right-sided colonic adenocarcinoma with adjacent organ invasion. Int J Colorectal Dis. 2006;21:265-268. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 47] [Cited by in F6Publishing: 45] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 12. | Edge SB, Compton CC. The American Joint Committee on Cancer: the 7th edition of the AJCC cancer staging manual and the future of TNM. Ann Surg Oncol. 2010;17:1471-1474. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5537] [Cited by in F6Publishing: 6120] [Article Influence: 437.1] [Reference Citation Analysis (0)] |
| 13. | Bassi C, Dervenis C, Butturini G, Fingerhut A, Yeo C, Izbicki J, Neoptolemos J, Sarr M, Traverso W, Buchler M; International Study Group on Pancreatic Fistula Definition. Postoperative pancreatic fistula: an international study group (ISGPF) definition. Surgery. 2005;138:8-13. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3282] [Cited by in F6Publishing: 3400] [Article Influence: 178.9] [Reference Citation Analysis (0)] |
| 14. | Dighe S, Purkayastha S, Swift I, Tekkis PP, Darzi A, A’Hern R, Brown G. Diagnostic precision of CT in local staging of colon cancers: a meta-analysis. Clin Radiol. 2010;65:708-719. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 103] [Cited by in F6Publishing: 116] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 15. | Costa SR, Henriques AC, Horta SH, Waisberg J, Speranzini MB. En-bloc pancreatoduodenectomy and right hemicolectomy for treating locally advanced right colon cancer (T4): a series of five patients. Arq Gastroenterol. 2009;46:151-153. [PubMed] [Cited in This Article: ] |
| 16. | Lee WS, Lee WY, Chun HK, Choi SH. En bloc resection for right colon cancer directly invading duodenum or pancreatic head. Yonsei Med J. 2009;50:803-806. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 19] [Cited by in F6Publishing: 18] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 17. | Luna-Pérez P, Rodríguez-Ramírez SE, De la Barrera MG, Zeferino M, Labastida S. Multivisceral resection for colon cancer. J Surg Oncol. 2002;80:100-104. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 27] [Cited by in F6Publishing: 27] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 18. | Yun SH, Yun HR, Lee WS, Cho YB, Lee WY, Chun HK. The clinical outcome and prognostic factors after multi-visceral resection for advanced colon cancer. Eur J Surg Oncol. 2009;35:721-727. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 8] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 19. | Sheng QS, Chen WB, Li MJ, Cheng XB, Wang WB, Lin JJ. Combined right hemicolectomy and pancreaticoduodenectomy for locally advanced right hemicolon cancer. Hepatobiliary Pancreat Dis Int. 2015;14:320-324. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 8] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 20. | Zhao YZ, Han GS, Lu CM, Ren YK, Li J, Ma PF, Gu YH, Liu CY, Wang JX. Right hemicolectomy and multivisceral resection of right colon cancer: A report of 21 cases. J Huazhong Univ Sci Technolog Med Sci. 2015;35:255-258. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 6] [Cited by in F6Publishing: 8] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 21. | Zhao YZ, Han GS, Li Z, Ren YK, Lu CM, Gu YH. [Treatment outcomes of multivisceral resection for locally advanced right colon cancer]. Zhonghua Weichang Waike Zazhi. 2011;14:372-374. [PubMed] [Cited in This Article: ] |
| 22. | Yoshimi F, Asato Y, Kuroki Y, Shioyama Y, Hori M, Itabashi M, Amemiya R, Koizumi S. Pancreatoduodenectomy for locally advanced or recurrent colon cancer: report of two cases. Surg Today. 1999;29:906-910. [PubMed] [Cited in This Article: ] |
| 23. | Curley SA, Evans DB, Ames FC. Resection for cure of carcinoma of the colon directly invading the duodenum or pancreatic head. J Am Coll Surg. 1994;179:587-592. [PubMed] [Cited in This Article: ] |
| 24. | Koea JB, Conlon K, Paty PB, Guillem JG, Cohen AM. Pancreatic or duodenal resection or both for advanced carcinoma of the right colon: is it justified? Dis Colon Rectum. 2000;43:460-465. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 53] [Cited by in F6Publishing: 50] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 25. | Otani K, Ishihara S, Hata K, Murono K, Sasaki K, Yasuda K, Nishikawa T, Tanaka T, Kiyomatsu T, Kawai K. Colorectal cancer with venous tumor thrombosis. Asian J Surg. 2016; Epub ahead of print. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 16] [Cited by in F6Publishing: 18] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 26. | Arredondo J, Martínez P, Baixauli J, Pastor C, Rodríguez J, Pardo F, Rotellar F, Chopitea A, Hernández-Lizoáin JL. Analysis of surgical complications of primary tumor resection after neoadjuvant treatment in stage IV colon cancer. J Gastrointest Oncol. 2014;5:148-153. [PubMed] [DOI] [Cited in This Article: ] [Cited by in F6Publishing: 5] [Reference Citation Analysis (0)] |
| 27. | Foxtrot Collaborative Group. Feasibility of preoperative chemotherapy for locally advanced, operable colon cancer: the pilot phase of a randomised controlled trial. Lancet Oncol. 2012;13:1152-1160. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 270] [Cited by in F6Publishing: 314] [Article Influence: 26.2] [Reference Citation Analysis (0)] |