Published online Aug 16, 2014. doi: 10.4253/wjge.v6.i8.345
Revised: June 3, 2014
Accepted: June 27, 2014
Published online: August 16, 2014
Endoscopic retrograde cholangiopancreatography (ERCP) in patients with surgically altered anatomy is challenging. Several operative interventions of both the gastrointestinal tract and the biliary and/or pancreatic system lead to altered anatomy, rendering ERCP more difficult or even impossible with a conventional side-viewing duodenoscope. Adapted endoscopes are available to reach the biliopancreatic system and to perform ERCP in patients with altered anatomy. However, both technical difficulties and complications determine the procedure’s success. Different technical approaches have been described and are highly dependent on local expertise and endoscopic equipment. Standardized practical guidelines are currently unavailable. This review focuses on the challenges encountered during ERCP in patients with altered anatomy and how to deal with them. The first challenge is reaching the papilla or the bilioenteric/pancreatoenteric anastomosis in the patient with postoperative altered anatomy. The second challenge is the cannulation of the biliopancreatic system and performing all conventional ERCP interventions and the third challenge is the control of possible complications. The available literature data on this topic is reviewed and illustrated with clinical cases.
Core tip: Endoscopic retrograde cholangiopancreatography in patients with surgically altered anatomy is difficult and faces several challenges. There are three important challenging steps in this endoscopic procedure: reaching the papilla or the bilioenteric/pancreatoenteric anastomosis, cannulation of the biliopancreatic system and prevention of endoscopic complications. Since there are no standardized practical and technical guidelines on this topic, this review illustrates these challenges with clinical cases.
- Citation: Moreels TG. Endoscopic retrograde cholangiopancreatography in patients with altered anatomy: How to deal with the challenges? World J Gastrointest Endosc 2014; 6(8): 345-351
- URL: https://www.wjgnet.com/1948-5190/full/v6/i8/345.htm
- DOI: https://dx.doi.org/10.4253/wjge.v6.i8.345
Endoscopic retrograde cholangiopancreatography (ERCP) for endoscopic treatment of biliopancreatic disorders is performed with a side-viewing duodenoscope introduced through the mouth into the second portion of the duodenum, where the major (or minor) papilla is cannulated. It is a highly efficient technique combining both endoscopic and radiological imaging[1]. However, ERCP is prone to complications, even in experienced hands. Apart from bleeding, perforation, cholecystitis and cholangitis, post-ERCP pancreatitis is the most common[2]. Therefore, it is considered an advanced endoscopy technique requiring specific training to perform sphincterotomy and sphincteroplasty, stone extraction, stent placement, tissue sampling and more[3].
However, additional difficulties and complications do arise when performing ERCP in postoperative patients with altered anatomy[4]. Proper knowledge of postoperative anatomy and training in conventional ERCP are mandatory before embarking into ERCP procedures in patients with surgically altered anatomy, as reviewed elsewhere[5,6]. In addition, when using device-assisted enteroscopy (DAE) to perform ERCP, training in deep enteroscopy is also necessary[4]. ERCP in patients with altered anatomy faces three important challenges determining the procedure’s success rate: (1) ability to reach intact papilla of Vater or bilioenteric/pancreatoenteric anastomosis; (2) ability to cannulate intact papilla of Vater or bilioenteric/pancreatoenteric anastomosis; and (3) procedure-related complications. These topics will be highlighted in the current review.
Because of these difficulties, ERCP procedures in patients with altered anatomy are mostly performed in tertiary referral centers for advanced endoscopy, in close collaboration with the radiologist, surgeon and anesthesiologist. In order to correctly inform the patient about success rate and complication risks, it is advised to discuss these aspects in advance with the patient (and/or relatives), even if the patient is referred from another center. Finally, general anesthesia (with endotracheal intubation) is preferred for these demanding ERCP procedures.
Although recently reviewed and illustrated elsewhere, it is important to recapitulate the most prevalent surgical anatomy variations encountered during ERCP[4,5]. In general, currently encountered postoperative anatomy variations can be divided into: Billroth II partial gastrectomy with intact papilla, short-limb Roux-en-Y reconstruction with intact papilla (total gastrectomy) or with bilioenteric/pancreatoenteric anastomosis (biliary diversion, Whipple resection) and long-limb Roux-en-Y reconstruction with intact papilla (gastric bypass, Scopinaro biliopancreatic diversion).
Since there is no standardized procedure to perform ERCP in patients with altered anatomy and difficult-to-access biliopancreatic system, different types of endoscopes can be used, depending on local expertise and availability[4-6]. A conventional side-viewing duodenoscope can be used in a case of short-limb postoperative anatomy with variable success[5]. However, due to the difficult endoscopic orientation of a side-viewing endoscope in intestinal anastomoses with variable length limbs, the conventional duodenoscope carries important drawbacks in postoperative patients[7]. Therefore, alternative endoscopes have been used in order to increase the ERCP success rate[4]. Forward-viewing gastroscopes and colonoscopes, with or without additional distal cap, have been shown to be useful[5,8]. DAE (single-balloon, double-balloon and spiral enteroscopy) can also be used in the original long (200 cm) version or with an adapted shorter (152 cm) length[4-6,9-12]. Prototype endoscopes like the swan neck shaped multi-bending backward-oblique viewing duodenoscope (M-D scope, TJF-Y0011; Olympus)[13], the variable stiffness duodenoscope (TJF-Y0001; Olympus)[14] and the multi-bending forward-viewing endoscope with two working channels (M-scope, GIF-2T260M, Olympus)[15] may increase ERCP success rate in patients with altered anatomy[4].
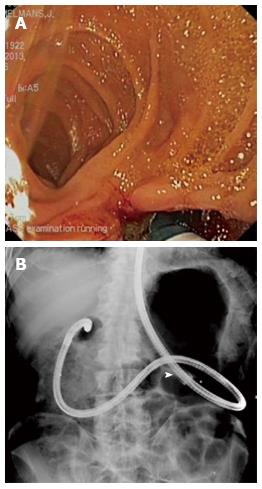
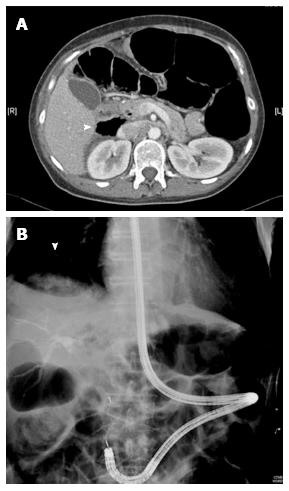
In order to perform ERCP, the endoscope is positioned in front of the intact papilla of Vater or bilioenteric/pancreatoenteric anastomosis. In patients with surgically altered anatomy, intubation of the endoscope is more challenging, depending on the type of surgery. There are several critical steps determining the success rate of the intubation procedure. In patients with Billroth II partial gastrectomy, the afferent limb is intubated through the gastrojejunostomy. However, the afferent limb is usually oriented on the right side of the anastomosis with a sharp angulation (Figure 1A). Crossing the anastomosis and angulation with a conventional side-viewing duodenoscope is difficult and increases the risk of perforation at the level of the anastomosis or the afferent limb[16]. Although the afferent limb is usually short (< 50 cm), its tortuous length may vary considerably, rendering complete intubation difficult. Forward-viewing endoscopes facilitate intubation of the afferent limb thanks to better endoscopic orientation during the intubation procedure[4,5]. In a case of a short-limb reconstruction, a conventional gastroscope can be used. However, sharp angulation at the level of the gastrojejunostomy or a long afferent limb may lead to loop formation in the gastric remnant, leading to failed intubation of the afferent limb (Figure 1B). Abdominal compression or changing the patient’s position can be used to guide the endoscope[5]. Alternatively, the afferent limb may be differentiated (and marked with a submucosal tattoo) with a user-friendly gastroscope before switching to the duodenoscope[5]. Longer (variable stiffness) colonoscopes or DAE may overcome this difficulty[4]. However, the steerable tip of the colonoscope makes wider angulations compared to the gastroscope or enteroscope. The use of a semi-rigid overtube in a case of DAE inhibits loop formation of the enteroscope in the gastric remnant[10].
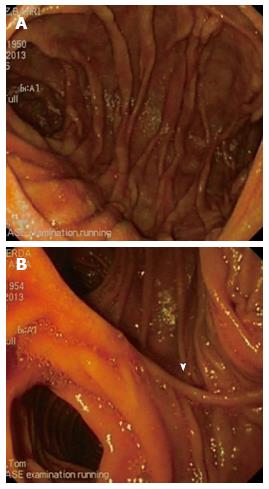
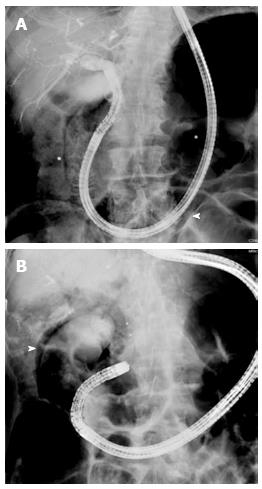
Postoperative Roux-en-Y anatomy is characterized by short (< 50 cm) or long (> 100 cm) limbs, depending on the type of surgery. Because of the lengthy limbs, longer endoscopes are usually necessary to reach the Roux-en-Y anastomosis and to intubate the afferent limb. Since conventional duodenoscopes are not long enough, forward-viewing colonoscopes or DAE are used to perform ERCP in patients with Roux-en-Y reconstruction of the small bowel, with DAE being the most effective[4,5,17,18]. The first critical step is to reach the Roux-en-Y anastomosis through the alimentary limb, especially in a case of long-limb reconstruction. Ring-shaped metal surgical clips can sometimes be seen on fluoroscopy, identifying the location of the Roux-en-Y anastomosis, which is constructed either end-to-side or side-to-side (Figure 2). Identification of the afferent limb is challenging. To intubate the correct limb, the anastomotic scar must be crossed, avoiding the common limb towards the colon[6]. When done so, there are two remaining limbs in the case of a side-to-side reconstruction. One is short and ends blindly. The afferent limb can be recognized based on the presence of luminal bile and antiperistaltic motility. Similarly to the Billroth II reconstruction, the angulation towards the afferent limb can be very sharp, leading to failed intubation. The use of a forward-viewing variable stiffness colonoscope or DAE with a semi-rigid overtube is mandatory in order to successfully intubate the afferent limb[4,5,17,19]. Sometimes abdominal compression may guide the endoscope into the right direction. Fluoroscopy is very helpful to identify the afferent limb since it is always heading towards the upper abdomen. When the endoscope heads down to the lower abdomen, it is located in the common limb.
Also, the afferent limb may be of considerable length and can be very torqued due to postoperative adhesions, posing a third critical step to reach the papilla or bilioenteric/pancreatoenteric anastomosis. Air enterogram by insufflation of a closed loop system helps to estimate the direction of the afferent limb and the distance towards the duodenum[11]. Until now, there appears to be no difference in efficacy in intubating the afferent limb between all three DAE methods (single-balloon, double-balloon, spiral enteroscopy)[18-20]. In addition, the short type single- and double-balloon enteroscopes are also effective to perform ERCP in patients with Roux-en-Y postoperative anatomy[9-12,21].
In all cases of altered postoperative anatomy, the papilla or bilioenteric/pancreatoenteric anastomosis is reached from below. This distal approach changes the direction of cannulation of papilla of Vater since the common bile duct is in direct line with the working channel of the forward-viewing endoscope, in contrast to conventional ERCP in normal anatomy using a side-viewing duodenoscope[6]. Unfortunately, this can be considered as the only advantage of the distal approach.
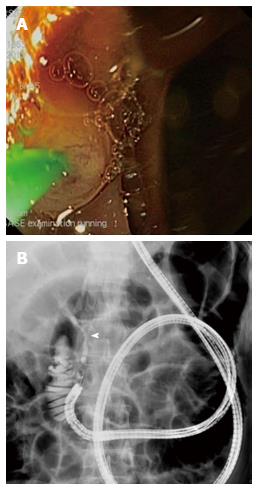
The first critical step to cannulate the intact papilla of Vater is the orientation of the endoscope. In contrast to conventional ERCP, the location of the papilla may be difficult, even when using a side-viewing duodenoscope in a Billroth II gastrectomy patient[5]. Rotation of the endoscope is often necessary. This is the case even more with a forward-viewing gastroscope, colonoscope or DAE. Complete intubation of the endoscope up to the blind end of the afferent limb and then slow retraction until the papilla is in sight is probably the most efficient way to locate it. Then, rotation of the endoscope in order to face the papilla in the 7 o’clock position enables cannulation with a straight catheter, keeping in mind that the common bile duct is thus in line with the working channel of the forward-viewing endoscope (Figure 3)[6]. However, unstable endoscope position and the lack of a forceps elevator modality renders cannulation challenging. A distal cap at the tip of the forward-viewing endoscope may help cannulation since it enables tilting of the papilla[8]. In general, it is easier to cannulate the common bile duct from the distal approach with a forward-viewing endoscope compared to the pancreatic duct.
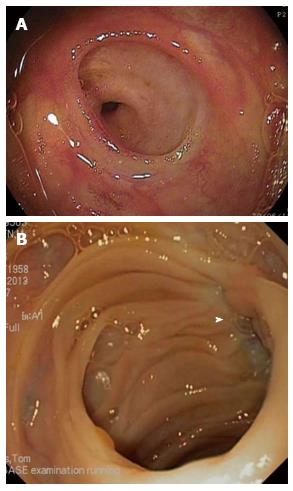
There is considerable advantage of cannulation of a bilioenteric/pancreatoenteric anastomosis over cannulation of an intact papilla because of the lack of a sphincter in a papillary structure. This results in higher ERCP success rates[22-24]. Classical end-to-side bilioenteric anastomosis can be clearly identified as a hole in the wall of the afferent limb (Figure 4A). Its presence and location can be identified by means of intermittent bile flow in the afferent limb. However, when stenosis occurs at the level of the bilioenteric or pancreatoenteric anastomosis, its location is difficult and should be identified with the help of fluoroscopy, showing the position of the endoscope’s tip near the liver or the pancreas. Air cholangiogram with insufflation of the closed afferent limb may locate the open bilioenteric anastomosis. Otherwise, mucosal scar tissue with star shaped folds may direct to the location of the strictured anastomosis (Figure 4B).
One has to take into account that using DAE for ERCP necessitates adapted specialized accessory catheters because of the length (230 cm) and the diameter (2.8 mm) of the working channel of currently used enteroscopes[4-6]. Conventional ERCP catheters can therefore not be used with these enteroscopes. Moreover, plastic stent placement is only possible with 5 or 7 Fr stents and not with the conventionally used 10 Fr stents. Self-expandable metal biliary or pancreatic stents cannot be used with enteroscopes because of the length and diameter mismatch of the working channel. Alternative procedures with a percutaneous or laparoscopy-assisted approach are mandatory when metal stent placement is required, as reviewed elsewhere[4,5].
A review of the literature demonstrates a complication risk ranging from 0% to 19.5% of ERCP procedures in patients with altered anatomy, with perforation being the most frequent and sometimes lethal, followed by bleeding, cholangitis, mucosal tears and post-ERCP pancreatitis[6]. The risk of post-ERCP pancreatitis remains relatively low, in contrast to conventional ERCP, since most indications for ERCP in patients with altered anatomy are restricted to the biliary tract, which is more easily cannulated in the distal approach compared to the pancreatic duct[2,6].
Intestinal perforations may occur at different levels along the intubated tract, leading to abdominal, retroperitoneal or subcutaneous free air[6]. ERCP in the early postoperative phase should be avoided in order not to disrupt fresh surgical anastomoses[23]. Difficult intubation across sharply angulated anastomoses or postoperatively fixed and torqued intestinal limbs may lead to perforation along the intestinal tract. At the level of the papilla, perforation may occur after sphincterotomy and/or sphincteroplasty due to a less well-controlled cutting procedure with a forward-viewing endoscope in an unstable position.
Finally, a peculiar barotrauma in a closed loop system may occur when intraluminal pressure increases steadily in the blind afferent limb. This may occur when using balloon-assisted enteroscopy overtubes sealing the distal end of the blind afferent limb. When air is insufflated continuously during the procedure without the ability to decompress via mouth or anus, intraluminal pressure increases in the closed afferent limb, resulting in air leakage through a wall weakness (sphincterotomy, mucosal tear in afferent limb, biliary tract after sphincterotomy/sphincteroplasty) (Figure 5). This risk is lower in gastric bypass patients since the insufflated air can escape into the excluded stomach which can still dilate and decompress the afferent intestinal limb. However, in all other surgical variations, this risk is present when performing single- or double-balloon enteroscopy ERCP. Another type of barotrauma can be seen during direct cholangioscopy using a slim forward-viewing endoscope. After sphincterotomy and additional sphincteroplasty, the forward viewing gastroscope, pediatric colonoscope or enteroscope can be introduced into the common bile duct since it is direct in line with the endoscope. Continuous air insufflation into the closed biliary tract may cause rupture of the gallbladder or dehiscence of the hepatic capsule (Figure 6). These types of barotraumas should be avoided by using CO2-insufflation which is absorbed much faster by the intestinal mucosa compared to air and intermittent desufflation of the overtube’s balloon in order to allow decompression of the afferent limb. This maneuver of balloon desufflation may lead to position loss of the enteroscope and the need for re-introduction.
ERCP in patients with altered anatomy remains a challenging procedure. Technical difficulties defined by inability to reach or to cannulate the biliopancreatic system and complications determine the overall success rate of these advanced endoscopic procedures. The availability of new types of endoscopes nowadays allows ERCP in patients with altered anatomy, even with long-limb Roux-en-Y reconstruction. However, the use of these new endoscopes may lead to new difficulties and complications like previously unseen barotraumas in closed afferent intestinal limbs. There is currently no gold standard approach to deal with biliopancreatic disorders in patients with surgically altered anatomy. In addition, there are no standardized technical guidelines available since ERCP in patients with altered anatomy is an endoscopic procedure in active evolution, aiming for faster, easier, more efficient and safer results.
P- Reviewer: Leitman IM, Murata A, Trifan A S- Editor: Ji FF L- Editor: Roemmele A E- Editor: Zhang DN
| 1. | Cotton PB. ERCP overview. A 30-year perspective. Cotton P, Leung J, editors. Massachusetts: Blackwell Publishing Ltd 2005; 1-8. [Cited in This Article: ] |
| 2. | Dumonceau JM, Andriulli A, Deviere J, Mariani A, Rigaux J, Baron TH, Testoni PA. European Society of Gastrointestinal Endoscopy (ESGE) Guideline: prophylaxis of post-ERCP pancreatitis. Endoscopy. 2010;42:503-515. [Cited in This Article: ] |
| 3. | Adler DG, Baron TH, Davila RE, Egan J, Hirota WK, Leighton JA, Qureshi W, Rajan E, Zuckerman MJ, Fanelli R. ASGE guideline: the role of ERCP in diseases of the biliary tract and the pancreas. Gastrointest Endosc. 2005;62:1-8. [Cited in This Article: ] |
| 4. | Moreels TG. ERCP in the patient with surgically altered anatomy. Curr Gastroenterol Rep. 2013;15:343. [Cited in This Article: ] |
| 5. | Lee A, Shah JN. Endoscopic approach to the bile duct in the patient with surgically altered anatomy. Gastrointest Endosc Clin N Am. 2013;23:483-504. [Cited in This Article: ] |
| 6. | Moreels TG. Altered anatomy: enteroscopy and ERCP procedure. Best Pract Res Clin Gastroenterol. 2012;26:347-357. [Cited in This Article: ] |
| 7. | Dubecz A, Ottmann J, Schweigert M, Stadlhuber RJ, Feith M, Wiessner V, Muschweck H, Stein HJ. Management of ERCP-related small bowel perforations: the pivotal role of physical investigation. Can J Surg. 2012;55:99-104. [Cited in This Article: ] |
| 8. | Park CH, Lee WS, Joo YE, Kim HS, Choi SK, Rew JS. Cap-assisted ERCP in patients with a Billroth II gastrectomy. Gastrointest Endosc. 2007;66:612-615. [Cited in This Article: ] |
| 9. | Cho S, Kamalaporn P, Kandel G, Kortan P, Marcon N, May G. ‘Short’ double-balloon enteroscope endoscopic retrograde cholangiopancreatography in patients with a surgically altered upper gastrointestinal tract. Can J Gastroenterol. 2011;25:615-619. [Cited in This Article: ] |
| 10. | Yamauchi H, Kida M, Okuwaki K, Miyazawa S, Iwai T, Takezawa M, Kikuchi H, Watanabe M, Imaizumi H, Koizumi W. Short-type single balloon enteroscope for endoscopic retrograde cholangiopancreatography with altered gastrointestinal anatomy. World J Gastroenterol. 2013;19:1728-1735. [Cited in This Article: ] |
| 11. | Iwai T, Kida M, Yamauchi H, Imaizumi H, Koizumi W. Short-type and conventional single-balloon enteroscopes for endoscopic retrograde cholangiopancreatography in patients with surgically altered anatomy: single-center experience. Dig Endosc. 2014;26 Suppl 2:156-163. [Cited in This Article: ] |
| 12. | Shimatani M, Takaoka M, Ikeura T, Mitsuyama T, Okazaki K. Evaluation of endoscopic retrograde cholangiopancreatography using a newly developed short-type single-balloon endoscope in patients with altered gastrointestinal anatomy. Dig Endosc. 2014;26 Suppl 2:147-155. [Cited in This Article: ] |
| 13. | Imazu H, Kanazawa K, Ikeda K, Kakutani H, Sumiyama K, Ang TL, Omar S, Tajiri H. Initial evaluation of a novel multibending backward-oblique viewing duodenoscope in endoscopic retrograde cholangiopancreatography. Endoscopy. 2012;44:99-102. [Cited in This Article: ] |
| 14. | Adler DG. Initial report of a variable stiffness duodenoscope for use during endoscopic retrograde cholangiopancreatography. J Clin Gastroenterol. 2011;45:590-592. [Cited in This Article: ] |
| 15. | Koo HC, Moon JH, Choi HJ, Ko BM, Hong SJ, Cheon YK, Cho YD, Lee JS, Lee MS, Shim CS. The utility of a multibending endoscope for selective cannulation during ERCP in patients with a Billroth II gastrectomy (with video). Gastrointest Endosc. 2009;69:931-934. [Cited in This Article: ] |
| 16. | Li G, Chen Y, Zhou X, Lv N. Early management experience of perforation after ERCP. Gastroenterol Res Pract. 2012;2012:657418. [Cited in This Article: ] |
| 17. | Azeem N, Tabibian JH, Baron TH, Orhurhu V, Rosen CB, Petersen BT, Gostout CJ, Topazian MD, Levy MJ. Use of a single-balloon enteroscope compared with variable-stiffness colonoscopes for endoscopic retrograde cholangiography in liver transplant patients with Roux-en-Y biliary anastomosis. Gastrointest Endosc. 2013;77:568-577. [Cited in This Article: ] |
| 18. | Itokawa F, Itoi T, Ishii K, Sofuni A, Moriyasu F. Single- and double-balloon enteroscopy-assisted endoscopic retrograde cholangiopancreatography in patients with Roux-en-Y plus hepaticojejunostomy anastomosis and Whipple resection. Dig Endosc. 2014;26 Suppl 2:136-143. [Cited in This Article: ] |
| 19. | Shah RJ, Smolkin M, Yen R, Ross A, Kozarek RA, Howell DA, Bakis G, Jonnalagadda SS, Al-Lehibi AA, Hardy A. A multicenter, U.S. experience of single-balloon, double-balloon, and rotational overtube-assisted enteroscopy ERCP in patients with surgically altered pancreaticobiliary anatomy (with video). Gastrointest Endosc. 2013;77:593-600. [Cited in This Article: ] |
| 20. | Moreels TG, Pelckmans PA. Comparison between double-balloon and single-balloon enteroscopy in therapeutic ERC after Roux-en-Y entero-enteric anastomosis. World J Gastrointest Endosc. 2010;2:314-317. [Cited in This Article: ] |
| 21. | Shimatani M, Takaoka M, Okazaki K. Tips for double balloon enteroscopy in patients with Roux-en-Y reconstruction and modified Child surgery. J Hepatobiliary Pancreat Sci. 2014;21:E22-E28. [Cited in This Article: ] |
| 22. | Moreels TG, Hubens GJ, Ysebaert DK, Op de Beeck B, Pelckmans PA. Diagnostic and therapeutic double-balloon enteroscopy after small bowel Roux-en-Y reconstructive surgery. Digestion. 2009;80:141-147. [Cited in This Article: ] |
| 23. | Itoi T, Ishii K, Sofuni A, Itokawa F, Tsuchiya T, Kurihara T, Tsuji S, Ikeuchi N, Umeda J, Moriyasu F. Single-balloon enteroscopy-assisted ERCP in patients with Billroth II gastrectomy or Roux-en-Y anastomosis (with video). Am J Gastroenterol. 2010;105:93-99. [Cited in This Article: ] |