Published online Aug 15, 2010. doi: 10.4291/wjgp.v1.i3.109
Revised: August 2, 2010
Accepted: August 9, 2010
Published online: August 15, 2010
We present a rare case of a 36 year old man who presented with recurrent fever but no other symptoms. Laboratory data provided no specific information for diagnosis. Abdominal ultrasonography revealed splenomegaly with multiple small hypoechoic lesions within the spleen. Computed tomography of abdomen showed a hypodense diffuse lesion. A diagnosis of isolated splenic tuberculosis was confirmed after a splenic puncture and histopathological examination.
- Citation: Zhan F, Wang CJ, Lin JZ, Zhong PJ, Qiu WZ, Lin HH, Liu YH, Zhao ZJ. Isolated splenic tuberculosis: A case report. World J Gastrointest Pathophysiol 2010; 1(3): 109-111
- URL: https://www.wjgnet.com/2150-5330/full/v1/i3/109.htm
- DOI: https://dx.doi.org/10.4291/wjgp.v1.i3.109
Splenic tuberculosis (splenic TB) is extremely rare and has no characteristic symptoms or abnormal imaging findings. Therefore, it is likely to be misdiagnosed as carcinoma of spleen, splenic abscess, lymphoma, rheumatic fever or others. Isolated splenic tuberculosis is rare although secondary involvement in miliary TB is common. The misdiagnosis rate is high if there is no tuberculosis history in other organs. In this case report, we present the presentation, diagnosis, treatment and a literature review.
A 36 year old Chinese man presented with a history of frequent fevers for 2 mo. The fever often occurred at night with body temperature ranging from 38.5°C to 40°C. He had chills before fevers and occasional shivers accompanying the fever. There was no history of throat pain, cough, sputum, chest or abdominal pain, night sweats, weight loss or anorexia. His urinary and bowel movements were normal. His medical history did not include any TB and HIV infection. He denied any history of recent foreign travel or a family history of TB and AIDS. On admission, when physically examined, his body temperature was 37.8°C and he had mild splenomegaly. Laboratory data showed that his red blood cell count was within normal limits, erythrocytic sedimentation rate (ESR) was 64 mm/h, Wildal’s reaction, tuberculous antibody test and HIV antibody reaction were all negative and C-protein level was 69.1 mg/L. Chest radiography revealed no abnormalities. Cardiac ultrasound showed no abnormality in morphology and function. An abdominal ultrasound scan showed that the thickness of the spleen was about 5.6 cm, indicating an enlarged spleen with multiple hypoechoic lesions representing solid foci, one of which was 1.0 cm × 0.8 cm with a clear boundary (Figure 1).
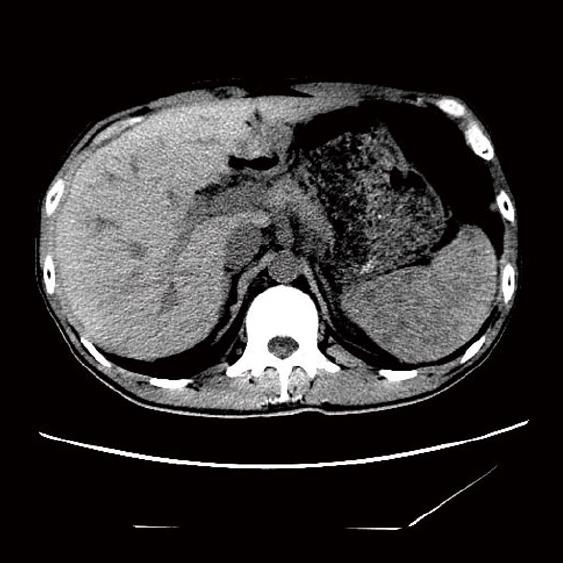
Bone marrow puncture and biopsy showed a phenomenon of animated myelosis including increased activity of granulocytic series and megakaryocytic series; pathological hematopoiesis can be seen. Computed tomography (CT) of abdomen revealed many hypodense cysts with an unclear boundary which became clear after an enhanced scanning. Fungus infection had not been ruled out because of the diffuse hypodense lesions in the spleen (Figure 2); splenic biopsy was suggested.
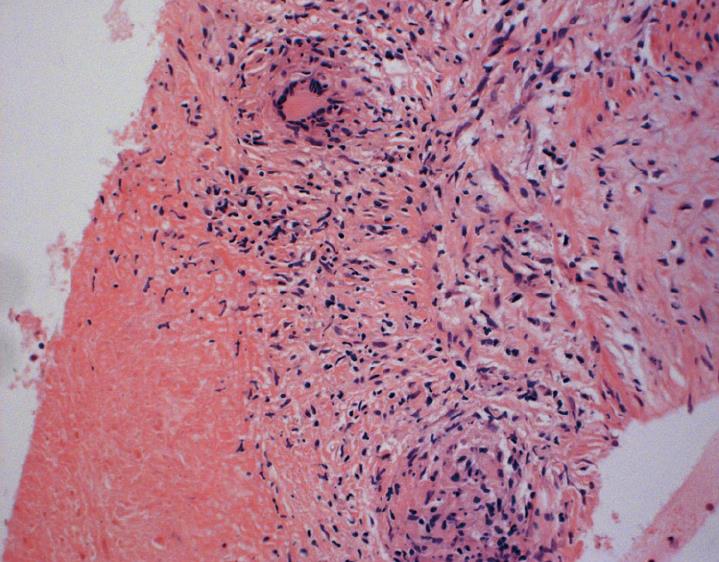
A CT-guided splenic puncture and biopsy were taken. The histopathological report showed that a granuloma nodule can be seen with large areas of caseation in the center surrounded by a variable number of Langhan’s giant cells and epithelioid cells accompanying inflammatory cells infiltration (Figure 3). Acid-fast staining found no acid-fast bacilli.
Therefore, a final diagnosis of isolated tuberculosis of the spleen was made as there was no other focus of tuberculosis detected in the lung, gastrointestinal tract or lymph nodes. Thus, the patient was started on quadruple anti-TB therapy (rimifon, streptomycin, rifapin, pyrazinamide and ethambutol). Three days later his fever and chills improved. A repeated abdominal ultrasound showed notable improvement of the lesion 6 mo later. No recurrence has been found in the last 3 years.
Tuberculosis is a multi-system disease, 90% of which locates primarily in lung, whereas isolated splenic tuberculosis, as we present here, is a rare form of extrapulmonary TB. The number of reports of the disease is less than 100 in China according to some expert’s estimates[1]. Patients with AIDS or who are otherwise immunocompetent have been reported to be at a high risk for splenic TB. Although Winternitz (1912) categorized splenic TB as a primary or secondary form, some scholars insist that all patients with splenic TB are secondary to the previous infection of tubercle bacillus in other organs[2]. In our case, the patient denied a history of TB and there was no indication of any other involvement in other sites or organs at the time of admission. There are no specific symptoms for establishing the diagnosis of splenic TB[3]. Fever was the only symptom in our case and is one of UFO (fever and pyrexia of unknown origin) as defined by Petersdorf and Beeson in 1961[4]. Helpful laboratory data includes anemia, elevated ESR, increased CPR and a positive OT test.
Ultrasound examination is simple, non-invasive and useful. There are 5 types of pathomorphological classifications for splenic TB including miliary TB, nodular TB, tuberculous spleen abscess, calcific TB and mixed type TB.
CT scan is also helpful in the diagnosis, especially for splenic abscess. However, it has its limitations. On one hand, there are many situations that may have presentations of multiple, hypodense splenic lesions on CT such as malignant lymphoma, metastatic cancer, echinococcal cysts, hemangioma or even infectious diseases due to frequent fever. Our patient may have been diagnosed with a fungus infection. Fungal splenic abscesses are being increasingly recognized, especially in immunosuppressed patients and Candida is the most involved fungus[5]. However, CT can not be suggestive of the nature of lesions in spleen. On the other hand, typical nodules on the splenic capsule are usually too small to be detected easily by CT scan[2].
Needle biopsy of the spleen is an important method of diagnosis. This can proceed by splenic aspiration puncture under image guidance. The typical manifestation is caseation along with granuloma of epitheloid cells and Langhan’s cells. Biopsys specimens from cervical lymph node, lymphonodi coeliac, hydroabdomen and pyocelia are also pathological evidence for diagnosis. In other situations, small nodules may be missed on needle biopsy and occasionally laparotomy or even splenectomy may be required. So far, histopathological examination is still an ideal method to confirm the diagnosis. However, many patients are reluctant to accept it due to its invasive nature. Therefore, it is common that patients with the disease are misdiagnosed or diagnosis is delayed.
Laparoscopy has been used in the diagnosis of splenic TB and has proved to be a minimally invasive approach avoiding unnecessary splenectomy. It is recommended for any form of splenic biopsy[6].
In a new case report of solitary splenic TB, microbiological and molecular examinations have been carried out which are helpful in etiological diagnosis[7].
Like the treatment of pulmonary tuberculosis, treatment of splenic TB must be carried out in accordance with the following principles - timely treatment in combination, regularly and properly through the whole course whether or not an operation is performed. Treatment for tuberculosis should last for more than 6 mo. Standard anti-tuberculosis medication should be taken preoperatively and postoperatively if an operation is carried out.
Peer reviewer: Chao Qin, MD, Department of Physiology, College of Medicine, University of Oklahoma, Health Sciences Center, Oklahoma City, OK 73104, United States
| 1. | Chen XZ, Peng B. Clinical diagnosis and treatment for splenic tuberculosis. Huaxi Medicine. 2008;23:114. [Cited in This Article: ] |
| 2. | Singh B, Ramdial PK, Royeppen E, Moodley J, Chetty R. Isolated splenic tuberculosis. Trop Doct. 2005;35:48-49. [Cited in This Article: ] |
| 3. | Ozgüroğlu M, Celik AF, Demir G, Aki H, Demirelli F, Mandel N, Büyükünal E, Serdengeçti S, Berkarda B. Primary splenic tuberculosis in a patient with nasal angiocentric lymphoma: mimicking metastatic tumor on abdominal CT. J Clin Gastroenterol. 1999;29:96-98. [Cited in This Article: ] |
| 4. | Ho PL, Chim CS, Yuen KY. Isolated splenic tuberculosis presenting with pyrexia of unknown origin. Scand J Infect Dis. 2000;32:700-701. [Cited in This Article: ] |
| 5. | Llenas-García J, Fernánde-Ruiz M, Caurcel L, Enguita-Valls A, Vila-Santos J, Guerra-Vales JM. Splenic abscess: A review of 22 cases in a single institution. Eur J Intern Med. 2009;20:537-539. [Cited in This Article: ] |
| 6. | Meshikhes AWN, Al-Momen SAM. Laparoscopic diagnosis of splenic tuberculosis. Surg Laparosc Endosc Tech. 2006;16:355-356. [Cited in This Article: ] |
| 7. | Fooladi AAI, Hosseini MJ, Azizi T. Splenic tuberculosis: a case report. Int J Infect Dis. 2009;13:e273-e275. [Cited in This Article: ] |