INTRODUCTION
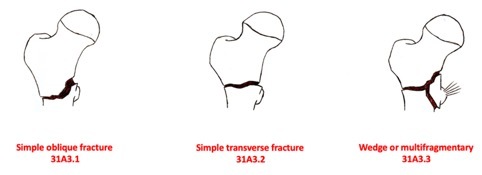
Globally, 4.5 million people are disabled from hip fractures each year,1 and the number is estimated to increase to 7.3 and up to 21.3 million by 2050.2 Reverse obliquity intertrochanteric fractures are classified by the Orthopaedic Trauma Association [OTA]/[AO] as 31A3. They account for up to one-third of all hip fractures, and 2–23% of all trochanteric fractures.3–5 This fracture type can also be divided into three subgroups: 31A3.1 are oblique fractures, 31A3.2 have a transverse fracture pattern, and 31A3.3 are multifragmentary with the fracture line involving the lesser trochanter3,4 (Fig. 1). Ideally, operative treatment of proximal femur fractures should take place within the first 24 hours.6 The choice of implant depends on the stability of the fracture pattern defined by the lateral cortical wall.7 Extramedullary devices, such as sliding hip screws, can be chosen if the lateral cortical wall is intact.8 At present, the treatment of choice for these fractures is intramedullary nailing, as it decreases soft tissue damage and permits early weight bearing.9 There are still controversies around the long-term benefits and risk of complications after fixation using short or long intramedullary nails after unstable intertrochanteric fractures.10 Multiple intramedullary nail designs have been used to manage intertrochanteric fractures.11 Cutting-out of the lag screw is the main complication of proximal femur fracture fixation.12 The strongest predictor of cutting-out in femoral nailing is tip-apex distance (TAD).13 Distances less than 25 mm are associated with a significantly decreased risk of slippage of the cephalic screw,14 while there is a very strong statistical relationship between a TAD greater than 25 mm and mobilization of the cephalic screw.15–17 Additionally, Kashigar et al.18 have reported the CalTAD using the same measurement technique of the TAD in the lateral view but a different one in the anteroposterior view (Fig. 2). In the present study, we compared three types of intramedullary devices routinely used in our department, the Zimmer Natural Nail System (ZNN CephaloMedullary Femoral Nail Zimmer; Warsaw; IN, USA), the Intertan Nail (Smith & Nephew GmbH, Marl, Germany) and the ELOS long (InTrauma, Rivoli, Italy) nails in patients treated for 31A3 proximal femur fractures. We investigated patients medical history and comorbidities, different surgical outcomes in terms of implant positioning and patients reported blood loss.
MATERIALS AND METHODS
We analysed the prospectively recorded data of all the patients admitted to the Department of Orthopaedic Clinic of the A.O.U. San Giovanni di Dio and Ruggi D’Aragona of Salerno with a proximal femur fracture from October 2018 to January 2022. Of them, only patients with a reverse oblique intertrochanteric fracture, classified by the OTA / OA as 31A3, were included. Patients underwent intramedullary nailing with various intramedullary devices used in our department: Zimmer Natural Nail System (ZNN CephaloMedullary Femoral Nail Zimmer; Warsaw; IN, USA), Intertan Nail (Smith & Nephew GmbH, Marl, Germany) and the long nail ELOS (InTrauma, Rivoli, Italy) (Fig.3, Fig.4). Based on the implant of choice, patients were allocated in three groups: Intertan, ZNN, and Elos long group. All the clinical data were stored in the files archived in the department. The results of laboratory investigations were stored in the computerized hospital database, which also contained the radiographic investigations performed before and after the surgery. Per each patient, we recorded: age, sex, type of fracture, duration of surgery, transfusions performed, hospitalization time, TAD, CalTAD, haemoglobin variation, characteristics of the nail and positioning of the same. Before surgery, patient signed an informed consent that informed about the operative procedure, functional and cosmetic expectations, and possible complications related to the surgery, consenting also to be part of any outcome research.
RESULTS
A total of 70 patients presented with a 31A3 fracture. The group included 11 males (16%) and 59 females (84%), with a mean age of 83.6 years (range 61 to 96 years). A Trigen Intertan Nail was the most frequently used intramedullary nail in 33 patients (47%), an Elos Long nail was used in 19 cases (27%), while a ZNN nail was used in 18 patients (26%). The mean time between admission and surgery was 2.5 days, with a mean Hb value of 10.5 g/dl reported preoperatively.
The Intertan group included 33 patients, 29 females (88%) and 4 males (12%), with a mean age of 83.2 years. Patients length of stay between admission to our department and surgery was 2.2 days and the mean Hb value was 11 g/dl. The most common comorbidities were chronic heart disease and hypertensive cardiomyopathy (26 patients, 79%), neurological conditions such as dementia, Alzehimer’s disease and stroke (14 patients, 42,5 %). In eight patients, cardiac and neurological comorbidities were associated with a reported diagnosis of type II diabetes mellitus (T2DM), while three patients (9%) presented with T2DM and hypercholesterolaemia. Post-operatively, the radiographic evaluation showed a mean TAD value of 18.5 mm, the CALTAD a mean of 23 mm, and the mean TADCALTAD was 41.4 mm. Patients treated with Intertan nail reported a mean 0.8 g/dl loss of Hb. Of them, 17 received blood transfusions, using a mean of 1.2 unit of blood per patient.
In 19 patients a long Elos nail was used. Of them, 13 were females (68%) and 6 males (32%) with a mean age of 83.2 years. The mean wait between admission and surgery was 2.9 days, while the mean preoperative Hb value was 10.3 g/dl. Fourteen patients (74%) had a medical history of cardiac diseases, such as chronic cardiomyopathy, hypertension, and deep vein thrombosis. Of them, two patients also suffered from T2DM (10%). Neurological comorbidities were reported in four patients (21%). From the radiographic evaluation, a mean 19.6 mm TAD was found, while the mean values of CALTAD and TADCALTAD were 21.4 mm and 41 mm. Postoperatively, the mean loss of Hb was 1 g/dl. 14 patients (74%) received a blood transfusion, finding a mean of 1,8 unit per patient.
A ZNN nail was used in the other 18 (26%) 31A3 fractures. Of them 17 (94%) were females and one male (6%), with a mean age of 84.5 years. The length of stay between admission and surgery was 2.7 days and the mean Hb value was 10 g/dl. Most patients (16.9%) suffered from chronic heart disease and hypertensive cardiomyopathy, and also from neurodegenerative diseases and T2DM. Post-operatively, the mean TAD was 20.8 mm, the mean CALTAD was 23.2 mm, and the mean TADCALTAD was 42.9 mm. The mean Hb loss was 0 g/dl, and 13 patients received blood transfusions with a mean of 3.6 units of blood per patient. The most common cause of fixation failure was the lag screw cut-out, which occurred in 2% of the patients, while intraoperative complications such as iatrogenic periprosthetic fractures occurred in just 1% of the patients. Comparisons between the groups for demographics data, comorbidities, intra- and post-operative parameters are presented in Table 1.
DISCUSSION
In the current investigation, most patients with a 31A3 fracture (33 patients, 47%) were treated with an Intertan nail with a mean time of 2.2 days from admission to surgery. Patients treated with an Intertan nail reported the lowest TAD, CALTAD, and TALCALTAD values and the lowest rate of Hb loss and blood transfusions.
Of the extracapsular fractures of the proximal femur, the 31A3 are reverse obliquity intertrochanteric femur fractures.19 They represent a challenge because of the configuration of the fracture line.20 Indeed, the fracture line usually exits the lateral cortex of the femur distal to the vastus ridge, increasing fracture instability.21 Several surgical options have been proposed to treat these fractures, including intramedullary nailing, sliding hip screws, and 95 degrees screw plates.20,22–24 From a biomechanical perspective, IM nail fixation can resist higher loading forces, and may provide greater stability than extramedullary fixation for unstable fracture patterns, including posteromedial wall involvement, insufficient lateral wall thickness, and reverse oblique type.10,23–26 Furthermore, these nails have shown a biomechanical advantage over the extramedullary fixation systems: the distance from the implant and the hip joint is reduced, diminishing the bending moment across the implant/fracture construct.25 Until 1990s, extramedullary fixation with sliding hip screws was the treatment of choice in patients with extracapsular fractures.26 Since then, two-thirds of the surgeons have been using intramedullary nails as the standard of care.27 A recent Bayesian network meta-analysis based on 36 randomized controlled trials identified short intramedullary nail as the preferable surgical method to treat intertrochanteric fracture, with lesser blood loss and high functional outcomes, according to the Harris hip score.27 Intramedullary nailing is usually performed using cephalomedullary nails, with a greater trochanter insertion of the nail, and securing the fixation system with a cephalic sliding screw, passed through the femoral neck into the femoral head.28 Based on the different designs, length, diameter, and number of cephalic screws, IM fixation systems can be secured with single, double cephalomedullary nails, and single or double integrated screws.25,28 In the current investigation, patients treated with the Intertan nail reported the best results in terms of outcomes. This IM nailing system uses 2 cephalocervical screws with an integrated mechanism, in which compression and rotational stability of the head-neck fragments are secured intraoperatively. The cannulated screw mechanism can be set in sliding mode, compression mode, and fixed angle mode as a surgeon choice based on the fracture characteristics.25,29,30 Even though many surgical strategies are available, proximal femur fractures are still associated with a high rate of postoperative complications.31 The occurrence of complications has been significantly linked with the length of stay between the admission to the department and surgery. Furthermore, a surgical delay after more than 24 hours increases the chance of perioperative complications, while the risk of mortality within the next year is 20% lower in patients operated on within 48 hours.32 The most common complication that leads to failure is mobilization of the cephalic screw, “cutting out”, frequently caused by a fracture collapse into varus.33,34 Since 1995, the distance from the tip of the cephalic screw and the apex of the femoral head, i.e. the tip to apex “TAD”, has been considered the most reliable risk factor for the screw mobilization for values lower than 25 mm.13 Another parameter that could predict the outcome of IM nailing was introduced by Kashigar et al. as CalTAD. The AP measure was the same as the TAD in the lateral view, and this value had to be added to the distance between the apex of the screw and the tangent to the medial cortex of the femoral neck in AP.18 Recently, Aicale et al. evaluated the role of another parameter in intramedullary fixation failure, defined as the “TADCalTAD”, resulting from the sum of TAD and CalTAD.35 Aicale et al. investigated the role of radiographic parameters of intramedullary devices positioning in the management of unstable intertrochanteric hip fractures, showing that a TAD and CalTAD less than 25 mm, and posited that a TADcalTAD less than 50 mm could prevent the mobilization of the lag screw and secure the construct stability.35 As a result of the fracture and its surgical treatment, most patients who suffer from hip fractures experience a significant blood loss.36 Consistent with previous works, we found a decrease in haemoglobin levels after surgical treatment of intertrochanteric fractures. However, Khan et al. reported a mean decrease in Hb levels of 3.1 g/dl, while our findings were significantly lower with a mean of 0.4 g/dL.37
This study has some limitations. Firstly, the choice of implant was not randomized. The three devices used in the study (Intertan, ELOS and ZNN) are all available in our centre and their use is certified in our country. Based on the workflow in our setting, once it had been established that an intramedullary implant was the proper surgical choice, the nail used for a given patient was determined by the availability of the implant itself, independently of the preference of the surgeon.
Furthermore, patients were lost to the long-term follow up. Our department policy provides short-term follow up and then discharges patients to the care of their general practitioner, who oversees the arrangement of long-term orthopaedics follow-up. We recognize the limited significancy of the statistical analysis. Indeed, a power analysis could not be performed because of the small number of patients included. Further studies are needed to establish the gold standard of treatment for reverse oblique intertrochanteric fractures.
CONCLUSION
Patients treated with an Intertan nail reported the lowest TAD, CALTAD, and TALCALTAD mean radiographic values, and the lowest rate of Hb loss and blood transfusions.
Acknowledgments
None
Author contributions
Author contributions: the authors contributed equally
Conflict of interest
The authors declare that they have no conflict of interest
Funding
None
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.