Published online May 8, 2015. doi: 10.5409/wjcp.v4.i2.19
Peer-review started: November 4, 2014
First decision: November 27, 2014
Revised: February 12, 2015
Accepted: March 5, 2015
Article in press: March 9, 2015
Published online: May 8, 2015
Acute appendicitis is one of the most common indications for abdominal surgery in pediatrics with peak incidence in the second decade of life. Acute appendicitis in the first years of life is an uncommon event. The clinical presentation is often varied and the diagnosis may be overshadowed by other medical conditions. Gastroenteritis is the most common misdiagnosis, with a history of diarrhea present in 33% to 41% of patients. Pain is the most common presenting symptom in children less than 5 years old, followed by vomiting, fever, anorexia and diarrhea. The most common physical sign is focal tenderness (61% of the patients) followed by guarding (55%), diffuse tenderness (39%), rebound (32%), and mass (6%). Neonatal appendicitis is a very rare disease with high mortality; presenting symptoms are nonspecific with abdominal distension representing the main clinical presentation. The younger the patient, the earlier perforation occurs: 70% of patients less than 3 years develop a perforation within 48 h of onset of symptoms. A timely diagnosis reduces the risk of complications. We highlight the epidemiology, pathophysiology, clinical signs and laboratory clues of appendicitis in young children and suggest an algorithm for early diagnosis.
Core tip: Acute appendicitis in the first years of life is an uncommon event but with a high incidence of early perforation the younger the patient. We highlight the epidemiology, pathophysiology, clinical signs, and laboratory clues of appendicitis in young children. The challenge for the practitioner is to perform a timely diagnosis of acute appendicitis in first years of life before complications occur.
- Citation: Marzuillo P, Germani C, Krauss BS, Barbi E. Appendicitis in children less than five years old: A challenge for the general practitioner. World J Clin Pediatr 2015; 4(2): 19-24
- URL: https://www.wjgnet.com/2219-2808/full/v4/i2/19.htm
- DOI: https://dx.doi.org/10.5409/wjcp.v4.i2.19
Acute appendicitis has the highest incidence during the second decade of life[1], and represents a frequent indication for abdominal surgery in pediatrics[2]. It is more common in males than in females (ratio 1.4:1)[2]. While up to 33% of affected children may present not distinct abdominal pain with consecutive pain localization in the right lower quadrant, nausea and vomiting, young children could show atypical or delayed symptoms presentation[3-5]. When the diagnosis is performed, perforation could be already present in 30%-75% of children, with young children being at higher risk[6]. Perforated appendicitis increases the morbidity with intra-abdominal abscess being an important complication[7]. In young children, appendicitis is an uncommon event with a varied presentation and complications that can develop rapidly[8,9]. A timely diagnosis although necessary can be difficult, representing a challenge for the physician.
In a study over a 12-year period, 1836 pediatric appendectomies were reviewed. Three hundred and twenty (17%) patients were under 5 years of age, 103 (5%) were less than 3 years, with only 7 patients (0.38%) younger than 1 year[7]. Perforation was more frequent in young children (the perforation rate was 86% in children less than 1 year of age, 74% between 1 and 1.9 years, 60% between 2 and 2.9 years, 64% between 3 and 3.9 years, and 49% between 4 and 4.9 years), while the rate in older patients was 5%[7]. Seven patients under 1 year of age were included so that the statistical relevance of the differences in the perforation rate of the different age groups would be limited[7]. Moreover, male patients present more risk of perforation than female patients also if the symptoms have a similar duration[10].
A single pediatric center study over a 28-year period reported a similar rate of appendicitis in patients under 1 year of age (0.34%) and 2.3% in patients under 3 years[11].
Andersen et al[9], in a cohort of Danish children, reported an annual incidence of 2.22/10000 among boys less than 4 years and 1.82/10000 among girls less than 4 years with a perforation rate of 0.64 and 0.62, respectively. The annual incidence among 10-19 years old boys and girls was 22/10000 and 18/10000 respectively, with a perforation rate of one third the rate of young children[9].
The risk of perforation increases with diagnostic delay. In children 5-12 years old, if the diagnosis is made in less than 24 h from the outbreak of symptoms, the reported perforation rate is 7%, if between 24-48 h 38%, and if more than 48 h 98%[8]. In patients < 3 years, the perforation rate is high (70%), even if the time to diagnosis is less than 48 h[4].
A timely diagnosis is more difficult in toddlers because of presentation to emergency department delayed since the outbreak of symptoms of 1.6 d for patients less than 5 years[7], and 3 d in patients less than 3 years[11].
Differences in the appendicitis clinical presentation could be explained by age-related variations in appendiceal anatomy and development. In the neonatal period, the appendix is 4.5 cm long reaching the length of 9.5 cm in adults[12]. Acute appendicitis is rare in neonates because they present a funnel-shaped appendix[13,14], have liquid diet, supine posture, low frequency of gastrointestinal and upper respiratory tract infections[15]. Furthermore, there is evidence that breast-feeding could reduce the risk of appendicitis[16].
Between 1-2 years of age, the appendix becomes similar to that of an adult and the susceptibility to inflammation increases. Lymphoid follicle hyperplasia and follicular size gradually increase with the major expression during adolescence, corresponding to the period of the highest rate of appendicitis[1]. Young children have an undeveloped omentum that is not able to limit the purulent material effusion from a perforation[17]. For this reason, diffuse peritonitis following a perforation is more likely in young children[18]. The mobility of fetal and infant appendices is accentuated and the probability of appendix to be fixed by mesenteric connections to the cecum, ascending colon, or abdominal wall is lower[19]. This could explain why the incidence of localized abscesses in young children is infrequent.
In preverbal toddlers and preschoolers, the anamnesis about the pain is difficult to examine[20]. In preverbal children, clinicians need to relay on the physical examination and on detecting contingent signs of pathology evaluating how children eat, move around, play, sleep, and defecate[20]. Many children, in particular young children, can be easily influenced. Even though their conflicting significances, questions such as “Does it hurt here” and “This feels fine, right” may lead to the same positive answer[20]. Abdominal pain usually begins as vague mid-abdominal or periumbilical pain migrating to the right lower quadrant during an interval of hours to days, and many school-aged children can accurately report and localize their pain movement. However, young children may not be able to describe accurately their symptoms, and the clinicians could locate the pain exclusively asking the children to show the painful abdominal point[20].
Pain is the most frequent presenting symptom in children less than 5 years old. In a cohort of 120 patients less than 5 years, 94% presented with pain, 83% with vomiting, 80% with fever, 74% with refusal to eat, and 32% with diarrhea[21]. When the data was restricted to children less than 3 years, vomiting, fever and diarrhea were more frequent[11]. If the appendicitis is non-perforated the most common physical sign is localized tenderness (61%) followed by guarding (55%), diffuse tenderness (39%), rebound (32%), and mass (6%)[21]. If the appendicitis is perforated, the most frequent sign is the guarding (79%) followed by diffuse tenderness (62%), rebound (39%), localized tenderness (33%), mass (9%), and rigidity (7%)[21].
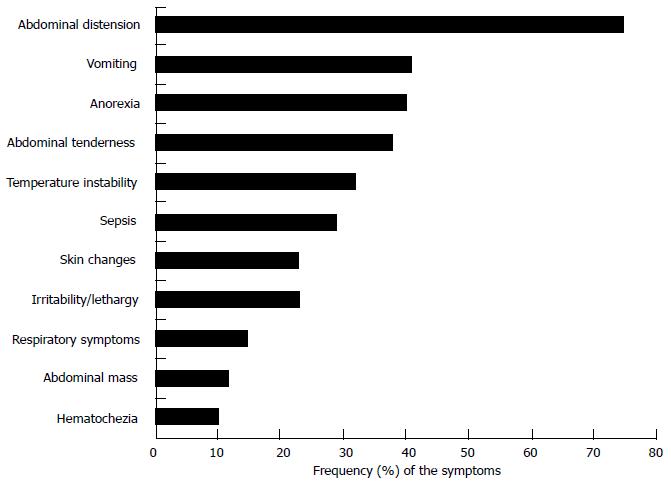
In the neonatal period, the signs and symptoms are nonspecific with irritability or lethargy (22%), abdominal distension (60%-90%), and vomiting (59%)[15,22]. Other symptoms include a palpable mass (20%-40%)[15], abdominal wall cellulitis (12%-16%), hypotension, hypothermia, and respiratory distress[22-25]. The most common clinical presenting signs and symptoms are reported in Figure 1[24].
White blood cell count (WBC) and C-reactive protein (CRP) are commonly used when an acute appendicitis is suspected. Conventional WBC count presents both low sensitivity and specificity, in fact it could increase in 70% of the patients presenting abdominal pain for causes different from appendicitis[26]. A high WBC count or a left shift (represented by higher than 80% polymorphonuclear cells along with bands) has good sensitivity (79%), while the coexistence of both positive WBC count and left shift present the greatest specificity (94%)[27]. The sensitivity and specificity of WBC counts range from 70%-80% and 60%-68%, respectively[28]. Up to 20% of children with pathologically proven appendicitis present a WBC in the normal range[29], while the leukocyte response declines in children younger than 5 years old with appendicitis[30].
CRP is more specific than WBC count, even if in the early stage of acute appendicitis the sensitivity is lower[26,31]. The reported sensitivity and specificity are of 57% and 87% respectively[28]. CRP presents higher sensitivity in discovering appendiceal perforation and abscess formation[26,31]. Recently, it has been demonstrated that the use of both WBC count and CRP may lead to enhanced negative predictive value[6,32]. Yokoyama et al[33] showed as indicative of surgical intervention a CRP cut-off value of 4.95 mg/dL (sensitivity 84% and specificity 76%). Procalcitonin is not helpful in the acute appendicitis diagnosis presenting a diagnostic accuracy lower than CRP and WBC[31]. When a complicated appendicitis is present the pooled procalcitonin sensitivity and specificity are 62% and 94%, respectively[31].
Computed tomography (CT) has been considered the radiological gold standard to confirm clinical suspicion of appendicitis with high sensitivity and specificity[34,35]. Repeated CT carries an established risk of increased incidence of cancer in children and its use should therefore be limited to clear indications with a well-defined risk to benefit ratio[36]. Less operator dependence, easier visualization of retrocecal appendix, less interference of bowel gas, obesity, or patient pain and tenderness with image quality are included among CT advantages. For these reasons, CT remains the most common primary imaging method before appendectomy in children[25,37]. To increase sensitivity of diagnosis but decrease radiation exposure, CT used in conjunction with equivocal ultrasonography (US) has been recommended as the most judicious diagnostic imaging pathway[38].
Using US for the acute appendicitis diagnosis is convenient and safe, but is highly operator dependent with a wide reported sensitivity range (44%-100%)[34,36,39]. There is evidence that the diagnostic accuracy can be improved[40] using specific US criteria and using repeated scans[41].
Magnetic resonance imaging (MRI) may also be used in young children[42]. Diagnostic imaging with US selectively followed by MRI is possible and comparable to CT, without differences in time to antibiotic administration and appendectomy, negative appendectomy and perforation rate, or length of stay[43]. Aspelund et al[43] showed an high US-MRI pathway specificity (99%) with a sensibility of 100%.
Appendicitis in young children is a diagnostic challenge. In a case series of 27 children less than 3 years, 67% had been visited by one or more clinicians without the diagnosis of acute appendicitis had been performed[11]. At this age the diagnosis of appendicitis may be hided by other medical conditions (Table 1). Gastroenteritis is the most common misdiagnosis (possible red flags to suspect appendicitis mimicking a gastroenteritis are shown in Table 1), in fact diarrhea may be present in 33%-41% of patients[4,26]. Importantly, as prior infective diseases may play a role in the physiopathology of acute appendicitis[54], diagnosis of a gastrointestinal, respiratory or urinary infection, should not rule out concomitant acute appendicitis[55].
| Condition | Diagnostic clues |
| Gastroenteritis | Continuous abdominal pain |
| Poor clinical condition with mild or no dehydration, continuous, focal abdominal pain, and lack of movement in infants and young children distinguishes appendicitis from gastroenteritis Acute appendicitis is more common during viral epidemics and bacterial gastroenteritis[44] | |
| Upper respiratory tract infection1 | The presence of concomitant signs of upper respiratory infection are common in toddlers and does not rule out the possibility of appendicitis |
| Pneumonia | Basal pneumonia may mimic appendicitis pain[45] Simultaneous pneumococcal pneumonia and appendicitis is well reported in the literature[46] |
| Sepsis | An acute appendicitis should be suspected and ruled out in any case of sepsis associated with abdominal pain and or abdominal tenderness[47] |
| Urinary tract infection | Peritoneal inflammation may cause voiding disturbances and bladder symptoms[48] |
| Blunt abdominal trauma | Acute appendicitis may be associated with blunt abdominal trauma[49-51] |
| Intussception | Abdominal US is highly operator dependent In presence of fever, localized pain and guarding in infants and young children, appendicitis should be ruled out[52] |
| NEC | With a history of NEC outside prematurity and signs of abdominal cellulitis, neonatal appendicitis should be ruled out[53] |
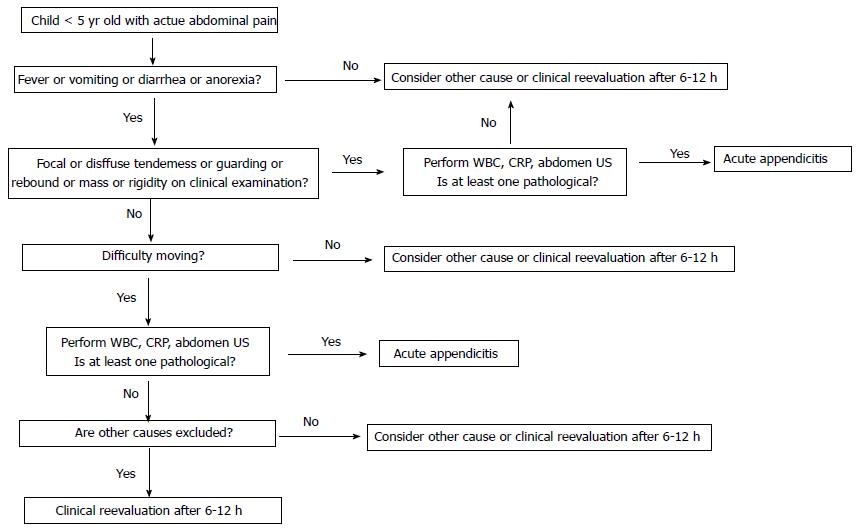
A timely diagnosis of acute appendicitis in young children is a challenge due to the rarity of the disease, the varied presentation, and the rapid development of complications. A high level of suspicion and the knowledge of specific red flags can increase diagnostic skill. We present a diagnostic algorithm (Figure 2) that could be used to assess acute appendicitis in young children, optimizing diagnostic sources and limiting the CT use.
P- Reviewer: Ince V, Kapischke M, Radojcic BS S- Editor: Gong XM L- Editor: A E- Editor: Wu HL
| 1. | Addiss DG, Shaffer N, Fowler BS, Tauxe RV. The epidemiology of appendicitis and appendectomy in the United States. Am J Epidemiol. 1990;132:910-925. [PubMed] [Cited in This Article: ] |
| 2. | Hall MJ, DeFrances CJ, Williams SN, Golosinskiy A, Schwartzman A. National Hospital Discharge Survey: 2007 summary. Natl Health Stat Report. 2010;1-20, 24. [PubMed] [Cited in This Article: ] |
| 3. | Davenport M. Acute abdominal pain in children. BMJ. 1996;312:498-501. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 27] [Cited by in F6Publishing: 29] [Article Influence: 1.0] [Reference Citation Analysis (1)] |
| 4. | Horwitz JR, Gursoy M, Jaksic T, Lally KP. Importance of diarrhea as a presenting symptom of appendicitis in very young children. Am J Surg. 1997;173:80-82. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 72] [Cited by in F6Publishing: 76] [Article Influence: 2.8] [Reference Citation Analysis (1)] |
| 5. | Irish MS, Pearl RH, Caty MG, Glick PL. The approach to common abdominal diagnosis in infants and children. Pediatr Clin North Am. 1998;45:729-772. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 50] [Cited by in F6Publishing: 52] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 6. | Stefanutti G, Ghirardo V, Gamba P. Inflammatory markers for acute appendicitis in children: are they helpful. J Pediatr Surg. 2007;42:773-776. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 43] [Cited by in F6Publishing: 45] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 7. | Bansal S, Banever GT, Karrer FM, Partrick DA. Appendicitis in children less than 5 years old: influence of age on presentation and outcome. Am J Surg. 2012;204:1031-1035; discussion 1035. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 59] [Cited by in F6Publishing: 57] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 8. | Rothrock SG, Pagane J. Acute appendicitis in children: emergency department diagnosis and management. Ann Emerg Med. 2000;36:39-51. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 226] [Cited by in F6Publishing: 200] [Article Influence: 8.3] [Reference Citation Analysis (1)] |
| 9. | Andersen SB, Paerregaard A, Larsen K. Changes in the epidemiology of acute appendicitis and appendectomy in Danish children 1996-2004. Eur J Pediatr Surg. 2009;19:286-289. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 22] [Cited by in F6Publishing: 22] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 10. | Augustin T, Cagir B, Vandermeer TJ. Characteristics of perforated appendicitis: effect of delay is confounded by age and gender. J Gastrointest Surg. 2011;15:1223-1231. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 55] [Cited by in F6Publishing: 55] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 11. | Alloo J, Gerstle T, Shilyansky J, Ein SH. Appendicitis in children less than 3 years of age: a 28-year review. Pediatr Surg Int. 2004;19:777-779. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 75] [Cited by in F6Publishing: 72] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 12. | Buschard K, Kjaeldgaard A. Investigation and analysis of the position, fixation, length and embryology of the vermiform appendix. Acta Chir Scand. 1973;139:293-298. [PubMed] [Cited in This Article: ] |
| 13. | Collins DC. 71,000 human appendix specimens. a final report, summarizing forty years’ study. Am J Proctol. 1963;14:265-281. [PubMed] [Cited in This Article: ] |
| 14. | Karaman A, Cavuşoğlu YH, Karaman I, Cakmak O. Seven cases of neonatal appendicitis with a review of the English language literature of the last century. Pediatr Surg Int. 2003;19:707-709. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 52] [Cited by in F6Publishing: 57] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 15. | Schorlemmer GR, Herbst CA. Perforated neonatal appendicitis. South Med J. 1983;76:536-537. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 24] [Cited by in F6Publishing: 28] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 16. | Alves JG, Figueiroa JN, Barros I. Does breast feeding provide protection against acute appendicitis A case-control study. Trop Doct. 2008;38:235-236. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 17. | Rasmussen OO, Hoffmann J. Assessment of the reliability of the symptoms and signs of acute appendicitis. J R Coll Surg Edinb. 1991;36:372-377. [PubMed] [Cited in This Article: ] |
| 18. | Gilbert SR, Emmens RW, Putnam TC. Appendicitis in children. Surg Gynecol Obstet. 1985;161:261-265. [PubMed] [Cited in This Article: ] |
| 19. | Maisel H. The position of the human vermiform appendix in fetal and adult age groups. Anat Rec. 1960;136:385-389. [DOI] [Cited in This Article: ] [Cited by in Crossref: 23] [Cited by in F6Publishing: 23] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 20. | Bundy DG, Byerley JS, Liles EA, Perrin EM, Katznelson J, Rice HE. Does this child have appendicitis. JAMA. 2007;298:438-451. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 209] [Cited by in F6Publishing: 219] [Article Influence: 12.9] [Reference Citation Analysis (0)] |
| 21. | Nance ML, Adamson WT, Hedrick HL. Appendicitis in the young child: a continuing diagnostic challenge. Pediatr Emerg Care. 2000;16:160-162. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 120] [Cited by in F6Publishing: 123] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 22. | Buntain WL, Krempe RE, Kraft JW. Neonatal appendicitis. Ala J Med Sci. 1984;21:295-299. [PubMed] [Cited in This Article: ] |
| 23. | Bryant LR, Trinkle JK, Noonan JA, Nighbert EJ. Appendicitis and appendiceal perforation in neonates. Am Surg. 1970;36:523-525. [PubMed] [Cited in This Article: ] |
| 24. | Schwartz KL, Gilad E, Sigalet D, Yu W, Wong AL. Neonatal acute appendicitis: a proposed algorithm for timely diagnosis. J Pediatr Surg. 2011;46:2060-2064. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 47] [Cited by in F6Publishing: 51] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 25. | Saito JM, Yan Y, Evashwick TW, Warner BW, Tarr PI. Use and accuracy of diagnostic imaging by hospital type in pediatric appendicitis. Pediatrics. 2013;131:e37-e44. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 83] [Cited by in F6Publishing: 85] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 26. | Andersson RE. Meta-analysis of the clinical and laboratory diagnosis of appendicitis. Br J Surg. 2004;91:28-37. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 308] [Cited by in F6Publishing: 286] [Article Influence: 14.3] [Reference Citation Analysis (0)] |
| 27. | Wang LT, Prentiss KA, Simon JZ, Doody DP, Ryan DP. The use of white blood cell count and left shift in the diagnosis of appendicitis in children. Pediatr Emerg Care. 2007;23:69-76. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 61] [Cited by in F6Publishing: 60] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 28. | Bates MF, Khander A, Steigman SA, Tracy TF, Luks FI. Use of white blood cell count and negative appendectomy rate. Pediatrics. 2014;133:e39-e44. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 32] [Cited by in F6Publishing: 33] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 29. | Grönroos JM. Do normal leucocyte count and C-reactive protein value exclude acute appendicitis in children. Acta Paediatr. 2001;90:649-651. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 36] [Cited by in F6Publishing: 25] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 30. | Paajanen H, Mansikka A, Laato M, Kettunen J, Kostiainen S. Are serum inflammatory markers age dependent in acute appendicitis. J Am Coll Surg. 1997;184:303-308. [PubMed] [Cited in This Article: ] |
| 31. | Yu CW, Juan LI, Wu MH, Shen CJ, Wu JY, Lee CC. Systematic review and meta-analysis of the diagnostic accuracy of procalcitonin, C-reactive protein and white blood cell count for suspected acute appendicitis. Br J Surg. 2013;100:322-329. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 166] [Cited by in F6Publishing: 178] [Article Influence: 14.8] [Reference Citation Analysis (0)] |
| 32. | Sack U, Biereder B, Elouahidi T, Bauer K, Keller T, Tröbs RB. Diagnostic value of blood inflammatory markers for detection of acute appendicitis in children. BMC Surg. 2006;6:15. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 76] [Cited by in F6Publishing: 82] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 33. | Yokoyama S, Takifuji K, Hotta T, Matsuda K, Nasu T, Nakamori M, Hirabayashi N, Kinoshita H, Yamaue H. C-Reactive protein is an independent surgical indication marker for appendicitis: a retrospective study. World J Emerg Surg. 2009;4:36. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 22] [Cited by in F6Publishing: 24] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 34. | Garcia Peña BM, Mandl KD, Kraus SJ, Fischer AC, Fleisher GR, Lund DP, Taylor GA. Ultrasonography and limited computed tomography in the diagnosis and management of appendicitis in children. JAMA. 1999;282:1041-1046. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 242] [Cited by in F6Publishing: 245] [Article Influence: 9.8] [Reference Citation Analysis (0)] |
| 35. | Hernanz-Schulman M. CT and US in the diagnosis of appendicitis: an argument for CT. Radiology. 2010;255:3-7. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 85] [Cited by in F6Publishing: 89] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 36. | Doria AS, Moineddin R, Kellenberger CJ, Epelman M, Beyene J, Schuh S, Babyn PS, Dick PT. US or CT for Diagnosis of Appendicitis in Children and Adults A Meta-Analysis. Radiology. 2006;241:83-94. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 486] [Cited by in F6Publishing: 448] [Article Influence: 24.9] [Reference Citation Analysis (0)] |
| 37. | Raval MV, Deans KJ, Rangel SJ, Kelleher KJ, Moss RL. Factors associated with imaging modality choice in children with appendicitis. J Surg Res. 2012;177:131-136. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 23] [Cited by in F6Publishing: 20] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 38. | Krishnamoorthi R, Ramarajan N, Wang NE, Newman B, Rubesova E, Mueller CM, Barth RA. Effectiveness of a staged US and CT protocol for the diagnosis of pediatric appendicitis: reducing radiation exposure in the age of ALARA. Radiology. 2011;259:231-239. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 146] [Cited by in F6Publishing: 151] [Article Influence: 11.6] [Reference Citation Analysis (0)] |
| 39. | Lowe LH, Penney MW, Stein SM, Heller RM, Neblett WW, Shyr Y, Hernanz-Schulman M. Unenhanced limited CT of the abdomen in the diagnosis of appendicitis in children: comparison with sonography. AJR Am J Roentgenol. 2001;176:31-35. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 83] [Cited by in F6Publishing: 84] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 40. | Goldin AB, Khanna P, Thapa M, McBroom JA, Garrison MM, Parisi MT. Revised ultrasound criteria for appendicitis in children improve diagnostic accuracy. Pediatr Radiol. 2011;41:993-999. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 90] [Cited by in F6Publishing: 83] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 41. | Dilley A, Wesson D, Munden M, Hicks J, Brandt M, Minifee P, Nuchtern J. The impact of ultrasound examinations on the management of children with suspected appendicitis: a 3-year analysis. J Pediatr Surg. 2001;36:303-308. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 62] [Cited by in F6Publishing: 61] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 42. | Cobben L, Groot I, Kingma L, Coerkamp E, Puylaert J, Blickman J. A simple MRI protocol in patients with clinically suspected appendicitis: results in 138 patients and effect on outcome of appendectomy. Eur Radiol. 2009;19:1175-1183. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 101] [Cited by in F6Publishing: 82] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 43. | Aspelund G, Fingeret A, Gross E, Kessler D, Keung C, Thirumoorthi A, Oh PS, Behr G, Chen S, Lampl B. Ultrasonography/MRI versus CT for diagnosing appendicitis. Pediatrics. 2014;133:586-593. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 107] [Cited by in F6Publishing: 109] [Article Influence: 10.9] [Reference Citation Analysis (0)] |
| 44. | Larner AJ. The aetiology of appendicitis. Br J Hosp Med. 1988;39:540-542. [PubMed] [Cited in This Article: ] |
| 45. | Vendargon S, Wong PS, Tan KK. Pneumonia presenting as acute abdomen in children: a report of three cases. Med J Malaysia. 2000;55:520-523. [PubMed] [Cited in This Article: ] |
| 46. | Dursun I, Kiziltan MY, Bozkaya D, Aygün A, Gücüyener K. Pneumococcal pneumonia preceding appendicitis in a child. Eur J Pediatr. 2004;163:500. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in F6Publishing: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 47. | Crocco S, Pederiva F, Zanelli E, Scarpa M, Barbi E, Ventura A. Stump appendicitis seven years after appendectomy. APSP J Case Rep. 2013;4:33. [PubMed] [Cited in This Article: ] |
| 48. | Place RC. Acute urinary retention in a 9-year-old child: an atypical presentation of acute appendicitis. J Emerg Med. 2006;31:173-175. [PubMed] [Cited in This Article: ] |
| 49. | Toumi Z, Chan A, Hadfield MB, Hulton NR. Systematic review of blunt abdominal trauma as a cause of acute appendicitis. Ann R Coll Surg Engl. 2010;92:477-482. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 18] [Cited by in F6Publishing: 21] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 50. | Amir A, Amir L, Waisman Y. Acute appendicitis after a blunt perineal trauma: an illustrative case. Pediatr Emerg Care. 2009;25:184-185. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 51. | Ahmed ST, Ranjan R, Saha SB, Singh B. Traumatic appendicitis misdiagnosed as a case of haemoperitoneum. BMJ Case Rep. 2014;pii:bcr2013202082. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 52. | Blevrakis E, Tampakaki Z, Dimopoulou A, Bakantaki A, Blevrakis E, Sakellaris G. Small bowel intussusception with pelvic plastron secondary to acute appendicitis in child. J Pediatr Surg. 2010;45:E5-E7. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 53. | Stiefel D, Stallmach T, Sacher P. Acute appendicitis in neonates: complication or morbus sui generis. Pediatr Surg Int. 1998;14:122-123. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 28] [Cited by in F6Publishing: 33] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 54. | Singer JI, Losek JD. Grunting respirations: chest or abdominal pathology. Pediatr Emerg Care. 1992;8:354-358. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 10] [Cited by in F6Publishing: 10] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 55. | Paul SP, Banks T, Fitz-John L. Abdominal pain in children with pneumonia. Nurs Times. 2012;108:21. [PubMed] [Cited in This Article: ] |