Published online May 8, 2016. doi: 10.5409/wjcp.v5.i2.182
Peer-review started: August 16, 2015
First decision: September 17, 2015
Revised: December 15, 2015
Accepted: January 5, 2016
Article in press: January 7, 2016
Published online: May 8, 2016
Several clinical guidelines for the management of infants with severe neonatal hyperbilirubinemia recommend immediate exchange transfusion (ET) when the risk or presence of acute bilirubin encephalopathy is established in order to prevent chronic bilirubin encephalopathy or kernicterus. However, the literature is sparse concerning the interval between the time the decision for ET is made and the actual initiation of ET, especially in low- and middle-income countries (LMICs) with significant resource constraints but high rates of ET. This paper explores the various stages and potential delays during this interval in complying with the requirement for immediate ET for the affected infants, based on the available evidence from LMICs. The vital role of intensive phototherapy, efficient laboratory and logistical support, and clinical expertise for ET are highlighted. The challenges in securing informed parental consent, especially on religious grounds, and meeting the financial burden of this emergency procedure to facilitate timely ET are examined. Secondary delays arising from post-treatment bilirubin rebound with intensive phototherapy or ET are also discussed. These potential delays can compromise the effectiveness of ET and should provide additional impetus to curtail avoidable ET in LMICs.
Core tip: Exchange transfusion (ET) is effective in preventing bilirubin-induced neurologic dysfunction in infants with severe hyperbilirubinemia. However, the timely initiation of this emergency procedure is frequently constrained by delays at various critical stages from the time the decision to commence ET is made and when ET is actually conducted. These delays must be carefully identified and appropriately addressed in each clinical setting to minimize their adverse impact in the provision of effective ET in low- and middle-income countries. Intensive phototherapy should also be considered a priority during this interval to minimize avoidable ETs.
- Citation: Mabogunje CA, Olaifa SM, Olusanya BO. Facility-based constraints to exchange transfusions for neonatal hyperbilirubinemia in resource-limited settings. World J Clin Pediatr 2016; 5(2): 182-190
- URL: https://www.wjgnet.com/2219-2808/full/v5/i2/182.htm
- DOI: https://dx.doi.org/10.5409/wjcp.v5.i2.182
Exchange transfusion (ET) is a definitive and effective therapy for preventing kernicterus, usually where intensive phototherapy is either lacking or proves to be ineffective in arresting rapidly rising bilirubin levels in infants with severe neonatal hyperbilirubinemia or symptoms of acute bilirubin encephalopathy (ABE)[1,2]. The procedure is not risk-free however, as it may be associated with such complications as sepsis, electrolyte imbalance, air embolism, portal vein thrombosis, cardiac overload, thrombophlebitis, thrombocytopenia, necrotizing enterocolitis, and the transmission of blood-borne diseases, even in settings with advanced clinical care[3-6]. Several guidelines for the management of neonatal hyperbilirubinemia in developed and developing countries recommend immediate ET for infants with, or at risk of, acute or chronic bilirubin encephalopathy[2,7,8]. This is primarily because the timing of ET vis-à-vis the complex interaction between the level and duration of exposure of the neuronal cells to unbound bilirubin crucially affects intervention outcomes[9]. However, this timely goal is rarely achieved in many low- and middle-income countries (LMICs), where excessive rates of ET persist as a result of weaknesses in the health-care delivery system in these locations[10-13]. For example, it is not uncommon for a severely jaundiced infant to first present in a hospital not adequately equipped to provide emergency care, including ET, and are thus subsequently referred to a better equipped hospital[11,14]. This experience often results in considerable delay in providing ET[15]. Several reports also suggest that delays of up to 24 h from the time the decision to carry out ET is made and when treatment is received by the affected infant in the same hospital are not uncommon[6,14,15], compared to the estimated 4-6 h in developed countries[16]. Such delays are likely to account for the high incidence of bilirubin-induced neurological dysfunctions (ABE and kernicterus) and the associated devastating consequences in many LMICs[15,17,18]. This paper, therefore, sets out to identify commonly reported facility-based challenges in providing timely and effective ET in hospitals designated for such an emergency procedure in LMICs.
We conducted an electronic search of PubMed, Scopus, Ovid EMBASE, and the Cumulative Index to Nursing and Allied Health Literature to retrieve articles published between January 1990 and June 2015 on exchange transfusion for hyperbilirubinemia in resource-limited countries. The search terms used were “neonatal hyperbilirubinemia”, “neonatal jaundice”, “exchange transfusion”, “bilirubin encephalopathy”, and/or “kernicterus”. The terms “resource-limited”, “resource-constrained”, and “resource-poor” countries are used interchangeably to refer to the 91 LMICs with a per capita gross national income (GNI) of ≤ $6000 using the Human Development Report 2013 published by the United Nations Development Program as previously reported (Table 1)[8,15]. These countries have an average life expectancy of 63.3 years and a median national frequency of 8.2% (inter-quartile range: 3.3%-14.6%) for glucose 6-phospho-dehydrogenase (G-6-PD) deficiency. Only articles or reports published from these 91 countries were reviewed. As this paper was designed as a narrative review, no systematic evaluation of the retrieved articles and reports was planned.
| SN | Country | Region | Life expectancy (yr) | GNI per capita ($) | Annual live births ('000) | Hospital delivery (%) | G6PD deficiency freq |
| 1 | Afghanistan | SOA | 49.1 | 1000 | 1408 | 33 | 7.4 |
| 2 | Angola | SSA | 51.5 | 4812 | 803 | 46 | 15.3 |
| 3 | Armenia | ECA | 74.4 | 5540 | 47 | 99 | - |
| 4 | Bangladesh | SOA | 69.2 | 1785 | 3016 | 29 | 3.8 |
| 5 | Belize | LAC | 76.3 | 5327 | 8 | 89 | 2.2 |
| 6 | Benin | SSA | 56.5 | 1439 | 356 | 87 | 23.0 |
| 7 | Bhutan | SOA | 67.6 | 5246 | 15 | 63 | 5.9 |
| 8 | Bolivia, Plurinational State of | LAC | 66.9 | 4444 | 264 | 68 | 0.2 |
| 9 | Burkina Faso | SSA | 55.9 | 1202 | 730 | 66 | 9.4 |
| 10 | Burundi | SSA | 50.9 | 544 | 288 | 60 | 7.2 |
| 11 | Cambodia | EAP | 63.6 | 2095 | 317 | 54 | 14.3 |
| 12 | Cameroon | SSA | 52.1 | 2114 | 716 | 61 | 12.5 |
| 13 | Cape Verde | SSA | 74.3 | 3609 | 10 | 76 | 0.1 |
| 14 | Central African Republic | SSA | 49.1 | 722 | 156 | 53 | 9.2 |
| 15 | Chad | SSA | 49.9 | 1258 | 511 | 16 | 13.4 |
| 16 | Comoros | SSA | 61.5 | 986 | 28 | 14.0 | |
| 17 | Congo | SSA | 57.8 | 2934 | 145 | 92 | 22.5 |
| 18 | Congo, Democratic Republic of the | SSA | 48.7 | 319 | 2912 | 75 | 19.2 |
| 19 | Côte d’Ivoire | SSA | 56.0 | 1593 | 679 | 57 | 15.0 |
| 20 | Cuba | LAC | 79.3 | 5539 | 110 | 100 | - |
| 21 | Djibouti | MEN | 58.3 | 2350 | 26 | 87 | 0.8 |
| 22 | Egypt | MEN | 73.5 | 5401 | 1886 | 72 | - |
| 23 | El Salvador | LAC | 72.4 | 5915 | 126 | 85 | 3.3 |
| 24 | Eritrea | SSA | 62.0 | 531 | 193 | 26 | 4.0 |
| 25 | Ethiopia | SSA | 59.7 | 1017 | 2613 | 10 | 1.0 |
| 26 | Fiji | EAP | 69.4 | 4087 | 18 | - | |
| 27 | Gambia | SSA | 58.8 | 1731 | 67 | 56 | 11.5 |
| 28 | Georgia | ECA | 73.9 | 5005 | 51 | 98 | 1.1 |
| 29 | Ghana | SSA | 64.6 | 1684 | 776 | 67 | 19.6 |
| 30 | Guatemala | LAC | 71.4 | 4235 | 473 | 51 | 2.7 |
| 31 | Guinea | SSA | 54.5 | 941 | 394 | 39 | 11.7 |
| 32 | Guinea-Bissau | SSA | 48.6 | 1042 | 59 | 42 | 8.4 |
| 33 | Guyana | LAC | 70.2 | 3387 | 13 | 89 | 3.0 |
| 34 | Haiti | LAC | 62.4 | 1070 | 266 | 25 | 5.2 |
| 35 | Honduras | LAC | 73.4 | 3426 | 205 | 67 | 2.9 |
| 36 | India | SOA | 65.8 | 3285 | 27098 | 47 | 8.0 |
| 37 | Indonesia | EAP | 69.8 | 4154 | 4331 | 55 | 7.1 |
| 38 | Iraq | MEN | 69.6 | 3557 | 1144 | 65 | 10.6 |
| 39 | Jordan | MEN | 73.5 | 5272 | 154 | 99 | 10.0 |
| 40 | Kenya | SSA | 57.7 | 1541 | 1560 | 43 | 11.3 |
| 41 | Kiribati | EAP | 68.4 | 3079 | 22 | 66 | - |
| 42 | Kyrgyzstan | ECA | 68.0 | 2009 | 131 | 97 | 0.3 |
| 43 | Lao People’s Democratic Republic | EAP | 67.8 | 2435 | 140 | 17 | 15.6 |
| 44 | Lesotho | SSA | 48.7 | 1879 | 60 | 59 | - |
| 45 | Liberia | SSA | 57.3 | 480 | 157 | 37 | 9.5 |
| 46 | Madagascar | SSA | 66.9 | 828 | 747 | 35 | 19.4 |
| 47 | Malawi | SSA | 54.8 | 774 | 686 | 73 | 20.8 |
| 48 | Mali | SSA | 51.9 | 853 | 728 | 45 | 12.2 |
| 49 | Marshall Islands | EAP | 72.3 | 4040 | 27 | 85 | - |
| 50 | Mauritania | SSA | 58.9 | 2174 | 118 | 48 | 9.6 |
| 51 | Micronesia, Federated States of | EAP | 69.2 | 3352 | 3 | - | |
| 52 | Moldova, Republic of | ECA | 69.6 | 3319 | 44 | 99 | - |
| 53 | Mongolia | EAP | 68.8 | 4245 | 65 | 99 | - |
| 54 | Morocco | MEN | 72.4 | 4384 | 620 | 73 | - |
| 55 | Mozambique | SSA | 50.7 | 906 | 889 | 58 | 12.1 |
| 56 | Myanmar | EAP | 65.7 | 1817 | 824 | 36 | 6.1 |
| 57 | Namibia | SSA | 62.6 | 5973 | 60 | 81 | 2.8 |
| 58 | Nepal | SOA | 69.1 | 1137 | 722 | 35 | 5.3 |
| 59 | Nicaragua | LAC | 74.3 | 2551 | 138 | 74 | 1.5 |
| 60 | Niger | SSA | 55.1 | 701 | 777 | 17 | 5.3 |
| 61 | Nigeria | SSA | 52.3 | 2102 | 6458 | 35 | 16.9 |
| 62 | Pakistan | SOA | 65.7 | 2566 | 4764 | 41 | 15.0 |
| 63 | Palestine, State of | MEN | 73.0 | 3359 | 33 | - | |
| 64 | Papua New Guinea | EAP | 63.1 | 2386 | 208 | 52 | 7.4 |
| 65 | Paraguay | LAC | 72.7 | 4497 | 158 | 82 | 3.2 |
| 66 | Philippines | EAP | 69.0 | 3752 | 2358 | 44 | 2.5 |
| 67 | Rwanda | SSA | 55.7 | 1147 | 449 | 69 | 5.8 |
| 68 | Samoa | EAP | 72.7 | 3928 | 4 | 81 | - |
| 69 | Sao Tome and Principe | SSA | 64.9 | 1864 | 5 | 79 | 7.4 |
| 70 | Senegal | SSA | 59.6 | 1653 | 471 | 73 | 15.1 |
| 71 | Sierra Leone | SSA | 48.1 | 881 | 227 | 50 | 7.9 |
| 72 | Solomon Islands | EAP | 68.2 | 2172 | 17 | 85 | 22.3 |
| 73 | Somalia | SSA | 51.5 | 150 | 416 | 9 | 3.1 |
| 74 | South Sudan | SSA | - | ||||
| 75 | Sri Lanka | SOA | 75.1 | 5170 | 373 | 98 | 2.9 |
| 76 | Sudan | SSA | 61.8 | 1848 | 1447 | 21 | 15.3 |
| 77 | Swaziland | SSA | 48.9 | 5104 | 35 | 80 | 8.7 |
| 78 | Syrian Arab Republic | MEN | 76.0 | 4674 | 466 | 78 | - |
| 79 | Tajikistan | ECA | 67.8 | 2119 | 194 | 88 | 0.8 |
| 80 | Tanzania, United Republic of | SSA | 58.9 | 1383 | 1913 | 50 | 16.4 |
| 81 | Timor-Leste | EAP | 62.9 | 5446 | 44 | 22 | 5.0 |
| 82 | Togo | SSA | 57.5 | 928 | 195 | 67 | 21.2 |
| 83 | Tonga | EAP | 72.5 | 4153 | 3 | 98 | - |
| 84 | Tuvalu | EAP | 67.5 | 5650 | 93 | - | |
| 85 | Uganda | SSA | 54.5 | 1168 | 1545 | 57 | 14.5 |
| 86 | Uzbekistan | ECA | 68.6 | 3201 | 589 | 97 | 1.0 |
| 87 | Vanuatu | EAP | 71.3 | 3960 | 7 | 80 | 8.0 |
| 88 | Vietnam | EAP | 75.4 | 2970 | 1458 | 92 | 8.9 |
| 89 | Yemen | MEN | 65.9 | 1820 | 940 | 24 | 4.6 |
| 90 | Zambia | SSA | 49.4 | 1358 | 622 | 48 | 21.0 |
| 91 | Zimbabwe | SSA | 52.7 | 424 | 377 | 65 | 14.8 |
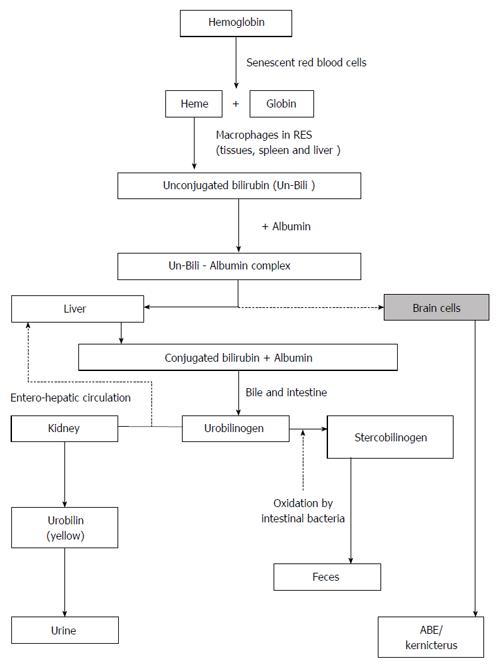
The metabolism of bilirubin has been well described in the literature[19-21]. Essentially, bilirubin production is a normal process of human physiology and begins from the degradation of heme from senescent red blood cells (Figure 1). Once produced, bilirubin is conjugated in the liver with glucuronic acid to form bilirubin glucuronide. Conjugated bilirubin is then conveyed across the canalicular membrane through the biliary tree to the intestinal lumen for excretion. Newborns, especially premature infants, have an immature bilirubin conjugation and excretion system. As a result, they have limited ability to conjugate bilirubin and excrete unconjugated bilirubin readily. These limitations account for an imbalance between bilirubin production and elimination. In effect, neonatal jaundice occurs when the rate at which bilirubin is produced exceeds the rate of elimination, reflecting the total bilirubin load in the body after birth, to become visible in the skin as yellow pigment. In full-term infants, serum bilirubin concentrations, known as physiologic jaundice, peak at 5 to 10 mg/dL in the first three days of life and decline thereafter to values commonly found in adults of approximately 1 mg/dL. However, in a few infants, serum bilirubin concentrations may become pathologic and exceed 17 mg/dL, which is indicative of a disorder that requires treatment. Total bilirubin levels beyond 17 mg/dL, especially in infants with predisposing hemolytic conditions, may lead to the movement of unconjugated bilirubin into brain cells to cause acute bilirubin encephalopathy. Continued exposure to free bilirubin may lead to irreversible damage or chronic bilirubin encephalopathy. Timely intensive phototherapy and ET can arrest this progression and prevent or minimize bilirubin-induced mortality and long-term neurologic morbidity.
The facilities and techniques for undertaking ET in LMICs have been well described in the literature[4,8]. The clinical criteria for initiating ET have also been discussed in greater detail elsewhere[8,22]. Typically, regardless of the total plasma/serum bilirubin (TSB) level, a “crash-cart approach” (initiation of immediate intensive phototherapy and fluid supplementation, followed by ET) is recommended for infants with early signs and symptoms of intermediate/advanced ABE (lethargy, hypotonia, poor feeding, seizures, opisthotonos, and impaired level of consciousness) with or without evidence of neurotoxicity risk factors (prematurity, isoimmune hemolytic disease, G6PD deficiency, asphyxia, sepsis, acidosis, and hypoalbuminemia). It is also worth noting that the clinical diagnosis of hemolytic jaundice remains a challenge owing to the lack of advanced tests like end-tidal carbon monoxide (ETCO), eosin-5-maleimide flow cytometry to identify red blood cell membrane defects, and next-generation sequencing of relevant genes for mutations and polymorphisms[23].
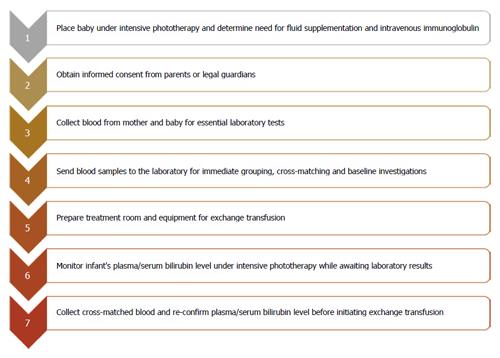
Studies describing the process from when the decision to conduct ET has been made and the actual execution of ET systematically were surprisingly rare from our literature review[4,9,24,25]. We therefore also relied on our practice experience spanning over three decades in providing newborn care in a LMIC. For example, from 2012 to 2014, approximately 120 ETs were conducted annually in our hospital, Massey Street Children’s Hospital in Lagos, which is the oldest children’s hospital in Nigeria[26]. Typically, in most clinical settings, once the need for ET has been established by the resident physician and the consultant, the typical steps to ET can be summarized as shown in Figure 2. The delays that may be encountered at any of these stages are described as follows:
Effective phototherapy has been shown to reduce the need for ET in several studies[27-31]. An effective phototherapy device should produce specific blue-light wavelengths (peak emission: 450 ± 20 nm), preferably in a narrow bandwidth to about 80% of an infant’s body surface area[32]. The light source may be fluorescent tubes, halogen lamps, or light emitting diodes. Whatever the light-source, conventional phototherapy should have an irradiance of at least 8-10 μW/cm2 per nanometer, and intensive phototherapy should have an irradiance of ≥ 30 μW/cm2 per nanometer (from either a single or multiple phototherapy units). The lack of effective phototherapy in many hospitals has been reported in several studies[33-36]. In one survey from Nigeria, for example, the vast majority (94%) of 63 phototherapy devices tested in twelve referral-level hospitals delivered irradiance of ≤ 10 μW/cm2 per nanometer and none were ≥ 30 μW/cm2 per nanometer[35].
Ineffective phototherapy is frequently attributed to erratic power supply, inadequate skin exposure (due to overcrowding from multiple infants being placed under a single device), sub-optimal irradiance levels, and poor device maintenance. A lack of intensive phototherapy during the waiting period for ET often results in a high incidence of kernicterus prior to ET and ultimately compromises the effectiveness of ET[11]. It is therefore not surprising to find adverse neurodevelopmental outcomes post-ET[17,18,37,38]. To ensure effective phototherapy, it is essential that the devices are properly monitored, regularly maintained, and that the staff are well trained to provide the best possible care for the affected infants preparatory to ET. The potential use of filtered sunlight phototherapy is currently being piloted and holds promise in tropical LMICs where effective conventional electric blue-light phototherapy devices cannot be routinely assured[39,40].
The administration of intravenous fluid supplementation should be considered for infants with evidence of dehydration, especially as a result of late presentation. This intervention has been found to decrease the need for ET by up to 70% without any long-term adverse effects[4,41]. Similarly, the use of intravenous immunoglobulin may be helpful in reducing the need for ET in infants with isoimmune hemolytic jaundice[4,42].
Information on grouping and cross-matching, as well as baseline investigations such as full blood count, sodium, potassium, calcium, TSB, magnesium and glucose, are required before initiating ET. Ethical considerations forbid blood or blood product transfusion without informed consent. However, delay in getting informed consent because the mother is not available, (due to death, critical illness, or being in another hospital) or the person with parental right is unavailable is not uncommon[6]. Delay may also be encountered in trying to convince parents who are reluctant to give consent on religious grounds[11]. Additionally, the mother’s blood may not be available in time, owing to critical illness or the mother being admitted to another hospital. Difficulties may also be encountered where the mother is unavailable due to premature death. These potential sources of delay should be anticipated and addressed appropriately. It is important that prenatal maternal education be considered, especially in settings where religious beliefs are likely to delay consent for ET.
The volume of requested blood will depend on the decision for a single (estimated blood volume × baby’s weight in kilograms) or double volume (estimated blood volume × 2 × baby’s weight in kilograms) ET. Given the wide prevalence of G6PD deficiency in many LMICs, it is not uncommon for centers to have a standing rule for double-volume ET that removes 85% of the infant’s red blood cells with up to 50% TSB decline and a potential rebound to two-thirds pre-exchange level, effectively removing one-third pre-exchange TSB level[4]. However, failure to request the right amount of blood is not unusual and often results in a delay or wastage. In fact, it is more common to find clinicians over-ordering just to be assured of the availability of sufficient blood. This often results in wastage of blood and remains a potential source of friction between clinicians and the laboratory personnel[43].
Getting blood samples to the laboratory may be challenging where the functional laboratory and blood bank are outside the immediate vicinity of the hospital, as frequently encountered in many LMICs. Laboratories are often centralized to serve diverse requirements from multiple clinical units. Information from the lab may therefore be difficult to track. Where the laboratory is accessible, hospital personnel may not be immediately available, due to shortage of staff, to collect the blood as soon as the laboratory sends information to the ward that it is ready. To facilitate efficient communication with laboratory personnel, it is important to designate somebody for this task well in advance, if possible.
The ET room must be warm and ready with essential items for the procedure, such as IV infusion pump, arterial line pack, blood warmer, and protective goggles, as well as automated monitors for cardiac, blood pressure, oxygen saturation, and respiratory function. Emergency trolley and suction equipment with appropriate catheters should be checked, stocked, and nearby. Many of these items may not be readily available and a significant number of critical items may also have to be purchased by the infant’s family. Where there is no designated room for ET, a suitable area has to be identified and screened off for the procedure. The need for infection control and keeping the baby warm must be considered.
In most hospitals, all laboratory services are centralized, implying that requests from ET personnel, even when urgent, have to be queued on arrival with other urgent requests. Laboratories in LMICs encounter several challenges that compromise their efficiency in achieving optimal turn-around time on the various requests for special investigations. These include inadequate and not up-to-date facilities, inadequate personnel, inadequate stock of blood, and, occasionally, inadequate blood samples for the required investigations.
Screening donor blood for hepatitis and human immunodeficiency virus is standard in many LMICs, but tests for G6PD status, cytomegalovirus (CMV), and malaria are often excluded, especially in regions where malaria is endemic. This may lead to using G6PD-deficient, CMV, or malaria-packed blood for ET. The use of G6PD-deficient blood has been associated with recurrent hemolysis and rebound TSB that often leads to repeat ET[44]. In the absence of blood warmer, the added time interval required to warm blood to body temperature may also prolong waiting time. Most laboratories lack diagnostic facilities for hemolytic disorders of newborns, and this frequently delays effective treatment for the affected infants.
A shortage in the number of laboratory personnel available to perform all the necessary laboratory analysis is also an important source of delay. A laboratory scientist who is in charge of carrying out the grouping and cross matching of blood for ET may be simultaneously engaged on other benches. This situation often leads to delays in issuing out blood for ET. Additionally, if the request for cross-matching gets to the laboratory very late in the day, call personnel in charge of several benches may have to be called in for grouping and cross-matching.
Blood samples from the baby may also be insufficient. Laboratory staff often complain about very small blood samples from the baby because of the method of grouping and cross-matching. A follow-up request for more blood from the laboratory causes further delay. The choice of blood, especially when the mother’s blood is not available, may also compound the problem. In situations where the mother is dead or critically ill, the best blood for ET is fresh O Rhesus “D” negative blood, but this is very scarce. Fresh whole blood less than 48 h old and not more than five days old is preferred for ET. However, since this is unattainable in most cases, the consequence is another delay in ET[13]. All blood donors should be voluntary according to internationally laid down guidelines, but blood banks in many LMICs find it difficult to convince individuals to donate blood. The end-result is delayed ET for newborns at risk of ABE/kernicterus while the perennial problem, of insufficient blood in the blood bank, persists. If the blood group that is compatible with the newborn and the mother is not available in the blood bank, other blood banks will have to be contacted, and this may extend to days before the compatible blood unit becomes available. The packed cell volume (PCV) of the donor blood is not expected to be less than 40% for male donors and 38% for female donors. However, the lack of adequate blood supply to blood banks often accounts for the reluctance of blood banks in rejecting donors with low packed red blood cell volume. Performing ET with low PCV donor blood is sub-optimum, leading invariably to additional transfusion with packed red cells.
Availability of real-time TSB measurement is imperative, but seldom achieved due to of the lack of a functional side laboratory with bilirubinometers in many neonatal intensive-care units. As a result, TSB monitoring still has to rely on sending blood samples to the main designated hospital laboratory for analysis. Even when intensive phototherapy is provided, the need for ET may be contingent on several factors, including accurate knowledge of the risk status of the infant and the presence of hemolytic disease. Where ET is successfully avoided as a result of the provision of effective phototherapy, the result is often unutilized blood from the blood bank. While this pattern is desirable and unavoidable, it has the impact of depleting the blood bank and causing unnecessary delay in meeting future requirements for ET. It is important to be alert to the likelihood of TSB rebound after otherwise successful intensive phototherapy, especially in infants with hemolytic jaundice. Lack of close monitoring of the affected infants may result in initially withholding ET, only for it to be later required. Failure to recognize the possibility of declining TSB level following intensive phototherapy coincident with the clinical onset of kernicterus could also be a source of potential delay[45]. It is important to view such a decline as a prognostic sign for neurologic dysfunction, rather than a sign of clinical improvement, before or after phototherapy.
The ET procedure itself seeks to remove or reduce circulating antibody-coated red blood cells and/or products of hemolysis in various immune or non-immune hemolytic anemias and other red cell enzyme deficiencies. This is accomplished by repeatedly exchanging small samples (5-10 mL/kg) of blood via an arterial catheter and replacing simultaneously with fresh donor blood providing fresh albumin with binding sites for bilirubin by continuous infusion into a peripheral or central vein. The procedure can typically last between 2 to 4 h depending on the choice between single or double volume ET.
Limited skill by clinicians can result in further delays. For example, inability to cannulate the umbilical vein and leakage of blood between the catheter and umbilical vein may unduly prolong the procedure. Difficulties may also be encountered in withdrawing blood in spite of the apparently successfully introduction of an umbilical catheter[46].
Post-ET monitoring is necessary because of the likelihood of repeat ET after a rebound of high TSB level due to unrecognized hemolytic disease, with potential secondary delays[28,30,44]. Not all attending clinicians in emergency situations are skillful in providing ET, even where facilities are available, and this may result in delays in getting a suitable individual when all preparations have been made. In settings where ET is infrequent, lack of expertise may be a source of delay, especially when referral to another hospital becomes imperative[14]. Lack of a clearly-defined protocol or failure to adhere to an existing protocol is likely to cause delay as a result of communication gaps among team members. Where ET protocol requires the express approval of a consultant before execution by attending junior physicians, this may result in more potential delays. When more than one infant requires urgent ET and resources are limited, identifying and prioritizing the infant(s) most at-risk of kernicterus may also inevitably result in delay for some infants. Additionally, inadequate support staff may be a source of delay in providing seamless communication with the laboratory and/or a skilled assistant for the procedure. In some settings, patients may be required to bear the costs of the laboratory investigations requested by the attending physicians, especially in private hospitals[47,48]. Inability to meet such expenses is also a potential source of delay in providing timely ET[49].
The nature and scope of these delays are likely to vary within and across LMICs. Perhaps the overarching implication of these challenges is the impetus to avoid ET as much as possible by facilitating early presentation and timely provision of effective/intensive phototherapy, as well as investment in functional, readily accessible, and appropriately staffed laboratories in all hospitals that offer emergency care for newborns. Side laboratory with facilities for real-time bilirubin measurements should be made available in all neonatal units. Education of mothers and caregivers on the value of timely presentation and intervention in preventing bilirubin-induced mortality and long-term neurodevelopmental disorders should be routinely offered during antenatal visits. There is also a need for better communication and understanding between clinicians and laboratory personnel, especially with regards to the challenge of minimizing wastage of blood due to over-ordering[43].
While the focus of this review is primarily to serve the needs of clinicians in LMICs, the emerging and rising profile of global child health makes the topic also relevant to clinicians in the developed world.
ET is widely embraced as an effective treatment for infants with, or at risk of, bilirubin-induced neurologic dysfunctions (ABE and kernicterus) in LMICs. However, several potential delays are associated with the various critical steps prior to the initiation of ET after the need for this emergency procedure has been established. Efforts to minimize these delays, including efficient laboratory and logistical support, are imperative in ensuring timely and efficacious ET. Timely, effective, and intensive phototherapy should also be routinely provided to curtail the prevailing high rates of avoidable ET in LMICs.
P- Reviewer: Mostafa BE, Sergi CM, Sangkhathat S, Teng RJ S- Editor: Gong XM L- Editor: Rutherford A E- Editor: Wang CH
| 1. | Ip S, Chung M, Kulig J, O’Brien R, Sege R, Glicken S, Maisels MJ, Lau J; American Academy of Pediatrics Subcommittee on Hyperbilirubinemia. An evidence-based review of important issues concerning neonatal hyperbilirubinemia. Pediatrics. 2004;114:e130-e153. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 245] [Cited by in F6Publishing: 216] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 2. | National Institute for Health and Clinical Excellence (NICE), UK. Neonatal jaundice. (Clinical guideline 98) 2010. 2015;Jul 14] Available from: http://www.nice.org.uk/CG98. [Cited in This Article: ] |
| 3. | Jackson JC. Adverse events associated with exchange transfusion in healthy and ill newborns. Pediatrics. 1997;99:E7. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 130] [Cited by in F6Publishing: 91] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 4. | Murki S, Kumar P. Blood exchange transfusion for infants with severe neonatal hyperbilirubinemia. Semin Perinatol. 2011;35:175-184. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 56] [Cited by in F6Publishing: 58] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 5. | Sanpavat S. Exchange transfusion and its morbidity in ten-year period at King Chulalongkorn Hospital. J Med Assoc Thai. 2005;88:588-592. [PubMed] [Cited in This Article: ] |
| 6. | Salas AA, Mazzi E. Exchange transfusion in infants with extreme hyperbilirubinemia: an experience from a developing country. Acta Paediatr. 2008;97:754-758. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 19] [Cited by in F6Publishing: 21] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 7. | American Academy of Pediatrics Subcommittee on Hyperbilirubinemia. Management of hyperbilirubinemia in the newborn infant 35 or more weeks of gestation. Pediatrics. 2004;114:297-316. [PubMed] [Cited in This Article: ] |
| 8. | Olusanya BO, Ogunlesi TA, Kumar P, Boo NY, Iskander IF, de Almeida MF, Vaucher YE, Slusher TM. Management of late-preterm and term infants with hyperbilirubinaemia in resource-constrained settings. BMC Pediatr. 2015;15:39. [PubMed] [Cited in This Article: ] |
| 9. | Bhutani VK, Johnson L. The jaundiced newborn in the emergency department: Prevention of kernicterus. Clin Ped Emerg Med. 2008;9:149-159. [DOI] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in F6Publishing: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 10. | Abu-Ekteish F, Daoud A, Rimawi H, Kakish K, Abu-Heija A. Neonatal exchange transfusion: a Jordanian experience. Ann Trop Paediatr. 2000;20:57-60. [PubMed] [Cited in This Article: ] |
| 11. | Owa JA, Ogunlesi TA. Why we are still doing so many exchange blood transfusion for neonatal jaundice in Nigeria. World J Pediatr. 2009;5:51-55. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 62] [Cited by in F6Publishing: 66] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 12. | Hameed NN, Na’ Ma AM, Vilms R, Bhutani VK. Severe neonatal hyperbilirubinemia and adverse short-term consequences in Baghdad, Iraq. Neonatology. 2011;100:57-63. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 39] [Cited by in F6Publishing: 44] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 13. | Rasul CH, Hasan MA, Yasmin F. Outcome of neonatal hyperbilirubinemia in a tertiary care hospital in bangladesh. Malays J Med Sci. 2010;17:40-44. [PubMed] [Cited in This Article: ] |
| 14. | Iskander I, Gamaleldin R, Kabbani M. Root causes for late presentation of severe neonatal hyperbilirubinaemia in Egypt. East Mediterr Health J. 2012;18:882-887. [PubMed] [Cited in This Article: ] |
| 15. | Olusanya BO, Ogunlesi TA, Slusher TM. Why is kernicterus still a major cause of death and disability in low-income and middle-income countries? Arch Dis Child. 2014;99:1117-1121. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 89] [Cited by in F6Publishing: 92] [Article Influence: 9.2] [Reference Citation Analysis (0)] |
| 16. | Murray NA, Roberts IA. Haemolytic disease of the newborn. Arch Dis Child Fetal Neonatal Ed. 2007;92:F83-F88. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 112] [Cited by in F6Publishing: 92] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 17. | Martínez-Cruz CF, García Alonso-Themann P, Poblano A, Cedillo-Rodríguez IA. Hearing and neurological impairment in children with history of exchange transfusion for neonatal hyperbilirubinemia. Int J Pediatr. 2014;2014:605828. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 12] [Cited by in F6Publishing: 11] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 18. | Mukhopadhyay K, Chowdhary G, Singh P, Kumar P, Narang A. Neurodevelopmental outcome of acute bilirubin encephalopathy. J Trop Pediatr. 2010;56:333-336. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 21] [Cited by in F6Publishing: 22] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 19. | Dennery PA, Seidman DS, Stevenson DK. Neonatal hyperbilirubinemia. N Engl J Med. 2001;344:581-590. [PubMed] [Cited in This Article: ] |
| 20. | Stevenson DK, Vreman HJ, Wong RJ. Bilirubin production and the risk of bilirubin neurotoxicity. Semin Perinatol. 2011;35:121-126. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 42] [Cited by in F6Publishing: 43] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 21. | Kaplan M, Bromiker R, Hammerman C. Hyperbilirubinemia, hemolysis, and increased bilirubin neurotoxicity. Semin Perinatol. 2014;38:429-437. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 48] [Cited by in F6Publishing: 111] [Article Influence: 11.1] [Reference Citation Analysis (0)] |
| 22. | Olusanya BO, Imam ZO, Emokpae AA, Iskander IF. Revisiting the Criteria for Exchange Transfusion for Severe Neonatal Hyperbilirubinemia in Resource-Limited Settings. Neonatology. 2016;109:97-104. [PubMed] [Cited in This Article: ] |
| 23. | Christensen RD, Yaish HM. Hemolytic Disorders Causing Severe Neonatal Hyperbilirubinemia. Clin Perinatol. 2015;42:515-527. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 26] [Cited by in F6Publishing: 25] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 24. | Pam S, Bode-Thomas F, Joseph DE, Akor F, Ejeliogu E. Which babies get blood in Jos, Nigeria? Pediatr Hematol Oncol. 2004;21:669-676. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 25. | Malla T, Singh S, Poudyal P, Sathian B, Bk G, Malla KK. A Prospective Study on Exchange Transfusion in Neonatal Unconjugated Hyperbilirubinemia--in a Tertiary Care Hospital, Nepal. Kathmandu Univ Med J (KUMJ). 2015;13:102-108. [PubMed] [Cited in This Article: ] |
| 26. | Emokpae AA, Mabogunje CA, Imam ZO, Olusanya BO. Heliotherapy for Neonatal Hyperbilirubinemia in Southwest, Nigeria: A Baseline Pre-Intervention Study. PLoS One. 2016;11:e0151375. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 10] [Cited by in F6Publishing: 10] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 27. | Edris AA, Ghany EA, Razek AR, Zahran AM. The role of intensive phototherapy in decreasing the need for exchange transfusion in neonatal jaundice. J Pak Med Assoc. 2014;64:5-8. [PubMed] [Cited in This Article: ] |
| 28. | Abd-Ellatif MA, Abd-Ellatif DA. The use of intensive phototherapy in severe neonatal hyperbilirubinemia. J Egypt Soc Parasitol. 2012;42:483-494. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 5] [Cited by in F6Publishing: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 29. | Lucas GN. Neonatal jaundice due to ABO incompatibility in Sri Lankan. Indian J Pediatr. 1996;63:381-384. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 9] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 30. | Sherbiny HS, Youssef DM, Sherbini AS, El-Behedy R, Sherief LM. High-intensity light-emitting diode vs fluorescent tubes for intensive phototherapy in neonates. Paediatr Int Child Health. 2015;Epub ahead of print. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 19] [Cited by in F6Publishing: 20] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 31. | Bansal A, Jain S, Parmar VR, Chawla D. Bilirubin rebound after intensive phototherapy for neonatal jaundice. Indian Pediatr. 2010;47:607-609. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 22] [Cited by in F6Publishing: 15] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 32. | Bhutani VK, Cline BK, Donaldson KM, Vreman HJ. The need to implement effective phototherapy in resource-constrained settings. Semin Perinatol. 2011;35:192-197. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 31] [Cited by in F6Publishing: 29] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 33. | Pejaver RK, Vishwanath J. An audit of phototherapy units. Indian J Pediatr. 2000;67:883-884. [PubMed] [Cited in This Article: ] |
| 34. | Cline BK, Vreman HJ, Faber K, Lou H, Donaldson KM, Amuabunosi E, Ofovwe G, Bhutani VK, Olusanya BO, Slusher TM. Phototherapy device effectiveness in Nigeria: irradiance assessment and potential for improvement. J Trop Pediatr. 2013;59:321-325. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 29] [Cited by in F6Publishing: 31] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 35. | Owa JA, Adebami OJ, Fadero FF, Slusher TM. Irradiance readings of phototherapy equipment: Nigeria. Indian J Pediatr. 2011;78:996-998. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 24] [Cited by in F6Publishing: 18] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 36. | Satrom K, Slusher T, Satrom J. Effectiveness of phototherapy units in Cameroon. J Trop Pediatr. 2014;60:264-266. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 12] [Cited by in F6Publishing: 13] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 37. | Mittal R, Ramesh AV, Panwar SS, Nilkanthan A, Nair S, Mehra PR. Auditory neuropathy spectrum disorder: its prevalence and audiological characteristics in an Indian tertiary care hospital. Int J Pediatr Otorhinolaryngol. 2012;76:1351-1354. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 21] [Cited by in F6Publishing: 22] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 38. | Olusanya BO, Akande AA, Emokpae A, Olowe SA. Infants with severe neonatal jaundice in Lagos, Nigeria: incidence, correlates and hearing screening outcomes. Trop Med Int Health. 2009;14:301-310. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 42] [Cited by in F6Publishing: 43] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 39. | Slusher TM, Vreman HJ, Olusanya BO, Wong RJ, Brearley AM, Vaucher YE, Stevenson DK. Safety and efficacy of filtered sunlight in treatment of jaundice in African neonates. Pediatrics. 2014;133:e1568-e1574. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 35] [Cited by in F6Publishing: 38] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 40. | Slusher TM, Olusanya BO, Vreman HJ, Brearley AM, Vaucher YE, Lund TC, Wong RJ, Emokpae AA, Stevenson DK. A Randomized Trial of Phototherapy with Filtered Sunlight in African Neonates. N Engl J Med. 2015;373:1115-1124. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 49] [Cited by in F6Publishing: 51] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 41. | Mehta S, Kumar P, Narang A. A randomized controlled trial of fluid supplementation in term neonates with severe hyperbilirubinemia. J Pediatr. 2005;147:781-785. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 46] [Cited by in F6Publishing: 44] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 42. | Alcock GS, Liley H. Immunoglobulin infusion for isoimmune haemolytic jaundice in neonates. Cochrane Database Syst Rev. 2002;CD003313. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 40] [Cited by in F6Publishing: 53] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 43. | Stern SC, Cockburn H, de Silva PM. Current practice in neonatal exchange transfusions: a retrospective audit based at one transfusion centre. Transfus Med. 1998;8:97-101. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 44. | Samanta S, Kumar P, Kishore SS, Garewal G, Narang A. Donor blood glucose 6-phosphate dehydrogenase deficiency reduces the efficacy of exchange transfusion in neonatal hyperbilirubinemia. Pediatrics. 2009;123:e96-e100. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 22] [Cited by in F6Publishing: 24] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 45. | Ackerman BD, Dyer GY, Taylor PM. Decline in serum bilirubin concentration coincident with clinical onset of kernicterus. Pediatrics. 1971;48:647-650. [PubMed] [Cited in This Article: ] |
| 46. | Laditan AAO, Effiong CE, Antia AU. Morbidity and Mortality from Exchange Blood Transfusion in Neonatal Jaundice. Niger J Paediatr. 1975;2:42-46. [Cited in This Article: ] |
| 47. | Saksena P, Reyburn H, Njau B, Chonya S, Mbakilwa H, Mills A. Patient costs for paediatric hospital admissions in Tanzania: a neglected burden? Health Policy Plan. 2010;25:328-333. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 15] [Cited by in F6Publishing: 17] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 48. | Ekwochi U, Osuorah DC, Ndu IK, Ezenwosu OU, Amadi OF, Nwokoye IC, Odetunde OI. Out-of-pocket cost of managing sick newborns in Enugu, southeast Nigeria. Clinicoecon Outcomes Res. 2014;6:29-35. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 2] [Cited by in F6Publishing: 9] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 49. | Ibekwe RC, Ibekwe MU, Muoneke VU. Outcome of exchange blood transfusions done for neonatal jaundice in abakaliki, South eastern Nigeria. J Clin Neonatol. 2012;1:34-37. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 17] [Cited by in F6Publishing: 18] [Article Influence: 1.6] [Reference Citation Analysis (0)] |