Abstract
Background:
Iran’s Health Transformation Plan (HTP) was implemented to decrease households’ out of pocket and protect them from facing catastrophic health expenditure and impoverishment from 2014. It is needed to assess the effect of HTP; therefore, the study aimed to examine the households’ impoverishment due to health expenditure after HTP.Methods:
A household survey was carried out in 2017 in Sistan and Baluchestan province in southeast Iran. About 2400 households were selected as the study sample using a multi-stage sampling technique. The household section of the World Health Survey questionnaire was used to collect data. Independent variables contained households’ characteristics, household income, chronic illness status, the use of health services, and health spending. The dependent variable was whether the household was faced with health spending impoverishment. Mixed effects logistic regression was used to assess the effect of the independent variables on the impoverishment using SPSS software 21.Results:
About 7.5% of the households had no basic insurance and 757 (31.6) heads’ of the households were unemployment. The results showed that about 5.4% of the households impoverished due to health expenditure. The households in the furthest region were forced with impoverishment more than other regions (23.0%). Living in a rural area, unemployment, economic status, and inpatients and outpatient costs were the main determinates on impoverishment (P < 0.05). In addition, having supplementary insurance was a protective factor in facing impoverishment (P = 0.05).Conclusions:
In general, despite the implementation of HTP, healthcare expenditures leading to impoverishment of high percent of the households and Iranian development goals have not been fulfilled in this region. Economic poverty of the people may also be an important factor in this regard. It is recommended that outpatient services are covered by health insurances.Keywords
1. Background
Health is strongly affected by the factors, which are outside the health care area. Poverty is one of the most important among them (1) and this relationship is identified for decades (2, 3). When individuals or households are forced to use a large fraction of their properties to pay for health care, the financial problems are created. This can treat living standards in a short time, which may lead to sacrifice instant consumption of other goods and services, or in the long time lead to losing assets or savings and creating debates (4).
According to the WHO announcement, catastrophic health expenditures (CHE) and impoverishment, due to health spending, are 2 indicators that measure the economic burden of health care (5). Financial catastrophic and impoverishment due to health spending are among the greatest problems worldwide, particularly in developing countries where out of pocket (OOP) payment is the main part of financing (6). Impoverishing payment in most cases pushes an individual or household under the poverty line. The expenditures lead to face the households with very hard choices such as forbear using health care services or receiving them and falling the family into the poverty trap (1, 2).
Impoverishment indicator is one of the best approaches to measure health financial burden, which states that health expenses must not push households into poverty or no deep financial problems to those under poverty line (4).
Studies show other household characteristics such as disabled or unemployed members, limited access to health insurance, old head of household, and those with chronic disease or hospitalized members are at a high risk of catastrophic and impoverishing expenditure (3, 4).
Three goals are determined for the health system by WHO and equitable contribution for financing of health expenses is one of them. This is the reason for emphasis on the impoverishing effect of health expenditures (7). In this regard, the Iranian government tried to reduce the OOP payment by some reforms in financing of the health system, such as universal health insurance law, in the 4 and 5 year National Development Plans; however, they were not successful (5). After that, to decrease the financial burden of the households, the Iranian government initiated the Iran’s Health Transformation Plan (HTP) in 2014. HTP was implemented in May 5, 2014, with 8 service packages (6). The main factors of the reform, which was introduced by experts in the health system are as follows: increasing health care costs, increasing public expectations, resources limitation and increasing public demand from the government due to poor governance, corruption and inefficiency of power, and bureaucratic inhibitors (8, 9). Three financial sources are determined for supporting the plan: increasing the public annual budget of health sector, resources of the targeted subsidies’ law (10% of total subsidies), and a specific 1% value added tax (VAT) for health. It is estimated that the financial sources for the health sector was 70% higher in 2015 compared to 2014 (10). After implementation of the HTP, some studies showed the decreasing of CHE in the some regions of Iran (11) as well as the positive effect of the plan. It should be noted that no study in this regard has been done in the poorest region of Iran.
In one hand, there are only some limited reports, which are provided by the offices responsible for HTP and other insurance schemes in Iran to evaluate the plan. On the other hand, few independent assessments of the program are done until now. Moreover, there is no consensus on whether HTP prevent effectively households from impoverishing health payment or not. Therefore, this study aimed to measure the percentage of households falling into poverty due to health expenditures and the factors affecting impoverishment in Sistan and Baluchistan as the widest and poorest province in Iran.
2. Methods
A household cross-sectional study was carried out in Sistan and Baluchestan by the Zahedan University of Medical Sciences (ZAUMS) in 2017. Sistan and Baluchestan province, the widest province, is located in southeast of Iran with about 2.5 million people (7). According to integrated health indicators categorization, the province is the poorest region in Iran (12). The study population contained all households living in the province (about 587921 households in urban and rural area).
The study sample was calculated based on the following formula:
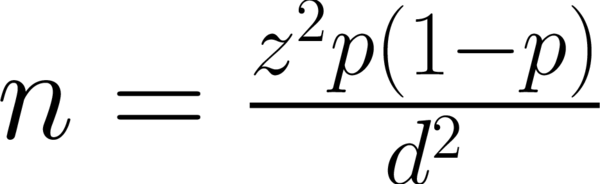
According to the previous study, α = 0.05, Z = 1.96, P = 14 (13), d = 0.02, and design effect = 2
In total, about 2400 households were selected for the study. According to the weight of the households in each city, in the province based on the 2011 census, which was done by statistical center of Iran, the samples were selected as following: Zahedan as the capital of province (816), Zabol (336), Iranshahr (264), Chabahar (312), Khash (192), Saravan (216), and Nikshahr (264), which were selected based on the their ration in urban and rural.The study sample was selected using stratified and cluster sampling in the urban and rural areas, respectively. Urban areas were divided into 5 districts (south, north, west, east, and center), each of which was considered to be a stratum. Sampling with the probability proportional to size was done in each stratum to determine its sample size. Having determined the city sample size, the sample size of each stratum was randomly selected using households’ ID numbers from the health centers. The questionnaires were completed by interviewing the heads or informed individuals of the households selected. If a researcher was unsuccessful after 2 tries in interviewing a household at a specific address, the next address was chosen as a replacement. In the rural area, each health house rural was considered to be a cluster and some of the health houses were selected by using systematic sampling. Since the number of households covered by each health house was different, sampling with the probability proportional to size was used to determine the sample size of the each health center. The selected sample size was equally divided among the wellness centers and the required data was gathered by interview of heads or informed individuals of the selected households. Researchers contacted the wellness centers to inform them of the number of households in their area that would take part in the interviews. The questionnaires were completed by interviewing the heads or informed individuals of the selected households.
The inclusion criteria in the study were tendency to participate in the study and attendance of the household head or informed person at the time of interview. The exclusion criteria included not remembering the household cost information.
Data was gathered using the household section of the questionnaire entitled World Health Survey (WHS), which was developed by WHO to evaluate the performance of health systems (13). Kavosi et al. confirmed the validity and reliability of the questionnaire (14). The WHS contains 2 main sections: the household questionnaire and the individual questionnaire. In this manuscript we report the results of the household questionnaire. It includes the following modules: ‘household roster’, ‘health intervention coverage’, ‘health insurance’, ‘health expenditure’, ‘indicators of permanent income’, and ‘health occupation’.
We determined a 1 month recall period for the household total expenditures, consumption rates, and outpatient medical care expenditures. Moreover, we determined a year recall period for the household expenditures and consumption of inpatient services. To calculate medical impoverishment, all expenditure variables were converted monthly. Moreover, the households expenditures were considered as an indicator of the households’ purchasing power as it has been mentioned in many previous studies, as well (15).
2.1. Assessment of Medical Impoverishment
A non-poor household will be poor due to heath payments, if it becomes poor after paying for health services or staying longer in poverty. We measured medical impoverishment by using the following data: total household expenditure (EXP), household food expenses, family size to determine the equivalent family size, per-capita food expenditure, subsistence expenditure (SE), and OOP healthcare payments.
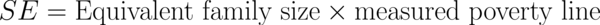
At first, family size and food expenses were converted into the equivalent family size and per-capita food expenditure, respectively. In order to obtain the household’s equivalent size, the real family size was powered by β [0.56], while in order to obtain the household’s per-capita food expenditure, the food expenses of the household were divided by the equivalent family size. Then, the ratio of food expenses to EXP was measured by dividing the food expenses by EXP and the households were ordered based on the obtained numbers. The poverty line was calculated as the household’s average equivalent food expenditure, which was from the 45 to 55 percentiles of the food expenditure to EXP. This number was considered to be the food poverty line in the research community. By taking this poverty line into account, each household’s SE was measured according to the following formula:
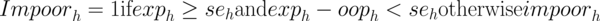
In order to show the effect of impoverishment due to health payments, the variable impoorh was made. If the EXP of a household was equal or exceed the SE but was less than the net SE after OOP healthcare payments, that household is incurring medical impoverishment, as defined below:
2.2. Determinants of Medical Impoverishment
Logistic regression model was employed to predict the likelihood of facing medical impoverishment and to calculate the odds ratios (OR) using the model coefficients. Besides, P-values less than 0.05 were considered as statistically significant. The proportion of households facing medical impoverishment is a dependent variable. The independent variables were gender, job, and educational status of the head of the household, location of residence, number of the household members, household economic status, number of members under the age 5 and over the age 65, basic and supplementary insurance status of the head of the household, use of dental services and inpatient medical services, OOP payment for medicine, physiotherapy, diagnosis services, existence of individual(s) in the household that require chronic medical care, and having a patient in hospital.
All the statistical analyses were performed using the SPSS statistical software (version 22. Armonk, NY: IBM Corp).
In the study, an informed consent form was completed by each participant and the authors have kept the information confidential.
3. Results
The study was done among the 2400 households in Sistan and Baluchistan province. In the study, most of the households were in Zahedan (34.0 %) and most of them lived in a rural area (70.1). About 91% of the head of households were male and 76% of the headers had a diploma or lower educational degree. Table 1, shows the demographic variables of the 2400 households. According to the results, the mean of age among the head of households was 39.78. As shown in Table 1, most of the households (1509 or 62.8%) was covered by the Iranian health insurance 1509 (62.8%). After that, social security, army, and other insurance covered 587 or 24.4%, 70 or 2.9%, and 53 or 2.2%, respectively. In addition, the findings showed that about 189 households (7.9%) had no basic insurance. According to the results, 1669 (69.6%) of the households had a house and others were tenants. The households use of income (1535 or 64.0%), saving (806 or 33.6%), borrow of family (762 or 31.8%), other ways (461 or 19.2%), insurance cost (408 or 17.0%), borrow of others (354 or 14.8%), and selling assets (245 or 10.2%) was used for financing their heath expenditure in 2017.
Frequency of the Studied Households and Impoverishment Caused Health Expenditure
| Variables | Dimensions | F (%) | Impoverished | |
|---|---|---|---|---|
| No | Yes | |||
| City | Iranshahr | 264 (11) | 249 (94.3) | 15 (5.7) |
| Zabol | 336 (14) | 306 (91.1) | 30 (8.9) | |
| Khash | 192 (8) | 183 (95.3) | 9 (4.7) | |
| Zahedan | 816 (34) | 782 (95.8) | 34 (4.2) | |
| Saravan | 216 (9) | 206 (95.4) | 10 (4.6) | |
| Nikshar | 264 (11) | 262 (99.2) | 2 (0.8) | |
| Chabehar | 312 (13) | 282 (90.4) | 30 (9.6) | |
| Region | Urban | 717 (29.1) | 1602 (95.2) | 81 (4.8) |
| Rural | 1683 (70.1) | 688 (93.2) | 49 (6.8) | |
| Gender of household head | Male | 2200 (91.7) | 2089 (95.5) | 111 (5.0) |
| Female | 200 (8.3) | 118 (90.5) | 19 (9.5) | |
| Employment status of household head | Employed | 1643 (68.4) | 1576 (95.9) | 67 (4.1) |
| Unemployed | 757 (31.6) | 694 (91.7) | 63 (8.3) | |
| Education of household head | Illiterate | 482 (20.1) | 446(92.5) | 36(7.5) |
| Elementary | 376 (15.7) | 355 (94.4) | 21 (5.4) | |
| Guid school | 450 (18.8) | 421 (93.6) | 29 (6.3) | |
| Diploma | 515 (21.5) | 490 (95.1) | 25 (4.9) | |
| Upper diploma | 474 (19.8) | 457 (96.4) | 17 (3.6) | |
| MS/PhD | 10 3(4.3) | 101 (98.1) | 2 (1.9) | |
| Basic insurance | yes | 2211 (92.1) | 2092 (94.6) | 119 (5.4) |
| No | 189 (7.9) | 178 (94.2) | 11 (5.8) | |
| Complementary insurance | yes | 118 (4.9) | 117 (99.1) | 1 (0.09) |
| No | 2282 (95.1) | 2146 (95.0) | 136 (5.0) | |
| Family size | < 2 | 435 (18.1) | 400 (92.0) | 35 (8.0) |
| 3 - 6 | 1780 (74.2) | 1700 (95.5) | 80 (4.5) | |
| > 7 | 185 (7.7) | 170 (91.9) | 15 (8.1) | |
| Economic status | Quintiles 1 | 483 (20.1) | 477 (98.6) | 7 (1.4) |
| Quintiles 2 | 476 (19.8) | 413 (86.8) | 63 (13.2) | |
| Quintiles 3 | 484 (20.1) | 459 (94.8) | 25 (5.2) | |
| Quintiles 4 | 476 (19.8) | 462 (97.0) | 14 (3.0) | |
| Quintiles 5 | 480 (20.0) | 459 (95.6) | 21 (4.4) | |
Results showed that about 152 (0.06%) of the households had an individual older the age of 65 years in their household, which 16 (9.9%) of them face impoverishment. Moreover, about 1058 (44.0%) of the households had a child lower than 5 years, which 49 (4.6%) of the households faced impoverishment. The findings showed that about 154 of the households had a person who was hospitalized in the period of the study, which 19 (12.3%) of them faced impoverishment. In addition, 240 (10.0%) of the households had a person in the households who need heath care in the study period.
According to Table 1, about 130 (5.4%) of the households faced health spending impoverishment in Sistan and Baluchistan in 2017. The shows shows that Chabahar households’ were the highest risk of facing health spending impoverishment (9.6%).
In the study, for multivariate analysis use of Logistic regression and the results are shown in Table 2.
According to Table 2, logistic regression showed the variables relationship with impoverishment among the households. It shows that the households who lived in the rural regions were faced with impoverishment more than the urban area (OR = 0.711; 95% confidence interval [CI], 0.185 - 0.453). Moreover, OR of the households, where their heads were unemployed or unable to work was 2.10, (CI: 1.29 - 3.42 and P = 0.003). As shown in Table 2, the households in the 3rd economic status faced with impoverishment were more than those in the lowest quintile (OR: 6.86, CI= 2.87 - 16.38 and P value = 0.001)
The Association Between the Determinants and Impoverishment Among the Sistan and Baluchestan Householdsa
| Variables | B | S.E. | P Value | Adjusted OR | 95% CI |
|---|---|---|---|---|---|
| Region | |||||
| Urban vs. rural | -0.903 | 0.228 | 0.001 | 0.406 | 0.259 - 0.634 |
| Head’s employment | |||||
| Unemployment vs. employment | 0.572 | 0.243 | 0.019 | 1.772 | 1.100 - 2.855 |
| Economic status | |||||
| 2nd Quintile vs. Lowest | 1.926 | 0.444 | 0.001 | 6.864 | 2.876 - 16.381 |
| Supplementary insurance | |||||
| Having supplementary insurance vs. not having | -1.947 | 1.008 | 0.53 | 0.143 | 0.020 - 1.029 |
| Inpatient medical care expenditures | |||||
| Inpatient medical care expenditures vs. Non-hospitalized | 0.840 | 0.256 | 0.001 | 2.315 | 1.403 - 3.821 |
| Outpatient medical care expenditures | |||||
| Outpatient medical care expenditures vs. nooutpatient medical care expenditures | 4.63 | 1.03 | 0.001 | 102.69 | 13.34 - 784.78 |
| Having dental expenditures vs. not having dental expenditures | 0.866 | 0.240 | 0.001 | 2.377 | 1.484 - 3.806 |
| Having radiology expendituresvs. not having radiology expenditures | 0.899 | 0.242 | 0.001 | 2.456 | 1.528 - 3.950 |
In addition, the use of inpatient and dental services by the households increased facing medical impoverishment (OR: 3.85, CI = 2.31 - 6.43 P = 0.001, and OR: 3.58, CI = 2.27 - 5.65 P = 0.001, respectively). The other variables are shown in Table 2. As shown in Table 2, having supplementary insurance is a protective factor in facing impoverishment and its’ P vale is in significant margin (P = 0.05).
4. Discussion
The study was designed to determine medical impoverishment among 2400 households in Sistan and Baluchistan. The main finding of the study showed that about 5.4% of the households had impoverished due to health care expenditure. The percentage of the households facing impoverishment due to health expenditures has to be lower than 1%, according to Iran's development program; however, the aim has not been reached in this study.
Besides, other studies were done in Iran that confirmed the present study (16, 17). In this regards, a study was done in Shiraz that showed that 7% of households was impoverished by health expenditure (16). It is notable that basic health insurances are weak in coverage of all outpatient services. Also, the studied regions are the poorest regions in the country and sometimes households refuse to receive health care due to poverty and inability to pay. It shows that HTP could not reach their goals absolutely in this province. This is in line with the study by Kien who studied impoverishment associated with non-communicable diseases in urban Hanoi, Vietnam and found that although the poor households in both slum and non-slum areas were at higher risk of experiencing CHE, only the poor households in slum areas were at higher risk of impoverishment due to healthcare spending (18). Moreover, Khan found that the poverty headcount increased by 3.5% due to OOP payments in Bangladesh (19).
Since impoverishment indices offer guidance for developing appropriate health policies and intervention programs to decrease financial inequity (18), it is recommended for health policy makers’ attention to poverty regions.
Based on the findings, living in rural area increase the risk of health related impoverishment among the households. Since households have low access to some health services such as hospital care; therefore, they had to travel to urban areas and pay more of their payment for indirect cost and it lead to households that face with impoverishment. Villagers have lower capacity to pay and less physical and time access to health services. They consequently refer to receive services when the disease has developed. Therefore, the needed services are more expensive and this is the other reason of impoverishment in rural regions. In line with the finding, most of the studies confirm that households in rural region suffer from impoverishment due to health spending (16, 20). Shi found that near 12% of the rural households impoverished because of health care expenditure in china (21). Khammarnia et al. in another study in the southwest of Iran showed that about 24.7% of rural households impoverished due to health expenditure before HTP (16). Furthermore, a study that was performed in Iran showed that the individuals who live in rural areas were more exposed to CHE compared to those in urban areas (20).
In this study, economic status was one of the most important reasons for the households' confronting poverty and the households in the 3rd economic quintile are more likely to be faced with poverty caused health rather than the lowest group. However, the most studies showed that lowest economic group face more than the upper groups (20). A study done in China showed that 36.2 of the households in the lowest economic status were impoverished by health care expenditure (21). The findings of various studies performed in both developing and developed countries have also confirmed the effect of the households' economic status on their being faced with poverty and CHE (16, 22, 23). Another study shows that households with higher income had a higher willing to pay and access ability to health services (24). Poverty reduction policies, which improve the level of total household welfare, can be helpful as well.
Since HTP emphasize on inpatient expenditure and urban and rural inpatient persons only pay 6% or 3% of hospital cost, respectively, the study shows that some of the households who used of inpatient care are faced with impoverishment. It is notable that most of the inpatient cases had to travel between 200 to 600 kilometers to receive hospital services, therefore, they had to pay indirect cost and direct non related health services cost such as expenditures for food, residence in cities, and etc. It has been shown repeatedly that after HTP, inpatient cost decreased (11). Nevertheless, it is needed to increase access to health services for people in poor regions. In this regards, Shi (21) found that having a hospitalized member in the household is a main factor in health impoverishment and about 29.7 of the households with a hospitalized member are impoverished by health care expenditure.
According to the results, use of outpatient services such as radiology and dental care by the households led to impoverishment. It is notable that HTP only cover inpatient care. Outpatient services are not completely in insurance coverage. On the other hands, one of the HTP's phases was the tariffs’ actualization and result in increased expenditure of outpatient services, which individuals have to pay. Therefore, although HTP decreased inpatient costs, it increased outpatient care costs. Therefore, same as inpatient care, it is recommended that outpatient care is mostly covered by insurance. According to other studies done before HTP, the outpatient costs lead to impoverishment in Iran (16). In Vietnam, the households with outpatient treatment consumed less food and educational services compared to those without outpatient treatment. The most significant decrease occurred in the lowest income quintile of the population (25).
According to the study results, households where their head was unemployed faced impoverishment more rather than other households. These households do not have enough money for payment, especially for health care; therefore, they are pushed to the under poverty line. In line with the study, Shi found that households whose head was unemployed were more likely to incur financial catastrophe and impoverishment due to health expenditure (21). In addition, other studies confirm the present study (3, 4). It is notable that the unemployment rate in the Sistan and Baluchistan province is the highest rate in Iran (26). Therefore, it is recommended that governmental managers pay more to attention to the province and provide more employment opportunities.
The study showed that supplementary insurance was a protective factor to impoverishment. Although the positive effect of this kind of insurance is confirmed in the study; however, due to economic difficulties, the low percent of households has the ability to buy it. It is needed for most households to get covered with that and in this regard, governmental organization should support households. Most of the studies confirmed the protective effect of supplementary insurance (27-29).
The main limitation of the present study was a probability of over- or under-reporting of the expenditures as well as recall biases. However, it was attempted to minimize these problems through shortening the recall period and also reconfirming the studied expenditure data by randomly contacting the households who had completed the questionnaires. Since the present study was done in one province, the generalizability is low and extending results to other regions should be done with caution.
4.1. Conclusions
In general, after the implementation of HTP, a high percentage of the households are still facing medical impoverishment, therefore, the last 2 5-Year national development plans goals have not been achieved in this regard. It seems that the coverage of outpatient health services and full implementation of health referral system across the country are necessary. Furthermore, health policy makers should pay more attention to rural areas and allocate healthcare resources among region equity. Finally, it is recommended to do the research in other regions of Iran.
Acknowledgements
References
-
1.
Wagstaff A, van Doorslaer E. Catastrophe and impoverishment in paying for health care: with applications to Vietnam 1993-1998. Health Econ. 2003;12(11):921-34. [PubMed ID: 14601155]. https://doi.org/10.1002/hec.776.
-
2.
Russell S. The economic burden of illness for households in developing countries: a review of studies focusing on malaria, tuberculosis, and human immunodeficiency virus/acquired immunodeficiency syndrome. Am J Trop Med Hyg. 2004;71(2 Suppl):147-55. [PubMed ID: 15331831].
-
3.
Somkotra T, Lagrada LP. Which households are at risk of catastrophic health spending: experience in Thailand after universal coverage. Health Aff (Millwood). 2009;28(3):w467-78. [PubMed ID: 19336470]. https://doi.org/10.1377/hlthaff.28.3.w467.
-
4.
Gotsadze G, Zoidze A, Rukhadze N. Household catastrophic health expenditure: evidence from Georgia and its policy implications. BMC Health Serv Res. 2009;9:69. [PubMed ID: 19400939]. https://doi.org/10.1186/1472-6963-9-69.
-
5.
Rashidian A. Universal health coverage in Iran. WHO Iran Newsletter; 2010.
-
6.
Ferdosi M, Kabiri S, Keyvanara M, Yarmohammadian MH. Challenges of Iran Health Transformation Plan about Inpatients Payment: Viewpoint of Experts. Health Scope. 2017;6(3).
-
7.
Khammarnia M, Amani Z, Hajmohammadi M, Ansari-Moghadam A, Eslahi M. A Survey of Iron Supplementation Consumption and its Related Factors in High School Students in Southeast Iran, 2015. Malays J Med Sci. 2016;23(5):57-64. [PubMed ID: 27904426]. https://doi.org/10.21315/mjms2016.23.5.8.
-
8.
Abolhallaje M, Jafari M, Seyedin H, Salehi M. Financial Management Reforms in the Health Sector: A Comparative Study Between Cash-based and Accrual-based Accounting Systems. Iran Red Crescent Med J. 2014;16(10). e15472. [PubMed ID: 25763194]. https://doi.org/10.5812/ircmj.15472.
-
9.
Kabir MJ, Abolhallaje M, Bastani P, Keshavarzi A. Necessary Requirements for Implementation of Financial Reform in the Iranian Health Sector. Health Scope. 2017;In Press(In Press). https://doi.org/10.5812/jhealthscope.14148.
-
10.
Moradi-Lakeh M, Vosoogh-Moghaddam A. Health sector evolution plan in Iran; equity and sustainability concerns. Int J Health Policy Manag. 2015;4(10):637.
-
11.
Piroozi B, Moradi G, Nouri B, Mohamadi Bolbanabad A, Safari H. Catastrophic Health Expenditure After the Implementation of Health Sector Evolution Plan: A Case Study in the West of Iran. Int J Health Policy Manag. 2016;5(7):417-23. [PubMed ID: 27694669]. https://doi.org/10.15171/ijhpm.2016.31.
-
12.
Ahmadi S, Sabori khah H, Darvishi H, Jabari H. Spatial Analysis of Iranian Provinces in Health Indicators. Q J Region Plann. 2014;4:31-44.
-
13.
Murray CJL, Xu K, Klavus J, Kawabata K, Hanvoravongchai P, Zeramdini R, et al. Assessing the distribution of household financial contributions to the health system: concepts and empirical application. Health systems performance assessment: debates, methods and empiricism. 12. Geneva: World Health Organization; 2003.
-
14.
Kavosi Z, Rashidian A, Pourreza A, Majdzadeh R, Pourmalek F, Hosseinpour AR, et al. Inequality in household catastrophic health care expenditure in a low-income society of Iran. Health Policy Plan. 2012;27(7):613-23. [PubMed ID: 22279081]. https://doi.org/10.1093/heapol/czs001.
-
15.
Knaul FM, Arreola-Ornelas H, Méndez-Carniado O, Bryson-Cahn C, Barofsky J, Maguire R, et al. Evidence is good for your health system: policy reform to remedy catastrophic and impoverishing health spending in Mexico. Lancet. 2006;368(9549):1828-41. https://doi.org/10.1016/s0140-6736(06)69565-2.
-
16.
Khammarnia M, Keshtkaran A, Kavosi Z, Hayati R. The Household Health Spending and Impoverishment: Findings from the Households Survey in Shiraz, Iran. Bangladesh Med Res Council Bull. 2015;40(2):58. https://doi.org/10.3329/bmrcb.v40i2.25184.
-
17.
Yazdi Feyzabadi V, Mehrolhassani MH, Haghdoost AA, Bahrampour M. The trend of impoverishing effects of out-of-pocket health expenditure in Iranian provinces in 2008-2014. Iran J Epidemiol. 2017;12(5):20-31.
-
18.
Kien VD, Van Minh H, Giang KB, Dao A, Ng N. Socioeconomic inequalities in catastrophic health expenditure and impoverishment associated with non-communicable diseases in urban Hanoi, Vietnam. Int J Equity Health. 2016;15(1):169.
-
19.
Khan JAM, Ahmed S, Evans TG. Catastrophic healthcare expenditure and poverty related to out-of-pocket payments for healthcare in Bangladesh—an estimation of financial risk protection of universal health coverage. Health Policy Plann. 2017;32(8):1102-10. https://doi.org/10.1093/heapol/czx048.
-
20.
Moghadam MN, Banshi M, Javar MA, Amiresmaili M, Ganjavi S. Iranian Household Financial Protection against Catastrophic Health Care Expenditures. Iran J Public Health. 2012;41(9):62-70. [PubMed ID: 23193508].
-
21.
Shi W, Chongsuvivatwong V, Geater A, Zhang J, Zhang H, Brombal D. Effect of household and village characteristics on financial catastrophe and impoverishment due to health care spending in Western and Central Rural China: A multilevel analysis. Health Res Policy Syst. 2011;9:16. [PubMed ID: 21466714]. https://doi.org/10.1186/1478-4505-9-16.
-
22.
Kavosi Z, Keshtkaran A, Hayati R, Ravangard R, Khammarnia M. Household financial contribution to the health System in Shiraz, Iran in 2012. Int J Health Policy Manag. 2014;3(5):243-9. [PubMed ID: 25337598]. https://doi.org/10.15171/ijhpm.2014.87.
-
23.
Kien VD, Van Minh H, Giang KB, Dao A, Tuan LT, Ng N. Socioeconomic inequalities in catastrophic health expenditure and impoverishment associated with non-communicable diseases in urban Hanoi, Vietnam. Int J Equity Health. 2016;15(1):169. [PubMed ID: 27737663]. https://doi.org/10.1186/s12939-016-0460-3.
-
24.
Javan-Noughabi J, Kavosi Z, Faramarzi A, Khammarnia M. Identification determinant factors on willingness to pay for health services in Iran. Health Econ Rev. 2017;7(1):40. [PubMed ID: 29159659]. https://doi.org/10.1186/s13561-017-0179-x.
-
25.
Nguyen KT, Khuat OT, Ma S, Pham DC, Khuat GT, Ruger JP. Coping with health care expenses among poor households: evidence from a rural commune in Vietnam. Soc Sci Med. 2012;74(5):724-33. [PubMed ID: 22305805]. https://doi.org/10.1016/j.socscimed.2011.10.027.
-
26.
Zahedan.irib. Broadcasting SBP. 2017. Available from: http://zahedan.irib.ir.
-
27.
Boone J. Basic versus supplementary health insurance: Moral hazard and adverse selection. J Public Econ. 2015;128:50-8. https://doi.org/10.1016/j.jpubeco.2015.05.009.
-
28.
Mousavi B, Soroush M, Maftoon F, Mohammad K, Ganjparvar Z. Satisfaction of Supplementary Insurance and Medical Services during Trips in War Survivors and their Families. Int J Travel Med Glob Health. 2016;4(2):65-8. https://doi.org/10.20286/ijtmgh-04026.
-
29.
Kaplan G, Shahar Y, Tal O. Supplementary Health Insurance from the consumer point of view: Are Israelis consumers doing an informed rational choice when purchasing Supplementary Health Insurance? Health Policy. 2017;121(6):708-14. [PubMed ID: 28431783]. https://doi.org/10.1016/j.healthpol.2017.03.019.

