A Concise Paradigm on Radical Hysterectomy: The Comprehensive Anatomy of Parametrium, Paracolpium and the Pelvic Autonomic Nerve System and Its Surgical Implication
Abstract
:1. Introduction
2. Results
2.1. In-Depth Literature Analysis of the Parametrium and Paracolpium
2.2. The New Three-Dimensional Precise Anatomic Description of the Parametrium and Paracolpium as a Result of Our Anatomical and Surgical Studies
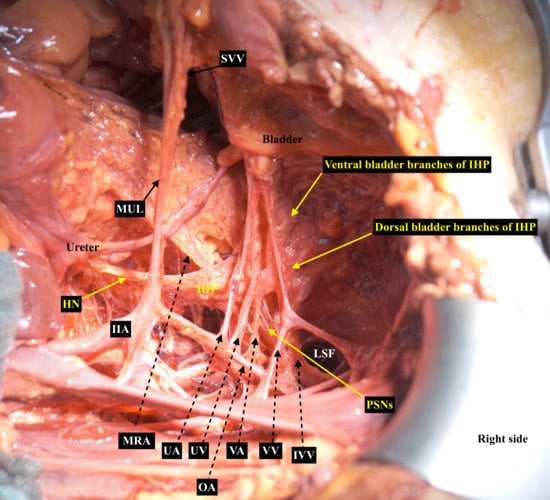
2.3. The Pelvic Autonomic Nervous System and Its Course Across the Paracolpium
2.4. The Surgical Impact of the Comprehensive Anatomy of Paracolpium and the Pelvic Autonomic Nervous System
3. Discussion
4. Materials and Methods
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Wertheim, E. The extended abdominal operation for carcinoma uteri (based on 500 operative cases). Am. J. Obstet. Dis. Women Child. 1912, 66, 169–232. [Google Scholar]
- Fritsch, H.; Zwierzina, M.; Riss, P. Accuracy of concepts in female pelvic floor anatomy: Facts and myths! World J. Urol. 2012, 30, 429–435. [Google Scholar] [CrossRef]
- Fritsch, H.; Hötzinger, H. Tomographical anatomy of the pelvis, visceral pelvic connective tissue, and its compartments. Clin. Anat. 1995, 8, 17–24. [Google Scholar] [CrossRef] [PubMed]
- Murakami, N.; Norihisa, Y.; Isohashi, F.; Murofushi, K.; Ariga, T.; Kato, T.; Inaba, K.; Okamoto, H.; Ito, Y.; Toita, T.; et al. Proposed definition of the vaginal cuff and paracolpium clinical target volume in postoperative uterine cervical cancer. Pract. Radiat. Oncol. 2016, 6, 5–11. [Google Scholar] [CrossRef]
- Ceccaroni, M.; Clarizia, R.; Roviglione, G.; Ruffo, G. Neuro-anatomy of the posterior parametrium and surgical considerations for a nerve-sparing approach in radical pelvic surgery. Surg Endosc. 2013, 27, 4386–4394. [Google Scholar] [CrossRef] [PubMed]
- Ramanah, R.; Berger, M.B.; Parratte, B.M.; DeLancey, J.O. Anatomy and histology of apical support: A literature review concerning cardinal and uterosacral ligaments. Int. Urogynecol. J. 2012, 23, 1483–1494. [Google Scholar] [CrossRef] [Green Version]
- Yabuki, Y.; Asamoto, A.; Hoshiba, T.; Nishimoto, H.; Nishikawa, Y.; Nakajima, T. Radical hysterectomy: An anatomic evaluation of parametrial dissection. Gynecol. Oncol. 2000, 77, 155–163. [Google Scholar] [CrossRef] [PubMed]
- Querleu, D.; Morrow, C.P. Classification of radical hysterectomy. Lancet Oncol. 2008, 9, 297–303. [Google Scholar] [CrossRef]
- Querleu, D.; Cibula, D.; Abu-Rustum, N.R. Update on the Querleu–Morrow Classification of Radical Hysterectomy. Ann. Surg. Oncol. 2017, 24, 3406–3412. [Google Scholar] [CrossRef] [PubMed]
- Yabuki, Y.; Takagi, H. Cardinal Ligament and Transverse Cervical Ligament are not Synonymous. J. Clin Med. Sci. 2018, 2, 1. [Google Scholar]
- Muallem, M.Z.; Diab, Y.; Sehouli, J.; Fujii, S. Nerve-sparing radical hysterectomy: Steps to standardize surgical technique. Int. J. Gynecol. Cancer 2019, 29, 1203–1208. [Google Scholar] [CrossRef] [PubMed]
- Muallem, M.Z.; Armbrust, R.; Neymeyer, J.; Miranda, A.; Muallem, J. Nerve Sparing Radical Hysterectomy: Short-Term Oncologic, Surgical, and Functional Outcomes. Cancers 2020, 12, 483. [Google Scholar] [CrossRef] [Green Version]
- Piver, S.; Rutledge, F.; Smith, J.P. Five classes of extended radical hysterectomy for women with cervical cancer. Obstet. Gynecol. 1974, 44, 265–272. [Google Scholar]
- Fujii, S.; Sekiyama, K. Precise Neurovascular Anatomy for Radical Hysterectomy; Springer Nature, Singapore Pte Ltd.: Singapore, 2020; p. 56. ISBN 978-981-13-8097-6. [Google Scholar]
- Girardi, F.; Lichtenegger, W.; Tamussino, K.; Haas, J. The importance of parametrial lymph nodes in the treatment of cervical cancer. Gynecol. Oncol. 1989, 34, 206–211. [Google Scholar] [CrossRef]
- Benedetti-Panici, P.; Maneschi, F.; D’Andrea, G.; Cutillo, G.; Rabitti, C.; Congiu, M.; Coronetta, F.; Capelli, A. Early cervical carcinoma. Cancer 2000, 88, 2267–2274. [Google Scholar] [CrossRef]
- Palfalvi, L.; Ungar, L. Laterally extended parametrectomy (LEP), the technique for radical pelvic sidewall dissection: Feasibility, technique, and results. Int. J. Gynecol. Cancer 2003, 13, 914–917. [Google Scholar] [CrossRef] [PubMed]
- Querleu, D.; Narducci, F.; Poulard, V.; Lacaze, S.; Occelli, B.; Leblanc, E.; Cosson, M. Modified radical vaginal hysterectomy with or without laparoscopic nerve-sparing dissection: A comparative study. Gynecol. Oncol. 2002, 85, 154–158. [Google Scholar] [CrossRef] [PubMed]
- Cibula, D.; Abu-Rustum, N.R.; Benedetti-Panici, P.; Köhler, C.; Raspagliesi, F.; Querleu, D.; Morrow, C.P. The new classification system of radical hysterectomy: Emphasis on a three-dimensional anatomic template for parametrial resection. Gynecol. Oncol. 2011, 122, 264–268. [Google Scholar] [CrossRef]
- Ercoli, A.; Delmas, V.; Gadonneix, P.; Fanfani, F.; Villet, R.; Paparella, P.; Mancuso, S.; Scambia, G. Classical and nerve-sparing radical hysterectomy: An evaluation of the risk of injury to the autonomous pelvic nerves. Surg. Radiol. Anat. 2003, 3–4, 200–206. [Google Scholar] [CrossRef] [PubMed]
- Muallem, M.Z. Nerve Sparing Radical Hysterectomy- Muallem Technique. Available online: https://www.youtube.com/watch?v=dr675cXra9c (accessed on 5 July 2020).
- Fujii, S.; Takakura, K.; Matsumura, N.; Higuchi, T.; Yura, S.; Mandai, M.; Baba, T. Precise anatomy of the vesicouterine ligament for radical hysterectomy. Gynecol. Oncol. 2007, 104, 186–191. [Google Scholar]
- Ralph, G.; Winter, R.; Michelitsch, L. Radicality of parametrial resection and dysfunction of the lower urinary tract after radical hysterectomy. Eur. J. Gynecol Oncol. 1991, 12, 27–30. [Google Scholar]
- Hinata, N.; Hieda, K.; Sasaki, H.; Kurokawa, T.; Miyake, H.; Fujisawa, M.; Murakami, G.; Fujimiya, M. Nerves and fasciae in and around the paracolpium or paravaginal tissue: An immunohistochemical study using elderly donated cadavers. Anat. Cell Biol. 2014, 47, 44–54. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Anson, B.J.; McVay, C.B. Surgical Anatomy, 6th ed; WB Saunders: Philadelphia, PA, USA, 1984; p. 556. [Google Scholar]
- Fröber, R. Surgical anatomy of the ureter. BJU Int. 2007, 100, 949–965. [Google Scholar] [CrossRef] [PubMed]
- Bhatla, N.; Berek, J.S.; Fredes, M.C.; Denny, L.A.; Grenman, S.; Karunaratne, K.; Kehoe, S.T.; Konishi, I.; Olawaiye, A.B.; Prat, J.; et al. Revised FIGO staging for carcinoma of the cervix uteri. Int. J. Gynaecol. Obstet. 2019, 145, 129–135. [Google Scholar] [CrossRef] [PubMed]
- Quinn, M.A.; Benedet, J.L.; Odicino, F.; Maisonneuve, P.; Beller, U.; Creasman, W.T.; Heintz, A.P.; Ngan, H.Y.; Pecorelli, S. Carcinoma of the cervix uteri. Int. J. Gynecol. Obstet. 2006, 95, 43–103. [Google Scholar] [CrossRef]





© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Muallem, M.Z.; Jöns, T.; Seidel, N.; Sehouli, J.; Diab, Y.; Querleu, D. A Concise Paradigm on Radical Hysterectomy: The Comprehensive Anatomy of Parametrium, Paracolpium and the Pelvic Autonomic Nerve System and Its Surgical Implication. Cancers 2020, 12, 1839. https://0-doi-org.brum.beds.ac.uk/10.3390/cancers12071839
Muallem MZ, Jöns T, Seidel N, Sehouli J, Diab Y, Querleu D. A Concise Paradigm on Radical Hysterectomy: The Comprehensive Anatomy of Parametrium, Paracolpium and the Pelvic Autonomic Nerve System and Its Surgical Implication. Cancers. 2020; 12(7):1839. https://0-doi-org.brum.beds.ac.uk/10.3390/cancers12071839
Chicago/Turabian StyleMuallem, Mustafa Zelal, Thomas Jöns, Nadja Seidel, Jalid Sehouli, Yasser Diab, and Denis Querleu. 2020. "A Concise Paradigm on Radical Hysterectomy: The Comprehensive Anatomy of Parametrium, Paracolpium and the Pelvic Autonomic Nerve System and Its Surgical Implication" Cancers 12, no. 7: 1839. https://0-doi-org.brum.beds.ac.uk/10.3390/cancers12071839