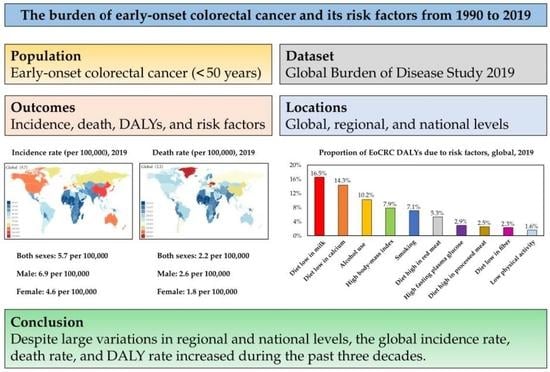
The Burden of Early-Onset Colorectal Cancer and Its Risk Factors from 1990 to 2019: A Systematic Analysis for the Global Burden of Disease Study 2019
Abstract
:Simple Summary
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Source
2.2. Definition of EoCRC
2.3. Estimation of Incidence, Deaths, and DALYs
2.4. Sociodemographic Index (SDI)
2.5. Risk Factors
3. Results
3.1. Incidence, Deaths, and DALYs in 2019
3.1.1. Global Level
3.1.2. Regional Level
3.1.3. National Level
3.2. The Impact of Sex and SDI on Incidence Rate, Death Rate, and DALY Rate
3.3. Risk Factors
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Akimoto, N.; Ugai, T.; Zhong, R.; Hamada, T.; Fujiyoshi, K.; Giannakis, M.; Wu, K.; Cao, Y.; Ng, K.; Ogino, S. Rising incidence of early-onset colorectal cancer—A call to action. Nat. Rev. Clin. Oncol. 2021, 18, 230–243. [Google Scholar] [CrossRef] [PubMed]
- Siegel, R.L.; Medhanie, G.A.; Fedewa, S.A.; Jemal, A. State Variation in Early-Onset Colorectal Cancer in the United States, 1995–2015. J. Natl. Cancer Inst. 2019, 111, 1104–1106. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Siegel, R.L.; Miller, K.D.; Jemal, A. Colorectal Cancer Mortality Rates in Adults Aged 20 to 54 Years in the United States, 1970–2014. JAMA 2017, 318, 572–574. [Google Scholar] [CrossRef] [PubMed]
- Vuik, F.E.; Nieuwenburg, S.A.; Bardou, M.; Lansdorp-Vogelaar, I.; Dinis-Ribeiro, M.; Bento, M.J.; Zadnik, V.; Pellise, M.; Esteban, L.; Kaminski, M.F.; et al. Increasing incidence of colorectal cancer in young adults in Europe over the last 25 years. Gut 2019, 68, 1820–1826. [Google Scholar] [CrossRef]
- Siegel, R.L.; Torre, L.A.; Soerjomataram, I.; Hayes, R.B.; Bray, F.; Weber, T.K.; Jemal, A. Global patterns and trends in colorectal cancer incidence in young adults. Gut 2019, 68, 2179–2185. [Google Scholar] [CrossRef] [Green Version]
- GBD 2019 Demographics Collaborators. Global age-sex-specific fertility, mortality, healthy life expectancy (HALE), and population estimates in 204 countries and territories, 1950–2019: A comprehensive demographic analysis for the Global Burden of Disease Study 2019. Lancet 2020, 396, 1160–1203. [Google Scholar] [CrossRef]
- GBD 2019 Diseases and Injuries Collaborators. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020, 396, 1204–1222. [Google Scholar] [CrossRef]
- GBD 2019 Risk Factor Collaborators. Global burden of 87 risk factors in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020, 396, 1223–1249. [Google Scholar] [CrossRef]
- GBD 2019 Colorectal Cancer Collaborators. Global, regional, and national burden of colorectal cancer and its risk factors, 1990-2019: A systematic analysis for the Global Burden of Disease Study 2019. Lancet Gastroenterol. Hepatol. 2022, 7, 627–647. [Google Scholar] [CrossRef]
- Sharma, R. A comparative examination of colorectal cancer burden in European Union, 1990–2019: Estimates from Global Burden of Disease 2019 Study. Int. J. Clin. Oncol. 2022, 1–12. [Google Scholar] [CrossRef]
- Nejadghaderi, S.A.; Roshani, S.; Mohammadi, E.; Yoosefi, M.; Rezaei, N.; Esfahani, Z.; Azadnajafabad, S.; Ahmadi, N.; Shahin, S.; Kazemi, A.; et al. The global, regional, and national burden and quality of care index (QCI) of colorectal cancer; a global burden of disease systematic analysis 1990–2019. PLoS ONE 2022, 17, e0263403. [Google Scholar] [CrossRef] [PubMed]
- Global Burden of Disease Cancer Collaboration; Kocarnik, J.M.; Compton, K.; Dean, F.E.; Fu, W.; Gaw, B.L.; Harvey, J.D.; Henrikson, H.J.; Lu, D.; Pennini, A.; et al. Cancer Incidence, Mortality, Years of Life Lost, Years Lived With Disability, and Disability-Adjusted Life Years for 29 Cancer Groups From 2010 to 2019: A Systematic Analysis for the Global Burden of Disease Study 2019. JAMA Oncol. 2022, 8, 420–444. [Google Scholar] [CrossRef] [PubMed]
- WHO. International Classification of Diseases (ICD). 2018. Available online: https://www.who.int/standards/classifications/classification-of-diseases (accessed on 15 July 2022).
- Yamauchi, M.; Morikawa, T.; Kuchiba, A.; Imamura, Y.; Qian, Z.R.; Nishihara, R.; Liao, X.; Waldron, L.; Hoshida, Y.; Huttenhower, C.; et al. Assessment of colorectal cancer molecular features along bowel subsites challenges the conception of distinct dichotomy of proximal versus distal colorectum. Gut 2012, 61, 847–854. [Google Scholar] [CrossRef]
- GBD 2017 Colorectal Cancer Collaborators. The global, regional, and national burden of colorectal cancer and its attributable risk factors in 195 countries and territories, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet Gastroenterol. Hepatol. 2019, 4, 913–933. [Google Scholar] [CrossRef] [Green Version]
- Rosato, V.; Bosetti, C.; Levi, F.; Polesel, J.; Zucchetto, A.; Negri, E.; La Vecchia, C. Risk factors for young-onset colorectal cancer. Cancer Causes Control 2013, 24, 335–341. [Google Scholar] [CrossRef]
- Archambault, A.N.; Lin, Y.; Jeon, J.; Harrison, T.A.; Bishop, D.T.; Brenner, H.; Casey, G.; Chan, A.T.; Chang-Claude, J.; Figueiredo, J.C.; et al. Nongenetic Determinants of Risk for Early-Onset Colorectal Cancer. JNCI Cancer Spectr. 2021, 5, pkab029. [Google Scholar] [CrossRef] [PubMed]
- Kim, N.H.; Jung, Y.S.; Yang, H.J.; Park, S.K.; Park, J.H.; Park, D.I.; Sohn, C.I. Prevalence of and Risk Factors for Colorectal Neoplasia in Asymptomatic Young Adults (20–39 Years Old). Clin. Gastroenterol. Hepatol. 2019, 17, 115–122. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Buc, E.; Kwiatkowski, F.; Alves, A.; Panis, Y.; Mantion, G.; Slim, K. Tobacco smoking: A factor of early onset of colorectal cancer. Dis. Colon Rectum 2006, 49, 1893–1896. [Google Scholar] [CrossRef]
- Chang, V.C.; Cotterchio, M.; De, P.; Tinmouth, J. Risk factors for early-onset colorectal cancer: A population-based case-control study in Ontario, Canada. Cancer Causes Control 2021, 32, 1063–1083. [Google Scholar] [CrossRef]
- Li, H.; Boakye, D.; Chen, X.; Hoffmeister, M.; Brenner, H. Association of Body Mass Index with Risk of Early-Onset Colorectal Cancer: Systematic Review and Meta-Analysis. Am. J. Gastroenterol. 2021, 116, 2173–2183. [Google Scholar] [CrossRef]
- Sung, J.J.; Ng, S.C.; Chan, F.K.; Chiu, H.M.; Kim, H.S.; Matsuda, T.; Ng, S.S.; Lau, J.Y.; Zheng, S.; Adler, S.; et al. An updated Asia Pacific Consensus Recommendations on colorectal cancer screening. Gut 2015, 64, 121–132. [Google Scholar] [CrossRef]
- Chen, F.W.; Sundaram, V.; Chew, T.A.; Ladabaum, U. Advanced-Stage Colorectal Cancer in Persons Younger than 50 Years Not Associated with Longer Duration of Symptoms or Time to Diagnosis. Clin. Gastroenterol. Hepatol. 2017, 15, 728–737.e723. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yang, W.; Liu, L.; Masugi, Y.; Qian, Z.R.; Nishihara, R.; Keum, N.; Wu, K.; Smith-Warner, S.; Ma, Y.; Nowak, J.A.; et al. Calcium intake and risk of colorectal cancer according to expression status of calcium-sensing receptor (CASR). Gut 2018, 67, 1475–1483. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Fang, Y.J.; Feng, X.L.; Abulimiti, A.; Huang, C.Y.; Luo, H.; Zhang, N.Q.; Chen, Y.M.; Zhang, C.X. Higher intakes of dietary vitamin D, calcium and dairy products are inversely associated with the risk of colorectal cancer: A case-control study in China. Br. J. Nutr. 2020, 123, 699–711. [Google Scholar] [CrossRef] [PubMed]
- Iamartino, L.; Elajnaf, T.; Kallay, E.; Schepelmann, M. Calcium-sensing receptor in colorectal inflammation and cancer: Current insights and future perspectives. World J. Gastroenterol. 2018, 24, 4119–4131. [Google Scholar] [CrossRef]
- Iamartino, L.; Elajnaf, T.; Gall, K.; David, J.; Manhardt, T.; Heffeter, P.; Grusch, M.; Derdak, S.; Baumgartner-Parzer, S.; Schepelmann, M.; et al. Effects of pharmacological calcimimetics on colorectal cancer cells over-expressing the human calcium-sensing receptor. Biochim. Biophys. Acta Mol. Cell Res. 2020, 1867, 118836. [Google Scholar] [CrossRef]
- Ma, J.; Giovannucci, E.; Pollak, M.; Chan, J.M.; Gaziano, J.M.; Willett, W.; Stampfer, M.J. Milk intake, circulating levels of insulin-like growth factor-I, and risk of colorectal cancer in men. J. Natl. Cancer Inst. 2001, 93, 1330–1336. [Google Scholar] [CrossRef] [Green Version]
- Kim, H.; Lipsyc-Sharf, M.; Zong, X.; Wang, X.; Hur, J.; Song, M.; Wang, M.; Smith-Warner, S.A.; Fuchs, C.; Ogino, S.; et al. Total Vitamin D Intake and Risks of Early-Onset Colorectal Cancer and Precursors. Gastroenterology 2021, 161, 1208–1217.e1209. [Google Scholar] [CrossRef]
- Schumacher, A.J.; Chen, Q.; Attaluri, V.; McLemore, E.C.; Chao, C.R. Metabolic Risk Factors Associated with Early-Onset Colorectal Adenocarcinoma: A Case-Control Study at Kaiser Permanente Southern California. Cancer Epidemiol. Biomark. Prev. 2021, 30, 1792–1798. [Google Scholar] [CrossRef]
- Celind, J.; Ohlsson, C.; Bygdell, M.; Nethander, M.; Kindblom, J.M. Childhood Body Mass Index Is Associated with Risk of Adult Colon Cancer in Men: An Association Modulated by Pubertal Change in Body Mass Index. Cancer Epidemiol. Biomark. Prev. 2019, 28, 974–979. [Google Scholar] [CrossRef] [Green Version]
- Matsui, S.; Okabayashi, K.; Tsuruta, M.; Shigeta, K.; Seishima, R.; Ishida, T.; Kondo, T.; Suzuki, Y.; Hasegawa, H.; Shimoda, M.; et al. Interleukin-13 and its signaling pathway is associated with obesity-related colorectal tumorigenesis. Cancer Sci. 2019, 110, 2156–2165. [Google Scholar] [CrossRef] [PubMed]
- Qin, Y.; Roberts, J.D.; Grimm, S.A.; Lih, F.B.; Deterding, L.J.; Li, R.; Chrysovergis, K.; Wade, P.A. An obesity-associated gut microbiome reprograms the intestinal epigenome and leads to altered colonic gene expression. Genome Biol. 2018, 19, 7. [Google Scholar] [CrossRef] [PubMed]
- Ye, P.; Xi, Y.; Huang, Z.; Xu, P. Linking Obesity with Colorectal Cancer: Epidemiology and Mechanistic Insights. Cancers 2020, 12, 1408. [Google Scholar] [CrossRef] [PubMed]
- Elangovan, A.; Skeans, J.; Landsman, M.; Ali, S.M.J.; Elangovan, A.G.; Kaelber, D.C.; Sandhu, D.S.; Cooper, G.S. Colorectal Cancer, Age, and Obesity-Related Comorbidities: A Large Database Study. Dig. Dis. Sci. 2021, 66, 3156–3163. [Google Scholar] [CrossRef] [PubMed]
- Ali Khan, U.; Fallah, M.; Sundquist, K.; Sundquist, J.; Brenner, H.; Kharazmi, E. Risk of colorectal cancer in patients with diabetes mellitus: A Swedish nationwide cohort study. PLoS Med. 2020, 17, e1003431. [Google Scholar] [CrossRef]
- Wu, J.; Chen, J.; Xi, Y.; Wang, F.; Sha, H.; Luo, L.; Zhu, Y.; Hong, X.; Bu, S. High glucose induces epithelial-mesenchymal transition and results in the migration and invasion of colorectal cancer cells. Exp. Ther. Med. 2018, 16, 222–230. [Google Scholar] [CrossRef] [Green Version]
- Chen, Y.C.; Ou, M.C.; Fang, C.W.; Lee, T.H.; Tzeng, S.L. High Glucose Concentrations Negatively Regulate the IGF1R/Src/ERK Axis through the MicroRNA-9 in Colorectal Cancer. Cells 2019, 8, 326. [Google Scholar] [CrossRef] [Green Version]
- Ran, H.; Zhu, Y.; Deng, R.; Zhang, Q.; Liu, X.; Feng, M.; Zhong, J.; Lin, S.; Tong, X.; Su, Q. Stearoyl-CoA desaturase-1 promotes colorectal cancer metastasis in response to glucose by suppressing PTEN. J. Exp. Clin. Cancer Res. 2018, 37, 54. [Google Scholar] [CrossRef]
- Syed, A.R.; Thakkar, P.; Horne, Z.D.; Abdul-Baki, H.; Kochhar, G.; Farah, K.; Thakkar, S. Old vs. new: Risk factors predicting early onset colorectal cancer. World J. Gastrointest. Oncol. 2019, 11, 1011–1020. [Google Scholar] [CrossRef]
- Rossi, M.; Jahanzaib Anwar, M.; Usman, A.; Keshavarzian, A.; Bishehsari, F. Colorectal Cancer and Alcohol Consumption-Populations to Molecules. Cancers 2018, 10, 38. [Google Scholar] [CrossRef] [Green Version]
- Hamada, T.; Nowak, J.A.; Masugi, Y.; Drew, D.A.; Song, M.; Cao, Y.; Kosumi, K.; Mima, K.; Twombly, T.S.; Liu, L.; et al. Smoking and Risk of Colorectal Cancer Sub-Classified by Tumor-Infiltrating T Cells. J. Natl. Cancer Inst. 2019, 111, 42–51. [Google Scholar] [CrossRef] [PubMed]
- Ugai, T.; Vayrynen, J.P.; Haruki, K.; Akimoto, N.; Lau, M.C.; Zhong, R.; Kishikawa, J.; Vayrynen, S.A.; Zhao, M.; Fujiyoshi, K.; et al. Smoking and Incidence of Colorectal Cancer Subclassified by Tumor-Associated Macrophage Infiltrates. J. Natl. Cancer Inst. 2021, 114, 68–77. [Google Scholar] [CrossRef] [PubMed]
- Gurjao, C.; Zhong, R.; Haruki, K.; Li, Y.Y.; Spurr, L.F.; Lee-Six, H.; Reardon, B.; Ugai, T.; Zhang, X.; Cherniack, A.D.; et al. Discovery and Features of an Alkylating Signature in Colorectal Cancer. Cancer Discov. 2021, 11, 2446–2455. [Google Scholar] [CrossRef] [PubMed]
- EuroSurg, C. Body mass index and complications following major gastrointestinal surgery: A prospective, international cohort study and meta-analysis. Colorectal Dis. 2018, 20, O215–O225. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Low, E.E.; Demb, J.; Liu, L.; Earles, A.; Bustamante, R.; Williams, C.D.; Provenzale, D.; Kaltenbach, T.; Gawron, A.J.; Martinez, M.E.; et al. Risk Factors for Early-Onset Colorectal Cancer. Gastroenterology 2020, 159, 492–501.e497. [Google Scholar] [CrossRef]
- REACCT Collaborative; Zaborowski, A.M.; Abdile, A.; Adamina, M.; Aigner, F.; d’Allens, L.; Allmer, C.; Alvarez, A.; Anula, R.; Andric, M.; et al. Characteristics of Early-Onset vs Late-Onset Colorectal Cancer: A Review. JAMA Surg. 2021, 156, 865–874. [Google Scholar] [CrossRef]
- Foppa, C.; Tamburello, S.; Maroli, A.; Carvello, M.; Poliani, L.; Laghi, L.; Malesci, A.; Montorsi, M.; Perea, J.; Spinelli, A. Early age of onset is an independent predictor for worse disease-free survival in sporadic rectal cancer patients. A comparative analysis of 980 consecutive patients. Eur. J. Surg. Oncol. 2022, 48, 857–863. [Google Scholar] [CrossRef]
- REACCT Collaborative. Post-Operative Functional Outcomes in Early Age Onset Rectal Cancer. Front. Oncol. 2022, 12, 868359. [Google Scholar] [CrossRef]
- O’Sullivan, D.E.; Sutherland, R.L.; Town, S.; Chow, K.; Fan, J.; Forbes, N.; Heitman, S.J.; Hilsden, R.J.; Brenner, D.R. Risk Factors for Early-Onset Colorectal Cancer: A Systematic Review and Meta-analysis. Clin. Gastroenterol. Hepatol. 2022, 20, 1229–1240.e1225. [Google Scholar] [CrossRef]
- Gausman, V.; Dornblaser, D.; Anand, S.; Hayes, R.B.; O’Connell, K.; Du, M.; Liang, P.S. Risk Factors Associated With Early-Onset Colorectal Cancer. Clin. Gastroenterol. Hepatol. 2020, 18, 2752–2759.e2752. [Google Scholar] [CrossRef]
- Global Burden of Disease Cancer Collaboration. Global, Regional, and National Cancer Incidence, Mortality, Years of Life Lost, Years Lived With Disability, and Disability-Adjusted Life-Years for 29 Cancer Groups, 1990 to 2017: A Systematic Analysis for the Global Burden of Disease Study. JAMA Oncol. 2019, 5, 1749–1768. [Google Scholar] [CrossRef] [Green Version]
- Foreman, K.J.; Lozano, R.; Lopez, A.D.; Murray, C.J. Modeling causes of death: An integrated approach using CODEm. Popul. Health Metr. 2012, 10, 1. [Google Scholar] [CrossRef] [Green Version]






| Population | Incidence | Deaths | DALYs | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1990 | 2019 | 2019 vs. 1990 | 1990 | 2019 | 2019 vs. 1990 | 1990 | 2019 | 2019 vs. 1990 | |||||||
| Number | Rate | Number | Rate | Rate Change | Number | Rate | Number | Rate | Rate Change | Number | Rate | Number | Rate | Rate Change | |
| 95% UI | per 100,000 | 95% UI | per 100,000 | 95% UI | 95% UI | per 100,000 | 95% UI | per 100,000 | 95% UI | 95% UI | per 100,000 | 95% UI | per 100,000 | 95% UI | |
| Global | 94,707 | 3.5 | 22,5736 | 5.7 | 64.3 | 50,437 | 1.9 | 86,546 | 2.2 | 18.3 | 2,516,721 | 92.8 | 4,259,922 | 108.3 | 16.7 |
| 90,421–99,416 | 3.3–3.7 | 207,658–246,756 | 5.3–6.3 | 49.1 to 81.0 | 47,475–53,368 | 1.8–2.0 | 80,162–93,431 | 2.0–2.4 | 7.0 to 29.3 | 2,368,906–2,663,625 | 87.3–98.2 | 3,942,850–4,590,979 | 100.2–116.7 | 5.8 to 27.4 | |
| Gender | |||||||||||||||
| Male | 50,671 | 3.7 | 137,138 | 6.9 | 86.9 | 26,990 | 2.0 | 51,000 | 2.6 | 30.5 | 134,8146 | 98.1 | 2,515,161 | 126.4 | 28.9 |
| 47,855–54,342 | 3.5–4.0 | 122,715–154,229 | 6.2–7.8 | 62.8 to 114.1 | 25,038–29,445 | 1.8–2.1 | 45,983–56,179 | 2.3–2.8 | 12.1 to 48.9 | 1,251,294–1,472,000 | 91.1–107.1 | 2,270,969–2,755,869 | 114.1–138.5 | 10.7 to 46.6 | |
| Female | 44,036 | 3.3 | 88,598 | 4.6 | 38.4 | 23,447 | 1.8 | 35,546 | 1.8 | 4.3 | 1,168,575 | 87.3 | 1,744,761 | 89.7 | 2.7 |
| 41,091–47,269 | 3.1–3.5 | 79,974–97,560 | 4.1–5.0 | 22.5 to 55.6 | 21,543–25,631 | 1.6–1.9 | 32,351–38,886 | 1.7–2.0 | −7.7 to 16.5 | 1,074,665–1,277,269 | 80.3–95.5 | 1,587,818–1,910,865 | 81.6–98.2 | −9.0 to 14.7 | |
| SDI regions | |||||||||||||||
| High SDI | 32,179 | 7.5 | 47,490 | 10.1 | 35.1 | 11,544 | 2.7 | 12,020 | 2.6 | −4.7 | 562,074 | 130.7 | 589,507 | 125.4 | −4.0 |
| 31,645–32,734 | 7.4–7.6 | 43,602–51,743 | 9.3–11.0 | 23.8 to 47.8 | 11,366–11,718 | 2.6–2.7 | 11,560–12,509 | 2.5–2.7 | −8.7 to −0.4 | 552,309–572,092 | 128.4–133.0 | 565,599–615,065 | 120.4–130.9 | −8.0 to 0.3 | |
| High-middle SDI | 27,713 | 4.6 | 69,369 | 9.5 | 108.0 | 14,898 | 2.5 | 22,183 | 3.0 | 23.7 | 74,2329 | 122.6 | 1,094,438 | 150.2 | 22.5 |
| 26,289–29,503 | 4.3–4.9 | 62,168–77,408 | 8.5–10.6 | 83.7 to 135.6 | 14,014–15,826 | 2.3–2.6 | 20,249–24,369 | 2.8–3.3 | 10.4 to 37.4 | 696,956–790,755 | 115.1–130.6 | 1,003,070–1,198,241 | 137.7–164.5 | 9.7 to 36 | |
| Middle SDI | 23,378 | 2.6 | 68,967 | 5.5 | 111.2 | 15,311 | 1.7 | 31,223 | 2.5 | 46.0 | 779,805 | 86.4 | 153,8506 | 122.0 | 41.2 |
| 21,458–25,471 | 2.4–2.8 | 61,737–76,542 | 4.9–6.1 | 83.3 to 141.1 | 13,878–16,640 | 1.5–1.8 | 28,191–34,399 | 2.2–2.7 | 27.0 to 67.4 | 707,052–846,544 | 78.4–93.8 | 1,390,711–1,693,029 | 110.3–134.3 | 23.5 to 61.3 | |
| Low-middle SDI | 8615 | 1.6 | 24,752 | 2.7 | 66.4 | 6433 | 1.2 | 15,376 | 1.6 | 38.4 | 321,443 | 59.5 | 754,341 | 80.8 | 35.9 |
| 7710–9670 | 1.4–1.8 | 22,289–27,556 | 2.4–3.0 | 41.0 to 92.6 | 5715–7231 | 1.1–1.3 | 13,666–17,137 | 1.5–1.8 | 16.1 to 60.7 | 285,755–361,100 | 52.9–66.8 | 672,864–840,215 | 72.1–90.0 | 14.5 to 57.3 | |
| Low SDI | 2777 | 1.2 | 7301 | 1.4 | 13.1 | 2226 | 1.0 | 5693 | 1.1 | 10.1 | 109,830 | 47.2 | 280,703 | 51.9 | 10.0 |
| 2284–3327 | 1.0–1.4 | 6291–8411 | 1.2–1.6 | −11.5 to 43.9 | 1836–2671 | 0.8–1.1 | 4933–6583 | 0.9–1.2 | −13.4 to 40.2 | 90,789–131,973 | 39.0–56.8 | 242,946–324,266 | 45.0–60.0 | −13.5 to 40.4 | |
| GBD regions | |||||||||||||||
| Andean Latin America | 351 | 1.9 | 1507 | 4.6 | 141.3 | 203 | 1.1 | 526 | 1.6 | 45.4 | 10,367 | 55.7 | 26,696 | 80.6 | 44.8 |
| 311–399 | 1.7–2.1 | 1160–1951 | 3.5–5.9 | 82.2 to 219.3 | 181–230 | 1.0–1.2 | 411–669 | 1.2–2.0 | 10.4 to 90.4 | 9230–11,732 | 49.6–63.0 | 20,869–34,030 | 63.0–102.7 | 10.5 to 89.7 | |
| Australasia | 941 | 8.7 | 1520 | 11.2 | 28.9 | 321 | 3.0 | 337 | 2.5 | −16.1 | 15,513 | 143.7 | 16,772 | 124.0 | −13.7 |
| 892–993 | 8.3–9.2 | 1194–1933 | 8.8–14.3 | 0.9 to 63.0 | 307–335 | 2.8–3.1 | 308–370 | 2.3–2.7 | −23.9 to −6.8 | 14,835–16,199 | 137.5–150.1 | 15,269–18,374 | 112.9–135.9 | −22.1 to −4.4 | |
| Caribbean | 575 | 3.2 | 1222 | 5.1 | 62.0 | 314 | 1.7 | 562 | 2.3 | 36.4 | 15,629 | 85.7 | 27,483 | 114.9 | 34.1 |
| 540–611 | 3.0–3.4 | 1006–1474 | 4.2–6.2 | 32.8 to 94.5 | 292–339 | 1.6–1.9 | 461–681 | 1.9–2.8 | 11.9 to 63.5 | 14,571–16,805 | 79.9–92.1 | 22,550–33,298 | 94.3–139.3 | 9.9 to 60.7 | |
| Central Asia | 1297 | 3.9 | 1831 | 3.7 | −3.6 | 806 | 2.4 | 983 | 2.0 | −16.6 | 41,844 | 125.4 | 49,357 | 101.1 | −19.4 |
| 1243–1359 | 3.7–4.1 | 1637–2062 | 3.4–4.2 | −14.1 to 8.9 | 773–844 | 2.3–2.5 | 878–1114 | 1.8–2.3 | −25.6 to −5.7 | 40,214–43,859 | 120.5–131.5 | 44,065–55,814 | 90.2–114.3 | −28.0 to −8.9 | |
| Central Europe | 3847 | 6.3 | 4850 | 9.2 | 45.9 | 2113 | 3.5 | 1861 | 3.5 | 2.0 | 101,778 | 166.8 | 88,617 | 168.1 | 0.8 |
| 3737–3969 | 6.1–6.5 | 4151–5579 | 7.9–10.6 | 25.8 to 67.3 | 2057–2174 | 3.4–3.6 | 1598–2134 | 3.0–4.0 | −12.2 to 17.4 | 99,088–104,830 | 162.4–171.8 | 76,070–101,521 | 144.3–192.6 | −13.0 to 15.6 | |
| Central Latin America | 1452 | 1.8 | 5782 | 4.4 | 146.5 | 876 | 1.1 | 2564 | 1.9 | 81.3 | 44,894 | 55.1 | 128,095 | 97.3 | 76.7 |
| 1413–1490 | 1.7–1.8 | 4916–6815 | 3.7–5.2 | 108.8 to 190.3 | 853–898 | 1.0–1.1 | 2171–3009 | 1.6–2.3 | 54.1 to 114.0 | 43,690–46,041 | 53.6–56.5 | 108,759–150,831 | 82.6–114.5 | 50.2 to 108.2 | |
| Central sub-Saharan Africa | 291 | 1.2 | 798 | 1.3 | 7.5 | 232 | 1.0 | 604 | 1.0 | 2.3 | 11,541 | 47.3 | 29,811 | 48.0 | 1.4 |
| 215–387 | 0.9–1.6 | 566–1082 | 0.9–1.7 | −3.1 to 5.6 | 177–305 | 0.7–1.3 | 428–821 | 0.7–1.3 | −34.6 to 49.1 | 8753–15,110 | 35.9–61.9 | 21,129–40,444 | 34.0–65.1 | −34.9 to 46.6 | |
| East Asia | 25,348 | 3.7 | 90,911 | 12.2 | 231.8 | 15,532 | 2.2 | 27,447 | 3.7 | 63.5 | 795,135 | 115.2 | 1,362,350 | 182.5 | 58.5 |
| 22,185–28,938 | 3.2–4.2 | 76,318–106,894 | 10.2–14.3 | 16.4 to 31.3 | 13,405–17,867 | 1.9–2.6 | 23,104–32,223 | 3.1–4.3 | 30.6 to 102.8 | 685,952–910,860 | 99.4–131.9 | 1,156,497–1,580,832 | 155.0–211.8 | 27.9 to 95.4 | |
| Eastern Europe | 6811 | 6.2 | 9239 | 9.4 | 52.6 | 3515 | 3.2 | 3459 | 3.5 | 10.7 | 171,933 | 155.8 | 168,129 | 171.5 | 10.0 |
| 6348–7172 | 5.8–6.5 | 8187–10,480 | 8.3–10.7 | 35.5 to 72.9 | 3276–3698 | 3.0–3.4 | 3063–3898 | 3.1–4.0 | −1.6 to 24.5 | 160,508–180,593 | 145.5–163.7 | 149,699–189,150 | 152.7–192.9 | −1.9 to 23.6 | |
| Eastern sub-Saharan Africa | 1067 | 1.3 | 3089 | 1.6 | 20.8 | 850 | 1.0 | 2298 | 1.2 | 12.8 | 42,134 | 50.8 | 113,630 | 57.1 | 12.5 |
| 858–1311 | 1.0–1.6 | 2526–3770 | 1.3–1.9 | −9.6 to 66.7 | 678–1043 | 0.8–1.3 | 1885–2808 | 0.9–1.4 | −15.7 to 58.8 | 33,615–51,821 | 40.5–62.4 | 92,977–138,693 | 46.7–69.7 | −16.1 to 58.8 | |
| High-income Asia Pacific | 7953 | 8.6 | 9294 | 11.5 | 33.8 | 2837 | 3.1 | 2056 | 2.5 | −17.0 | 137,712 | 148.3 | 100,488 | 123.8 | −16.5 |
| 7714–8186 | 8.3–8.8 | 8007–10,617 | 9.9–13.1 | 15.5 to 53.2 | 2779–2892 | 3.0–3.1 | 1941–2160 | 2.4–2.7 | −21.3 to −12.5 | 134,351–140,739 | 144.6–151.5 | 94,554–105,865 | 116.5–130.5 | −20.9 to −12.1 | |
| High-income North America | 11,665 | 7.8 | 18,499 | 11.1 | 41.4 | 3604 | 2.4 | 4545 | 2.7 | 12.4 | 177,662 | 119.5 | 223,318 | 133.9 | 12.0 |
| 11,348–11,962 | 7.6–8 | 15,902–21,547 | 9.5–12.9 | 21.3 to 65.6 | 3517–3688 | 2.4–2.5 | 4399–4709 | 2.6–2.8 | 7.5 to 18.5 | 172,981–182,260 | 116.4–122.6 | 214,946–232,481 | 128.9–139.4 | 7.3 to 18.2 | |
| North Africa and Middle East | 3126 | 1.9 | 11,101 | 3.3 | 72.9 | 2180 | 1.3 | 5485 | 1.6 | 22.5 | 108,846 | 67.0 | 270,165 | 81.0 | 20.8 |
| 2608–3801 | 1.6–2.3 | 9616–12,783 | 2.9–3.8 | 34.1 to 116.9 | 1816–2650 | 1.1–1.6 | 4716–6362 | 1.4–1.9 | −5.5 to 54.2 | 90,784–132,718 | 55.9–81.7 | 232,244–312,325 | 69.6–93.6 | −6.9 to 51.9 | |
| Oceania | 61 | 1.9 | 165 | 2.4 | 25.7 | 43 | 1.4 | 112 | 1.6 | 21.6 | 2174 | 68.7 | 5624 | 82.7 | 20.4 |
| 49–76 | 1.5–2.4 | 126–215 | 1.9–3.2 | −2.7 to 68.9 | 34–54 | 1.1–1.7 | 85–147 | 1.2–2.2 | −6.3 to 64.3 | 1715–2728 | 54.2–86.2 | 4292–7320 | 63.1–107.6 | −6.7 to 61.4 | |
| South Asia | 6136 | 1.2 | 18,253 | 1.9 | 61.6 | 4824 | 0.9 | 12,421 | 1.3 | 39.9 | 237,610 | 44.9 | 606,012 | 62.2 | 38.6 |
| 5397–6949 | 1.0–1.3 | 15,671–21,008 | 1.6–2.2 | 29.2 to 94.8 | 4265–5455 | 0.8–1.0 | 10,758–14,391 | 1.1–1.5 | 12.1 to 68.9 | 209,984–268,190 | 39.7–50.7 | 523,107–698,658 | 53.7–71.7 | 11.5 to 66.9 | |
| Southeast Asia | 6101 | 2.6 | 18,976 | 5.2 | 103.1 | 4241 | 1.8 | 10,550 | 2.9 | 62.4 | 214,313 | 90.7 | 517,741 | 143.0 | 57.7 |
| 5195–6824 | 2.2–2.9 | 15,675–22,334 | 4.3–6.2 | 66.5 to 142.2 | 3617–4793 | 1.5–2.0 | 8800–12,385 | 2.4–3.4 | 34.9 to 90.8 | 181,999–242,558 | 77.0–102.6 | 433,010–606,340 | 119.6–167.5 | 31.1 to 85.3 | |
| Southern Latin America | 950 | 3.9 | 2233 | 6.6 | 69.2 | 584 | 2.4 | 1022 | 3.0 | 25.8 | 28,375 | 115.8 | 50,050 | 147.0 | 26.9 |
| 903–999 | 3.7–4.1 | 1694–2913 | 5.0–8.6 | 27.5 to 121.5 | 558–613 | 2.3–2.5 | 936–1116 | 2.8–3.3 | 13.7 to 38.9 | 27,108–29,756 | 110.7–121.5 | 45,995–54,610 | 135.1–160.4 | 15.3 to 39.7 | |
| Southern sub-Saharan Africa | 566 | 2.2 | 1111 | 2.6 | 21.1 | 406 | 1.6 | 738 | 1.7 | 12.1 | 20,452 | 78.4 | 36,624 | 86.6 | 10.4 |
| 508–631 | 1.9–2.4 | 955–1277 | 2.3–3.0 | −1.2 to 45.3 | 366–452 | 1.4–1.7 | 635–852 | 1.5–2.0 | −9.2 to 35.3 | 18,430–22,833 | 70.6–87.5 | 31,528–42,278 | 99.9–74.5 | −10.2 to 33.7 | |
| Tropical Latin America | 1917 | 2.4 | 5755 | 4.8 | 97.8 | 1239 | 1.6 | 2857 | 2.4 | 51.9 | 62,339 | 79.4 | 139,457 | 117.0 | 47.4 |
| 1856–1983 | 2.4–2.5 | 5415–6061 | 4.5–5.1 | 84.5 to 110.6 | 1201–1283 | 1.5–1.6 | 2698–3003 | 2.3–2.5 | 42.1 to 61.5 | 60,473–64,504 | 77.0–82.1 | 131,965–146,425 | 110.7–122.8 | 38.4 to 56.3 | |
| Western Europe | 13,442 | 6.9 | 17,021 | 8.9 | 28.4 | 5082 | 2.6 | 4247 | 2.2 | −15.2 | 245,078 | 126.7 | 206,454 | 108.3 | −14.6 |
| 13,129–13,761 | 6.8–7.1 | 14,619–19,670 | 7.7–10.3 | 10.3 to 49.2 | 4992–5173 | 2.6–2.7 | 4053–4426 | 2.1–2.3 | −19.0 to −11.8 | 240,230–250,088 | 124.2–129.3 | 196,144–215,816 | 102.9–113.2 | −18.5 to −10.8 | |
| Western sub-Saharan Africa | 811 | 1.0 | 2577 | 1.2 | 25.9 | 635 | 0.7 | 1872 | 0.9 | 16.8 | 31,392 | 36.9 | 93,047 | 43.3 | 17.4 |
| 642–1009 | 0.8–1.2 | 2060–3112 | 1.0–1.4 | −3.7 to 63.7 | 500–791 | 0.6–0.9 | 1494–2316 | 0.7–1.1 | −10.4 to 51.8 | 24,824–39,038 | 29.1–45.8 | 74,217–114,855 | 34.5–53.4 | −9.8 to 52.8 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gu, W.-J.; Pei, J.-P.; Lyu, J.; Akimoto, N.; Haruki, K.; Ogino, S.; Zhang, C.-D. The Burden of Early-Onset Colorectal Cancer and Its Risk Factors from 1990 to 2019: A Systematic Analysis for the Global Burden of Disease Study 2019. Cancers 2022, 14, 3502. https://0-doi-org.brum.beds.ac.uk/10.3390/cancers14143502
Gu W-J, Pei J-P, Lyu J, Akimoto N, Haruki K, Ogino S, Zhang C-D. The Burden of Early-Onset Colorectal Cancer and Its Risk Factors from 1990 to 2019: A Systematic Analysis for the Global Burden of Disease Study 2019. Cancers. 2022; 14(14):3502. https://0-doi-org.brum.beds.ac.uk/10.3390/cancers14143502
Chicago/Turabian StyleGu, Wan-Jie, Jun-Peng Pei, Jun Lyu, Naohiko Akimoto, Koichiro Haruki, Shuji Ogino, and Chun-Dong Zhang. 2022. "The Burden of Early-Onset Colorectal Cancer and Its Risk Factors from 1990 to 2019: A Systematic Analysis for the Global Burden of Disease Study 2019" Cancers 14, no. 14: 3502. https://0-doi-org.brum.beds.ac.uk/10.3390/cancers14143502