A Multi-Modal Family Peer Support-Based Program to Improve Quality of Life among Pediatric Brain Tumor Patients: A Mixed-Methods Pilot Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Recruitment and Participants
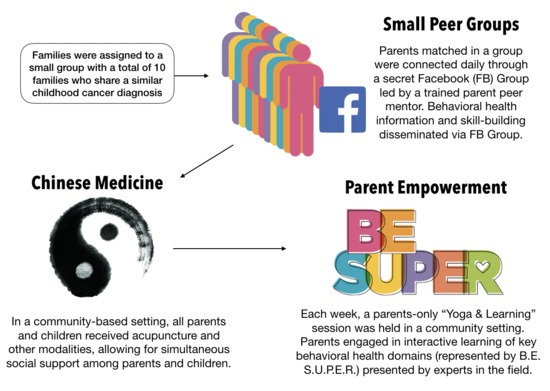
2.2. Intervention
2.3. Measures
2.4. Analysis
3. Results
3.1. Adherence
3.2. Usability and Acceptability
3.3. Exploratory Outcomes
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Hudson, M.M.; Ness, K.K.; Gurney, J.G.; Mulrooney, D.A.; Chemaitilly, W.; Krull, K.R.; Green, D.M.; Armstrong, G.T.; Nottage, K.A.; Jones, K.E.; et al. Clinical ascertainment of health outcomes among adults treated for childhood cancer. JAMA 2013, 309, 2371–2381. [Google Scholar] [CrossRef] [PubMed]
- Oeffinger, K.C.; Mertens, A.C.; Sklar, C.A.; Kawashima, T.; Hudson, M.M.; Meadows, A.T.; Friedman, D.L.; Marina, N.; Hobbie, W.; Kadan-Lottick, N.; et al. Chronic health conditions in adult survivors of childhood cancer. N. Engl. J. Med. 2006, 355, 1572–1582. [Google Scholar] [CrossRef] [PubMed]
- Meeske, K.; Katz, E.R.; Palmer, S.N.; Burwinkle, T.; Varni, J.W. Parent proxy-reported health-related quality of life and fatigue in pediatric patients diagnosed with brain tumors and acute lymphoblastic leukemia. Cancer 2004, 101, 2116–2125. [Google Scholar] [CrossRef] [PubMed]
- Pogorzala, M.; Styczynski, J.; Kurylak, A.; Debski, R.; Wojtkiewicz, M.; Wysocki, M. Health-related quality of life among paediatric survivors of primary brain tumours and acute leukaemia. Qual. Life Res. 2010, 19, 191–198. [Google Scholar] [CrossRef]
- Effinger, K.E.; Stratton, K.L.; Fisher, P.G.; Ness, K.K.; Krull, K.R.; Oeffinger, K.C.; Armstrong, G.T.; Robison, L.L.; Hudson, M.M.; Leisenring, W.M.; et al. Long-term health and social function in adult survivors of paediatric astrocytoma: A report from the Childhood Cancer Survivor Study. Eur. J. Cancer 2019, 106, 171–180. [Google Scholar] [CrossRef] [PubMed]
- Stolley, M.R.; Restrepo, J.; Sharp, L.K. Diet and physical activity in childhood cancer survivors: A review of the literature. Ann. Behav. Med. 2010, 39, 232–249. [Google Scholar] [CrossRef] [Green Version]
- Armstrong, G.T.; Oeffinger, K.C.; Chen, Y.; Kawashima, T.; Yasui, Y.; Leisenring, W.; Stovall, M.; Chow, E.J.; Sklar, C.A.; Mulrooney, D.A.; et al. Modifiable risk factors and major cardiac events among adult survivors of childhood cancer. J. Clin. Oncol. 2013, 31, 3673–3680. [Google Scholar] [CrossRef]
- Jones, L.W.; Liu, Q.; Armstrong, G.T.; Ness, K.K.; Yasui, Y.; Devine, K.; Tonorezos, E.; Soares-Miranda, L.; Sklar, C.A.; Douglas, P.S.; et al. Exercise and risk of major cardiovascular events in adult survivors of childhood hodgkin lymphoma: A report from the childhood cancer survivor study. J. Clin. Oncol. 2014, 32, 3643–3650. [Google Scholar] [CrossRef]
- Ford, J.; Barnett, M.; Werk, R. Health behaviors of childhood cancer survivors. Children 2014, 1, 355–373. [Google Scholar] [CrossRef] [Green Version]
- Smith, W.A.; Li, C.; Nottage, K.A.; Mulrooney, D.A.; Armstrong, G.T.; Lanctot, J.Q.; Chemaitilly, W.; Laver, J.H.; Srivastava, D.K.; Robison, L.L.; et al. Lifestyle and metabolic syndrome in adult survivors of childhood cancer: A report from the St. Jude Lifetime Cohort Study. Cancer 2014, 120, 2742–2750. [Google Scholar] [CrossRef]
- Spector, D.J.; Noonan, D.; Mayer, D.K.; Benecha, H.; Zimmerman, S.; Smith, S.K. Are lifestyle behavioral factors associated with health-related quality of life in long-term survivors of non-Hodgkin lymphoma? Cancer 2015, 121, 3343–3351. [Google Scholar] [CrossRef] [PubMed]
- Howell, C.R.; Wilson, C.L.; Ehrhardt, M.J.; Partin, R.E.; Kaste, S.C.; Lanctot, J.Q.; Pui, C.-H.; Robison, L.L.; Hudson, M.M.; Ness, K.K. Clinical impact of sedentary behaviors in adult survivors of acute lymphoblastic leukemia: A report from the St. Jude Lifetime Cohort study. Cancer 2017, 124, 1036–1043. [Google Scholar] [CrossRef]
- Tonorezos, E.S.; Sharp, L. Health promotion for adolescent leukemia survivors. Pediatr. Blood Cancer 2013, 60, 893–894. [Google Scholar] [CrossRef] [PubMed]
- Tonorezos, E.; Henderson, T. Clinical guidelines for the care of childhood cancer survivors. Children 2014, 1, 227–240. [Google Scholar] [CrossRef] [PubMed]
- Robison, L.L.; Hudson, M.M. Survivors of childhood and adolescent cancer: Life-long risks and responsibilities. Nat. Rev. Cancer 2014, 14, 61. [Google Scholar] [CrossRef] [PubMed]
- Kirchhoff, A.C.; Leisenring, W.; Krull, K.R.; Ness, K.K.; Friedman, D.L.; Armstrong, G.T.; Stovall, M.; Park, E.R.; Oeffinger, K.C.; Hudson, M.M.; et al. Unemployment among adult survivors of childhood cancer: A report from the childhood cancer survivor study. Med. Care 2010, 48, 1015–1025. [Google Scholar] [CrossRef] [Green Version]
- Hocking, M.C.; Hobbie, W.L.; Deatrick, J.A.; Lucas, M.S.; Szabo, M.M.; Volpe, E.M.; Barakat, L.P. Neurocognitive and family functioning and quality of life among young adult survivors of childhood brain tumors. Clin. Neuropsychol. 2011, 25, 942–962. [Google Scholar] [CrossRef] [Green Version]
- Greenzang, K.A.; Cronin, A.M.; Kang, T.I.; Mack, J.W. Parental distress and desire for information regarding long-term implications of pediatric cancer treatment. Cancer 2018, 124, 4529–4537. [Google Scholar] [CrossRef] [Green Version]
- Wilford, J.G.; Hopfer, S.; Wenzel, L. Perceptions of changes in clinical, informational, and supportive relationships after end of treatment among parents of young childhood cancer survivors. Psychooncology 2019, 28, 913–919. [Google Scholar] [CrossRef]
- Leventhal-Belfer, L.; Bakker, A.M.; Russo, C.L. Parents of childhood cancer survivors: A descriptive look at their concerns and needs. J. Psychosoc. Oncol. 1993, 11, 19–41. [Google Scholar] [CrossRef]
- Tackett, A.P.; Cushing, C.C.; Suorsa, K.I.; Mullins, A.J.; Gamwell, K.L.; Mayes, S.; McNall-Knapp, R.; Chaney, J.M.; Mullins, L.L. Illness uncertainty, global psychological distress, and posttraumatic stress in pediatric cancer: A preliminary examination using a path analysis approach. J. Pediatr. Psychol. 2016, 41, 309–318. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wilford, J.; Buchbinder, D.; Fortier, M.A.; Osann, K.; Shen, V.; Torno, L.; Sender, L.S.; Parsons, S.K.; Wenzel, L. She was a little social butterfly a qualitative analysis of parent perception of social functioning in adolescent and young adult brain tumor survivors. J. Pediatr. Oncol. Nurs. 2017, 34, 239–249. [Google Scholar] [CrossRef] [PubMed]
- Hocking, M.C.; McCurdy, M.; Turner, E.; Kazak, A.E.; Noll, R.B.; Phillips, P.; Barakat, L.P. Social competence in pediatric brain tumor survivors: Application of a model from social neuroscience and developmental psychology. Pediatr. Blood Cancer 2015, 62, 375–384. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Dennis, C.-L.; Hodnett, E.; Kenton, L.; Weston, J.; Zupancic, J.; Stewart, D.E.; Kiss, A. Effect of peer support on prevention of postnatal depression among high risk women: Multisite randomised controlled trial. BMJ 2009, 338, a3064. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cherrington, A.L.; Khodneva, Y.; Richman, J.S.; Andreae, S.J.; Gamboa, C.; Safford, M.M. Impact of peer support on acute care visits and hospitalizations for individuals with diabetes and depressive symptoms: A cluster-randomized controlled trial. Diabetes Care 2018, 41, 2463–2470. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Field, T.; Diego, M.; Delgado, J.; Medina, L. Peer support and interpersonal psychotherapy groups experienced decreased prenatal depression, anxiety and cortisol. Early Hum. Dev. 2013, 89, 621–624. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Centola, D. An experimental study of homophily in the adoption of health behavior. Science 2011, 334, 1269–1272. [Google Scholar] [CrossRef] [PubMed]
- Gage-Bouchard, E.A.; LaValley, S.; Mollica, M.; Beaupin, L. Communication and exchange of specialized health-related support among people with experiential similarity on facebook. Health Commun. 2017, 32, 1233–1240. [Google Scholar] [CrossRef] [PubMed]
- Behler, R.; Suh, C.; Brashears, M.; Shi, Y. Familiar faces, familiar spaces: Social similarity and co-presence in non-relational behavioral convergence. Netw. Sci. 2018, 6, 396–429. [Google Scholar] [CrossRef]
- Wu, S.; Sapru, A.; Stewart, M.A.; Milet, M.J.; Hudes, M.; Livermore, L.F.; Flori, H.R. Using acupuncture for acute pain in hospitalized children. Pediatr. Crit. Care Med. 2009, 10, 291. [Google Scholar] [CrossRef] [Green Version]
- Golianu, B.; Yeh, A.; Brooks, M. Acupuncture for pediatric pain. Children 2014, 1, 134–148. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Meyer, R.M.L.; Barber, B.A.; Kobylecka, M.; Gold, J.I. Examining the association between parental stress related to child illness and child pain across acupuncture treatments. Med. Acupunct. 2014, 26, 23–30. [Google Scholar] [CrossRef]
- Cheng, C.S.; Chen, L.Y.; Ning, Z.Y.; Zhang, C.Y.; Zhu, X.-Y.; Xie, J. Acupuncture for cancer-related fatigue in lung cancer patients: A randomized, double blind, placebo-controlled pilot trial. Support. Care Cancer 2017, 25, 3807–3814. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Lin, L.; Li, H.; Hu, Y.; Tian, L. Effects of acupuncture on cancer-related fatigue: A meta-analysis. Support. Care Cancer 2018, 26, 415–425. [Google Scholar] [CrossRef]
- Molassiotis, A.; Bardy, J.; Finnegan-John, J.; Mackereth, P.; Ryder, D.W.; Filshie, J.; Ream, E.; Richardson, A. Acupuncture for cancer-related fatigue in patients with breast cancer: A pragmatic randomized controlled trial. J. Clin. Oncol. 2012, 30, 4470–4476. [Google Scholar] [CrossRef]
- Mao, H.; Mao, J.J.; Guo, M.; Cheng, K.; Wei, J.; Shen, X.; Shen, X. Effects of infrared laser moxibustion on cancer-related fatigue: A randomized, double-blind, placebo-controlled trial. Cancer 2016, 122, 3667–3672. [Google Scholar] [CrossRef] [PubMed]
- Thompson, L.M.; Osian, S.R.; Jacobsen, P.B.; Johnstone, P.A. Patient-reported outcomes of acupuncture for symptom control in cancer. J. Acupunct. Meridian Stud. 2015, 8, 127–133. [Google Scholar] [CrossRef] [Green Version]
- Tao, W.W.; Jiang, H.; Tao, X.M.; Jiang, P.; Sha, L.Y.; Sun, X.C. Effects of acupuncture, tuina, tai chi, qigong, and traditional chinese medicine five-element music therapy on symptom management and quality of life for cancer patients: A meta-analysis. J. Pain Symptom Manag. 2016, 51, 728–747. [Google Scholar] [CrossRef] [Green Version]
- Lau, C.H.; Wu, X.; Chung, V.C.; Liu, X.; Hui, E.P.; Cramer, H.; Lauche, R.; Wong, S.Y.S.; Lau, A.Y.; Sit, R.W.S.; et al. Acupuncture and related therapies for symptom management in palliative cancer care: Systematic review and meta-analysis. Medicine 2016, 95, e2901. [Google Scholar] [CrossRef]
- Dennis, C.-L. Peer support within a health care context: A concept analysis. Int. J. Nurs. Stud. 2003, 40, 321–332. [Google Scholar] [CrossRef]
- Saran, I.; Fink, G.; McConnell, M. How does anonymous online peer communication affect prevention behavior? Evidence from a laboratory experiment. PLoS ONE 2018, 13, e0207679. [Google Scholar] [CrossRef] [PubMed]
- Duggan, M.; Lenhart, A.; Lampe, C.; Ellison, N.B. Parents and Social Media; Pew Research Center: Washington, DC, USA, 2015. [Google Scholar]
- Niela-Vilén, H.; Axelin, A.; Salanterä, S.; Melender, H.-L. Internet-based peer support for parents: A systematic integrative review. Int. J. Nurs. Stud. 2014, 51, 1524–1537. [Google Scholar] [CrossRef] [PubMed]
- Coulson, N.S.; Greenwood, N. Families affected by childhood cancer: An analysis of the provision of social support within online support groups. Child Care Health Dev. 2011, 38, 870–877. [Google Scholar] [CrossRef] [PubMed]
- Thoits, P.A. Mechanisms linking social ties and support to physical and mental health. J. Health Soc. Behav. 2011, 52, 145–161. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Centola, D.; van de Rijt, A. Choosing your network: Social preferences in an online health community. Soc. Sci. Med. 2015, 125, 19–31. [Google Scholar] [CrossRef] [PubMed]
- Health, N.I.O. Patient-Reported Outcome Measurement Information System: Instrument Details. 2019. Available online: http://www.healthmeasures.net/explore-measurement-systems/promis/measure-development-research (accessed on 28 February 2020).
- Merchant, G.; Weibel, N.; Patrick, K.; Fowler, J.H.; Norman, G.J.; Gupta, A.; Servetas, C.; Calfas, K.; Raste, K.; Pina, L.; et al. Click “like” to change your behavior: A mixed methods study of college students’ exposure to and engagement with Facebook content designed for weight loss. J. Med. Internet Res. 2014, 16, e158. [Google Scholar] [CrossRef]
- Hales, S.B.; Davidson, C.; Turner-McGrievy, G.M. Varying social media post types differentially impacts engagement in a behavioral weight loss intervention. Transl. Behav. Med. 2014, 4, 355–362. [Google Scholar] [CrossRef] [Green Version]
- Naslund, J.A.; Aschbrenner, K.A.; Marsch, L.A.; McHugo, G.J.; Bartels, S.J. Facebook for supporting a lifestyle intervention for people with major depressive disorder, bipolar disorder, and schizophrenia: An exploratory study. Psychiatr. Q. 2018, 89, 81–94. [Google Scholar] [CrossRef]
- Wakefield, C.E.; Sansom-Daly, U.M.; McGill, B.C.; Ellis, S.J.; Doolan, E.L.; Robertson, E.G.; Mathur, S.; Cohn, R.J. Acceptability and feasibility of an e-mental health intervention for parents of childhood cancer survivors: “Cascade”. Support. Care Cancer 2016, 24, 2685–2694. [Google Scholar] [CrossRef]
- Cernvall, M.; Carlbring, P.; Ljungman, L.; Ljungman, G.; Essen, L. Internet-based guided self-help for parents of children on cancer treatment: A randomized controlled trial. Psycho-Oncol. 2015, 24, 1152–1158. [Google Scholar] [CrossRef]
- van Dijk-Lokkart, E.M.; Braam, K.I.; Kaspers, G.J.L.; van Dulmen-den Broeder, E.; Takken, T.; Grootenhuis, M.A.; Streng, I.C.; Bierings, M.; Merks, J.H.; Heuvel-Eibrink, M.M.V.D.; et al. Applicability and evaluation of a psychosocial intervention program for childhood cancer patients. Support. Care Cancer 2015, 23, 2327–2333. [Google Scholar] [CrossRef] [PubMed]
- Sahler, O.J.Z.; Dolgin, M.J.; Phipps, S.; Fairclough, D.L.; Askins, M.A.; Katz, E.R.; Noll, R.B.; Butler, R.W. Specificity of problem-solving skills training in mothers of children newly diagnosed with cancer: Results of a multisite randomized clinical trial. J. Clin. Oncol. 2013, 31, 1329–1335. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Marsland, A.L.; Long, K.A.; Howe, C.; Thompson, A.L.; Tersak, J.; Ewing, L.J. A pilot trial of a stress management intervention for primary caregivers of children newly diagnosed with cancer: Preliminary evidence that perceived social support moderates the psychosocial benefit of intervention. J. Pediatr. Psychol. 2013, 38, 449–461. [Google Scholar] [CrossRef] [Green Version]
- Ljungman, L.; Cernvall, M.; Grönqvist, H.; Ljótsson, B.; Ljungman, G.; von Essen, L. Long-term positive and negative psychological late effects for parents of childhood cancer survivors: A systematic review. PLoS ONE 2014, 9, e103340. [Google Scholar] [CrossRef] [PubMed] [Green Version]




| Variable | Parents (n = 12) | Children (n = 10) |
|---|---|---|
| Age, years: mean (SD) | 38.3 (7.8) | 7.8 (3.5) |
| Gender (%) | ||
| Female | 10 (83%) | 6 (60%) |
| Male | 2 (17%) | 4 (40%) |
| Ethnicity (%) | ||
| Non-Hispanic white | 5 (42%) | |
| Hispanic or Latino | 7 (58%) | |
| Diagnosis (%) | ||
| Atypical Teratoid Rhabdoid | 1 (10%) | |
| Ependymoma | 1 (10%) | |
| Low-grade glioma | 4 (40%) | |
| Pineoblastoma | 3 (30%) | |
| Treatments Received (%) | ||
| Surgery only | 3 (30%) | |
| Surgery + chemotherapy | 1 (10%) | |
| Surgery + chemo + radiation | 6 (10%) | |
| Treatment status (%) | ||
| Still in treatment | 5 (50%) | |
| Less than 2 years off treatment | 1 (10%) | |
| More than 2 years off treatment | 4 (40%) | |
| Marriage Status (%) | ||
| Married | 9 (75%) | |
| Separated | 0 (0%) | |
| Divorced | 0 (0%) | |
| Never married | 3 (25%) | |
| Education | ||
| Some College or below | 7 (58%) | |
| College degree or above | 5 (42%) |
| ID | What was the most valuable part of the Ohana Project for you and your child? |
|---|---|
| 01 | TCM, educational presentations, and the Facebook interaction. I loved seeing what other people wrote and recipes/pics and the OHANA things to strive for everyday. All of it was so valuable. |
| 02 | I really liked the Facebook post of what people were doing and the encouragement. The first four weeks were my favorite. We had small, manageable goals. Posting was my favorite. Sometimes yoga was hard for me on Sundays but it was always good. |
| 03 | Learning in the Facebook group more about how to eat properly. Acupuncture, meditation, importance of sleep habits and vigorous exercise. |
| 04 | Connecting with other parents and kids on a similar journey. We don’t feel lost and alone in this anymore. |
| 05 | Acupuncture |
| 06 | The [acupuncture] appointments were the best. Parent yoga was a close second. |
| 07 | Everything was great but definitely having the support of other parents going through the same thing was super valuable. Our time receiving acupuncture in a group setting was priceless, therapeutic and comforting. |
| 08 | For me I would say it was the community aspect. I felt grateful to be around other families going through the same journey as my child and I. The knowledge and support I received from [the Facebook group] are irreplaceable. |
| 09 | Acupuncture! |
| 10 | The most valuable part was being part of a community that understood what we were going through. We all felt appreciated. |
| 11 | The connections with other families. It was really just a great group of families. |
| What would you tell another cancer family about the Ohana Project? | |
| 01 | The Ohana project was so helpful to be around other parents and families that are on the same level as you. They understand what you have gone through or are going through. Acupuncture has become a regular routine for us and our daughter feels she needs it to function in the week. |
| 02 | It is really good for new parents that have just been given the diagnosis. It creates an automatic community for them. It’s also good for those who have been in the fight longer because it’s very easy to get off course. |
| 03 | It provides a community of like-minded people experiencing similar challenges. It provides access to peer-reviewed, proven scientific data and the experts that support such data on health & well-being. |
| 04 | As parents we would do ANYTHING to take our child’s pain or discomfort or sadness away. The Ohana Project gives parents tangible things to do to help our children thrive during treatment and beyond. The Ohana Project connects parents and children going through a similar journey and provides them with evidence-based research and classes, acupuncture, and social support through those new family connections. It is such an impactful and life changing program that I feel provides the missing link in healthcare. |
| 05 | Great information, guidance and support |
| 06 | It’s refreshing to be surrounded by others who are going through the exact same thing. It’s a judgement free zone. |
| 07 | It was our saving grace! Being recently diagnosed, it helped bring us out of our DARK place. |
| 08 | Trust that it is a process. Do not be so tough on yourself, it’s not a race better yet a marathon to the best version of health, community, and thriving during and after treatment. |
| 09 | This was a growing period for our family and many changes were made for the positive. Having support of other like-minded people was life changing for us! |
| 10 | Every family that has a child battling cancer should experience the Ohana Project. The small community support is so important. |
| 11 | The Ohana project is exactly like the name “a family” of parents and children going through the same journey as you are. A place where children can meet and play with kids just like them, going through the same experiences they are. Where parents can share and learn from one another without judgment. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wilford, J.G.; McCarty, R.; Torno, L.; Mucci, G.; Torres-Eaton, N.; Shen, V.; Loudon, W. A Multi-Modal Family Peer Support-Based Program to Improve Quality of Life among Pediatric Brain Tumor Patients: A Mixed-Methods Pilot Study. Children 2020, 7, 35. https://0-doi-org.brum.beds.ac.uk/10.3390/children7040035
Wilford JG, McCarty R, Torno L, Mucci G, Torres-Eaton N, Shen V, Loudon W. A Multi-Modal Family Peer Support-Based Program to Improve Quality of Life among Pediatric Brain Tumor Patients: A Mixed-Methods Pilot Study. Children. 2020; 7(4):35. https://0-doi-org.brum.beds.ac.uk/10.3390/children7040035
Chicago/Turabian StyleWilford, Justin G., Ruth McCarty, Lilibeth Torno, Grace Mucci, Nadia Torres-Eaton, Violet Shen, and William Loudon. 2020. "A Multi-Modal Family Peer Support-Based Program to Improve Quality of Life among Pediatric Brain Tumor Patients: A Mixed-Methods Pilot Study" Children 7, no. 4: 35. https://0-doi-org.brum.beds.ac.uk/10.3390/children7040035