Major Complication Following Kawasaki Disease in an Infant—The Development of Apical Infarction and Aneurysm Formation
Abstract
:1. Introduction
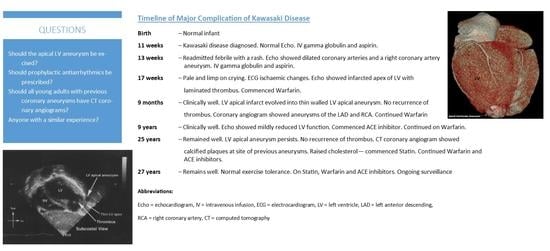
2. Case Report
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Newburger, J.W.; Takahashi, M.; Burns, J.C. Kawasaki disease. J. Am. Coll. Cardiol. 2016, 67, 1738–1749. [Google Scholar] [CrossRef]
- McCrindle, B.W.; Rowley, A.; Newburger, J.W.; Burns, J.C.; Bolger, A.F.; Gewitz, M.; Baker, A.L.; Jackson, M.A.; Takahashi, M.; Shah, P.B.; et al. Diagnosis, Treatment, and Long-Term Management of Kawasaki Disease: A Scientific Statement for Health Professionals from the American Heart Association. Circulation 2017, 135, e927–e999. [Google Scholar] [CrossRef]
- Spensley, J.; Menahem, S. Mucocutaneous lymph node disease in childhood. Aust. Paediatr. J. 1976, 12, 21. [Google Scholar]
- Newburger, J.W.; Takahashi, M.; Beiser, A.; Burns, J.C.; Bastian, J.; Chung, K.J.; Colan, S.D.; Duffy, C.E.; Fulton, D.R.; Glode, M.P.; et al. A Single Intravenous Infusion of Gamma Globulin as Compared with Four Infusions in the Treatment of Acute Kawasaki Syndrome. N. Engl. J. Med. 1991, 324, 1633–1639. [Google Scholar] [CrossRef] [PubMed]
- Kim, N.S.; Menahem, S. Serious sequels of Kawasaki Disease. Cardiol. Young 1998, 8, 386–389. [Google Scholar] [CrossRef]
- Zanon, G.; Zucchetta, P.; Varnier, M.; Vittadello, F.; Milanesi, O.; Zulian, F. Do Kawasaki disease patients without coronary artery abnormalities need a long-term follow-up? A myocardial single-photon emission computed tomography pilot study. J. Paediatr. Child. Health 2009, 45, 419–424. [Google Scholar] [CrossRef]
- Pahl, E.; Sehgal, R.; Chrystof, D.; Neches, W.H.; Webb, C.L.; Duffy, C.E.; Shulman, S.T.; Chaudhry, F.A. Feasibility of Exercise Stress Echocardiography for the Follow-up of Children With Coronary Involvement Secondary to Kawasaki Disease. Circulation 1995, 91, 122–128. [Google Scholar] [CrossRef] [PubMed]
- Ogawa, S.; Fukazawa, R.; Ohkubo, T.; Zhang, J.; Takechi, N.; Kuramochi, Y.; Hino, Y.; Jimbo, O.; Katsube, Y.; Yamamoto, M. Silent myocardial ischemia in Kawasaki disease: Evaluation of percutaneous transluminal coronary angioplasty by dobutamine stress testing. Circulation 1997, 96, 3384–3389. [Google Scholar] [CrossRef]
- Cantin, L.; Chartrand-Lefebvre, C.; Marcotte, F.; Pressacco, J.; Ducharme, A.; Lapierre, C. Coronary artery noninvasive imaging in adult Kawasaki disease. Clin. Imaging 2009, 33, 181–187. [Google Scholar] [CrossRef] [PubMed]
- Kahn, A.M.; Budoff, M.J.; Daniels, L.B.; Jimenez-Fernandez, S.; Cox, A.S.; Gordon, J.B.; Burns, J.C. Calcium Scoring in Patients with a History of Kawasaki Disease. JACC Cardiovasc. Imaging 2012, 5, 264–272. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Blankier, S.; McCrindle, B.W.; Ito, S.; Yeung, R.S.M. The role of atorvastatin in regulating the immune response leading to vascular damage in a model of Kawasaki disease. Clin. Exp. Immunol. 2011, 164, 193–201. [Google Scholar] [CrossRef] [PubMed]
- Kato, H.; Sugimura, T.; Akagi, T.; Sato, N.; Hashino, K.; Maeno, Y.; Kazue, T.; Eto, G.; Yamakava, R. Long-term consequences of Kawasaki disease: A 10- to 21-year follow-up study of 594 patients. Circulation 1996, 94, 1379–1385. [Google Scholar] [CrossRef] [PubMed]
- Suzuki, A.; Kamiya, T.; Ono, Y.; Kohata, T.; Okuno, M. Myocardial ischemia in Kawasaki disease: Follow-up study by cardiac catheterization and coronary angiography. Pediatr. Cardiol. 1988, 9, 1–5. [Google Scholar] [CrossRef]
- Terai, M.; Shulman, S.T. Prevalence of coronary artery abnormalities in Kawasaki disease is highly dependent on gamma globulin dose but independent of salicylate dose. J. Pediatr. 1997, 131, 888–893. [Google Scholar] [CrossRef]
- Maddox, R.A.; Holman, R.C.; Uehara, R.; Callinan, L.S.; Guest, J.; Schonberger, L.B.; Nakamura, Y.; Yashiro, M.; Belay, E. Recurrent Kawasaki disease: USA and Japan. Pediatr. Int. 2015, 57, 1116–1120. [Google Scholar] [CrossRef] [Green Version]
- Manlhiot, C.; Millar, K.; Golding, F.; McCrindle, B.W. Improved classification of coronary artery abnormalities based only on cor-onary artery z-scores after Kawasaki disease. Pediatr Cardiol. 2009, 31, 242–249. [Google Scholar] [CrossRef]
- Yeu, B.K.; Menahem, S.; Goldstein, J. Giant Coronary Artery Aneurysms in Kawasaki Disease—The Need for Coronary Artery Bypass. Hear. Lung Circ. 2008, 17, 404–406. [Google Scholar] [CrossRef]
- Kato, H. Cardiovascular complications in Kawasaki disease: Coronary artery lumen and long-term consequences. Prog. Pediatr. Cardiol. 2004, 19, 137–145. [Google Scholar] [CrossRef]
- Kavey, R.E.; Allada, V.; Daniels, S.R.; Hayman, L.L.; McCrindle, B.W.; Newburger, J.W.; Parekh, R.S.; Steinberger, J. Cardiovascular risk reduction in high-risk pediatric patients: A scientific statement from the American Heart Association Expert Panel on Population and Prevention Science; the Councils on Cardiovascular Disease in the Young, Epidemiology and Prevention, Nutrition, Physical Activity and Metabolism, High Blood Pressure Research, Cardiovascular Nursing, and the Kidney in Heart Disease; and the Interdisciplinary Working Group on Quality of Care and Outcomes Research. Circulation 2006, 114, 2710–2738. [Google Scholar] [CrossRef]
- Jiang, J.; Shang, X.; Wang, H.; Xu, Y.-B.; Gao, Y.; Zhou, Q. Diagnostic value of contrast-enhanced ultrasound in thyroid nodules with calcification. Kaohsiung J. Med. Sci. 2015, 31, 138–144. [Google Scholar] [CrossRef] [Green Version]
- Ercan, A.; Senkaya, I.; Semizel, E.; Cil, E. Left ventricular aneurysm in a 4-year-old boy. Tex. Hear. Inst. J. 2005, 32, 614–615. [Google Scholar]
- Meyer, B.J.; Amann, F.W.; Jenni, R.; Bertel, O.; Von Segesser, L.K.; Turina, M. Malignant ventricular arrhythmia in congenital aneurysms of the left ventricle in adulthood. Helvetica Chir. Acta 1992, 58, 479–483. [Google Scholar]
- Mitsomoy, M.F.; Ajaja, M.R.; Fkiri, B.; Haddour, L.; Cheikhoui, Y. Management of the congenital aneurysm of the left ventricle as-sociated with mitral insufficiency in a child: A case report. J. Cardiovac. Thoarc. Res. 2013, 5, 35–36. [Google Scholar]
- Jamshidi, R.; Hornberger, L.K.; Karl, T.R. Left Ventricular Aneurysm in a Child with Severe Combined Immunodeficiency Syndrome. Ann. Thorac. Surg. 2009, 88, 1678–1680. [Google Scholar] [CrossRef]
- Ibanez, B.; James, S.; Agewall, S.; Antunes, M.J.; Bucciarelli-Ducci, C.; Bueno, H.; Caforio, A.L.; Crea, F.; Goudevenos, J.A.; Widimský, P. ESC Scientific Document Group. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2018, 39, 119. [Google Scholar]
- O’Gara, P.T.; Kushner, F.G.; Ascheim, D.D.; Casey, D.E.; Chung, M.K.; de Lemos, J.A.; Ettinger, S.M.; Fang, J.C.; Fesmire, F.M.; Franklin, B.A.; et al. 2013 ACCF/AHA Guideline for the Man-agement of ST-Elevation Myocardial Infarction. J. Am. Coll. Cardiol. 2013, 61, e78–e140. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tsuda, E.; Hirata, T.; Matsuo, O.; Abe, T.; Sugiyama, H.; Yamada, O. The 30-Year Outcome for Patients After Myocardial Infarction Due to Coronary Artery Lesions Caused by Kawasaki Disease. Pediatr. Cardiol. 2010, 32, 176–182. [Google Scholar] [CrossRef] [PubMed]
- Sui, Y.; Teng, S.; Qian, J.; Zhao, Z.; Zhang, Q.; Wu, Y. Treatment outcomes and therapeutic evaluations of patients with left ven-tricular aneurysm. J. Int. Med. Res. 2019, 47, 244–251. [Google Scholar] [CrossRef] [Green Version]
- Tsuda, E.; Arakaki, Y.; Shimizu, T.; Sakaguchi, H.; Yoshimura, S.; Yazaki, S.; Echigo, S. Changes in causes of sudden deaths by decade in patients with coronary arterial lesions due to Kawasaki disease. Cardiol. Young 2005, 15, 481–488. [Google Scholar] [CrossRef]



Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Menahem, S.; Lefkovits, J. Major Complication Following Kawasaki Disease in an Infant—The Development of Apical Infarction and Aneurysm Formation. Children 2021, 8, 981. https://0-doi-org.brum.beds.ac.uk/10.3390/children8110981
Menahem S, Lefkovits J. Major Complication Following Kawasaki Disease in an Infant—The Development of Apical Infarction and Aneurysm Formation. Children. 2021; 8(11):981. https://0-doi-org.brum.beds.ac.uk/10.3390/children8110981
Chicago/Turabian StyleMenahem, Samuel, and Jeffrey Lefkovits. 2021. "Major Complication Following Kawasaki Disease in an Infant—The Development of Apical Infarction and Aneurysm Formation" Children 8, no. 11: 981. https://0-doi-org.brum.beds.ac.uk/10.3390/children8110981